Abstract
Introduction
Alcohol or drug impaired driving can cause motor vehicle crashes, injuries, and death. Estimates of drug impaired driving are difficult to obtain. This study explores self-reported prevalence of and factors associated with alcohol, marijuana, and prescription opioid use and impaired driving among adults aged 21 years and older in the U.S.
Methods
Self-reported data from 3,383 adults in the 2015 Fall ConsumerStyles survey were analyzed. Respondents were asked about alcohol, marijuana, and prescription opioid use and driving while impaired in the last 30 days. Weighted prevalence estimates were calculated. Prevalence ratios and Poisson log-linear regressions were used to identify factors associated with substance use and impaired driving.
Results
Alcohol use was reported by 49.5% (n=1,676) of respondents; of these 4.9% (n=82) reported alcohol impaired driving. Marijuana use was reported by 5.5% (n=187) of respondents; of these 31.6% (n=59) reported marijuana impaired driving. Prescription opioid use was reported by 8.8% (n=298) of respondents; of these 3.4% (n=10) reported prescription opioid impaired driving. Polysubstance use of alcohol and marijuana (concurrent use) was reported by 2.7% (n=93) respondents. Among those, 10.8% (n=10) reported driving impaired by both alcohol and marijuana.
Conclusions
Impaired driving was self-reported among alcohol, marijuana, and prescription opioid users. This report demonstrates the need for more robust alcohol and drug-related data collection, reporting, and analyses, as well as the emerging need for surveillance of marijuana and prescription opioid impaired driving. States can consider using proven strategies to prevent impaired driving and evaluate promising practices.
Keywords: driver safety, impaired driving, alcohol, marijuana, prescription opioid pain relievers
INTRODUCTION
In 2014, there were 28 million people aged 21 years and older who self-reported driving under the influence of illicit drugs or alcohol in the past year (SAMHSA 2015). The 2013/2014 National Roadside Survey reported that among nighttime weekend drivers, 8.3% tested positive for alcohol, 12.6% for marijuana, and 7.3% for prescription or over-the-counter drugs (Berning et al. 2015). It is important to note that testing positive for a drug is indicative of use and not a reliable source to measure impairment. Nevertheless, driving under the influence of alcohol or drugs can cause motor vehicle crashes, injuries, and death (NCSA 2016, Hartman et al. 2013). Among the 22,433 drivers fatally injured in motor vehicle crashes who were tested for alcohol in 2015, 7,646 (34.1%) tested positive for any detectable amount (NHTSA 2015). Alcohol is a significant risk factor for motor vehicle crashes, injuries, and deaths because it delays normal brain function by slowing information processing speed and affecting hand-eye coordination (NCADD 2017). Additionally, as blood alcohol concentration levels increase, impairment also increases (CDC 2017). Among the 17,659 drivers fatally injured in motor vehicle crashes who were tested for any drug in 2015, 2,200 (12.5%) tested positive for marijuana or hashish (NHTSA 2015). Marijuana use has been shown to decrease cognitive functioning and has negative effects on the skills needed for driving, including an increase in lane weaving, poor reaction time, and altered attention to the road (Hartman et al. 2013). Among the 17,659 drivers fatally injured in motor vehicle crashes who were tested for any drug in 2015, 652 (3.7%) tested positive for prescription opioids, such as hydrocodone, oxycodone, morphine, and codeine (NHTSA 2015). Prescription opioids (used medically or non-medically) could put drivers at risk because they can cause sleepiness, dizziness, and confusion (Ramsin et al. 2008). Polysubstance use, especially when substances are used in addition to alcohol, have been shown to have additive or synergistic negative effects on driving. The combination of multiple substances decreases cognitive functioning and increases the risk of motor vehicle crash related injury and death beyond the risk of using a single substance alone (Hartman et al. 2013, Wilson et al. 2014). Drugs are metabolized and tolerated differently in each person, and the effects of polysubstance use are not yet fully understood (Berning et al. 2014, CDC 2017).
There are many more studies on self-reported alcohol impaired driving than on drug impaired driving (SAMHSA 2015, NCSA 2016, Kelly et al. 2004). This is partially due to inconsistent testing of drugs (e.g., testing for tetrahydrocannabinol (THC), marijuana’s main psychoactive component versus metabolites), testing for a limited number of drugs, varying data collection methods, and reporting limitations that make obtaining estimates of drug impaired driving difficult (Berning et al. 2014). The purposes of this exploratory study were to estimate prevalence of and factors associated with alcohol use, alcohol-impaired driving, marijuana use, marijuana-impaired driving, prescription opioid pain reliever use (medical and non-medical), prescription opioid pain reliever impaired driving, polysubstance use and polysubstance-impaired driving among adults aged 21 years and older in the United States (U.S.).
METHODS
In order to explore self-reported substance use and impaired driving, we analyzed a subset of data from the 2015 Fall ConsumerStyles online panel survey administered by Porter Novelli (Washington, D.C.). ConsumerStyles measures health knowledge, attitudes, and behaviors of adults in the U.S. The panel maintains approximately 55,000 panelists and respondents were recruited using both random-digit dial and address-based sampling methods (Appendix A). The survey was conducted online; if needed, households were provided with a laptop computer and access to the Internet. Respondents who completed the survey received reward points worth approximately $5. The Fall ConsumerStyles survey was fielded from September 28, 2015 to October 16, 2015 to 4,665 adults (18 years and older). A total of 3,550 individuals aged 18 years and older completed the survey, for a reported response rate of 76%. Self-reported data from the 3,383 individuals legally able to drink alcohol (aged 21 years and older) were included in this study. Respondents were asked about their use of three types of substances in the last 30 days: alcohol, marijuana/hashish, and prescription opioids (“e.g., Vicodin, OxyContin, Percocet, or hydrocodone”). Prescription opioids may include use as prescribed, non-medical use, misuse, or some combination. Respondents who reported use were then asked if they had driven while impaired in the last 30 days by the substance used with the following questions: “have you driven when you’ve had perhaps too much to drink?”, “have you driven while perhaps under the influence of marijuana or hashish?”, or “have you driven while ‘high’ or experiencing side effects of a prescription opioid pain reliever?” Response options were, “yes,” “no,” or “not sure.” Responses were dichotomized into Yes or No (No and Not sure combined) for analyses. Porter Novelli weighted the data by gender, age, household income, race/ethnicity, household size, education, Census region, metropolitan area status, and prior Internet access to match U.S. Current Population Survey proportions (Census 2014). Secondary analysis of ConsumerStyles data was determined by the Centers for Disease Control and Prevention to be exempt from human subject regulations.
Weighted prevalence estimates were calculated for all 10 outcome variables including: 1) alcohol use, 2) alcohol impaired driving, 3) marijuana use, 4) marijuana impaired driving, 5) prescription opioid use (medical and non-medical), 6) prescription opioid impaired driving, 7) polysubstance alcohol plus marijuana use, 8) polysubstance alcohol plus marijuana impaired driving, 9) polysubstance alcohol plus prescription opioid use, and 10) polysubstance alcohol plus prescription opioid impaired driving. Bivariate analyses (Prevalence Ratios [PR]) using chi-square tests were used to explore empirical associations between demographic variables (Appendix B) and outcome variables 1–5, and 7 (above). Outcomes 6, 8, 9 and 10 were not further explored because sample size was less than 20 for each outcome. Dependent variables that were statistically associated (p ≤ 0.05) with an outcome variable were included in separate Poisson, log-linear regression models for the six outcome variables (outcomes 1–5 and 7). Poisson log-linear regression modeling was selected because it is appropriate to use when calculating multi-variable prevalence ratios among cross-sectional studies with binary outcomes (Barros et al. 2003). The log-linear regression models were constructed manually to calculate adjusted Poisson prevalence ratios (aPR) (Barros et al. 2003), 95% confidence intervals (95% CI) and tested for goodness of fit. Five of the six models had good fit; alcohol use, X2 (10) = 118.4, p<0.001; alcohol impaired driving, X2 (9) = 31.1, p<0.001; marijuana use, X2 (12) = 69.2, p<0.001; prescription opioid use, X2(9) = 81.0, p<0.001; and polysubstance (alcohol and marijuana) use, X2 (9) = 44.4, p<0.001. Marijuana impaired driving did not have good fit, X2 (5) = 9.1, p=0.104 and could not be improved further likely due to small sample size. However, the authors still reported findings on marijuana impaired driving because of the exploratory nature of this study and the large proportion of marijuana users who self-reported driving while impaired by marijuana. Analyses were performed using SPSS (IBM SPSS Statistics, Version 23.0).
RESULTS
A majority of the 3,383 respondents were White, non-Hispanic (65.8%), aged 45 and older (56.4%), and had completed a high school degree or less education (40.9%) (Appendix A). This is similar to the 2014 demographic Census population estimates (Census 2014).
Alcohol
Alcohol use in the past 30 days was reported by 49.5% (n =1,676) of respondents. Alcohol use was more prevalent among people aged 21 to 34 years (aPR=1.27, 95% CI 1.14–1.40) compared with those aged 35 to 44 years, education levels of some college (aPR=1.18, 95% CI 1.08–1.28) and Bachelor’s degree or higher (aPR=1.17, 95 % CI 1.08–1.27) compared with those who completed a high school degree or less education, males (aPR=1.15, 95% CI 1.08–1.22) compared with females, head of households (aPR=1.13, 95% CI 1.02–1.24) compared with those who were not head of households and those who had an annual household income between $40,000 and $74,999 (aPR=1.32, 95% CI 1.19–1.47) and $75,000+ (aPR=1.59, 95% CI 1.441.75) compared with less than $40,000.
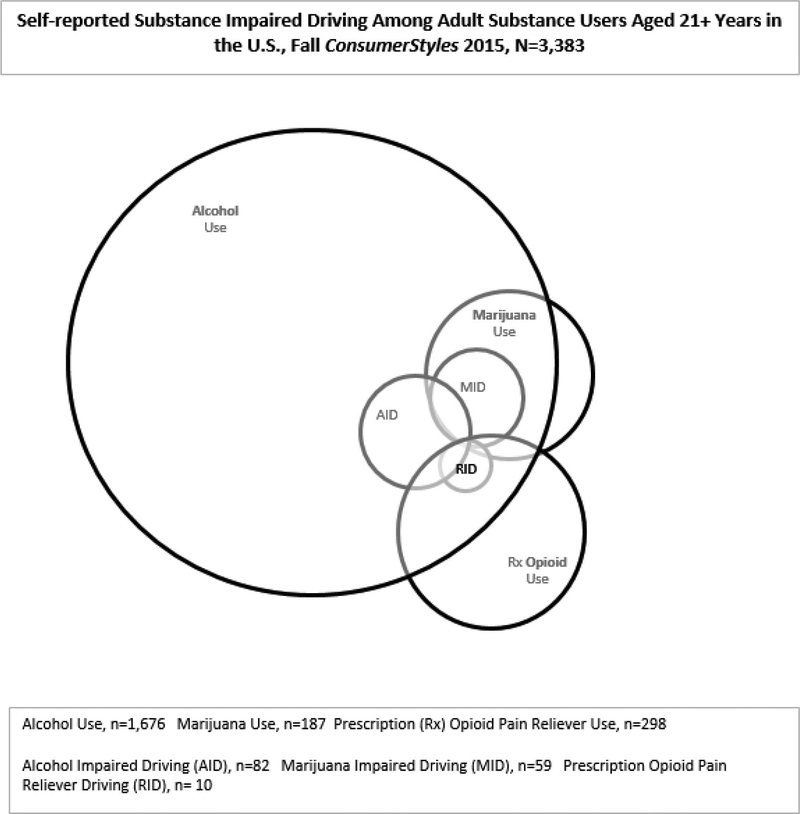
Among alcohol users, 4.9% (n=82) reported alcohol impaired driving (Figure). Alcohol impaired driving was less prevalent among people aged 45 years and older (aPR=0.58, 95% CI 0.33–0.99) compared with 35 to 44 year olds, head of households (aPR=0.47, 95% CI 0.28–0.79) compared with those who were not head of households, had an annual household income of $40,000 to $74,999 (aPR=0.41, 95% CI 0.21–0.80) compared with less than $40,000, and respondents who lived in the South Census region (aPR=0.51, 95 %CI 0.29–0.88) and West region (aPR=0.51, 95% CI 0.27–0.95) compared with the Northeast Census region (Table 1).
Figure 1.
TABLE 1.
Alcohol Use and Alcohol Impaired Driving by Selected Characteristics Among Adults (21+ Years) in the US, ConsumerStyles 2015 (Appendix C, Table A)
| Alcohol Use, N=1676 | Alcohol Impaired Driving, N=82 | |
|---|---|---|
| aPR (95% CI) | aPR (95% CI) | |
| 21–34 | 1.27 (1.14–1.40)* | 0.61 (0.34–1.10) |
| 35–44 | <ref> | <ref> |
| 45+ | 0.99 (0.90–1.08) | 0.58 (0.33–0.99)* |
| High School graduate or less | <ref> | b |
| Some college | 1.18 (1.08–1.28)* | b |
| Bachelor’s degree or higher | 1.17 (1.08–1.27)* | b |
| White, non-Hispanic | <ref> | b |
| Other, multiple race, Hispanic | 0.96 (0.89–1.03 | b |
| Female | <ref> | <ref> |
| Male | 1.15 (1.08–1.22)* | 1.52 (0.98–2.36) |
| No | <ref> | <ref> |
| Yes | 1.13 (1.02–1.24)* | 0.47 (0.28–0.79)* |
| <$40,000 | <ref> | <ref> |
| $40,000 to $74,999 | 1.32 (1.19–1.47)* | 0.41 (0.21–0.80)* |
| $75,000 + | 1.59 (1.44–1.75)* | 0.84 (0.52–1.37) |
| Married | <ref> | b |
| Not Married | 0.95 (0.87–1.03) | b |
| Northeast | b | <ref> |
| Midwest | b | 0.72(0.39–1.32) |
| South | b | 0.51 (0.29–0.88)* |
| West | b | 0.51 (0.27–0.95)* |
a = not all respondents answered every question
b = not included in model, p>0.05
aPR=adjusted Prevalence Ratio
95% CI= confidence interval of 95%
p-value <0.05 and statistically significant
Marijuana
Marijuana use in the last 30 days was reported by 5.5% (n=187) of respondents. Marijuana use was more prevalent among males (aPR=1.76, 95% CI 1.32–2.34) compared with females. Among marijuana users, 31.6% (n=59) reported driving while marijuana impaired (Figure). Although the marijuana impaired driving model did not have good fit, it showed that marijuana impaired driving was more prevalent among other, multiple race, and Hispanics (aPR=1.51, 95% CI 1.01–2.25) compared with White, non-Hispanics, and among males (aPR=1.70, 95% CI 1.022.84) compared with females (Table 2).
TABLE 2.
Marijuana Use and Marijuana Impaired Driving by Selected Characteristics Among Adults (21+ Years) in the US, ConsumerStyles 2015 (Appendix C, Table B)
| Marijuana Use, N=187 | Marijuana Impaired Driving, N=59 | |
|---|---|---|
| aPR (95% CI) | aPR (95% CI) | |
| 21–34 | 1.53 (0.99–2.36) | 1.73 (0.79–3.79) |
| 35–44 | <ref> | <ref> |
| 45+ | 0.71 (0.46–1.08) | 1.29 (0.60–2.80) |
| High School degree or less | <ref> | b |
| Some college | 1.05 (0.75–1.46) | b |
| Bachelor’s degree or higher | 0.73 (0.50–1.06) | b |
| White, non-Hispanic | b | <ref> |
| Other, multiple race, Hispanic | b | 1.51 (1.01–2.25)* |
| Female | <ref> | <ref> |
| Male | 1.76 (1.32–2.34)* | 1.70 (1.02–2.84)* |
| No | <ref> | <ref> |
| Yes | 0.91 (0.65–1.28) | 0.97 (0.61–1.55) |
| <$40,000 | <ref> | b |
| $40,000 to $74,999 | 0.77 (0.54–1.11) | b |
| $75,000 + | 0.74 (0.51–1.06) | b |
| Married | <ref> | b |
| Not Married | 1.17 (0.83–1.65) | b |
| Northeast | <ref> | b |
| Midwest | 1.08 (0.68–1.70) | b |
| South | 0.80 (0.53–1.22) | b |
| West | 1.44 (0.96–2.18) | b |
a = not all respondents answered every question
b = not included in model, p>0.05
aPR=adjusted Prevalence Ratio
95%CI= confidence interval of 95%
p-value <0.05 and statistically significant
Prescription Opioid Pain Relievers
In the last 30 days, 8.8% (n=298) of respondents reported prescription opioid use (medical and non-medical). Prescription opioid use was more prevalent among those aged 45 years or older (aPR=1.46, 95% CI 1.04–2.04) compared with those 35 to 44 years and those who lived in the Midwest (aPR=1.61, 95% CI 1.10–2.35), South (aPR=1.45, 95% CI 1.01–2.08), and West (aPR=1.61, 95% CI 1.11–2.34) Census regions compared with the Northeast Census region. Prescription opioid use was less prevalent among those with a Bachelor’s degree or higher (aPR=0.40, 95% CI 0.29–0.56) compared with those who completed a high school degree or less education and those who had an annual household income of $40,000 to $74,999 (aPR=0.68, 95% CI 0.52–0.90) compared with less than $40,000 (Table 3). Of those reporting prescription opioid use, 3.4% (n=10) reported driving while “high” or experiencing side effects of prescription opioids (Figure).
TABLE 3.
Prescription Opioid Use by Selected Characteristics Among Adults (21+ Years) in the US, Fall ConsumerStyles 2015 (Appendix C, Table C)
| Prescription Opioid Use, N=298 | |
|---|---|
| aPR (95% CI) | |
| 21–34 | 0.83 (0.55–1.26) |
| 35–44 | <ref> |
| 45+ | 1.46 (1.04–2.04)* |
| High School degree or less | <ref> |
| Some college | 0.82 (0.64–1.05) |
| Bachelor’s degree or higher | 0.40 (0.29–0.56)* |
| White, non-Hispanic | b |
| Other and multiple race, non-Hispanic | b |
| Female | b |
| Male | b |
| No | b |
| Yes | b |
| <$40,000 | <ref> |
| $40,000 to $74,999 | 0.68 (0.52–0.90)* |
| $75,000 + | 0.79 (0.61–1.04) |
| Married | b |
| Not Married | b |
| Northeast | <ref> |
| Midwest | 1.61 (1.10–2.35)* |
| South | 1.45 (1.01–2.08)* |
| West | 1.61 (1.11–2.34)* |
a = not all respondents answered every question
b = not included in model
aPR=adjusted Prevalence Ratio
95% CI= confidence interval of 95%
p-value <0.05 and statistically significant
Poly Substance
In the last 30 days, 2.7% (n=93) of respondents reported using both alcohol plus marijuana at the same time. Alcohol plus marijuana use was less prevalent among those 45 years or older (aPR=0.56, 95% CI 0.32–0.97) compared with those aged 35 to 44 years, and those with an annual household income of $40,000 to $74,999 (aPR=0.52, 95% CI 0.31–0.87) and $75,000+ (aPR=0.55, 95% CI 0.34–0.88) compared with an income of less than $40,000 (Table 4). Among respondents, 0.5% (n=17) reported using alcohol plus prescription opioids at the same time. Impaired driving following the use of any substance was reported by 4.1% of respondents (n = 139); of these 51.8% (n = 72) reported impaired driving by alcohol only, 34.5% (n = 48) reported impaired driving by marijuana only, and 6.5% (n = 9) reported impaired driving by prescription opioid only. Among the 139 respondents who reported impaired driving, nine (6.5%) reported driving while impaired by alcohol plus marijuana, one (0.7%) reported driving while impaired by alcohol plus marijuana plus prescription opioids. No respondents reported impaired driving with alcohol plus prescription opioids or marijuana plus prescription opioids.
TABLE 4.
Self-Reported Polysubstance Use by Selected Characteristics Among Adults (21+ Years) in the US, Fall ConsumerStyles 2015 (Appendix C, Table D)
| Alcohol and Marijuana Use, n=93 | |
|---|---|
| aPR (95% CI) | |
| 21–34 | 1.08 (0.63–1.85) |
| 35–44 | <ref> |
| 45+ | 0.56 (0.32–0.97)* |
| High School degree or less | <ref> |
| Some college | 1.43 (0.91–2.25) |
| Bachelor’s degree or higher | 0.77 (0.44–1.36) |
| White, non-Hispanic | <ref> |
| Other and multiple race, non-Hispanic | 1.32 (0.88–1.97) |
| Female | <ref> |
| Male | 1.46 (0.98–2.20) |
| No | <ref> |
| Yes | 0.70 (0.44–1.10) |
| <$40,000 | <ref> |
| $40,000 to $74,999 | 0.52 (0.31–0.87)* |
| $75,000 + | 0.55 (0.34–0.88)* |
| Married | b |
| Not Married | b |
| Northeast | b |
| Midwest | b |
| South | b |
| West | b |
a = not all respondents answered every question
b = not included in model
aPR=adjusted Prevalence Ratio
95% CI= confidence interval of 95%
p-value <0.05 and statistically significant
DISCUSSION
Although reports have described motor vehicle crashes involving drug use (Kelly et al. 2004) and self-reported “illicit” drug use (SAMHSA 2015), this report is the most geographically diverse study to explore self-reported marijuana and prescription opioid impaired driving separately. Of the substances respondents were asked about in this 2015 study, alcohol was the most frequently used (49.5%), followed by prescription opioids (8.8%), and then marijuana (5.5%). Similar to our findings, the National Survey on Drug Use and Health reported that within the past 30 days alcohol was used among half the population (NIAAA 2017, SAMHSA 2014). Among all respondents in this study, 2.4% reported driving while alcohol impaired. This percentage is higher than a 2012 nationally representative study among U.S. adults that estimated 1.8% of respondents self-reported driving while alcohol-impaired and estimated 121 million drunk driving episodes occurred during that year (Jewett et al. 2015). Effective interventions for reducing alcohol-impaired driving include: increasing alcohol ignition interlock use for all offenders of driving while impaired (including first time offenders) (Voas et al. 2016); the use of publicized sobriety checkpoints (GHSA 2017); and saturation patrols (Goodwin et al. 2015). Studies on self-reported impaired driving by substances other than alcohol are limited. Marijuana was reportedly used the least in this study and the small sample size likely hindered the goodness of fit of the marijuana impaired driving model. The purpose of reporting the results of the marijuana impaired driving model here was not to interpret a causal path from marijuana user (exposure) to marijuana impaired driving (outcome), but rather to aid in hypothesis generation for more in-depth research. Regardless, our finding that among marijuana users, almost one third self-reported marijuana impaired driving is comparable with previous research findings. In 2016, a survey conducted among Colorado adults (18+ years) reported 57% of marijuana users self-reported driving within two hours of consuming marijuana (NRC 2017). In addition, a study conducted among first year college students from two large public universities in Wisconsin and Washington reported that 31% of marijuana users reported driving after marijuana use within the last 28 days (Whitehill et al. 2014). Although there are differences in methodology (self-reported driving after use versus self-reported impaired driving) and study population (younger population), all three studies, including this one, highlight the large proportion of marijuana users engaging in impaired driving and/or driving after use.
The large proportion of users that drive after consuming marijuana is of concern because there is sound science on the effects marijuana imposes on brain function (Hartman et al. 2013). Despite this concern, marijuana was perceived as the least harmful drug among 15 substance types in a study conducted in the U.S. and the United Kingdom (U.K.) (Morgan et al. 2013).
Approximately 6,000 drug users reported how they perceived harm based on long term physical risk and risk to society (i.e. risk of damaging family relationships, damage to property, or cost of policing). Among the drug users, alcohol ranked the most harmful, opioids ranked 3rd, and marijuana ranked 14th (Morgan et al. 2013).
With the legalization of either recreational or medical marijuana use in many states (NCSL 2017), and the low perceptions of the risk of harm by marijuana use (Morgan et al. 2013, Allen et al. 2016), the potential for an increase in marijuana impaired driving, motor vehicle crashes, and their resulting injuries, deaths, and costs may be possible. Some studies have shown an association between marijuana use and motor vehicle crashes, others have not (Asbridge et al. 2012). The limitations of databases, such as the Fatality Analysis Reporting System (FARS) and the National Roadside Survey, for drugged driving research contributes to the contradictory results (Romano et al. 2017). At the state level, there is variability among forensic laboratories for qualitative (presence of active THC and/or metabolites) and quantitative (amount of active THC and/or metabolites) testing of THC (Berning et al. 2014) which in turn affects drugged driving data reporting within FARS. Additionally, the complex toxicology of marijuana makes assessing its effects on crash risk complicated as there is a rapid increase and subsequent decrease of THC in blood after use. Marijuana impairment is non-linear with THC blood levels (Bondallaz et al. 2016). Effective interventions to reduce marijuana impaired driving include substance use screening and brief intervention (Harris et al. 2014), and expanded training for law enforcement to recognize drug impaired drivers (i.e., Drug Recognition Experts [DRE]) (Hartman et al. 2016, Celeste 2017).
While state laws defining alcohol impaired driving are generally similar (IIHS 2017), marijuana use and driving laws (NCSL 2017) for each state vary widely and are changing rapidly, which contributes to the variability in data collection and forensic testing. As of August 2015, the year of our study, nine states had zero tolerance laws (illegal to drive with any measurable amount of specified drug) for THC or metabolites, three states had zero tolerance laws for THC but no restriction on metabolites, five states had per se laws (illegal to drive with excessive amounts of a specified drug) with states setting variable cut off limits of allowable THC in the body, and one state had a reasonable inference law (court considers all reasonable inferences for decisions) for THC (GHSA 2016). Other issues that make research on marijuana impaired driving challenging are that an accurate roadside drug test does not exist, marijuana can remain in a user’s system for days or weeks after use, and drivers are not always tested for drugs. If drivers are tested following a crash they can have multiple drugs in their system making identification of the drug or drugs that contributed to the crash difficult (CDC 2017). Standardized and expanded toxicology testing, improved data collection and reporting paired with more robust research are needed to understand marijuana impairment and how it affects driving ability and crash risk. According to the 2007 National Roadside Survey, 1.6% of all drivers (both during the daytime and nighttime) tested positive for narcotic (opioid) analgesics (Lacey et al. 2009, Lacey et al. 2011). Studies focusing on prescription opioids, their effects on driving, and prevalence of driving under the influence of prescription opioids are also limited (Rudisill et al. 2016). However, a case-control study of patients who sustained motor vehicle crash injuries and controls (patients without motor vehicle crash injuries) from 2003 to 2011, found that prescription opioids with daily dosages ≥20 morphine milligram equivalents (MME) were associated with increased risk of a motor vehicle crash among drivers (aged 18 to 64) admitted to an emergency department (Gomes et al. 2013). In addition to known side effects of prescription opioids, initial dosing, tolerance (loss of analgesic potency) and physical dependence (altered physiological state) should also be considered when determining impaired driving by prescription opioids (Ramsin et al. 2008). Effective interventions to reduce prescription opioid impaired driving include substance use screening and brief intervention (Harris et al. 2014), and expanded training for law enforcement to recognize drug impaired drivers (i.e., DRE) (Hartman et al. 2016, Celeste 2017).
Polysubstance use, especially when substances are used in addition to alcohol, have been shown to have additive or synergistic negative effects on driving. The combination of multiple substances decreases cognitive functioning and increases the risk of motor vehicle crash related injury and death beyond the risk of using a single substance alone (Hartman et al. 2013, Wilson et al. 2014). Drugs are metabolized and tolerated differently in each person, and the effects of polysubstance use are not yet fully understood (Berning et al. 2014, CDC 2017). A case-control study using 2007 data reported that the odds of involvement in a fatal motor vehicle crash were increased when drivers tested positive for alcohol (16 fold), marijuana (2 fold), and alcohol and marijuana (25 fold), compared with drivers who tested negative for alcohol and marijuana (Chihuri et al. 2017). In 2015 among those killed in a motor vehicle crash that were tested for alcohol, marijuana, and prescription opioids, approximately 1,200 (7% of those tested) had alcohol and at least one other substance in their system (NHTSA 2015), which is similar to our findings. However, marijuana and prescription opioid testing may not be ordered because a positive alcohol test is sufficient for a driving while intoxicated (DWI) charge or conviction. Improved data collection, data linkage between law enforcement reports, medical and toxicology data, as well as standardization of data reporting are needed to improve monitoring and our understanding of impaired driving. More driving simulation studies examining the effect of polysubstance use on driving ability are needed to determine the extent of additive and synergistic effects of each drug on crash risk.
The findings in this exploratory study are subject to limitations. Although, ConsumerStyles is representative of the US population, a probability sample, uses a random-digit-dial and internet panel, it is a cross-sectional survey (Yeager et al. 2011). Second, readers must interpret results with caution because the overall small sample size may compromise the external validity of our results, therefore making our findings lack generalizability. This is especially true for the marijuana impaired driving outcome since the model was not a good fit and could not be improved due to the small sample size of marijuana users in this study or this study may have lacked variables that would explain the lack of fit. Regardless, the marijuana impaired driving results were reported because of the large proportion of marijuana users that reported driving while marijuana impaired and to allow for hypothesis generation for future research.
Additionally, a model was not built for prescription opioid impaired driving due to small sample size; therefore, our findings around prescription opioid impaired driving were limited. Third, the study used self-reported alcohol and drug use and impaired driving data which may lead to inaccurate accounts of impaired driving (impairment was not defined for respondents and relied on their judgment). However, the Driving under the Influence of Drugs, Alcohol and Medicines (DRUID) study reported that an early indicator for alcohol impairment was when subjects “felt” intoxicated (Schnabel et al. 2010) therefore, subjects understand that when they “feel” impaired, that they are impaired. In addition, the alcohol impaired driving question used in this survey has also been used in CDC’s national Behavioral Risk Factor Surveillance System survey for many years (CDC 2017). Unfortunately, we found no such indicator for impairment due to substances other than alcohol in the literature.
Despite these limitations and challenges, impaired driving remains a significant contributor to motor vehicle crash deaths with over 10,000 people dying in alcohol impaired driving crashes each year (NCSA 2015) and an unknown number dying in drug impaired or polysubstance impaired driving crashes. The results of our study re-affirm the continued need for alcohol impaired driving surveillance and prevention as well as the emerging need for marijuana and prescription opioid impaired driving surveillance and prevention. This report should be used for hypothesis generation and demonstrates the need for more robust alcohol and drug-related data collection, reporting, and analyses. Further research on drug-impaired related crashes (fatal and non-fatal) should include the following: 1. toxicology results of active components of drugs to determine drug concentration levels associated with impairment, 2. behavioral test results obtained through DRE evaluation (Hartman et al. 2016) reports. The combination of toxicology results and DRE reports will increase our understanding of individual impairment differences, the degree of driving impairment among different types of drugs, and the effects of polysubstance (alcohol and drugs) use in addition to individual drug effects on driving. Surveillance of crashes involving drug impaired driving would be strengthened by the standardization and expansion of forensic toxicology testing methodologies and reporting (Peterson et al. 2018) across states and jurisdictions. Standardized and expanded testing and reporting across states from law enforcement and healthcare providers could inform future research and prevention efforts.
Alcohol and drug impaired driving, the low perceived risks of marijuana use (Kelly et al. 2004, Allen et al. 2016), and the increase in opioid use, misuse, and opioid use disorder (HHS 2016) are evolving safety concerns and underscore the need for implementation of effective interventions to prevent alcohol, drug, and polysubstance impaired driving. Drugs and alcohol interfere with the brain’s ability to function properly and understanding how and when drugs impair cognition will inform prevention efforts for drug and polysubstance impaired driving (CDC 2017). Effective interventions for reductions in substance use and impaired driving include substance use screening and brief intervention (Harris et al. 2014), increased alcohol ignition interlock use for all offenders of driving while impaired (Voas et al. 2016), expanded training for law enforcement to recognize drug impaired drivers (i.e., DRE) (Hartman et al. 2016, Celeste 2017), the use of publicized sobriety checkpoints (GHSA 2017) and saturation patrols (Goodwin et al. 2015).
Supplementary Material
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- Allen JA, Davis KC, Duke JC, Nonnemaker JM, Bradfield BR, Farrelly MC, et al. , Association between self-reports of being high and perceptions about the safety of drugged and drunk driving. Health Education Research, 2016. [DOI] [PubMed] [Google Scholar]
- Asbridge M, Hayden JA, Cartwright JL, Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ, 2012. 344: p. e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barros A, Hirakata V, Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Medical Research Methodology, 2003. 3: p. 21–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berning A, Compton R, Wochinger K, Results of the 2013–2014 National Roadside Surveyof alcohol and drug use by drivers. 2015, National Highway Traffic Safety Administration: Washington, DC. [Google Scholar]
- Berning A, Smither DD, Understanding the Limitations of Drug Test Information, Reporting, and Testing Practices in Fatal Crashes. 2014.
- Bondallaz P, Favrat B, Chtioui H, Fornari E, Maeder P, Giroud C, Cannabis and its effects on driving skills. Forensic Science International, 2016. 268: p. 92–102. [DOI] [PubMed] [Google Scholar]
- Celeste MA, A Judicial Perspective on Expert Testimony in Marijuana Driving Cases. Journal of Medical Toxicology, 2017. 13(1): p. 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census.gov: American Community Survey Estimates 2014. 2017; Available from: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml.
- Centers for Disease Control and Prevention: Behavioral Risk Factor Surveillance System (BRFSS). 2017. Atlanta, GA: [Cited August/25/2017]; Available from: http://www.cdc.gov/brfss/. [Google Scholar]
- Centers for Disease Control and Prevention: What are the effects of blood alcohol concentration (BAC)? Impaired Driving: Get the Facts 2017 January 26, 2017. [Cited May/22/2017]; Available from: https://www.cdc.gov/motorvehiclesafety/impaired_driving/impaired-drv_factsheet.html.
- Centers for Disease Control and Prevention: What You Need to Know About Marijuana Use and Driving. 2017; Available from: https://www.cdc.gov/marijuana/pdf/marijuana-driving-508.pdf.
- Chihuri S, Li G, Chen Q, Interaction of marijuana and alcohol on fatal motor vehicle crash risk: a case–control study. Injury Epidemiology, 2017. 4: p. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services: The Opioid Epidemic: By the Numbers, Department of Health and Human Services; 2016: Washington, DC. [Google Scholar]
- Gomes T, Redelmeier D, Juurlink D, Dhalla I, Camacho X, Mamdani M, Opioid dose and risk of road trauma in Canada: a population-based study. JAMA internal medicine, 2013. 173(3): p. 196–201. [DOI] [PubMed] [Google Scholar]
- Goodwin A, Thomas L, Kirley B, Hall W, O’Brien N, Hill K, Countermeasures that work: A highway safety countermeasure guide for State highway safety offices, Eighth edition, National Highway Traffic Safety Administration, Editor. 2015: Washington, D.C. [Google Scholar]
- Governors Highway Safety Association: Drug-Impaired Driving: A Guide for What States Can Do, Governors Highway Safety Association; 2016. p. 51. [Google Scholar]
- Governors Highway Safety Association. Sobriety Checkpoint Laws. State Laws and Funding[cited June/14/2017]; Available from: http://www.ghsa.org/html/stateinfo/laws/checkpoint_laws.html.
- Harris S, Louis Jacques J, Knight J, Screening and brief intervention for alcohol and otherabuse. Adolescent medicine, 2014. 25(1): p. 126–156. [PubMed] [Google Scholar]
- Hartman RL, Huestis MA, Cannabis effects on driving skills. Clin Chem, 2013. 59(3): p. 478–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman RL, Richman JE, Hayes CE, Huestis MA, Drug Recognition Expert (DRE)examination characteristics of cannabis impairment. Accident Analysis & Prevention, 2016. 92: p. 219–229. [DOI] [PubMed] [Google Scholar]
- Insurance Institute for Highway Safety: Impaired Driving: DUI/DWI. 2017 July 2017 [Cited July/18/2017]; Available from: http://www.iihs.org/iihs/topics/laws/dui?topicName=impaired-driving.
- Jewett A, Shults RA, Banerjee T, Bergen G, Alcohol-Impaired Driving Among Adults -United States, 2012. MMWR Morb Mortal Wkly Rep, 2015. 64(30): p. 814–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly E, Darke S, and Ross J, A review of drug use and driving: epidemiology, impairment, risk factors and risk perceptions. Drug and Alcohol Review, 2004. 23(3): p. 319–344. [DOI] [PubMed] [Google Scholar]
- Lacey JH, Kelley-Baker T, Furr-Holden D, Voas RB, Romano E, Ramirez A, et al. , 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Drug Results, National Highway Traffic Safety Administration; 2009: Washington DC. [Google Scholar]
- Lacey JH, Kelley-Baker T, Voas RB, Romano E, Furr-Holden CD, Torres P, et al. , Alcohol- and drug-involved driving in the United States: methodology for the 2007 National Roadside Survey. Evaluation review, 2011. 35(4): p. 319–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CJA, Noronha LA, Muetzelfeldt M, Fielding A, Curran HV, Harms and benefits associated with psychoactive drugs: findings of an international survey of active drugusers. Journal of Psychopharmacology (Oxford, England), 2013. 27(6): p. 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Statistics and Analysis: Alcohol-impaired Driving: 2015 Data, National Center for Statistics and Analysis; 2016, [Google Scholar]
- National Conference of State Legislatures: State Medical Marijuana Laws. 2017 [cited June/3/2017]; Available from: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- National Council on Alcoholism and Drug Dependence: Driving While Impaired --Alcohol and Drugs 2017 [cited June/14/2017] ; Available from: https://www.ncadd.org/about-addiction/driving-while-impaired-alcohol-and-drugs.
- National Highway Traffic Safety Administration. Fatality Analysis Reporting System. 2015 [September/12/2016]; Available from: http://www-fars.nhtsa.dot.gov/QueryTool/QuerySection/SelectYear.aspx.
- National Institute on Alcohol Abuse and Alcoholism: Alcohol Facts and Statistics. 2017;Available from: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-facts-and-statistics.
- National Research Center, Inc. 2017. 2016 Mail Survey about Driving Behaviors Colorado Department of Transportation. Boulder, CO: pp. 135. [Google Scholar]
- Peterson A, Sauber-Schatz E, Mack K, Ability to monitor driving under the influence of marijuana among non-fatal motor vehicle crashes: An evaluation of the Colorado electronicaccident reporting system. 2018. Journal of Safety Research. Available from:https://www.sciencedirect.com/science/article/pii/S002243751830149X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsin BM, Trescot AM, Sukdeb D, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid Complications and Side Effects. Pain Physician Journal, 2008. 11(2S): p. S105–S120. [PubMed] [Google Scholar]
- Romano E, Torres-Saavedra P, Voas RB, Lacey JH, Marijuana and the Risk of Fatal CarCrashes: What Can We Learn from FARS and NRS Data? The Journal of Primary Prevention, 2017. 38(3): p. 315–328. [DOI] [PubMed] [Google Scholar]
- Rudisill TM, Motao Z, Kelley GA, Pilderton C, Rudisill BR, Medication use and the risk of motor vehicle collisions among licensed drivers: A systematic review. Accident Analysis &Prevention, 2016. 96: p. 255–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnabel E, Hargutt V, Krüger H-P., Meta-analysis of empirical studies concerning the effects of alcohol on safe driving, in Driving under the Influence of Drugs, Alcohol and Medicines. 2010, University of Wuerzburg: Germany. [Google Scholar]
- Substance Abuse and Mental Health Service Administration: Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, in NSDUH Series H-48, Substance Abuse and Mental Health Services Administration. 2014: Rockville, MD. [Google Scholar]
- Substance Abuse and Mental Health Service Administration: Results from the 2014 National Survey on Drug Use and Health: Detailed Tables, Substance Abuse and Mental Health ServiceAdministration, Editor. 2015, Center for Behavioral Health Statitistics and Quality: Rockville, MD. [Google Scholar]
- Voas R, Tippetts AS, Bergen G, Grosz M, Marques P, Mandating Treatment Based on Interlock Performance: Evidence for Effectiveness. Alcoholism: clinical and experimental research, 2016. 40(9): p. 1953–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehill JM, Rivara FP, Moreno MA, Marijuana-using drivers, alcohol-using drivers, and their passengers: Prevalence and risk factors among underage college students. JAMA Pediatrics, 2014. 168(7): p. 618–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson FA, Stimpson JP, Pagán JA, Fatal Crashes from Drivers Testing Positive for Drugs in the U.S., 1993–2010. Public Health Reports, 2014. 129(4): p. 342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, Krosnick JA, Chang L, Javitz HS, Levendusky MS, Simpser A, et al. , Comparing the Accuracy of RDD Telephone Surveys and Internet Surveys Conducted with Probability and Non-Probability Samples. Public Opinion Quarterly, 2011. 75(4): p. 709–747. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.