Abstract
BACKGROUND:
Many individuals complain of disturbed sleep during the wintertime when their air conditioner (AC) is off. Therefore, we conducted this study to objectively assess the impact of AC sound on sleep latency, sleep duration, and sleep efficiency.
METHODS:
An experimental study was conducted on 48 healthy young adults, in their homes, to assess the effect of a standardized AC white noise, on sleep latency, duration, and efficiency, while simultaneously monitoring light intensity and room temperature. The study was conducted during the winter months. Sleep quality was objectively assessed using sleep actigraphy. Participants were monitored for two nights, during which two different, randomized sets of conditions were used: During one of the nights, the adults were exposed to 43 dB AC white noise; during the other night, adults were not exposed to the AC white noise.
RESULTS:
Actigraphy results showed that the mean sleep duration during the AC sound nights (ASNs) was 466.8 ± 60.8 min, compared to 478.8 ± 55.4 min during the non-AC sound nights (NASNs) (P = 0.6). Sleep-onset latency was 10.8 ± 15.2 min and 15.1 ± 18.2 min during the ASNs and the NASNs, respectively (P = 0.8). Moreover, there was no difference in sleep efficiency, 81% ± 7.8% vs. 78.8% ± 15.4% in the ASNs and NASNs, respectively (P = 0.9).
CONCLUSION:
AC sound had no significant positive effect on sleep duration, latency, and efficiency.
Keywords: Actigraphy, sleep duration, sleep efficiency, sleep latency, sleep quality, white noise
Sleep is a physiological state that is necessary for living organisms to recover normally. Normal sleep promotes health,[1] by serving several different functions, such as clearance of metabolic waste products, neural maturation, learning, memory consolidation, restorative processes, and repair and growth throughout the brain and body.[2,3]
Noise can have both auditory and extra-auditory health effects, which can alter sleep. Portas et al. using functional magnetic resonance imaging and electroencephalography showed bilateral auditory, parietal, and frontal cortical enhancement, during both wakefulness and sleep when subjects were exposed to auditory stimuli.[4]
Sleep is sensitive to several environmental factors that can reduce sleep quality and length. Ambient noise is an external stimulus that is still processed by humans' sensory functions during sleep.[5] Although sensitivity to noise decreases during sleep, it has been shown that humans still respond to noise stimulation during sleep.[5] In addition, the current data show that subjects do not adapt to these changes following long exposure times.[5]
White noise is a random signal having equal intensity at different frequencies. White noise makes hearing threshold level reaching its maximum rate, which means that in the presence of such sounds in the background of the environment, the more intense auditory stimuli are less capable of stimulating the cerebral cortex during sleep.[6] Overall, masking ambient noise with white noise has been proposed to improve sleep quality. A study conducted on guinea pigs showed that deaf guinea pigs presented an increase in both slow-wave sleep and rapid eye movement (REM) sleep compared to controls, thus showing that the auditory system modulates central nervous system structures that are involved in the sleep-wake cycle.[7] Healthy subjects who wore earplugs to reduce perceived simulated Intensive Care Unit (ICU) noise showed a significant decrease in REM sleep latency, increase in the percentage of REM sleep, and reduced arousal.[8]
It has been proposed that white noise auditory masking (defined as decreased audibility of background noise due to the presence of white noise) occurs because white noise decreases the difference between the background noise sound level and the disturbing signal sound level, which in turn reduces the bilateral auditory evoked response to the disturbing signal and increases the subjective arousal threshold.[9,10,11] There are two plausible hypotheses to why white noise reduces sleep disruption. First, white noise may influence the arousal threshold by making it greater than the total increase in sound level. Second, white noise may reduce the difference between the background noise level and the disturbing signal noise level, leading to the improvement of sleep consolidation and a decline in sleep arousal, despite an elevation in the mean baseline level of sound, in addition to the white noise sound level.[12] However, the current data have reported conflicting results regarding the effects of white noise on sleep quality.[11,13,14,15,16]
In hot climate countries, many people complain of disturbed sleep during the wintertime when they are not using their air conditioner (AC). A previous survey conducted by the National Sleep Foundation revealed that 5% of the American population uses sound generators such as fans, air purifiers, vacuum cleaners, and broadband noise (e.g., white noise) devices in their rooms to mask ambient noise and promote sleep.[17] It is thought that AC and other devices sound may act as white noise and hence help improve sleep quality.[17]
No study has objectively assessed the impact of AC sound on sleep parameters. Although the exact mechanisms are misunderstood, the studies mentioned above suggest that there is a relationship between noise and sleep. We hypothesize that the AC sound, which acts as white noise, will reduce sleep latency, increase sleep duration, and improve sleep efficiency. Therefore, this study attempts to better understand this relationship by assessing the effect of a standard monotonous AC sound on sleep latency, duration, bouts, and efficiency in healthy young adults using actigraphy while controlling for light intensity and room temperature.
Subjects and Methods
Subjects
This case-crossover study was conducted on a nonrandom sample of 48 healthy young adults (aged 18–25 years). Participants were recruited through advertisements placed on bulletin boards in the university. The sample size was calculated using the following formula: n = Z-score2× StdDev2/m2, where N is the required sample size, Z-score is the confidence level at 95% (1.96), StdDev is the standard deviation of the quantitative output (from an earlier published paper studying the effect of ICU noise, considered, white noise, on sleep),[12] and m is the margin of error (the used value is 10%).[18] The calculated sample size was 45. All participants were interviewed by the researchers, who excluded those with sleep disorders, circadian rhythm problems, psychiatric disorders, and hearing problems, those taking sleep promoting or altering medications, those who were smokers, those who were obese (body mass index >30 kg/m2), and those who were living in a noisy environment. Based on previous studies, the annoyance by outdoor and indoor noise sources was determined by the question, “Thinking about the last 12 months, when you are at home, how much would you say noise from the following sources (road noise, neighbor flat noise, parking noise, airplane noise, commercial noise, and train noise) bothers or annoys you?”[4,6,19] The strength of noise annoyance was rated by the five-step International Commission on Biological Effects of Noise scale of none, slight, moderate, strong, and too extreme.[4,6,19] Those who scored “none” or “slight” were included in the study. In addition, individuals who co-sleep in the same bed or room with another individual or those who attend and take care of others (e.g., parents or children) were excluded. Work and university classes' schedules for the participants were not different during the study days.
The project was approved by the ethics committee in our institute, and informed consent was obtained.
The study took place in Riyadh city in the subjects' houses, in 2016 and 2017 during December, January, and February. The average maximum temperature during these months was between 20°C and 22.0°C.[20]
Sleep measurements
Sleep latency, duration, and efficiency were measured using an actigraph (Actiwatch® L) (a noninvasive small actigraph unit in a wristwatch-like package) (Philips/Respironics, Inc., Murrysville, PA, USA).[21] Actigraphy is a noninvasive method that continuously monitors activity or movement, using a small device known as an actigraph. These medical devices are often used in clinical practice to monitor sleep disorders, especially circadian rhythm disorders, insomnia, and conditions that cause prolonged sleep and excessive daytime sleepiness. These devices are also used in research to study sleep conditions.[21] Periods of movement likely correspond to wakefulness, while those of relative stillness likely correspond to sleep or quiescence. This device is also able to record events, such as sleep or wake times. Multiple published studies have demonstrated the validity and accuracy of wrist actigraphy in detecting sleep latency, duration, and timing.[18]
Subjects wore the actigraph on their nondominant hand for three consecutive nights. No data were lost.
Measured sleep parameters
These are the definitions of the sleep parameters measured by actigraphy:[22]
Nocturnal sleep duration: The sum of all the minutes scored as sleep from the overall time in bed
Sleep latency: The time required for sleep onset after the intent to sleep has been initiated
Sleep efficiency: The percentage of time spent in bed sleeping. The scored total sleep time is divided by total time in bed and then multiplied by 100
Wake after sleep onset (WASO): Time spent awake in bed after the first nocturnal sleep onset. This period reflects sleep fragmentation and poor sleep quality
Sleeping bout: The total number of continuous blocks in an interval where the activity within the epoch was within the sleep threshold and therefore scored as “sleep”
Number of nocturnal sleeping bouts: The number of nocturnal sleeping bouts during time in bed. The higher the number, the more fragmented the sleep
Average duration of nocturnal sleeping bouts: Average duration of nocturnal sleeping bouts during time in bed. A higher duration indicates longer sleeping bouts, which means less nocturnal sleeping disturbances.
Study protocol
Before commencing the study (1st week of December 2017), a pilot study was conducted on five young adults to assess the effect of AC sound on their sleep latency, duration, and efficiency. Data were collected by the research team using actigraphy and a self-administered customized sleep diary.
The first night was used to let the subjects adapt to the device, AC white noise, and study protocol and to eliminate the first-night effect.[23] The first-night data were therefore not included in the analysis. The adults were then monitored for two consecutive nights; during one of the nights, the AC noise (white noise) was on, and during the other night, the AC noise was off. AC sound was randomly assigned to either night. The participants were instructed to maintain a regular sleep/wake pattern for 1 week before starting the study and to maintain that during the study.
To produce the AC white noise, the “White Noise Pro” (TMSOFT, LLC.) phone application was used. This phone application generated a recorded residential air conditioning (HVAC) sound, which was set to 43 dB (which is the average sound intensity off measured AC sounds).[19] The phone was placed 1 m away from the subject. As with AC, the sound cycles on and off.
The data were read and analyzed using actigraphy associated software (Philips Respironics).
Participants were asked to keep a self-administered sleep diary during both experimental days to record their presleep daily routine before going to bed and their sleep pattern from the previous night., The sleep diary consisted of three sections: (1) general information section to assess sleep hygiene; (2) presleep section including questions assessing the use of sleep-promoting and sleep-altering medications, naps, daytime sleepiness, stimulants, bedtime routine, and sleep disturbance factors; and (3) postsleep section including questions assessing sleep onset, sleep duration, in-bed and out-of-bed times, sleep maintenance, sleep disturbance factors, and attitude toward the AC sound. The completion rate of the sleep diary was 100%.
To control for other factors that may influence the measured sleep parameters, the participants were asked to turn their lights and ACs off and light intensity was measured using an actiwatch light model.[6] The room temperature range was measured using an Elitech DT-3 thermometer (Elitech In., NJ, USA).
Statistical analysis
Numeric data are expressed as mean ± StdDev, while categorical data are expressed as numbers and percentages. For group comparisons, we used paired-sample t-tests for numerical variables if the normality assumptions were met; if not, we used Wilcoxon tests. For categorical variables, we used Chi-square tests. Statistical Package for the Social Sciences (SPSS), IBM version 23 (SPSS Inc., Chicago, IL, USA) software was used for data analysis and management.
Results
Demographic characteristics
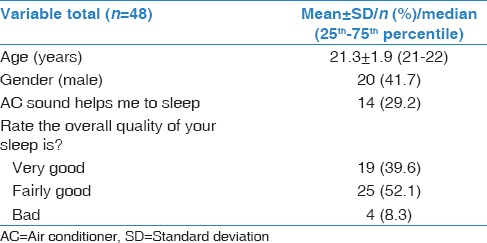
Table 1 presents the demographic characteristics of the participants. The mean age of the participants was 21 ± 1.9 years, and 58.3% of the subjects (n = 28) were females. Before the beginning of this study, approximately 29.2% (n = 14) of the participants believed that AC sound helps them to sleep; the remaining 70.8% (n = 34) believed that AC sound does not affect their sleep. The participants subjectively reported the quality of their sleep before the experiment, which ranged from very good (39.6% of participants), to fairly good (52.1%), to bad (8.3%).
Table 1.
Demographic and general information
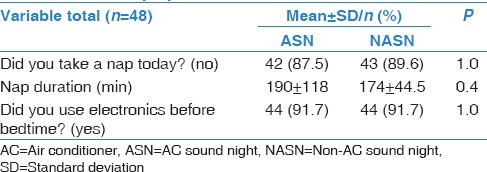
Sleep diary data
Table 2 shows the presleep routine during the AC sound nights (ASNs) and the non-AC sound nights (NASNs). A total of 91.7% (n = 44) used electronics before going to sleep, and the average room temperature was 21.5°C (19.8°C–23.2°C) during ASNs and 21.9°C (20.3°C–23.3°C) during NASNs. There was no significant difference between the duration of daytime naps before ASNs and NASNs. During ASNs, 77.1% of participants reported waking up once or more, of which 50% detailed that the wake duration lasted less than 5 min. On the contrary, during NASNs, 41.7% of participants reported waking up once or more, of which 20.8% detailed that the wake duration lasted less than 5 min.
Table 2.
Presleep questionnaire
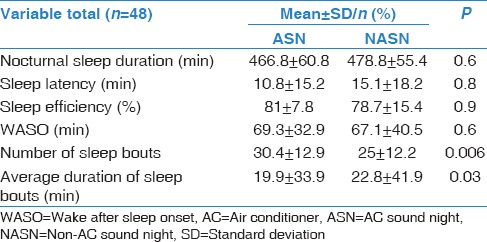
Actigraphy data
The results of the actigraphy are shown in Table 3. The mean sleep duration was not significantly different between ASNs and NASNs (P = 0.7), with a mean of 466.8 ± 60.8 min for ASNs and 478.8 ± 55.4 min for NASNs. In addition, the sleep-onset latency was not significantly different between ASNs and NASNs (P = 0.8), with a mean of 10.8 ± 15.2 min for ASNs and 15.1 ± 18.2 min for NASNs. Sleep efficiency was 81% ± 7.8% for ASNs and 78.8% ± 15.4% for NASNs (P = 0.9). WASO was 69.3 ± 32.9 min for ASNs and 67.1 ± 40.5 min for NASNs (P = 0.6). The number of sleep bouts was significantly higher (30.4 ± 12.9 vs. 25 ± 12.2, P = 0.006) and the average duration of sleep bouts was significantly lower (19.9 ± 33.9 min vs. 22.8 ± 41.9 min, P = 0.03) during ASNs compared to during NASNs, which indicates that sleep quality was lower during ASNs.
Table 3.
Actigraphy sleep data measured during air conditioner sound nights and non-AC sound nights
Discussion
The present study is the first study that objectively measured the effect of AC sound on sleep, in healthy young adults, while controlling for other factors that could affect sleep such as room temperature and light intensity. In contrast to our hypothesis and to one-third of participants' beliefs, the results indicated that AC sound had no significant effect on sleep latency, duration, and efficiency. Objective actigraphy measurements of sleep latency, efficiency, and duration were approximately the same for both nights. In fact, the number of sleep bouts and the average duration of sleep bouts indicated that sleep quality was better during NASNs. These results oppose the general public's common belief that AC sound improves sleep.[17]
Sleep is a sensitive process, which can be disturbed by environmental and external cues,[24] such as the characteristics of the sleep environment, including noise, light, and ambient temperature. Multiple animal studies have suggested that sleep disturbance can occur due to different types of noise. A previous animal study revealed that continuously exposing rabbits to 78 dB white noise, a constant noise characterized by an equal distribution of frequencies, leads to the disruption of REM sleep, which is an important sleep stage.[25] In fact, REM sleep episodes' duration and frequency increased after the white noise was stopped.[25] However, previous studies looking at the effect of white noise on sleep quality have not been consistent. Moreover, most previous studies that have assessed the effects of white noise on sleep have not assessed sleep quality objectively and have used a small sample size.
Our results are in line with those from two studies that assessed sleep quality objectively and reported no improvement in sleep quality during white noise exposure. In well-designed study, Scott assessed sleep architecture in eight subjects who were monitored for eight consecutive nights in a sleep laboratory during which subjects were exposed to 93 dB white noise or no noise.[13] This study showed that the duration of stages N1 and N2 of non-REM sleep was increased, while the duration of REM sleep was decreased, during noise nights, indicating a decreased quality of sleep during noise nights. The second study assessed the effects of white noise on sleep architecture in 12 patients and revealed that sleep microstructure was negatively affected by a 45 dB white noise.[15] However, the ambient noise during the last study never exceeded 27 dB.[15]
On the other hand, some studies have reported beneficial effects of white noise on sleep. A study that subjected 30 patients, who were recovering from coronary bypass surgery, to white noise reported that subjective sleep quality was higher in these patients compared to 30 matched controls who were not subjected to white noise.[16] Another small study subjected neonates to white noise ranging from 67 to 72.5 dB.[14] The investigators reported that 80% of neonates fell asleep within 5 min after white noise administration, compared to only 25% of controls.[14] However, both studies did not objectively assess sleep parameters and sleep quality, thus implying that it is difficult to accurately interpret their results. A recent study assessed the effects of normal environmental noise (40.1 dB) compared to broadband sound administration, uniformly distributed in the room by two speakers (46.0 dB), on sleep quality in 18 subjects.[11] Sleep architecture was monitored via two overnight sleep studies which took place approximately 1 week apart. Broadband sound administration significantly reduced sleep-onset latency by 38%, compared to normal environmental noise.[11] Nevertheless, the beneficial effect of broadband sound administration on sleep-onset latency was not seen in sleep architecture. In fact, broadband sound administration seemed to provoke a mild reduction of REM sleep and mild increase of stage N2 sleep (P = 0.06), which suggests that broadband sound administration could potentially lead to a decline in sleep quality.
The discrepancies found between the studies mentioned above might be explained by the fact that some of these studies did not use objective tests to assess sleep duration and quality. In addition, different studies used different sound pressures. Therefore, it is possible that a higher sound pressure and perhaps a higher perceived noise intensity might have detrimental effects on sleep architecture and sleep quality. Another plausible explanation is that the distribution of noise sounds and the distance of the sound source from subjects was different in each study.[11] For example, in the study by Messineo et al., the filtered noise was homogeneously diffused in the room (not localized), and it had been customized with specific features to fit the room acoustics.[11] In our study, however, we tried to simulate an AC sound meaning that the source of the sound was fixed only on one side.
One of the strengths of this study is that objective measures were used to assess sleep parameters. In addition, we monitored other factors that may also affect the measured sleep parameters, such as room temperature, light intensity, and naps, to make sure that these factors did not change during both experimental nights. Nevertheless, the study has a few limitations that need to be addressed. First, our study sample was only composed of young adults, meaning that these results cannot be extrapolated to other age groups since sleep perception and sleep quality change with age.[26,27] Future studies should assess the effect of AC sound on different age groups and patients with sleep disorders such as insomnia. Second, although clear instructions were given to the participants on how to reduce background noises at home during the experimental period, background noises were not objectively monitored. Nevertheless, we included participants with low background noise. Third, although actigraphy is an accepted methodology to investigate sleep/wake cycles, it is less sensitive to assess awakenings and arousals. Fourth, sleep monitoring for two nights may not be enough to detect changes in sleep; therefore, future studies should to monitor sleep for longer periods.
Conclusion
Our study is the first experimental study that assesses the effects of AC sound on sleep while monitoring for changes in light and room temperature. Our results show no positive effect of AC sound on sleep. Considering that the world is becoming more urbanized which is leading to increased usage of ACs in homes, our results highlight the necessity for further studies to investigate the detrimental effects that AC sound may have on sleep and other health aspects.
Financial support and sponsorship
The study was supported by College of Medicine Research Center, Deanship of Scientific Research, King Saud University Project, Saudi Arabia.
Conflict of interest
There are no conflicts of interest.
Acknowledgments
We are thankful to Tareq Aljurf for helping with the preparation and structuring of the research and Todd Morr, the developer of the White Noise Pro application who helped us with the settings and the stabilizing of the sound intensity used in this study. We thank the Deanship of Scientific Research and RSSU at King Saud University for their technical support.
References
- 1.Buysse DJ. Sleep health: Can we define it? Does it matter. Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krueger JM, Obal F., Jr Sleep function. Frontiers in bioscience: A journal and virtual library. 2003;8:d511–9. doi: 10.2741/1031. [DOI] [PubMed] [Google Scholar]
- 3.Benington JH. Sleep homeostasis and the function of sleep. Sleep. 2000;23:959–66. [PubMed] [Google Scholar]
- 4.Portas CM, Krakow K, Allen P, Josephs O, Armony JL, Frith CD, et al. Auditory processing across the sleep-wake cycle: Simultaneous EEG and fMRI monitoring in humans. Neuron. 2000;28:991–9. doi: 10.1016/s0896-6273(00)00169-0. [DOI] [PubMed] [Google Scholar]
- 5.Muzet A. Environmental noise, sleep and health. Sleep Med Rev. 2007;11:135–42. doi: 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Farokhnezhad Afshar P, Bahramnezhad F, Asgari P, Shiri M. Effect of white noise on sleep in patients admitted to a coronary care. J Caring Sci. 2016;5:103–9. doi: 10.15171/jcs.2016.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pedemonte M, Peña JL, Torterolo P, Velluti RA. Auditory deprivation modifies sleep in the guinea-pig. Neurosci Lett. 1997;223:1–4. doi: 10.1016/s0304-3940(97)13392-4. [DOI] [PubMed] [Google Scholar]
- 8.Wetter TC. Article reviewed: Auditory processing across the sleep-wake cycle: Simultaneous EEG and fMRI monitoring in humans. Sleep Med. 2001;2:355–7. doi: 10.1016/s1389-9457(01)00103-4. [DOI] [PubMed] [Google Scholar]
- 9.Zwislocki JJ. Masking: experimental and theoretical aspects of simultaneous, forward, backward, and central masking. In: Carterette EC, Friedman MP, editors. Handbook of Perception. New York, San Francisco, London: Academic Press; 1978. pp. 238–336. [Google Scholar]
- 10.Delgutte B. Physiological models for basic auditory percepts. In: Hawkings HL, McCullen TA, Popper AN, Fay RR, editors. Auditory computation. New York, Berlin, Heidelberg: Springer; 1996. pp. 157–220. [Google Scholar]
- 11.Messineo L, Taranto-Montemurro L, Sands SA, Oliveira Marques MD, Azabarzin A, Wellman DA, et al. Broadband sound administration improves sleep onset latency in healthy subjects in a model of transient insomnia. Front Neurol. 2017;8:718. doi: 10.3389/fneur.2017.00718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stanchina ML, Abu-Hijleh M, Chaudhry BK, Carlisle CC, Millman RP. The influence of white noise on sleep in subjects exposed to ICU noise. Sleep Med. 2005;6:423–8. doi: 10.1016/j.sleep.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Scott TD. The effects of continuous, high intensity, white noise on the human sleep cycle. Psychophysiology. 1972;9:227–32. doi: 10.1111/j.1469-8986.1972.tb00757.x. [DOI] [PubMed] [Google Scholar]
- 14.Spencer JA, Moran DJ, Lee A, Talbert D. White noise and sleep induction. Arch Dis Child. 1990;65:135–7. doi: 10.1136/adc.65.1.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terzano MG, Parrino L, Fioriti G, Farolfi A, Spaggiari MC, Anelli S, et al. Variations of cyclic alternating pattern rate and homeostasis of sleep organization: A controlled study on the effects of white noise and zolpidem. Pharmacol Biochem Behav. 1988;29:827–9. doi: 10.1016/0091-3057(88)90218-3. [DOI] [PubMed] [Google Scholar]
- 16.Williamson JW. The effects of ocean sounds on sleep after coronary artery bypass graft surgery. Am J Crit Care. 1992;1:91–7. [PubMed] [Google Scholar]
- 17.The National Sleep Foundation. Bedroom Poll. 2012. [Last accessed on 2018 Feb 18]. Available from: https://sleepfoundation.org/sites/default/files/bedroompoll/NSF_Bedroom_Poll_Report.pdf .
- 18.Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139:1514–27. doi: 10.1378/chest.10-1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morr T. TMSOFT White Noise. 2017. [Last accessed on 2016 Oct]. Available from: https://www.tmsoft.com/white-noise/
- 20. [Last accessed on 2016 Jan 20];Information W.W.C. Weather in Riyadh, Saudi Arabia. 2016 [Google Scholar]
- 21.Weiss AR, Johnson NL, Berger NA, Redline S. Validity of activity-based devices to estimate sleep. J Clin Sleep Med. 2010;6:336–42. [PMC free article] [PubMed] [Google Scholar]
- 22.Spina G, Spruit MA, Alison J, Benzo RP, Calverley PM, Clarenbach CF, et al. Analysis of nocturnal actigraphic sleep measures in patients with COPD and their association with daytime physical activity. Thorax. 2017;72:694–701. doi: 10.1136/thoraxjnl-2016-208900. [DOI] [PubMed] [Google Scholar]
- 23.Tamaki M, Nittono H, Hayashi M, Hori T. Examination of the first-night effect during the sleep-onset period. Sleep. 2005;28:195–202. doi: 10.1093/sleep/28.2.195. [DOI] [PubMed] [Google Scholar]
- 24.Ehlers CL, Frank E, Kupfer DJ. Social zeitgebers and biological rhythms. A unified approach to understanding the etiology of depression. Arch Gen Psychiatry. 1988;45:948–52. doi: 10.1001/archpsyc.1988.01800340076012. [DOI] [PubMed] [Google Scholar]
- 25.Khazan N, Sawyer CH. “Rebound” recovery from deprivation of paradoxical sleep in the rabbit. Proc Soc Exp Biol Med. 1963;114:536–9. doi: 10.3181/00379727-114-28725. [DOI] [PubMed] [Google Scholar]
- 26.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. [Meta-Analysis Research Support, Non-U.S. Gov’t] 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 27.Grandner MA, Martin JL, Patel NP, Jackson NJ, Gehrman PR, Pien G, et al. Age and sleep disturbances among American men and women: data from the U.S. Behavioral Risk Factor Surveillance System. Sleep. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] 2012;35:395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]


