Abstract
The authors describe the clinical investigation and progress of a 13‐year‐old girl diagnosed with hypertension 4 years prior to her admission. A thorough history was taken and physical examination performed. Laboratory analysis and relevant radiological evaluation were obtained in order to determine the etiology for suspected secondary hypertension, and later to differentiate between the possible causes of hyperreninemic hypertension. The patient had an accessory left renal artery, presumptively leading to renin secretion by the underperfused kidney. The patient was treated medically with spontaneous resolution of her hypertension and near normalization of plasma renin activity. On repeat imaging, the artery was not demonstrated. The authors concluded that the diagnosis of hyperreninemic hypertension in young ages should prompt investigation for the etiology. However, cautious observation is a valid option that might lead to spontaneous resolution.
Case Report
We describe a 13‐year‐old girl diagnosed with hypertension. The patient complained of severe headaches since the age of 7 years. After 2 years, a diagnosis of hypertension, with blood pressure (BP) values up to 170/90 mm Hg (height‐ and age‐adjusted 95th percentile 119/79 mm Hg), was determined. Her parents had no relevant medical history, whereas the mother's sister (aged 37 years) experienced migraines. In addition, both the paternal grandmother and great‐grandmother had hypertension presenting during adulthood (>60 years). In light of the high BP values, target organs had been evaluated, including fundoscopy that revealed a mild bilateral hypertensive retinopathy and echocardiography that demonstrated changes secondary to systemic hypertension with preserved left ventricular function. Treatment with amlodipine was initiated and later replaced with enalapril, achieving normal BP values.
During her initial evaluation in the community, the patient underwent investigation for secondary hypertension etiologies. This included kidney and renal arteries ultrasonography with Doppler, 24‐hour urinary collection for vanilmandelic acid, and thyroid function tests, which were all within reference ranges. In contrast, both plasma aldosterone (PA) levels (89.4 ng/mL; reference range, 1.5–50) and plasma renin activity (PRA; 13.9 ng/mL/h; reference range, 0.1–2.8) were elevated, as was chromogranin A plasma level (152 ng/mL; reference range, 31–94). Thus, the workup focused on finding the etiology for excessive renin production, and included angiographic computerized tomography (CT) of the renal arteries, which was interpreted as a narrowing of the left renal vein. The patient was then referred for evaluation at the National Institutes of Health (NIH) clinical center for further evaluation.
The patient first admitted to the NIH Clinical Center complaining of fatigue and headaches. Her BP was 106/54 mm Hg (between 50th and 90th percentile adjusted to height and age), while being treated with enalapril 2.5 mg PO once daily. Her body mass index (BMI) was 16.9 kg/m2 (between 25th and 50th percentile for her age). She underwent a workup for hypertension, including protein/creatinine ratio, creatinine clearance, urinary metanephrines, and midnight plasma cortisol measurements, which were all within normal limits. Her PRA level was elevated (8.7 ng/mL/h; reference range, 0.9–2.9), whereas her PA levels were within reference range (7.4 ng/dL; reference range, 1.5–50), and both were measured during treatment with enalapril. Findings from ultrasonography of the kidneys showed an undetermined lesion near the left kidney that was interpreted as either accessory renal artery or a renal tumor. Results from magnetic resonance imaging (MRI) were negative for renal mass, and CT angiography findings showed a small caliber accessory renal artery supplying the left upper pole (FigureA). Both 18‐Fluorodeoxyglucose positron emission tomography and Indium‐111 pentetreotide scintigraphy (octreoscan) did not show any pathological uptake to suggest the presence of a tumor. The patient was then referred to renal venous sampling, which showed lateralization to the right (FigureB). Since the patient's BP was well controlled and the diagnosis could not be determined, she was discharged and advised to continue her antihypertensive treatment.
Figure 1.
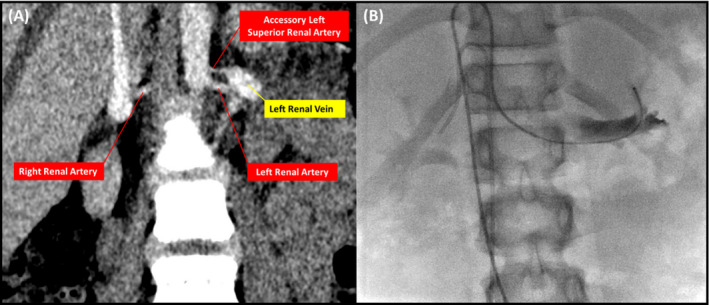
Findings from computed tomographic angiography of the abdomen showing small accessory left superior renal artery (A) and renal venous catheter with its tip placed in the draining vein of the superior pole of the left kidney (B).
Two months following her evaluation at the NIH Clinical Center, the patient's BP values spontaneously normalized and her medical treatment was gradually withdrawn to complete discontinuation. The patient returned for a follow‐up visit in March 2016. She received no medical treatment and had normal BP measurements. Repeat ultrasonography showed normal vascularity, with a possible artifact on the upper pole of the right kidney. Her PRA level was slightly elevated (5.1 ng/mL/h; reference range, 0.9–2.9) but lower compared with earlier measurements, and her PA value was within reference range (34 ng/mL; reference range, 1.5–50) and lower compared with her PA value at presentation.
Discussion
Hypertension in childhood is defined as systolic and/or diastolic values >95th percentile, with a prevalence of 1.6% in the United States among children aged 8 to 17 years.1 In contrast to high BP presenting in adulthood, which is mainly attributed to essential hypertension, secondary hypertension is the main etiology among children, reaching a prevalence of 98% among children younger than 15 years.2 Renal parenchymal disease is the etiology among most patients presenting between the ages of 6 and 10 years with hypertension.3 Other etiologies include renal vascular disease, aortic coarctation, and more rarely systemic arteritis; tumors such as neuroblastoma and Wilms tumor; endocrine diseases such as adrenocortical hyperfunctioning states, reninoma, thyrotoxicosis, pheocromocytoma; and finally neurologic disorders.3
The patient described here experienced hyperreninemic hypertension, narrowing the differential diagnosis to either renin‐secreting tumor or renal hypoperfusion caused by renal artery stenosis. Thus, ultrasonography of the kidneys was performed, raising suspicion for reninoma, which was not supported using other modalities including MRI and CT. Moreover, the spontaneous resolution of her hypertension and the decline in renin over time is not in agreement with autonomous renin secretion.
In order to rule out possible renal artery stenosis, CT angiography of the renal artery was performed, demonstrating an accessory left superior renal artery (FigureA). Accessory renal arteries are frequent, with an average prevalence of 30% but can be as high as 61% in selected populations.4 Moreover, despite its low prevalence,5 accessory renal artery stenosis is a possible etiology for secondary hypertension.5, 6 Hence, the patient was referred for renal venous sampling (FigureB). However, the test results did not support the diagnosis, pointing to a contralateral localization of hyperreninemia. This led to the decision on expectant management.
Interestingly, following the diagnosis, the patient's BP values normalized, leading to cessation of any antihypertensive treatment. In line with these clinical findings, her levels of PRA decreased and PA normalized. Moreover, a repeat renal artery ultrasound did not demonstrate the accessory artery, possibly as a result of spontaneous collapse of this vessel. Since there was no clinical justification, no further imaging modality was used.
Conclusions
Stenosis of an accessory renal artery is a possible etiology for secondary hypertension among young children. Among such patients with well controlled BP and good compliance, expectant management is a valid treatment option, enabling possible spontaneous resolution.
Disclosures
The authors have nothing to disclose.
J Clin Hypertens (Greenwich). 2017;19:100–102. DOI: 10.1111/jch.12893. Published 2016. This article is a U.S. Government work and is in the public domain in the USA
IHA and AT contributed equally to this manuscript.
References
- 1. Kit BK, Kuklina E, Carroll MD, et al. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999–2012. JAMA Pediatr. 2015;169:272–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wyszyńska T, Cichocka E, Wieteska‐Klimczak A, et al. A single pediatric center experience with 1025 children with hypertension. Acta Paediatr. 1992;81:244–246. [DOI] [PubMed] [Google Scholar]
- 3. Mitsnefes MM. Hypertension in children and adolescents. Pediatr Clin North Am. 2006;53:493–512. [DOI] [PubMed] [Google Scholar]
- 4. Gulas E, Wysiadecki G, Cecot T, et al. Accessory (multiple) renal arteries ‐ Differences in frequency according to population, visualizing techniques and stage of morphological development. Vascular. 2016;24:531–537. [DOI] [PubMed] [Google Scholar]
- 5. Bude RO, Forauer AR, Caoili EM, Nghiem HV. Is it necessary to study accessory arteries when screening the renal arteries for renovascular hypertension? Radiology. 2003;226:411–416. [DOI] [PubMed] [Google Scholar]
- 6. Berland LL, Koslin DB, Routh WD, Keller FS. Renal artery stenosis: prospective evaluation of diagnosis with color duplex US compared with angiography. Work in progress. Radiology. 1990;174:421–423. [DOI] [PubMed] [Google Scholar]


