Abstract
Background
Hypertension self-care practice is essential for blood pressure control and reduction of hypertension complications. Nevertheless, we know little concerning hypertension self-care practice in Ethiopia. The purpose of this study was to assess hypertension self-care practice and associated factors among patients in public health facilities in Dessie town, Ethiopia.
Methods
In this cross-sectional study, 309 hypertensive patients (mean age 58.8 years, 53.4% women) completed the interviewer-administered questionnaire in Amharic language. Descriptive and logistic regression analyses were conducted using SPSS version 22.
Result
The mean score for hypertension self-care was 37.7 ± 8.2 and 51% scored below the mean. Divorced participants (AOR = 0.115, 95% CI = 0.026, 0.508, p-value < 0.01) and those who lack source of information (AOR = 0.084, 95% CI = 0.022, 0.322, p-value < 0.01) were less likely to have good self-care practice. But, participants who had convenient place for exercise (AOR = 2.968, 95% CI = 1.826, 4.825, p-value < 0.01), who had good social support (AOR = 2.204, 95% CI = 1.272, 3.821, p-value < 0.01), who had traditional clergy-based teaching (AOR = 2.209, 95% CI = 1.064, 4.584, p-value < 0.05), and who had good self-care agency (AOR = 1.222, 2.956, p-value < 0.05) were more likely to have good self-care practice.
Conclusion
Most of the study participants reported poor self-care practices. Factors associated with hypertension self-care practice are marital status, education, source of self-care information, place for exercise, social support, and self-care agency. Targeted interventions are needed to improve hypertension self-care practice.
Keywords: Self-care practice, Hypertension, Social support, Self-care agency, Ethiopia
Background
Hypertension or high blood pressure is the leading global health problem which is prevalent in all regions and countries of the world [1–4]. It is one of the three leading risk factors for global disease burden accounting for 7% of the global disability-adjusted life years (DALYs) [4]. About 31.1% of the world adult population lives with hypertension, and 28.5% are in high-income countries while 31.5% are in low-and middle-income countries [5]. The age-standardized prevalence of hypertension is 25.9% among different population groups in the sub-Saharan Africa [6]. In Ethiopia, the prevalence of hypertension is 31.5% among men and 28.9% among women in Addis Ababa, [7] 18.8% in Sidama Zone, [8] 28.3% in Gondar, [9] 13.2% in Jimma, [10] and 11% in Mekele [11]. Thus, hypertension has become an important health threat in this resource limited country – Ethiopia.
Hypertension is an important risk factor for cardiovascular disease and mortality. According to the World Health Organization’s (WHO) report, complications of hypertension accounts for 9.4 million of the annual 17 million worldwide deaths from cardiovascular disease [12]. The report further explains that hypertension is responsible for approximately 45% of deaths resulting from heart disease and 51% of deaths from stroke. In addition, hypertension is a risk factor for renal and eye diseases [13, 14].
Studies have demonstrated that self-care practice is essential for blood pressure control and reduction of hypertension complications of cardiovascular and renal diseases [15–17]. Hypertension self-care has been defined as “a dynamic and active process requiring knowledge, attitude, discipline, determination, commitment, self-regulation, empowerment and self-efficacy” [18]. It involves medication taking, consumption of low-sodium and low-fat diet, exercise, limiting alcohol drinking, not smoking, weight reduction, self-monitoring blood pressure, regular healthcare visit, and reducing stress [19]. The use of a combination of diet rich in fruits, vegetables, and low-fat dairy products with reduced saturated and total fat lowers systolic blood pressure by 5.5 mmHg and diastolic blood pressure by 3 mmHg [20–22]. Restricting sodium intake to no more than 2.4 g per day would lowers systolic blood pressure by 2–8 mmHg in hypertensive patients [23–25]. Performing regular aerobic physical activity at least 30 min daily and 150 min per week would reduces systolic blood pressure by 4–9 mmHg [26, 27]. A 50% reduction of daily alcohol consumption would also lower systolic blood pressure by 2–7 mmHg and diastolic blood pressure by 2–5 mmHg [28, 29]. Reducing weight to maintain normal body mass index (18.5–24.9 Kg/m2) would lower systolic blood pressure by 3–7 mmHg and diastolic blood pressure by 3–9 mmHg [30–32].
Nevertheless, hypertensive patients often do not implement the recommended self-care practices and ultimately suffer from uncontrolled blood pressure. According to a recent study, about 50% of hypertensive patients in southwest Ethiopia live with uncontrolled blood pressure [33]. A multitude of factors may affect hypertension self-care practice. These may include demographic factors such as age, education, employment, and health literacy [34–37], illness duration [34, 36], empowerment factors such as self-care agency and self-efficacy [34, 38, 39], hypertension knowledge [40], and social support [38, 41]. However, we know little concerning hypertension self-care in Ethiopia. Therefore, the purpose of this study was to assess hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. This study was informed by the Health-Promoting Self-Care System Model (HPSCSM) which is used as a framework for identifying and explaining patterns among factors that influence the decision-making, performance and outcomes of health-promoting lifestyles [42]. The HPSCSM was built by synthesizing concepts from Orem’s Self-Care Deficit Nursing Theory [43], Cox’s Interaction Model of Client Health Behavior [44], and Pender’s Health Promotion Model [45]. The HPSCSM proposes that demographics, social factors, environmental factors, perceived health state, and health care expenditure influence individual’s performance of health-promoting self-care. The association between these variables and hypertension self-care practice was analyzed in this study.
Methods
Design and sample
This was institution-based cross-sectional study conducted in 4 public health institutions in Dessie town using proportionally allocated stratified sampling method. The study conformed to the fundamental principles of research ethics and approved by the Institutional Review Board (IRB) of the College of Health Science at Addis Ababa University. Permission to conduct the research was obtained from the authorities in the study settings and informed consents were secured from each participant. A total of 309 participants, with 98% of response rate, consented and recruited from one public hospital and three health centers in Dessie town from March to May 2017. The sample size was determined using a single population proportion formula based on the following assumptions: considering 95% of confidence level, 5% margin of error, and 50% population proportion. A sample size correction formula was also applied since the total hypertensive patient population was less than 10,000. The study participants were finally recruited using systematic sampling technique with the patients’ follow up registry serving as a sampling frame in each participating institution. Every 4 patient in the registry was recruited from each institution with the first one determined using a lottery method. Patients were included in this study if they meet the following criteria: being on hypertension follow up at least for the last 6 months; 18 years or older; and can read and write in Amharic language. Patients were excluded if they were critically sick and have serious mental or cognitive impairment. The participants completed the interviewer-administered questionnaire immediately after giving consent.
Measures
Sociodemographic information such as age, sex, ethnicity, income, marital status, residence place, income, and educational status were collected using eight structured items included in the interviewer-administered questionnaire. A single dichotomous item was used to measure family history of hypertension. Duration since diagnosed as hypertensive and source of information about hypertension self-care were respectively measured using single multiple-choice type items. We have also used one dichotomous item to measure availability of convenient place to perform physical activity.
The behavioral scale of Hypertension Self-Care Profile (HBP-SCP) [46] was used to measure the self-care practice of participants in this study. The HBP-SCP is a 20-item measure with each question having 4 response options: not at all = 1, sometimes = 2, often = 3, and always = 4. A total score can range from 20 to 80 with higher score indicating better self-care practice. The behavioral scale of the original HBP-SCP [46] had Cronbach’s alpha of 0.83 where as alpha of approximately 0.85 was recently reported by two studies from Singapore [47, 48].
The Appraisal of Self-Care Agency – Revised (ASAS-R) [49, 50] was used to measure self-care agency in this study. The ASAS-R is a 15-item measure that assesses the extent of self-care agency of individuals on a 5-point Likert scale ranging from 1 = totally disagree to 5 = totally agree. The total score can range from 15 to 75 with higher score indicating better self-care agency. A Cronbach’s alpha of 0.89 was reported for the original version of ASAS-R [49].
The Multidimensional Scale of Perceived Social Support (MSPSS) was used to measure subjectively assessed social support [51, 52]. The MSPSS is a 12-item measure of the perceived adequacy of social support on a 7-point Likert-type scale ranging from 1 = very strongly disagree to 7 = very strongly agree. The total score range from 12 to 84 with higher score indicating better perceived social support. Cronbach’s alpha of 0.87 was reported for patient groups [53].
Data analysis
Data was entered into the Statistical Package for Social Sciences (SPSS) version 22 and then checked and cleaned. Descriptive statistics were calculated to describe the characteristics of the participants and the measured variables. Mean with standard deviation and percentages were used to present the descriptive statistics. Pearson’s correlation was computed to explore the bivariate correlation between hypertension self-care, self-care agency, and social support scores. In preparation for logistic regression analysis, we have dichotomized the HBP-SCP score as follow: good self-care practice for a score equal to or above the mean and poor self-care practice for a score below the mean. We have also used the same procedure to dichotomize the ASAA-R and MSPSS scores. The sociodemographic variables, source of information, place of exercise, social support, and self-care agency associations with self-care were analyzed first by using simple logistic (bivariate) regression model. Then, we used variable selection method for the multiple logistic analyses rather than pre-specifying the model because of lack of theoretical bases that serve as priori. Thus, only those variables with p-value less than or equal to 0.2 were taken as candidate for multiple logistic regression analysis. A p-value cut-off 0.2 was used to reduce the number of variables entered in the regression model presuming that there would not be much change for the variables with p-value more than 0.2. In both simple and multiple regression models, the statistical significance of associations between variables were determined using odds ratios with 95% confidence interval (CI) and p-values below 0.05.
Result
Participant characteristics
Table 1 shows that the participants mean age was 58.8, the majority were between 40 and 60 years (n = 142, 49.1%), female (n = 165, 53.4%), Muslims (n = 158, 51.1%), urban dwellers (n = 260, 84.1%), ethnic Amhara (n = 288, 93.8), and married (n = 214, 69.3%). From the total participants, 139 (45%) were farmers, 90 (29.1%) had family history of hypertension, 186 (60.2%) got information about self-care through health education, 180 (58.3%) lived with hypertension for more than 2 years, and 169 (54.7%) had no convenient place for physical activity. Table 1 also shows the disaggregated mean scores of the HBP-SCP.
Table 1.
Characteristics of the study participants (N = 309)
| Characteristics | n (%) | HBP-SCP Score, Mean (SD) | |
|---|---|---|---|
| Age (in years): Mean = 58.8 |
<40 years | 26 (8.4) | 40.6 (7.8) |
| 40–60 years | 142 (49.1) | 37.4 (8.2) | |
| >60 years | 130 (42.1) | 37.6 (8.4) | |
| Gender: | Male | 144 (46.6) | 39.2 (9.0) |
| Female | 165 (53.4) | 36.4 (7.3) | |
| Religious affiliation: | Orthodox | 143 (46.3) | 39.1 (8.6) |
| Muslim | 158 (51.1) | 36.5 (7.8) | |
| Protestant | 5 (1.6) | 40.4 (8.7) | |
| Residence place: | Urban | 260 (84.1) | 37.9 (8.4) |
| Rural | 49 (15.9) | 36.8 (7.6) | |
| Ethnicity: | Amhara | 288 (93.8) | 37.7 (8.2) |
| Tigre | 14 (4.3) | 38.6 (8.9) | |
| Oromo | 4 (1.3) | 39.7 (9.0) | |
| Others | 1 (0.6) | – | |
| Marital status: | Single | 20 (6.5) | 40.4 (8.7) |
| Married | 214 (69.3) | 38.1 (8.3) | |
| Divorced | 28 (9.1) | 32.8 (6.7) | |
| Widowed | 47 (15.2) | 37.1 (7.8) | |
| Educational status: | Unable to read & write | 100 (32.4) | 34.4 (6.6) |
| Traditional clergy-based teaching | 59 (19.1) | 37.2 (7.9) | |
| Primary school | 69 (22.3) | 38.2 (8.5) | |
| Secondary school | 35 (11.3) | 40.0 (8.4) | |
| College/University | 46 (14.9) | 44.4 (7.7) | |
| Occupation: | Farmer | 139 (45.0) | 35.5 (6.4) |
| Government employee | 49 (15.9) | 42.6 (8.1) | |
| Private employee | 24 (7.8) | 37.2 (7.8) | |
| Merchant | 59 (19.1) | 38.3 (8.8) | |
| Others | 37 (12) | 39.7 (11.0) | |
| Monthly income (in ETB): | <500 | 84 (26.2) | 37.4 (9.1) |
| 501–1000 | 84 (27.5) | 35.1 (8.2) | |
| >1000 | 141 (46.3) | 39.5 (7.3) | |
| Family history of HBP: | Yes | 90 (29.1) | 38.0 (8.2) |
| No | 219 (70.9) | 37.6 (8.3) | |
| Source of information: | Books | 28 (9.1) | 45.4 (8.6) |
| News | 1 (0.3) | – | |
| Health education | 186 (60.2) | 38.8 (8.4) | |
| No information | 94 (30.4) | 33.4 (4.9) | |
| Duration with HBP: | <6 months | 1 (0.3) | – |
| 6months – 2 years | 126 (40.8) | 37.0 (7.2) | |
| >2 years | 180 (58.3) | 38.3 (8.9) | |
| Place for exercise: | Yes | 140 (45.3) | 40.2 (9.2) |
| No | 169 (54.7) | 36.1 (7.1) | |
SD Standard Deviation, HBP-SCP Hypertension Self-Care Profile, HBP Hypertension, ETB Ethiopian Currency
Self-care practice and correlations
As presented in Table 2, the overall mean score for hypertension self-care practice was 37.7 ± 8.2. From the total participants, 51% scored below the mean on the HBP-SCP, indicating poor self-care practice. On the other hand, 52.8 and 70.2% scored equal to or above the mean on self-care agency and social support scales, respectively.
Table 2.
Mean scores and correlation coefficient of HBP-SCP, ASAS-R, and MSPSS (N = 309)
| Variables | Mean (SD) | 1 | 2 | 3 |
|---|---|---|---|---|
| 1. Hypertension self-care profile (HBP-SCP) | 37.7 (8.2) | 1 | ||
| 2. Appraisal of self-care agency (ASAS-R) | 27.8 (7.0) | - 0.33* | 1 | |
| 3. Multidimensional scale of social support (MSPSS) | 40.2 (12.4) | 0.35* | - 0.30* | 1 |
*2-tailed p-value = 0.01
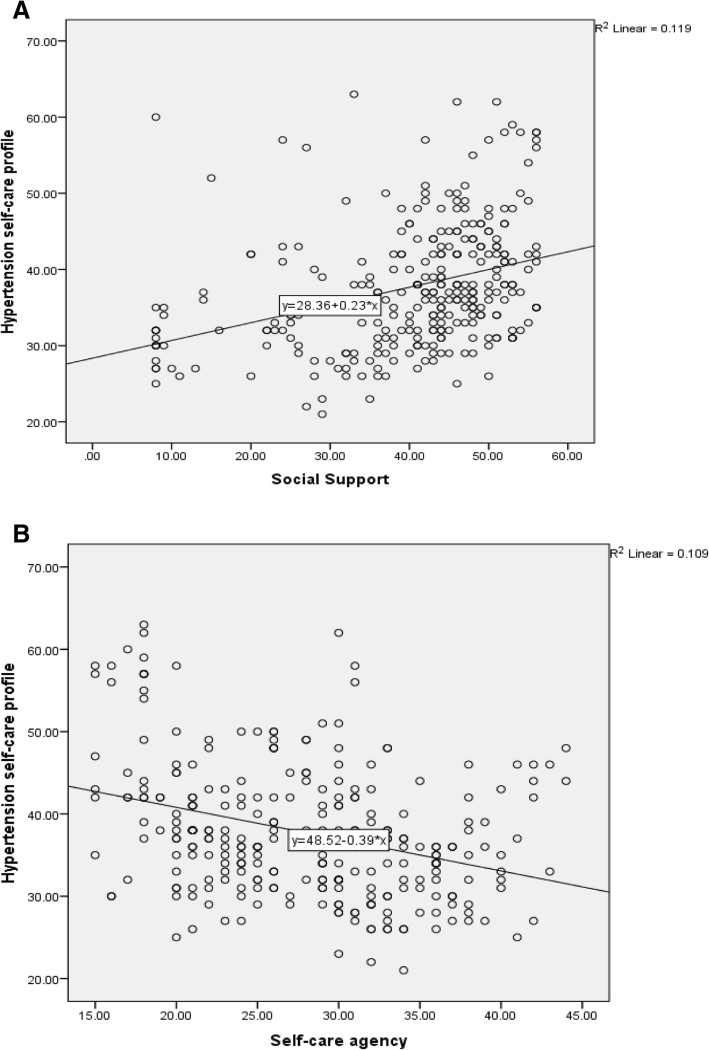
Figure 1 presents the correlation coefficient between hypertension self-care practice, self-care agency, and social support. Social support was positively correlated with hypertension self-care practice (R2 = 0.119, p = 0.01) while self-care agency was negatively correlated (R2 = 0.109, p = 0.01).
Fig. 1.
Correlation between hypertension self-care profile with social support (Pane a) and self-care agency (Panel b)
Factors associated with hypertension self-care practice
In the simple logistic regression analysis, educational status of the participants, source of self-care information, income, gender, age, marital status, occupation, self-care agency, and social support had statistically significant association with hypertension self-care practice. However, in multiple logistic regression analysis only marital status, education, source of self-care information, place for exercise, social support, and self-care agency had statistically significant association with hypertension self-care practice (Table 3). Divorced participants were about 88% less likely to have good self- care practice compared to those who were single (AOR = 0.115, 95% CI = 0.026, 0.508, p-value < 0.01). Participants who had traditional clergy-based teaching were 2.2 times more likely to have good self-care practice compared to those who were unable to read and write (AOR = 2.209, 95% CI = 1.064, 4.584, p-value < 0.05). Compared to participant who obtained self-care information from books those who had no access to sources of information were about 92% less likely to have good self-care practice (AOR = 0.084, 95% CI = 0.022, 0.322, p-value < 0.01). Participant who had convenient place for exercise were about 3 times more likely to have good self-care practice compared to those who had not (AOR = 2.968, 95% CI = 1.826, 4.825, p-value < 0.01). Compared to participants with poor social support those who had good social support were 2.2 times more likely to have good self-care practice (AOR = 2.204, 95% CI = 1.272, 3.821, p-value < 0.01). Finally, participants who possessed good self-care agency were about 2 times more likely to have good self-care practice compare to those who had poor self-care agency (AOR = 1.222, 2.956, p-value < 0.05).
Table 3.
Factors associated with hypertension self-care practice (N = 309)
| Variable | Self-care practice | Crude Odds Ratio (COR), 95% CI | Adjusted Odds Ratio (AOR), | |||
|---|---|---|---|---|---|---|
| Good (n) | Poor (n) | 95% CI | p-value | |||
| Gender | Male | 80 | 64 | 1.0 | 1.0 | |
| Female | 73 | 92 | 0.64 (0.40, 0.99) | 0.58 (0.37, 0.92) | 0.058 | |
| Age | <40 years | 18 | 8 | 1.0 | 1.0 | |
| 40–60 years | 74 | 78 | 0.42 (0.17, 1.02) | 0.32 (0.12, 0.83) | 0.058 | |
| >60 years | 60 | 70 | 0.381 (0.16, 0.94) | 0.33 (0.13, 0.88) | 0.06 | |
| Marital status | Single | 16 | 4 | 1.0 | 1.0 | |
| Married | 108 | 106 | 0.26 (0.08, 0.79) | 0.32 (0.09, 1.07) | 0.17 | |
| Divorced | 8 | 20 | 0.1 (0.03, 0.39) | 0.12 (0.03, 0.51)*** | 0.001 | |
| Widowed | 21 | 26 | 0.20 (0.06, 0.69) | 0.27 (0.07, 1.06) | 0.011 | |
| Educational status | Unable to read and write | 33 | 67 | 1.0 | 1.0 | |
| Traditional clergy-based teaching | 29 | 30 | 1.96 (1.02, 3.79) | 2.21 (1.06, 4.58)** | 0.036 | |
| Primary school | 33 | 36 | 1.86 (0.99, 3.49) | 1.86 (0.92, 3.89) | 0.046 | |
| Secondary school | 24 | 11 | 4.43 (1.94, 10.12) | 2.52 (0.92, 6.91) | 0.026 | |
| College/university | 34 | 12 | 5.75 (2.64, 12.53) | 1.93 (0.71, 5.24) | 0.013 | |
| Source of information | Books | 24 | 4 | 1.0 | 1.0 | |
| News | 0 | 1 | 0.00 [0.00] | 0.0 (0, 0.00) | 1.00 | |
| Health education | 103 | 83 | 0.21 (0.07, 0.62) | 0.31 (0.09,1.05) | 0.005 | |
| No information | 26 | 68 | 0.06 (0.02, 0.20) | 0.08 (0.02, 0.32)*** | 0.000 | |
| Place for exercise | No | 66 | 103 | 1.0 | 1.0 | |
| Yes | 87 | 53 | 2.56 (1.62, 4.06) | 2.97 (1.83, 4.83)*** | 0.000 | |
| Social support | Good social support | 123 | 94 | 2.70 (1.62, 4.51) | 2.20 (1.27, 3.82)*** | 0.005 |
| Poor social support | 30 | 62 | 1.0 | 1.0 | ||
| Self-care agency | Good Self-care agency | 65 | 98 | 2.29 (1.45, 3.16) | 1.82 (1.12,2.96)** | 0.015 |
| Poor Self-care agency | 88 | 58 | 1.0 | 1.0 | ||
**p-value < 0.05; ***p-value < 0.01
Discussion
In this study, we explored the level of self-care practice and associated factors among hypertensive patients in public health facilities of Dessie town. Of the total participants, 51% had poor hypertension self-care practice. Poor self-care practice can be associated with increased prevalence of uncontrolled hypertension. Previous study reported a high prevalence of uncontrolled hypertension in Ethiopia [33]. Poor self-care practice may also contribute to the high risk of developing cardiovascular and renal complications among hypertensive patients.
Our study identified that marital status, education, source of self-care information, place for exercise, social support, and self-care agency have strong association with hypertension self-care practice. Compared to single hypertension patients those who were divorced engaged less in self-care practice. Previous studies in other disease conditions have also shown the influence of divorce on self-care behaviors [54]. This may be linked to the detrimental effect of divorce on mental and physical health status a person [55, 56] that in turn affects the ability to perform self-care activities [57]. Thus, divorced hypertension patients need to be given due considerations when designing and implementing self-care interventions.
This study revealed that hypertensive patients who had traditional clergy-based teaching were better off in self-care practices compared to those who cannot read and write. This corroborates with the findings of studies from other settings that identified lack of education and poor health literacy as risk factors for non-adherence to the recommended hypertension self-care practices. [35, 37]. Possessing the at least traditional clergy-based education could enable the patient to understand and follow the recommended self-care practices. This implies the need to design an educational intervention convenient for those who cannot read and write.
The presence of a convenient place for exercise is also an important predictor of hypertension self-care practice in this study. This finding corroborates with the established evidence that safe, walkable, and aesthetically pleasant physical environment positively influence individuals participation in physical activity [58–60]. Thus, facilitating physical activity among hypertensive patients require efforts in environmental planning and policy change. It may also requires creating community awareness about the importance of modifying the aesthetic nature of the local environment such as footpaths and trails, increasing accessibility of places to walk to, and reducing the level of road traffics for health.
Both social support and self-care agency were also good predictors of hypertension self-care practice in this study. Though limited, previous studies have also shown that higher socials support [41, 61] and self-care agency [62] are positively associated with hypertension self-care practices. This implies the need to develop strategies to improve social support and self-care agency in order to enhance hypertension self-care practice. Prospective studies are also needed to determine the effects of social support and self-care agency on hypertension self-care practice.
Our study shows that women hypertensive patient and those above 40 years of age were less likely to engage in hypertension self-care practice, using the 95% CI. This is contrary to the findings of a study conducted among African American, in which older adults and women more likely engaged in hypertension self-care [39]. The discrepancy may be linked to the difference in exposure to self-care information and the tools used the measure self-care.
Limitations
This study has numerous limitations. Firstly, the use of cross-sectional design does not allow inferring causality. Prospective and experimental studies are warranted. Secondly, self-report measures were used for data collection, thus subject to recall bias that may affect the precision of measurement. Thirdly, we were not able to measure blood pressure due to lack of resources to purchase standardized measurement apparatus. Fourthly, even though our sampling approach was robust, we are not sure that the recruited participants were the same as those who were not recruited. This might have been source of selection bias. Finally, some potential influencing factors such as self-esteem, perceived health state, and health care experience were not measured in this study.
Conclusion
Most of the hypertensive patients in this study reported poor self-care practices. Living in divorce status, the inability to read and write, lack of source of self-care information, lack of place for exercise, poor social support, and poor self-care agency may be the predisposing factors for this poor hypertension self-care practice. These findings suggest that patient’s marital status, the ability to read and write, and the presence of convenient environment for physical activity should be considered when planning hypertension self-care education. Instituting strategies to improve social support and self-care agency combined with prospective studies to determine their effective on hypertension self-care practices is also implied.
Acknowledgements
We would like to thank the patients who volunteered to provide data for this study.
Funding
The study was funded by Addis Ababa University.
Availability of data and materials
The dataset generated and analyzed during this study is not publicly available in order to maintain data security but are available from the corresponding author on reasonable request.
Abbreviations
- ASAS-R
Appraisal of Self-Care Agency-Revised
- CI
Confidence interval
- DALYS
Global disability-adjusted life years
- HB-SCP
Hypertension Self-Care Profile
- HPSCSM
Health-Promoting Self-Care System
- MSPSS
Multidimensional Scale of Perceived Social Support
- SPSS
Statistical Package for Social Sciences
- WHO
World Health Organization
Authors’ contributions
SA, FA, and DG were involved in conceptualizing and designing the study, analyzing and interpreting the data, and drafting and critically reviewing the manuscript. Three of them read and approved the manuscript.
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Institutional Review Board (IRB) of Addis Ababa University, College of Health Sciences. Permission to conduct the research was obtained from the authorities in the study settings and informed consents were secured from each participant. Confidentiality of the participant was maintained by not including names or any personal identifier during data collection, analysis, and reporting. Participants right to refuse participation, not to answer any question they don’t want to, or withdraw participation after enrolling was fully respected.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sewunet Ademe, Phone: +251-918126233, Email: sewunet.ademe@gmail.com.
Fekadu Aga, Phone: +251-911033684, Email: fiqaaduuagaa@yahoo.com.
Debela Gela, Phone: +251-913179679, Email: debelagela@gmail.com.
References
- 1.Hedner T, Kjeldsen SE, Narkiewicz K. State of global health – hypertension burden and control. Blood Press. 2012;21(Suppl 1):1–2. doi: 10.3109/08037051.2012.704786. [DOI] [PubMed] [Google Scholar]
- 2.Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. 2013;15(3):134–136. doi: 10.1007/s11906-013-0340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Abate KH, Akinyemiju TF, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm hg, 1990-2015. JAMA. 2017;317(2):165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 4.Lim SS, Vos T, Flaxman AD, Daniel G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, Bajunirwe F, Njelekela M, Chiwanga FS, Reid T, et al. The burden of hypertension in sub-Saharan Africa: a four-country cross sectional study. BMC Public Health. 2015;15:1211. doi: 10.1186/s12889-12015-12546-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tesfaye F, Byass P, Wall S. Population based prevalence of high blood pressure among adults in Addis Ababa: uncovering a silent epidemic. BMC Cardiovascular Disorders. 2009;9:39. doi: 10.1186/1471-2261-1189-1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giday A, Wolde M, Yihdego D. Hypertension, obesity and central obesity in diabetics and non diabetics in southern Ethiopia. Ethiop J Health Dev. 2010;24(2):145–147. doi: 10.4314/ejhd.v24i2.62964. [DOI] [Google Scholar]
- 9.Awoke A, Awoke T, Alemu S, Megabiaw B: Prevalence and associated factors of hypertension among adults in Gondar, Northwest Ethiopia: a community based cross-sectional study. BMC Cardiovascular Disorders 2012, 12(113):http://www.biomedcentral.com/1471-2261/1412/1113. [DOI] [PMC free article] [PubMed]
- 10.Gudina EK, Michael Y, Assegid S. Prevalence of hypertension and its risk factors in Southwest Ethiopia: a hospital-based cross-sectional survey. Integrated Blood Pressure Control. 2013;6:111–117. doi: 10.2147/IBPC.S47298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zikru AB, Gebru HB, Kahsay AB. Prevalence and associated factors of hypertension among adult population in Mekele City, northern Ethiopia. IJIPSR. 2014;2(3):653–668. [Google Scholar]
- 12.WHO . A global brief on hypertension: Silen killer, global public health crisis. Geneva: WHO; 2013. [Google Scholar]
- 13.Arguedas J, MI O, Wright J: Treatment blood pressure targets for hypertension. Cochrane Database of Systematic Reviews 2009, Issue 3:Art. No.: CD004349.DOI: 004310.001002/14651858.CD14004349.pub14651852. [DOI] [PubMed]
- 14.Fraser-Bell S, Symes R, Vaze A. Hypertensive eye disease: a review. Clin Exp Ophthalmol. 2017;45:45–53. doi: 10.1111/ceo.12905. [DOI] [PubMed] [Google Scholar]
- 15.Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, Feig DS, Cafazzo JA. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension. 2012;60:51–57. doi: 10.1161/HYPERTENSIONAHA.111.188409. [DOI] [PubMed] [Google Scholar]
- 16.Maciejewski ML, Bosworth HB, Olsen MK, Smith VA, Edelman D, Powers BJ, Kaufman MA, Oddone EZ, Jackson GL. Do the benefts of participation in a hypertension self-management trial persist after patients resume usual care? Circ Cardiovas Qual Outcomes. 2014;7:269–275. doi: 10.1161/CIRCOUTCOMES.113.000309. [DOI] [PubMed] [Google Scholar]
- 17.Kim KB, Han H-R, Huh B, Nguyen T, Lee H, Kim MT. The effect of a cCommunity-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27(9):1199–1208. doi: 10.1093/ajh/hpu041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balduino AFA, Mantovani MF, Lacerda MR, Meier MJ. Conceptual analysis of self-management of hypertensive individuals. Rev Gaúcha Enferm. 2013;34(4):37–44. doi: 10.1590/S1983-14472013000400005. [DOI] [PubMed] [Google Scholar]
- 19.Han H-R, Song H-J, Nguyen T, Kim MT. Measuring self-care in patients with hypertension: a systematic review of literature. J Cardiovasc Nurs. 2014;29(1):55–67. doi: 10.1097/JCN.0b013e3182775fd1. [DOI] [PubMed] [Google Scholar]
- 20.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Setkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 21.Svetkey LP, Simons-Morton D, Vollmer WM, Appel LJ, Conlin PR, Ryan DH, Ard J, Kennedy BM. Effects of dietary patterns on blood pressure: subgroup analysis of the dietary approaches to stop hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159:285–293. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 22.Sacks FM, Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Setkey LP, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A dietary approach to prevent hypertension: A review of the Dietary Approaches to Stop Hypertension (DASH) Study. Clinical Cardiology. 1999;22(Suppl.III):III-6–III-10. doi: 10.1002/clc.4960221503. [DOI] [PubMed] [Google Scholar]
- 23.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 24.Chobanian AV, Hill M. National Heart, Lung, and Blood Institute workshop on sodium and blood pressure: a critical review of current scientific evidence. Hypertension. 2000;35:858–863. doi: 10.1161/01.HYP.35.4.858. [DOI] [PubMed] [Google Scholar]
- 25.Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, Conlin PR, Svetkey LP, Erlinger TP, Moore TJ, et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135(12):1084–1086. doi: 10.7326/0003-4819-135-12-200112180-00005. [DOI] [PubMed] [Google Scholar]
- 26.Kelley GA, Kelley KS. Progressive resistance exercise and resting blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2000;35:838–843. doi: 10.1161/01.HYP.35.3.838. [DOI] [PubMed] [Google Scholar]
- 27.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 28.Xin X, He J, Frontini MG, Ogden L, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–1117. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 29.Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e108–e120. doi: 10.1016/S2468-2667(17)30003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Whelton PK, Appel LJ, Charleston J, Dalcin A, Haythornthwaite J, Rosofsky W, Wanek K, Walker G, Oberman A, Bragg C, et al. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure: the trials of hypertension prevention, phase II. Arch Intern Med. 1997;157:657–667. doi: 10.1001/archinte.1997.00440270105009. [DOI] [PubMed] [Google Scholar]
- 31.He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35:544–549. doi: 10.1161/01.HYP.35.2.544. [DOI] [PubMed] [Google Scholar]
- 32.Stevens VJ, Obarzanek E, Cook NR, Lee I-M, Appel LJ, West DS, Milas NC, Mattfeldt-Beman M, Belden L, Bragg C, et al. Long-term weight loss and changes in blood pressure: results of the trials of hypertension prevention, Phase II. Ann Int Med. 2001;134(1):1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 33.Asgedom SW, Gudina EK, Desse TA: Assessment of blood pressure control among hypertensive patients in Southwest Ethiopia. PLoS ONE 2016, 11(11):e0166432. doi:0166410.0161371/journal.pone.0166432. [DOI] [PMC free article] [PubMed]
- 34.Lee J-E, Han H-R, Song H, Kim J, Kim KB, Ryu JP, Kim MT. Correlates of self-care behaviors for managing hypertension among Korean Americans: a questionnaire survey. Int J Nurs Stud. 2010;47:411–417. doi: 10.1016/j.ijnurstu.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Anowie F, Darkwa S. The knowledge, attitudes and lifestyle practices of hypertensive patients in the Cape Coast Metropolis-Ghana. J Sci Res Rep. 2015;8(7):1–15. [Google Scholar]
- 36.Khresheh R, Mohammed N. Self-care behaviors among women with hypertension in Saudi Arabia. IOSR J Nursi Health Sci. 2016;5(3):52–56. [Google Scholar]
- 37.Crowley MJ, Gurubber JM, Olsen MK, Bosworth HB. Factors associated with non-adherence to three hypertension self-management behaviors: preliminary data for a new instrument. J Gen Intern Med. 2012;28(1):99–106. doi: 10.1007/s11606-012-2195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang AK, Lee EJ. Factors affecting self-care in elderly patients with hypertension in Korea. Int J Nurs Pract. 2015;21:584–591. doi: 10.1111/ijn.12271. [DOI] [PubMed] [Google Scholar]
- 39.Warren-Findlow J, Seymour RB, Huber LRB. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37(1):15–24. doi: 10.1007/s10900-011-9410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bilal M, Haseeb A, Lashkerwala SS, Zahid I, Siddiq K, Saad M, Dar MI, Arshad MH, Shahnawaz W, Ahmed B, et al. Knowledge, awareness and self-care practices of hypertension among cardiac hypertensive patients. Global J Health Sci. 2016;8(2):9–19. doi: 10.5539/gjhs.v8n2p9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hu H, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Hum Hypertens. 2015;29:198–203. doi: 10.1038/jhh.2014.58. [DOI] [PubMed] [Google Scholar]
- 42.Simmons SJ. The health-promoting self-care system model: directions for nursing research and practice. J Adv Nurs. 1990;15:1162–1166. doi: 10.1111/j.1365-2648.1990.tb01708.x. [DOI] [PubMed] [Google Scholar]
- 43.Orem D. The development of the self-care deficit theory of nursing: events and circumstances. In: Renpenning KM, Tylor SG, editors. Self-Care Theory in Nursing: Selected papers of Dorothea Orem. New York: Springer Publishing Company, Inc; 2003. [Google Scholar]
- 44.Cox CL. An interaction model of client health behavior: theoretical prescription for nursing. Adv Nurs Sci. 1982;5(1):41–56. doi: 10.1097/00012272-198210000-00007. [DOI] [PubMed] [Google Scholar]
- 45.Johnson JL, Ratner PA, Bottorff JL, Hayduk LA. An exploration of Pender’s health promotion model using LISREL. Nurs Res. 1993;42(3):132–138. doi: 10.1097/00006199-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 46.Han H-R, Lee H, Commodore-Mensha Y, Kim M. Development and validation of the hypertension self-care profile: a practical tool to measure hypertension self-care. J Cardiovasc Nurs. 2014;29(3):E11–E20. doi: 10.1097/JCN.0b013e3182a3fd46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koh YLE, Lua YHA, Hong L, Bong HSS, Yeo LSJ, Tsang LPM, Ong KZ, Wong SWS, Tan NC. Using a web-based approach to assess test–retest reliability of the “hypertension self-care profile” tool in an Asian population: a validation study. Medicine. 2016;95(9):1–8. doi: 10.1097/MD.0000000000002955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seow KC, Yusoff DM, Koh YLE, Tan NC: What is the test-retest reliability of the Malay version of the Hypertension Self-Care Profle self effcacy assessment tool? A validation study in primary care. BMJ Open 2017, 7:e016152. doi:016110.011136/bmjopen-012017-016152. [DOI] [PMC free article] [PubMed]
- 49.Sousa VD, Zauszniewski JA, Bergquist-Beringer S, Musil CM, Neese JB, Jaber AF. Reliability, validity and factor structure of the appraisal of self-care agency scale – revised (ASAS-R) J Eval Clin Pract. 2010;16:1031–1040. doi: 10.1111/j.1365-2753.2009.01242.x. [DOI] [PubMed] [Google Scholar]
- 50.Damásio BF, Koller SH. The appraisal of self-care agency scale – revised (ASAS-R): adaptation and construct validity in the Brazilian context. Cad Saúde Pública, Rio de Janeiro. 2013;29(10):2071–2082. doi: 10.1590/0102-311X00165312. [DOI] [PubMed] [Google Scholar]
- 51.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]
- 52.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3 & 4):610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 53.Wongpakaran T, Wongpakaran N, Ruktrakul R. Reliability and validity of the multidimensional scale of perceived social support (MSPSS): Thai version. Clin Pract Epidemiol Ment Health. 2011;7:163–166. doi: 10.2174/1745017901107010161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Challaghan D. Healthy behaviors, self-efficacy, self-care, and basic conditioning factors in older adults. J Community Health Nurs. 2005;22(3):169–178. doi: 10.1207/s15327655jchn2203_4. [DOI] [PubMed] [Google Scholar]
- 55.Lorenz FO, Wickrama KAS, Conger RD, Elder GH. The short-term and decade-long effects of divorce on women’s midlife health. J Health Soc Behav. 2006;47(2):111–125. doi: 10.1177/002214650604700202. [DOI] [PubMed] [Google Scholar]
- 56.Hewitt B, Turrell G, Giskes K. Marital loss, mental health and the role of perceived social support: findings from six waves of an Australian population based panel study. J Epidemiol Community Health. 2012;66:308–314. doi: 10.1136/jech.2009.104893. [DOI] [PubMed] [Google Scholar]
- 57.Denyes MJ, Orem DE, SozWiss GB. Self-care: a foundational science. Nurs Sci Q. 2001;14(1):48–54. doi: 10.1177/089431840101400113. [DOI] [PubMed] [Google Scholar]
- 58.Barnett DW, Barnett A, Nathan A, Cauwenberg JV, Cerin E. Built environmental correlates of older adults’ total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14:103. doi: 10.1186/s12966-12017-10558-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carlin A, Perchoux C, Puggina A, Aleksovska K, Buck C, Burns C, Cardon G, Chantal S, Ciarapica D, Condello G, et al. A life course examination of the physical environmental determinants of physical activity behaviour: a “determinants of diet and physical activity” (DEDIPAC) umbrella systematic literature review. PLoS One. 2017;12(8):e0182083. doi: 10.1371/journal.pone.0182083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cerin E, Nathan A, Cauwenberg JV, Barnett DW, Barnett A. The neighbourhood physical environment and active travel in older adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14:15. doi: 10.1186/s12966-12017-10471-12965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Flynn SJ, Ameling JM, Hill-Briggs F, Wolf JL, Bone LR, Levine DM, Roter DL, Lewis-Boyer L, Fisher AR, Purnell L, et al. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. Patient Prefer Adherence. 2013;7:741–749. doi: 10.2147/PPA.S46517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Drevenhorn E, Bengtson A, Nyberg P, Kjellgren KI. Assessment of hypertensive patients’ self-care agency after counseling training of nurses. J Am Assoc Nurse Pract. 2015;27:624–630. doi: 10.1002/2327-6924.12222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and analyzed during this study is not publicly available in order to maintain data security but are available from the corresponding author on reasonable request.