Abstract
This study employed secondary analyses of existing ecological momentary assessment (EMA) data to characterize hostile and irritable affect in the day-to-day experience of 52 smokers with, and 65 smokers without, posttraumatic stress disorder (PTSD). EMA monitoring occurred over a mean of 8.2 days, and participants responded to an average of 2.8 random prompts/day. Analyses included Wilcoxon rank sum tests of group differences, and path analyses of cross-lagged multilevel models. Participants with PTSD endorsed a significantly higher proportion of total EMA entries indicating hostile affect and irritable affect than did individuals without PTSD. Cross-lagged analyses indicated that over a period of hours, PTSD symptoms significantly predicted subsequent hostile and irritable affect, but hostile and irritable affect did not predict subsequent PTSD symptoms. Findings suggest that day-to-day exposure to PTSD-related trauma cues may contribute to chronically elevated levels of anger-related affect. Such heightened affective arousal may, in turn, underlie an increased risk for verbal or physical aggression, as well as other health and quality-of-life related impairments associated with PTSD. Clinical implications include conceptualizing anger treatment in the broader context of trauma history and symptoms, and specifically targeting physiological arousal and maladaptive hostile cognitions triggered by trauma reminders in patients with PTSD.
Keywords: Hostility, Irritability, Arousal dysregulation, Veterans
1. Introduction
In 1980, Posttraumatic Stress Disorder (PTSD) was introduced as an Anxiety Disorder in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) (American Psychiatric Association, 1980), an historic but controversial step that went a long way towards legitimizing the “Post-Vietnam Syndrome” that had been described by Vietnam combat veterans (Scott, 1990). Although pioneering researchers of PTSD observed that anger and fear were both common reactions to threat and were likely central to symptom manifestation and treatment (Beckham et al., 1996; Riggs et al., 1992), PTSD was primarily conceptualized as a fear- and anxiety-related phenomenon for over three decades. Fear-based models framed the majority of empirical research, and empirically-supported therapies for PTSD have been developed as expansions of established exposure-based treatments for anxiety disorders (Foa and Kozak, 1986; Foa et al., 1989). While these therapies have been shown to be largely effective (Chard et al., 2012; Rauch et al., 2012), anger has been found to be associated with increased drop-out and attenuated effectiveness (Foa et al., 1995; Lloyd et al., 2014; Miles et al., 2015a, 2015b). In some cases, significant functional impairment in the domain of anger remains even following successful treatment for PTSD (Forbes et al., 2005).
When the fifth edition of the DSM was published in 2013 (American Psychiatric Association, 2013), PTSD was moved from the Anxiety Disorders section into the newly-created Trauma- and Stressor-Related Disorders section. This re-classification was accompanied by an expansion of the definition of the “persistent negative emotional state” that could be associated with PTSD, such that “horror, anger, guilt, or shame” were identified as potential elements of posttraumatic affective disturbance (American Psychiatric Association, 2013). Anger, particularly the outward expression of anger through “verbal or physical aggression toward people or objects” (American Psychiatric Association, 2013), was defined in more detail within the hyperarousal cluster. Since then research has continued to demonstrate that posttraumatic stress is, indeed, associated with affective disturbances other than fear (Power and Fyvie, 2013; Tye et al., 2015). A meta-analysis found that PTSD is associated with anger particularly in military samples (Orth and Wieland, 2006), and anger is a frequently cited problem in military personnel returning from combat deployments (Gonzalez et al., 2016; Heesink et al., 2015; Sayer et al., 2010; Wilk et al., 2015). Dealing with anger is cited as one of the primary concerns among help-seeking veterans with PTSD (Crawford et al., 2015).
Studies suggest that PTSD-related anger may not resolve over time without treatment. There is growing evidence that anger increases over time after a traumatic event in individuals with PTSD (Orth and Wieland, 2006), and several studies have found that anger in individuals with PTSD is associated with severity and chronicity of symptoms over time (Andrews et al., 2000; Feeny et al., 2000; Koenen et al., 2003; Kulkarni et al., 2012; Novaco and Chemtob, 2002; Orth et al., 2008). Two longitudinal studies have examined the relationship between anger and PTSD symptoms. In the first study, women were assessed within approximately 10 days of an assault, and then three more times over the course of one month. Findings indicated that while PTSD symptoms at baseline predicted subsequent anger levels, baseline anger levels did not predict PTSD symptoms (Orth et al., 2008). A second study evaluated police recruits (87.2% male) during training and again one year later. Over this longer span of time PTSD symptoms again predicted anger at one year, but baseline anger also predicted PTSD symptoms over the next year (Meffert et al., 2008).
The current investigation used ecological momentary assessment (EMA) to examine the association between PTSD symptoms and hostile and irritable affect in the daily experiences of both veteran and non-veteran participants with and without PTSD over approximately one week. To our knowledge, no study has used EMA to examine the directional nature of the association of PTSD symptoms and anger in day-to-day functioning.
Using EMA allows for a proximal examination of “real-world” changes in affect that are likely to be more dynamic that static, providing a finer-grained understanding of these relationships than is accessible through more conventional methods of self-report. Understanding how PTSD and anger are linked at this level of analysis is likely to be particularly relevant to clinicians, because individuals’ responses to everyday trauma and anger triggers are most likely to directly impact their overall functioning and quality of life. We hypothesized that individuals with PTSD would report higher frequency and intensity of hostile and irritable affect throughout the week compared to individuals without PTSD. Building upon prior research that suggests that PTSD symptoms predict subsequent anger over weeks or months (Meffert et al., 2008; Orth et al., 2008), we also hypothesized that increases or decreases in PTSD symptoms would predict hostile and irritable affect at a subsequent reading taken a few hours later. Given inconsistent findings in previous studies regarding the association of changes in anger predicting later PTSD symptoms (Meffert et al., 2008; Orth et al., 2008), analyses regarding the association of changes in hostile and irritable affect and subsequent PTSD symptoms were exploratory and no specific a priori hypothesis was specified.
2. Methods
2.1. Participants
Participants (N=114) were drawn from a sample collected for a broader smoking-cessation trial in individuals with and without PTSD (Beckham et al., 2013). Eligible participants were between 18 and 65 years of age, generally healthy, not currently seeking treatment for nicotine dependence, and currently smoking at least 10 cigarettes per day. Participants were excluded for major unstable medical problems, using non-cigarette forms of nicotine, pregnancy, non-English speaking, current substance abuse/dependence, schizophrenia, current manic syndrome, lifetime but not current PTSD, and current bupropion or benzodiazepine use. This study was approved by the Duke University School of Medicine Institutional Review Board (IRB) and the Durham VA IRB and Research and Development Committees. See Table 1 for participant demographic and clinical characteristics.
Table 1.
Description of sample.
| Total Sample (n=117) |
PTSD (n = 52) |
No PTSD (n = 65) |
|
|---|---|---|---|
| Age | 42.4 (9.8) | 42.4 (10.1) | 42.5 (9.6) |
| Education | 12.8 (2.5) | 12.6 (1.8) | 12.9 (3.0) |
| Hollingsworth | 54.3 (13.6) | 56.9 (11.5) | 52.2 (14.9) |
| Gender | |||
| Male | 52% (61) | 42% (22) | 60% (39) |
| Female | 48% (56) | 58% (30) | 40% (26) |
| Race/Ethnicity | |||
| White/Caucasian | 34% (40) | 40% (21) | 29% (19) |
| Black/African-American | 62% (72) | 52% (27) | 69% (45) |
| Bi-racial/Multiracial/Other | 4% (5) | 8% (4) | 2% (1) |
| Mean total responses to random prompts | 22.47 (10.75) | 23.69 (11.33) | 21.52 (9.81) |
| Mean per day responses to random prompts | 2.84 (1.19) | 2.65 (1.01) | 3.03 (1.30) |
| CAPS Total score*** | 34.3 (31.3) | 63.7 (20.5) | 9.6 (11.4) |
| DTS Total Score*** | 5.5 (10.3) | 10.7 (13.2) | 1.1 (3.0) |
| PTSD | 44% (52) | – | – |
| Veteran Status | |||
| Veteran | 25% (29) | 25% (13) | 25% (16) |
| Non-veteran | 75% (88) | 75% (39) | 75% (49) |
| Current MDD*** | |||
| Present | 15% (18) | 31% (16) | 3% (2) |
| Absent | 85% (99) | 69% (36) | 97% (63) |
| Lifetime MDD*** | |||
| Present | 44% (51) | 69% (36) | 23% (15) |
| Absent | 56% (66) | 31% (16) | 77% (50) |
Note: significant difference observed between PTSD and no-PTSD groups:
p < 0.05,
p < 0.01,
p<0.001. For means, standard deviation is in parentheses; for percentages, n is in parentheses. Percentages reflect ratio of row characteristic within the columns (e.g., for Gender: 52% of the Total Sample was men, and 48% of the Total Sample was women).
2.2. Procedures
Participants completed a screening and baseline session prior to the initiation of EMA data collection. Psychiatric disorders were assessed using the Structured Clinical Interview for the DSM-IV Axis I disorders (SCID) (First et al., 1996) and the Clinician Administered PTSD Scale for the DSM-IV (CAPS) (Blake et al., 1995). Current diagnosis was determined by a 1-month timeframe for PTSD, major depressive disorder, and anxiety disorders, and a 3-month time frame for current substance abuse or dependence. CAPS and SCID interviews were conducted by Bachelor's, Master's, or Ph.D. level raters who were supervised by Master's or Ph.D. level clinicians with years of experience working with patients with PTSD. Each rater was trained using SCID and CAPS standardized training (i.e. manual, videotapes, and co-ratings with a trained rater). Interrater reliability, as determined by Fleiss’ kappa for diagnoses based on videotapes of patient interviews, was excellent (κ = 0.96).
For multilevel path analyses examining the association of changes in PTSD symptoms and in hostile and irritable affect over the course of the day (described in detail in the Analysis section below), we limited analyses to those participants who met criterion A1 for PTSD. This eliminated 3 participants without PTSD from the multilevel path analyses. As such, all of the 114 participants included in these analyses reported having “experienced, witnessed, or [been] confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others” (American Psychiatric Association, 1994), regardless of their response at the time of the trauma (criterion A2), or their subsequent experience of PTSD symptomatology (criteria sets B-F).
Participants carried Palm Pilot devices provided to them by the study team for EMA data collection. EMA data consisted of responses to random prompts over a week-long baseline observation period during which smokers smoked ad lib. While participants also self-initiated diary entries prior to smoking episodes, these entries were not included in these analyses. Diary entries were time-stamped to ensure temporal accuracy (i.e., participants could not delay or clump entries) and to assess protocol adherence. Investigator-initiated alarms were designed to go off randomly between 1 and 3 h after a completed assessment. Following missed or skipped alarms, the next alarm was designed to go off 30–45 min later. Participants had a 2-min window after the alarm to begin the assessment. They were instructed to ignore any signal that occurred during an incompatible activity (i.e., driving) and were allowed to suspend prompting when responding would be too costly (i.e., religious services, driving). Additionally, participants were able to delay an assessment with a 5-min delay function. Finally, participants were able to inactivate alarms for 15–120 min when they expected to be unavailable and for 4–11 h overnight for sleeping (Beckham et al., 2013, 2005).
At each prompt, participants were asked to respond to questions describing their smoking urge, setting, activity, PTSD symptoms, and mood”right now”. Presence and severity of DSM-IV PTSD symptoms were measured using items from the Davidson Trauma Scale (DTS) (Davidson et al., 1997). If a given symptom was determined as present, participants then indicated its severity using a 5-point scale (0=“not at all distressing” to 4=“extremely distressing”). Seven of 12 PTSD symptoms from the DTS were assessed: PTSD cluster B re-experiencing symptoms (intrusive thoughts, event recurring, upsetting reminders, and physically upset by reminders); PTSD cluster C avoidance and numbing symptoms (avoiding thoughts and feelings, difficulty enjoying things, feeling distant, and numbing of feelings); and PTSD cluster D hyperarousal symptoms (irritation, difficulty concentrating, on edge, and easily startled). Certain PTSD symptoms that would not be expected to change across the course of one day were omitted from the diary: recurrent distressing dreams (B2), inability to recall an important aspect of the trauma (C3), sense of a foreshortened future (C7), and difficulty falling or staying asleep (D1). The anger/irritability item (D2) was included in the diary prompts but omitted from measures of PTSD for this investigation. Severity scores for the 11 items that were included were summed to create a total severity score (Beckham et al., 2013).
“Irritable” and “hostile” affect were measured using these two items of the Positive and Negative Affect Schedule (PANAS) (Watson et al., 1988). Participants were asked to rate the extent to which they felt each emotion “right now” via a Likert scale using the following anchors: 1=“Very slightly/Not at all”; 2=“A little”; 3=“Moderately”; 4=“Quite a bit”; 5=“Extremely”. At each reading hostile affect and irritable affect were separately scored as present if the participant endorsed the item at 2 or greater; otherwise each was scored as absent.
2.3. Analysis
To compare participants with and without PTSD on the frequency with which they experienced hostility or irritability, we calculated the number of endorsements (present/absent) of PANAS “hostile” and PANAS “irritable” for each person, divided by the total number of diary responses over the week for that person. This resulted in a “mean” score between 0 and 1, reflecting the proportion of responses to random prompts to which each participant reported feeling “hostile” or “irritable” at any level of severity. Because the affect data demonstrated significant skew, nonparametric Wilcoxon rank sum tests were used for these analyses.
To explore the direction of the association between hostile and irritable affect and PTSD symptoms over time, we tested multilevel cross-lagged path models examining whether PTSD symptoms as indexed by Davidson Trauma Scale (DTS) scores predicted changes in hostile/irritable affect at the following time point, controlling for the effects of previous hostile/irritable affect; and also whether hostile/irritable affect predicted changes in DTS scores at the following time point, controlling for the effects of previous DTS scores. Multilevel modeling was appropriate because our data was characterized by two levels of observations: those made at the level of each diary reading (Level 1) and those made at the level of each participant (Level 2). The advantage of path analysis over univariate approaches, such as multiple regression, is that multiple dependent variables can be examined simultaneously. Moreover, using fit indices, one can examine all viable paths in the model and then determine whether elimination of one or more of those paths significantly reduces model fit. For instance, in the present study, we could examine not only the autoregressive effects of hostility/irritability (Path a, Fig. 1) and PTSD symptom severity (Path b), but also whether previous hostility/irritability predicted subsequent PTSD symptom severity (Path c) and whether previous PTSD symptom severity predicted subsequent hostility and irritability (Path d).
Fig. 1.
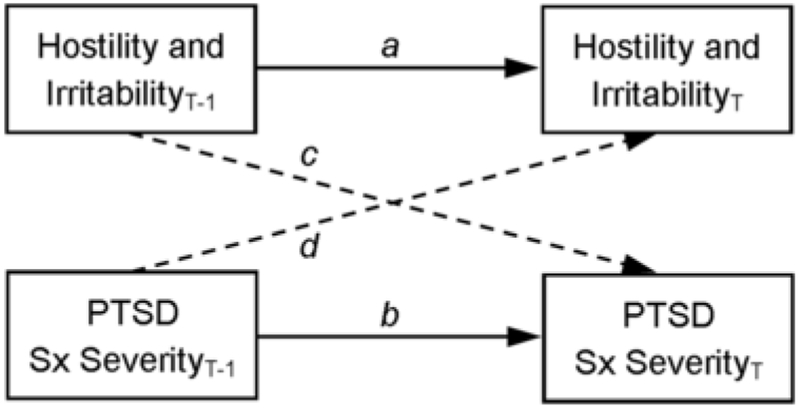
Cross-lagged path analysis of hostility/irritability and PTSD symptom severity.
Prior to conducting the cross-lagged analyses, we first examined the distribution of PTSD symptom severity and hostility/irritability scores. Both were characterized by overdispersion (PTSD symptom severity M = 4.98, SD = 11.51; hostility/irritability M = 0.62, SD = 1.26) and a large number of zeros (67.1% for PTSD symptom severity, 72.2% for hostility/irritability). To determine whether to model the data as negative binomial or zero-inflated negative binomial, we examined the fit of the corresponding null models (i.e., models absent predictors). Due to the non-normal data, the Satorra-Bentler chi-square test of difference was used to compare the models (Curran et al., 1996). According to this test, the zero-inflated negative binomial model was superior to the negative binomial model, Satorra-Bentler X2(4)=182.92, p<0.001. We then created lagged hostility/irritability and PTSD symptom severity values using observations from the previous reading. Because the effect of lagged variables likely diminished over time, we omitted lagged values that occurred more than 5 h prior to the subsequent reading.
In the initial path analysis we modeled PTSD symptom severity and hostility/irritability scores as a function of their lagged values, covarying for age, sex, and minority status. We then examined three additional models in which the cross-lagged paths (Paths c and d in Fig. 1) were removed, first individually and then simultaneously. The negative binomial portion of the model was used to model lagged effects. Only intercepts were modeled in the zero-inflated (logistic) portion of the model after efforts to model lag effects failed to yield converged models. The Satorra-Bentler chi-square test was used to compare nested models. Bayesian information criteria (BIC; Schwartz, 1978) were consulted to aid in comparison of non-nested models. In using BIC values to compare models, a 10-point difference can be interpreted as “very strong” evidence (i.e., p<0.05) of the superiority of the model with the smaller BIC (Kass and Raftery, 1995; Raftery, 1995). A difference of 6–9 points may be interpreted as “strong” support for a meaningful difference between the models.
After identifying the best-fitting model, we then examined whether the lagged effects were equivalent across PTSD diagnosis. In particular, we analyzed whether lagged effects of PTSD symptom severity and hostility/irritability on subsequent symptoms and mood were equal across groups with and without PTSD. Cross-lagged analyses were performed using robust maximum likelihood method via Mplus 7.
3. Results
Participants (N=117) with (n=52) and without (n=65) PTSD were monitored for a mean of 8.2 (3.4) days. Average age of participants was 42 years. Fifty-two percent of the sample was male and 25% were military veterans. Sixty-two percent of the sample identified as Black or African-American, 34% as White or Caucasian, and 4% as Native American or as more than one race. No significant differences were observed between the groups with and without PTSD for age, gender, race, or veteran status. A total of 2659 responses to random prompts were recorded. No differences between groups were observed in overall responding to the random prompts (t=1.72, n.s.). See Table 1.
Across groups, participants endorsed “Very little/Not at all” to most diary prompts for both hostile (87.6%) and irritable (73.6%) affect. Participants with PTSD endorsed a significantly higher proportion of total prompts over the week as present for hostile affect (Z=3.20, p<0.002) and for irritable affect (Z=3.94, p<0.0001) than did individuals without PTSD. See Table 2. Across all participants and EMA readings, hostile and irritable affect were positively correlated with one another, r(2694) = 0.57, p <0.001, and with PTSD symptom severity, r(2694) = 0.27, p < 0.001 and r(2694) = .41, p < 0.001, respectively. Composite hostile and irritable affect scores were also positively correlated with PTSD symptom severity scores, r(2694) = 0.40, p <0.001.
Table 2.
Proportion of total diary entries endorsing presence of anger-related affect (PANAS).
| Total Sample (n=117) |
PTSD (n=52) |
No PTSD (n=65) |
|
|---|---|---|---|
| Hostile Affect** | |||
| Mean (SD) | .14 (.25) | .19 (.26) | .10 (.23) |
| Median (var) | .00 (.06) | .09 (.07) | .00 (.05) |
| Irritable Affect*** | |||
| Mean (SD) | .28 (.31) | .38 (.31) | .20 (.28) |
| Median (var) | .18 (.09) | .28 (.10) | .07 (.08) |
Note: significant difference observed between PTSD and no-PTSD groups:
p < .05,
p < .01,
p<.001.
Path analyses examined the lagged associations between PTSD symptoms and hostile and irritable affect (see Fig. 1). Results examining the initial Level-1 effects from the cross-lagged model, indicated that the effect of hostility and irritability at time T-1 was not associated with PTSD symptom severity at time T; however, PTSD symptom severity at T-1 was significantly related to levels of hostility and irritability at time T (See Fig. 2). Dropping the path from PTSD symptom severity at time T-1 to hostility and irritability at time T (Path d) did not significantly diminish model fit, Satorra-Bentler X2(1)=0.00, p>0.99, nor did dropping the path from hostility and irritability at time T-1 to PTSD symptom severity at time T (Path c), Satorra-Bentler X2(1)=0.00, p>0.99. However, dropping both paths significantly reduced model fit, Satorra-Bentler X2(2) = 13.82, p<0.01. Examination of BICs provided very strong evidence that the model dropping Path c (BIC = 20,170.48) was superior to the model dropping Path d (BIC = 20,184.73), with a difference of 14.25 points. As depicted in Fig. 3, prior PTSD symptom severity was a significant predictor of subsequent hostility and irritability.
Fig. 2.
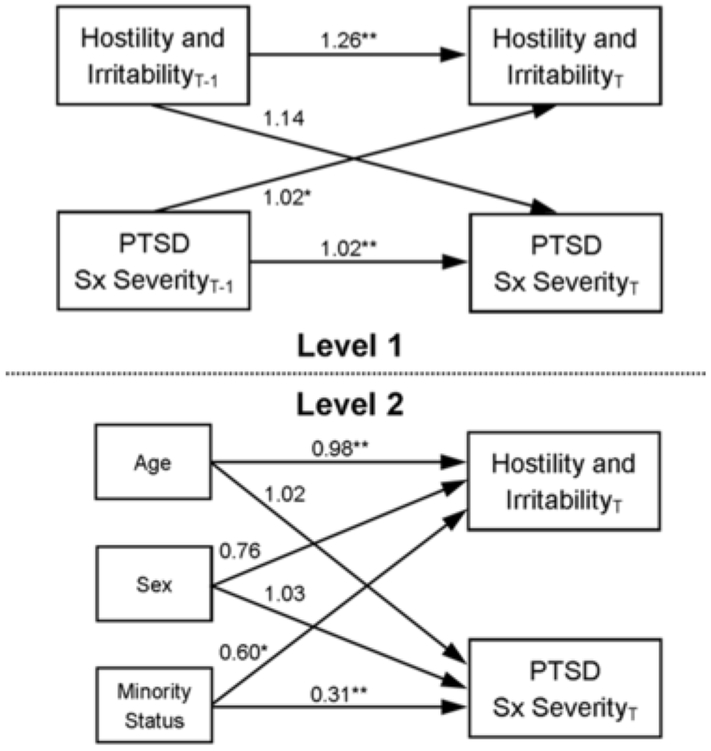
Multilevel path analysis featuring all cross-lagged effects. Coefficients represent multiplicative effects of predictor variables on outcome variables. Level 1 refers to within-person EMA reading-level relationships. Level 2 refers to between-person relationships.*p < 0.05, **p < 0.01.
Fig. 3.
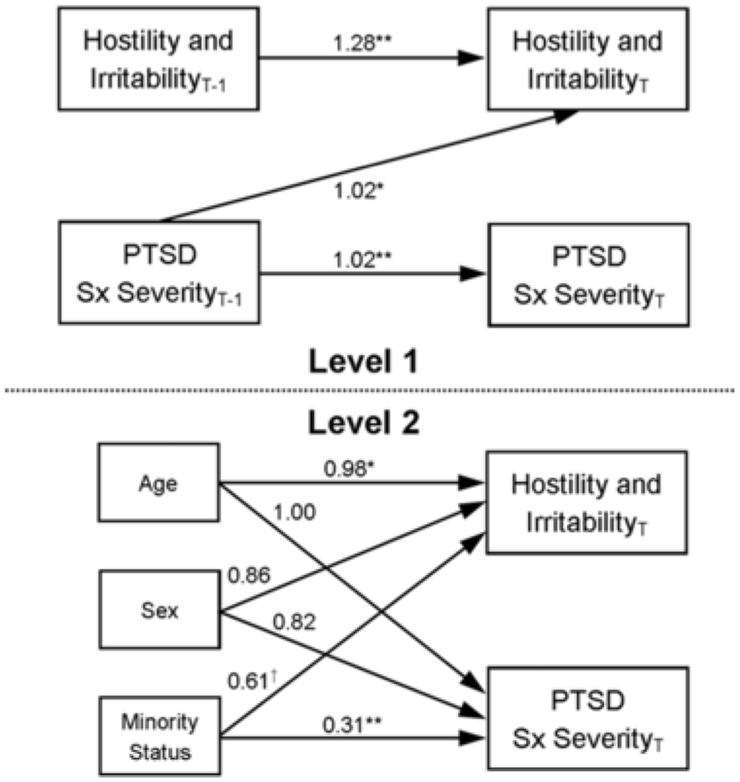
Best-fitting multilevel cross-lagged model. Coefficients represent multiplicative effects of predictor variables on outcome variables. Level 1 refers to within-person EMA reading-level relationships. Level 2 refers to between-person relationships. *p < .05, **p < .01.
Next, we examined whether the lagged effects of PTSD symptom severity and hostility/irritability (Path a, b, and d, Fig. 1) were similar across participants with and without a DSM-IV diagnosis of PTSD. According to Wald chi-square tests, the autoregressive effect of hostility/irritability was not significantly distinct between the no-PTSD (B = 0.32, p = 0.01) and PTSD diagnostic groups (B = 0.36, p <0.01), Wald X2(1) = 0.08, p = 0.78. Although the autoregressive effect of PTSD symptom severity was significant across individuals with (B = 0.02, p < 0.01) and without (B = 0.09, p < 0.01) a PTSD diagnosis, the effect was distinct between the two groups, Wald X2(1) = 4.90, p = 0.03, likely reflecting differences in base rates and means of PTSD symptom severity. Finally, the cross-lagged effect of PTSD symptom severity on subsequent hostility/irritability (Path d) was not significantly different in the no-PTSD (B = 0.05, p = 0.03) and PTSD (B = 0.01, p = 0.03) diagnostic groups, Wald X2(1) = 3.14, p = 0.08, suggesting that PTSD symptoms drive hostility and irritability similarly across both groups.
4. Discussion
This investigation used ecological momentary assessment (EMA) to characterize the relationship between posttraumatic stress disorder symptomatology and hostile and irritable affect over a week-long period of observation. Findings extend previous literature reporting that PTSD is associated with the development and maintenance of anger-related affect over weeks, months and years (Andrews et al., 2000; Feeny et al., 2000; Koenen et al., 2003; Kulkarni et al., 2012; Meffert et al., 2008; Novaco and Chemtob, 2002; Orth et al., 2008; Orth and Wieland, 2006), suggesting that a similar pattern of relationships exits between PTSD and hostile and irritable affect when these variables are measured over the course of hours and days. Compared to those without PTSD, individuals with PTSD reported higher frequency of both PANAS-rated hostile and irritable affect over the course of a week-long observation period. Multilevel path analysis of cross-lagged models suggested that over a period of hours PTSD symptoms predicted irritable and hostile affect, but hostile and irritable affect did not predict PTSD.
These data indicated that people with PTSD are more likely to feel irritable or hostile at any given time than those without PTSD, and that while PTSD symptoms, including PTSD-related triggers, cognitions, and affect, predicted subsequent angry affect such as hostility or irritability, the reverse is not necessarily true. Research has linked hostility in individuals with PTSD to physiological hyperarousal (Beckham et al., 2009, 2002; Vrana et al., 2009), and improved arousal regulation has been found to be the one of the primary mechanisms of change in anger management therapy for veterans with PTSD (Mackintosh et al., 2014a, 2014b). Considered in the context of these prior studies, our findings may suggest that directly targeting the PTSD-related physiological arousal (Beckham et al., 2009, 2002; Dennis et al., 2016, 2017; Mackintosh et al., 2014a, 2014b; Vrana et al., 2009) and hostile cognitions (Van Voorhees et al., 2016) that contribute to irritability and anger may be an important part of a holistic approach to minimizing the functional impact of the disorder. Current empirically support therapies specifically target the avoidance symptoms that are understood to maintain PTSD (Cahill et al., 2003; Foa et al., 2006; Resick et al., 2010), while less attention is given to directly targeting physiological arousal and hostile interpersonal attributions cued by trauma triggers. Supplementing trauma-focused treatment with training in physiological self-regulation or cognitive reappraisal skills that can be used in the moment when confronted with trauma triggers may help to mitigate some of impact of PTSD on day-to-day affect and functioning (Mackintosh et al., 2014a, 2014b).
It is interesting to note that like those without PTSD, the majority of the time individuals with PTSD did not report hostile or irritable affect. However, it may be that even relatively small increases in the proportion of time spent coping with anger-related affect could have a significant impact on interpersonal functioning, physical health, and overall sense of well-being. On an interpersonal level, heightened levels of negative affective arousal in response to day-to-day exposure to emotionally distressing trauma cues may underlie the increased risk for infrequent (but often socially and interpersonally devastating) verbal or physical aggression that has been observed in individuals with PTSD (Elbogen et al., 2012, 2014a, 2014b; Miles et al., 2015a, 2015b; Van Voorhees et al., 2016). People with PTSD who experience anger often report that they avoid interpersonal engagement as much as possible in an effort to prevent such undesirable outcomes (Frueh et al., 1997; Miles et al., 2015a, 2015b). This, in turn, is likely to result in further isolation from the type of social support resources that have been consistently demonstrated to improve functional outcomes in trauma survivors (Charuvastra and Cloitre, 2008; Elbogen et al., 2014a, 2014b; Han et al., 2014; Van Voorhees et al., 2012). Physically, PTSD has been linked to increased risk for cardiovascular disease, an association that could be partially mediated by physiological “wear-and-tear” related to more frequent anger-related sympathetic arousal (Suls, 2013).
In the path analyses examining the lagged associations between PTSD symptoms and hostile and irritable affect we included only the participants who had experienced a DSM-IV criterion A trauma, and our findings suggest that in this sample fluctuations in PTSD symptom severity predicted changes in hostile and irritable affect similarly in individuals with and without a diagnosis of PTSD. This finding that PTSD symptoms appear to contribute to hostility and irritability similarly in individuals with trauma histories, regardless of whether they meet formal criteria for a PTSD diagnosis, is consistent with literature that suggests that it can be difficult to delineate a firm diagnostic cut-point for clinically significant impairment (Cukor et al., 2010; Jakupcak et al., 2007; Zlotnick et al., 2002).
The larger study from which these data were drawn was designed as part of a smoking cessation trial, and thus all of the participants were current, dependent cigarette smokers. Analyses for this study were conducted on data from the baseline week during which participants were smoking as usual, and we do not have any reason to suspect that nicotine withdrawal symptoms impacted the outcomes reported here in any systematic way. However, while rates of cigarette smoking among individuals with PTSD have been observed to be between 34–86% depending upon the sample (Fu et al., 2007), care must be taken to generalizing the findings presented here to non-smoking populations.
For the cross-lagged analyses, the interval between readings was an important factor influencing the findings. Restricting the interval to examine lag effects meant losing data, while increasing the interval would potentially diminish the lag effects. Thus, our decision to limit analyses to readings within 5 h of each other was made in consideration of these trade-offs. It is possible that we would have found different results had we further restricted or relaxed this criterion.
Finally, while the results of this study are strengthened by the use of EMA techniques, all symptom measures were self-report. Insight and willingness to label affective experience may differ across individuals and between groups, introducing a potentially important confound to the findings.
Our findings suggest that treating problems with anger in individuals with PTSD may require an approach that takes into account the ways in which trauma-related cues may trigger angry feelings and contribute to a more generalized, day-to-day experience of hostility and irritability. Current approaches to “anger management” typically do not take into account the range of psychiatric problems that can underlie the behavioral manifestation of problematic anger (Del Vecchio and O'Leary, 2004; Mackintosh et al., 2014a, 2014b; Novaco and Chemtob, 2015). In treating anger and aggression in individuals with PTSD, it may be useful to examine anger in the broader context of trauma related triggers, keeping in mind that managing PTSD-related anger may be facilitated by targeting physiological reactivity and maladaptive cognitions triggered by trauma reminders. In a similar vein, it is important for clinicians treating PTSD to be aware of the role that anger-related affect and arousal may play in patients’ day-to-day functioning and quality of life, as well how it might affect their capacity to benefit from current empirically-supported therapies for PTSD (Lloyd et al., 2014; Rizvi et al., 2009). Finally, though the current sample included both veterans and non-veterans and we do not present any veteran-specific outcomes, both PTSD and trauma-related anger are issues that have been found to disproportionately affect veterans (Kessler et al., 1995; Novaco and Chemtob, 2002, 2015; Orth and Wieland, 2006). Given that a large number of veterans of the conflicts in Iraq and Afghanistan diagnosed with PTSD specifically indicate the need for help with anger management (Crawford et al., 2015), policy makers concerned with veterans affairs may want to consider focusing additional research and clinical resources into the development and implementation of therapies for PTSD-related anger. Some progress has been made in this area in recent years (Taft et al., 2016; Van Voorhees and Beckham, 2015), but a great deal of work needs to be done to address the current and growing need.
Acknowledgments
Disclaimer and funding sources
Preparation of this work was supported by a grant from the National Cancer Institute (2R01CA081595), a Career Development Award (1K2RX001298) from the Rehabilitation Research & Development Service of the Department of Veterans Affairs Office of Research & Development (VA ORD), and a Senior Research Career Scientist Award (11S-RCS-009) from the Clinical Science Research and Development Service of the VA ORD. This work was also supported by resources from the Durham VA Medical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health, the Department of Veterans Affairs, or the US Government.
Footnotes
Uncited reference
References
- Andrews B, Brewin CR, Rose S, Kirk M, 2000. Predicting PTSD symptoms in victims of violent crime: the role of shame, anger, and childhood abuse. J. Abnorm. Psychol 109 (1), 69–73. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 1980. The Diagnsotic and Statistical Manual of Mental Disorders, 3rd ed. American Psychiatric Association, Washington, DC. [Google Scholar]
- American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. American Psychiatric Association, Washington, DC. [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. American Psychiatric Association, Arlington, VA. [Google Scholar]
- Beckham JC, Calhoun PS, Dennis MF, Wilson SM, Dedert EA, 2013. Predictors of lapse in first week of smoking abstinence in PTSD and non-PTSD smokers. Nicotine Tob. Res 15 (6), 1122–1129. 10.1093/ntr/nts252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Vrana SR, Mozley SL, Erkanli A, Clancy CP, et al. , 2005. Immediate antecedents of cigarette smoking in smokers with and without post-traumatic stress disorder: a preliminary study. Exp. Clin. Psychopharmacol 13 (3), 219–228, (doi:2005-10634-008). [DOI] [PubMed] [Google Scholar]
- Beckham JC, Flood AM, Dennis MF, Calhoun PS, 2009. Ambulatory cardiovascular activity and hostility ratings in women with chronic posttraumatic stress disorder. Biol. Psychiatry 65 (3), 268–272, (doi:S0006-3223)(08)(00796-8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Roodman AA, Barefoot JC, Haney TL, Helms MJ, Fairbank JA, et al. , 1996. Interpersonal and self-reported hostility among combat veterans with and without posttraumatic stress disorder. J. Trauma. Stress 9 (2), 335–342. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Vrana SR, Barefoot JC, Feldman ME, Fairbank J, Moore SD, 2002. Magnitude and duration of cardiovascular responses to anger in Vietnam veterans with and without posttraumatic stress disorder. J. Consult. Clin. Psychol 70 (1), 228–234. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Chamey DS, et al. , 1995. The development of a clinician-administered PTSD scale. J. Trauma. Stress 8 (1), 75–90. [DOI] [PubMed] [Google Scholar]
- Chard KM, Ricksecker EG, Healy ET, Karlin BE, Resick PA, 2012. Dissemination and experience with cognitive processing therapy. J. Rehabil. Res. Dev 49 (5), 667–678. [DOI] [PubMed] [Google Scholar]
- Charuvastra A, Cloitre M, 2008. Social bonds and posttraumatic stress disorder. Annu. Rev. Psychol 59, 301–328. 10.1146/annurev.psych.58.110405.085650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford EF, Elbogen EB, Wagner HR, Kudler H, Calhoun PS, Brancu M, et al. , 2015. Surveying treatment preferences in U.S. Iraq-Afghanistan veterans with PTSD symptoms: a step toward veteran-centered care. J. Trauma. Stress 28 (2), 118–126. 10.1002/jts.21993. [DOI] [PubMed] [Google Scholar]
- Cukor J, Wyka K, Jayasinghe N, Difede J, 2010. The nature and course of subthreshold PTSD. J. Anxiety Disord 24 (8), 918–923. 10.1016/j.janxdis.2010.06.017. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, et al. , 1997. Assessment of a New Self-rating Scale for Post-traumatic Stress Disorder. Psychol. Med 27, 153–160. [DOI] [PubMed] [Google Scholar]
- Del Vecchio T, O'Leary KD, 2004. Effectiveness of anger treatments for specific anger problems: a meta-analytic review. Clin. Psychol. Rev 24 (1), 15–34. 10.1016/j.cpr.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Dennis PA, Dedert EA, Van Voorhees EE, Watkins LL, Hayano J, Calhoun PS, et al. , 2016. Examining the crux of autonomic sysfunction in posttraumatic stress disorder: whether chronic or situational distress underlies elevated heart rate and attenuated heart rate variability. Psychosom. Med 10.1097/psy.0000000000000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis PA, Kimbrel NA, Sherwood A, Calhoun PS, Watkins LL, Dennis MF, et al. , 2017. Trauma and autonomic dysregulation: episodic-versus systemic-negative affect underlying cardiovascular risk in posttraumatic stress disorder. Psychosom. Med 79 (5), 496–505. 10.1097/psy.0000000000000438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen EB, Johnson SC, Newton VM, Straits-Troster K, Vasterling JJ, Wagner HR, et al. , 2012. Criminal justice involvement, trauma, and negative affect in Iraq and Afghanistan war era veterans. J. Consult. Clin. Psychol 80 (6), 1097–1102. 10.1037/a0029967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen EB, Johnson SC, Newton VM, Timko C, Vasterling JJ, Van Male LM, et al. , 2014. Protective mechanisms and prevention of violence and aggression in veterans. Psychol. Serv 11 (2), 220–228. 10.1037/a0035088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen EB, Johnson SC, Wagner HR, Sullivan C, Taft CT, Beckham JC, 2014. Violent behaviour and post-traumatic stress disorder in US Iraq and Afghanistan veterans. Br. J. Psychiatry 204, 368–375. 10.1192/bjp.bp.113.134627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny NC, Zoellner LA, Foa EB, 2000. Anger, dissociation, and posttraumatic stress disorder among female assault victims. J. Truama Stress 13 (1), 89–100. 10.1023/A:1007725015225. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, 1996. User's Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders – Research Version. Biometrics Research Department, New York. [Google Scholar]
- Foa EB, Huppert JD, Cahill LP, 2006. Emotional processing theory: an update In: Rothbaum BO (Ed.), Pathological Anxiety: Emotional Processing in Etiology and Treatment. Guilford Press, New York, NY, pp. 3–22. [Google Scholar]
- Foa EB, Kozak MJ, 1986. Emotional processing of fear: exposure to corrective information. Psychol. Bull 99 (1), 20–35. [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Massie ED, Yarczower M, 1995. The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behav. Ther 26, 487–499. [Google Scholar]
- Foa EB, Steketee GS, Rothbaum B, 1989. Behavioral/cognitive conceptualizations of posttraumatic stress disorder. Behav. Ther 20, 155–176. [Google Scholar]
- Forbes D, Bennett N, Biddle D, Crompton D, McHugh T, Elliott P, et al. , 2005. Clinical presentations and treatment outcomes of peacekeeper veterans with PTSD: preliminary findings. Am. J. Psychiatry 162 (11), 2188–2190. 10.1176/appi.ajp.162.11.2188. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Henning KR, Pellegrin KL, Chobot K, 1997. Relationship between scores on anger measures and PTSD symptomatology, employment, and compensation-seeking status in combat veterans. J. Clin. Psychol 53 (8), 871–878. 10.1002/(SICI)1097-4679(199712). [DOI] [PubMed] [Google Scholar]
- Fu SS, McFall M, Saxon AJ, Beckham JC, Carmody TP, Baker DG, et al. , 2007. Post-traumatic stress disorder and smoking: a systematic review. Nicotine Tob. Res 9 (11), 1071–1084, (doi:783717367). [DOI] [PubMed] [Google Scholar]
- Gonzalez OI, Novaco RW, Reger MA, Gahm GA, 2016. Anger intensification with combat-related PTSD and depression comorbidity. Psychol. Trauma 8 (1), 9–16. 10.1037/tra0000042. [DOI] [PubMed] [Google Scholar]
- Han SC, Castro F, Lee LO, Chamey ME, Mant BP, Brailey K, et al. , 2014. Military unit support, postdeployment social support, and PTSD symptoms among active duty and National Guard soldiers deployed to Iraq. J. Anxiety Disord 28 (5), 446–453. 10.1016/j.janxdis.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Heesink L, Rademaker A, Vermetten E, Geuze E, Kleber R, 2015. Longitudinal measures of hostility in deployed military personnel. Psychiatry Res. 10.1016/j.psychres.2015.05.082. [DOI] [PubMed] [Google Scholar]
- Hembree EA, Rauch SA, Foa EB, 2003. Beyond the manual: the insider's guide to prolonged exposure for PTSD. Cogn. Behav. Pract 10, 22–30. [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, et al. , 2007. Anger, hostility, and aggression among Iraq and Afghanistan War veterans reporting PTSD and subthreshold PTSD. J. Trauma. Stress 20 (6), 945–954. 10.1002/jts.20258. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, 1995. Posttraumatic stress disorder in the national comorbidity survey. Arch. Gen. Psychiatry 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, Sommer JF Jr., 2003. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American Legionnaires. J. Cons. Clin. Psychol 71 (6), 980–986. 10.1037/0022-006X.71.6.980. [DOI] [PubMed] [Google Scholar]
- Kulkarni M, Porter KE, Rauch SA, 2012. Anger, dissociation, and PTSD among male veterans entering into PTSD treatment. J. Anxiety Disord 26 (2), 271–278, (doi:S0887-6185)(11)(00192-7). [DOI] [PubMed] [Google Scholar]
- Lloyd D, Nixon RD, Varker T, Elliott P, Perry D, Bryant RA, et al. , 2014. Comorbidity in the prediction of cognitive processing therapy treatment outcomes for combat-related posttraumatic stress disorder. J. Anxiety Disord 28 (2), 237–240 10.1016/j.janxdis.2013.12.002. [DOI] [PubMed] [Google Scholar]
- Mackintosh MA, Morland LA, Frueh BC, Greene CJ, Rosen CS, 2014. Peeking into the black box: mechanisms of action for anger management treatment. J. Anxiety Disord 28 (7), 687–695. 10.1016/j.janxdis.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Mackintosh MA, Morland LA, Kloezeman K, Greene CJ, Rosen CS, Elhai JD, et al. , 2014. Predictors of anger treatment outcomes. J. Clin. Psychol 70 (10), 905–913. 10.1002/jclp.22095. [DOI] [PubMed] [Google Scholar]
- Meffert SM, Metzler TJ, Henn-Haase C, McCaslin S, Inslicht S, Chemtob C, et al. , 2008. A prospective study of trait anger and PTSD symptoms in police. J. Trauma. Stress 21 (4), 410–416. 10.1002/jts.20350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles SR, Menefee DS, Wanner J, Teten Tharp A, Kent TA, 2015. The relationship between emotion dysregulation and impulsive aggression in veterans with post-traumatic stress disorder symptoms. J. Interpers. 10.1177/0886260515570746. [DOI] [PubMed] [Google Scholar]
- Miles SR, Smith TL, Maieritsch KP, Ahearn EP, 2015. Fear of losing emotional control is associated with cognitive processing therapy outcomes in U.S. veterans of Afghanistan and Iraq. J. Trauma. Stress 28 (5), 475–479. 10.1002/jts.22036. [DOI] [PubMed] [Google Scholar]
- Novaco RW, Chemtob CM, 2002. Anger and combat-related posttraumatic stress disorder. J. Trauma. Stress 15 (2), 123–132. 10.1023/A:1014855924072. [DOI] [PubMed] [Google Scholar]
- Novaco RW, Chemtob CM, 2015. Violence associated with combat-related posttraumatic stress disorder: the importance of anger. Psychol Trauma. 10.1037/tra0000067. [DOI] [PubMed] [Google Scholar]
- Orth U, Cahill SP, Foa EB, Maercker A, 2008. Anger and posttraumatic stress disorder symptoms in crime victims: a longitudinal analysis. J. Consult. Clin. Psychol 76 (2), 208–218, (doi:2008-03290-004). [DOI] [PubMed] [Google Scholar]
- Orth U, Wieland E, 2006. Anger, hostility, and posttraumatic stress disorder in trauma-exposed adults: a meta-analysis. J. Consult. Clin. Psychol 74 (4), 698–706, (doi:2006-09621-007). [DOI] [PubMed] [Google Scholar]
- Power MJ, Fyvie C, 2013. The role of emotion in PTSD: two preliminary studies. Behav. Cogn. Psychother 41 (2), 162–172. 10.1017/S1352465812000148. [DOI] [PubMed] [Google Scholar]
- Rauch SA, Eftekhari A, Ruzek JI, 2012. Review of exposure therapy: a gold standard for PTSD treatment. J. Rehabil. Res. Dev 49 (5), 679–688. [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Chard KM, 2010. Cognitive Processing Therapy: Veteran/military Version: Therapist's Manual. Department of Veterans Affairs, Washington, DC. [Google Scholar]
- Riggs DS, Dancu CV, Gershuny BS, Greenburg D, Foa EB, 1992. Anger and post-traumatic stress disorder in female crime victims. J. Trauma. Stress 5 (4), 613–625. [Google Scholar]
- Rizvi SL, Vogt DS, Resick PA, 2009. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behav. Res. Ther 47 (9), 737–743. 10.1016/j.brat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M, 2010. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatr. Serv 61 (6), 589–597, (doi:61/6/589). [DOI] [PubMed] [Google Scholar]
- Scott WJ, 1990. PTSD in DSM-III: a case in the politics of diagnosis and disease. Soc. Probl 37 (3), 294–310. 10.2307/800744. [DOI] [Google Scholar]
- Suls J, 2013. Anger and the heart: perspectives on cardiac risk, mechanisms and interventions. Prog. Cardiovasc. Dis 55 (6), 538–547. 10.1016/j.pcad. [DOI] [PubMed] [Google Scholar]
- Taft CT, Creech SK, Gallagher MW, Macdonald A, Murphy CM, Monson CM, 2016. Strength at home couples program to prevent military partner violence: a randomized controlled trial. J. Consult. Clin. Psychol 10.1037/ccp0000129. [DOI] [PubMed] [Google Scholar]
- Tye S, Van Voorhees E, Hu C, Lineberry T, 2015. Preclinical perspectives on posttraumatic stress disorder criteria in DSM-5. Harv. Rev. Psychiatry 23 (1), 51–58. 10.1097/HRP.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees EE, Beckham JC, 2015. Advancements in treating intimate partner violence in veterans. J. Clin. Psychiatry 76 (6), e826–e827. 10.4088/JCP.14com09556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees EE, Dedert EA, Calhoun PS, Brancu M, Runnals J, Beckham JC, 2012. Childhood trauma exposure in Iraq and Afghanistan war era veterans: implications for posttraumatic stress disorder symptoms and adult functional social support. Child Abus. Negl 36 (5), 423–432. 10.1016/j.chiabu.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Van Voorhees EE, Dennis PA, Neal LC, Hicks TA, Calhoun PS, Beckham JC, et al. , 2016. Posttraumatic stress disorder, hostile cognitions, and aggression in Iraq/Afghanistan era veterans. Psychiatry 79 (1), 70–84. 10.1080/00332747.2015.1123593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrana SR, Hughes JW, Dennis MF, Calhoun PS, Beckham JC, 2009. Effects of posttraumatic stress disorder status and covert hostility on cardiovascular responses to relived anger in women with and without PTSD. Biol. Psychol 82 (3), 274–280, (doi:S0301-0511)(09)(00164-1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A, 1988. Development and validation of brief measures of positive and negative affect: the PANAS scales. J. Pers. Soc. Psychol 54 (6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wilk JE, Quartana PJ, Clarke-Walper K, Kok BC, Riviere LA, 2015. Aggression in US soldiers post-deployment: associations with combat exposure and PTSD and the moderating role of trait anger. Aggress. Behav 41 (6), 556–565. 10.1002/ab.21595. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Franklin CL, Zimmerman M, 2002. Does "subthreshold" posttraumatic stress disorder have any clinical relevance?. Compr. Psychiatry 43 (6), 413–419. 10.1053/comp. [DOI] [PubMed] [Google Scholar]


