Abstract
Introduction:
Patients with psychosis often seek treatment at a later date after the onset of illness. There are a multitude of factors behind the treatment delay in these patients, reduction of this delay will help in better prognosis of these patients.
Materials and Methods:
A cross sectional study was conducted to understand the various reasons responsible for treatment delay in patients with psychosis. 25 subjects were selected by purposive sampling and their family members were interviewed. Qualitative analysis was carried out to identify various factors.
Results:
Reasons for treatment delay were at several levels like illness related, patient related, treatment related, family related factors. However the most common themes among these were unawareness of illness, explanatory models of illness, stigma, financial constraints. Other themes like relation of symptoms with premorbid personality, life events, absence of paternal support were also unfolded in the current study.
Conclusions:
There is significant delay between onset of psychosis and treatment seeking. Several factors are responsible for treatment delay in patients with psychotic illness. However they vary depending upon the socio-cultural background of the patient and their family members. Hence the interventions devised towards reducing the delay should be individualised.
Keywords: Duration of untreated psychosis, patients with psychosis, treatment delay
INTRODUCTION
Patients with psychiatric disorders are the ones who are frequently underdiagnosed and undertreated. Although this applies to common mental disorders too, patients with psychotic disorders are more commonly undertreated or not treated. Moreover, those who seek treatment often have a delay between the onset of symptoms/syndrome and the initiation of adequate psychiatric treatment. The reasons behind not getting treated or getting treated at a later date are varied and diverse. Delay in treatment seeking is not only influenced by the factors such as stigma, societal attitudes, unawareness, and underdiagnosis but also is colored by the sociocultural background of the patient. All these together prolong the duration of untreated psychosis (DUP). As already replicated in many studies, the longer the DUP, the poorer is the quality of life and outcome.[1]
The prevention of psychiatric disorders is gaining more relevance nowadays. Reducing the DUP by early identification and treatment is an important measure of secondary prevention of psychotic illnesses. Thus, response to antipsychotics can be improved by initiating treatment in the “critical period.”[2] Achieving this requires a multipronged approach as it involves dealing with delay with help-seeking on the one hand and delay in referral on the other hand. Another component of delay in treatment is delay in recognition of the diagnosis. While delay in recognition lies completely with the expertise, skills, and knowledge of a psychiatrist, former types are more widespread and difficult to handle.[3]
Delay in help-seeking is the first step in this pathway of care. One of the highly influential studies done till date, the Treatment and Intervention in Psychosis Study (TIPS), demonstrated the impact of community and family education in reducing treatment delay.[1] Similarly, stigma associated with mental illness has been proven as a culprit for delay in treatment by many studies.[4] The other diverse factors which cannot be neglected, especially in Indian settings, are the influence of religiosity or spirituality, cultural factors, and shared models of illness. All these have a direct impact on treatment delay in these patients.[5,6]
Overall, there are several hurdles to be crossed before a patient with mental illness actually seeks treatment. Finding out these reasons can help both the patient and the family members by reducing the morbidity and burden associated with untreated psychosis and thereby improving the overall prognosis of these patients. Although studies till date have examined certain correlates of treatment delay, most of them have identified stigma and poor awareness about illness as factors of concern. The influence of other factors is unclear and an overall picture is not portrayed. Moreover, the majority of studies done till now have been quantitative in nature, with only a few qualitative studies which have tried to explore the factors behind the delay in treatment.[7] Qualitative research is more useful in detecting subtle influences in treatment delay and portraying a broader picture of the entire process. This led to the current study, which sought to identify reasons for delay in treatment seeking using a qualitative method of investigation.
MATERIALS AND METHODS
This is a hospital-based cross-sectional study, conducted at the Department of Psychiatry (outpatients and inpatients) of the Raipur Institute of Medical Sciences in India. It is a 350-bed hospital-cum-medical college, which caters to the needs of nearby villages apart from the city of Raipur. Twenty-five patients with nonaffective psychotic disorders (schizophrenia, schizoaffective disorder, or psychotic disorder – not otherwise specified) and their family members participated in this study. The diagnoses of schizophrenia, schizoaffective disorder, or psychotic disorder – not otherwise – were confirmed using the Mini-International Neuropsychiatric Interview-Plus version (MINI-Plus).[8] Family members aged between 18 and 60 years, who are able to understand and speak Hindi, and those who were in regular contact with patients (i.e., meeting the patient at least once in a month) were included in the study. Patients with organic mental disorders, mental retardation, or seizures and those with other comorbid Axis I disorders were excluded from the study. Written informed consent was taken from all the participants, and ethical clearance was obtained from the Institutional Ethics Committee before the conduct of the study.
Demographic information of both patient and family members was recorded using standard format of sociodemographic profile sheet. DUP is defined as the number of months from the onset of positive psychotic symptoms until the start of proper treatment. MINI-Plus was used in the patients to ascertain the diagnostic category (schizophrenia, schizoaffective disorder, or psychotic disorder – not otherwise specified). A semi-structured clinical interview was conducted in family members to assess the various factors responsible for the delay in treatment seeking. Open-ended questions were utilized to probe for potential determinants of treatment delay. All the family members were asked a set of questions such as: What led to the delay in the treatment of the patient? What did they think was the reason for the illness? What were the reasons for seeking treatment now? Verbatim was recorded using audiotape.
Qualitative analysis
We used content analysis for the purpose of this study. The recorded responses were translated into English; all the information which was related to personal identity of the patient was removed, and clean transcripts were made. Transcripts made in English were assessed separately by both the investigators (MSS and MD). Each investigator generated separate categories and themes after reading the transcripts word by word. Theme generation was continued till the point of saturation was reached, and no further themes could be generated. Only categories and themes mutually agreed upon by both the investigators were used in the results as this would increase their validity.
RESULTS
Sociodemographic profile
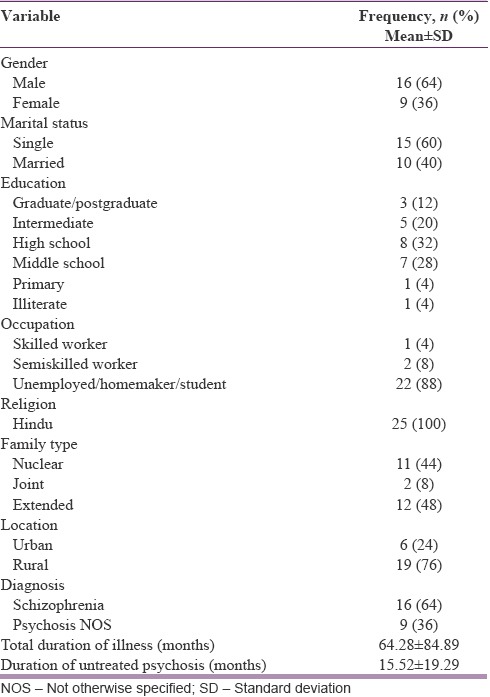
Most of the patients them were male (64%), single (60%), or unemployed/homemakers by occupation and belonged to rural locations (76%). The majority had studied up to middle school-intermediate level (80%). Nuclear and extended families were equally distributed among the patients. About 64% of patients were diagnosed as having schizophrenia whereas the rest were diagnosed as psychotic disorder – not otherwise specified. Mean total duration of illness was 64 months, and the DUP was 15 months [Table 1a].
Table 1a.
Sociodemographic profile of patients
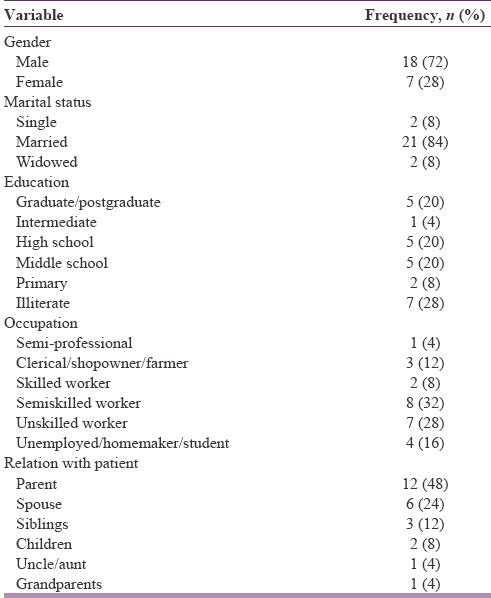
Most of the family members were males (72%), were married (84%), and educated up to middle school graduation levels (84%); 60% of the family members were either semiskilled or unskilled workers. Family members were parents (48%), spouses (24%), siblings (12%), children (8%), uncle/aunts (4%), or grandparents (4%) of patients [Table 1b].
Table 1b.
Sociodemographic profile of family members
Findings of qualitative analysis
Based on the content analysis technique used, we have generated certain categories of factors responsible for treatment delay and generated themes in each category.
Categories responsible for treatment delay in patients with psychosis based on the current study are:
Illness-related factors
Patient-related factors
Treatment-related factors
Family-related factors
Other factors.
Illness-related factors
Unawareness of illness
Most of the family members that we interviewed had no knowledge about the patient's illness at the beginning. It was one of the most commonly repeated themes in our analysis.
Patient 1# “When he fell ill for the first time, we were wondering why he was behaving in such a way. We used to think why he was getting irritable. Though he used to eat and sleep well he used to interact very less with family members. We had no clue of what was happening to him.”
Patient 3# “……She couldn’t sleep at all for the whole night. She used to stare at the roof for prolonged periods of time. At that time we didn’t have knowledge about this problem. But when she started to break household objects, abuse us verbally and physically then we thought that there is something wrong with her.”
Patient 4# “When her symptoms started we couldn’t know. We couldn’t understand that it's an illness for several years.”
Patient 11#“No one in our house had this kind of symptoms anytime before, so we were unable to recognize the problem in the beginning.”
Patient 13# “She was absolutely fine and was reading. We don’t know what happened to her. All of a sudden she started to hit us, hurl abuses at us and would tear her clothes. She stopped going to the college. But we didn’t get her treated for about a month or so. Because we didn’t know that some ‘mental illness’ can present like this.”
Explanatory models of illness
Supernatural causation of illness
After unawareness of illness, supernatural causation of illness was the commonly recurring theme. Most of the patient's family members felt that changes in patient's behavior were due to the effect of black magic, evil spirits, and evil eye. Few examples are provided here to substantiate the finding.
Patient 5# “…We thought it was due to intrusion of a ghost into her body. We took her to various faith healers to get rid of the ‘evil’ inside her. There was not much of improvement.”
Patient 9# “He has been captured by ‘Zinn’. All of a sudden he became weak and fragile, stopped eating food properly. He was not able to manage himself properly.”
Patient 13# “….We took her to ‘baba’ and got the rituals in order to get rid of the demonic possession. But she didn’t improve with that.”
Patient 12# “We took him to an ayurvedic doctor initially. Later we thought that it's something related to witchcraft. Then we got the rituals accordingly as suggested by the priests. But he never improved.”
Patient 15# “Someone told us that she was under the effect of an evil spirit. We took her to a faith healer, who also diagnosed that she is under the effect of black magic. When there was no improvement with treatment from one faith healer we took her to a different one.”
Physical causation of illness
Although the majority attributed their ward's illness to supernatural causation, few of them still had physical causation theories in their mind. As can be seen in the examples given below, few of the family members thought that the patient's behavior was due to fever or jaundice. However, with a close observation, we can conclude that their attribution was due to temporal correlation with the symptoms and physical illness or presentation of symptoms similar to that of a common physical illness like loss of appetite in jaundice.
Patient 3# “…This illness began 5–6 years back. First she developed fever for 4–5 days, then she couldn’t sleep at all for the whole night. …Then we showed her to physician in Mahasamund. He gave some medicines for fever but she continued to be ill.”
Patient 20# “But when she refused to eat and wasn’t feeling hungry we thought it might be due to jaundice. Then we took her to a physician.”
Stigma associated with illness
Stigma and mental illness go hand in hand. In India, people avoid consulting psychiatrists for the fear of stigma. From our analysis given below, we can clearly see how people still discriminate patient with mental illness either by labeling or social distancing. From the below examples, we can note how people portray a person with mental illness in their minds.
Patient 1# “…Even the villagers didn’t know what it was. They thought he just became afraid and there is nothing much to worry. They used to make fun of him saying ‘coward’ has come”-subtheme-labeling.
Patient 7# “When the problem started he used to run away from home. Neighbors suggested me to tie him up at home. His wife left him after having 3 sons because of this problem. He used to trouble us a lot”-subtheme-social distancing/isolation.
Patient 25# “For the 1st month we didn’t understand what's wrong with her. Thereafter when we saw her behavior we felt that she was almost doing like a ‘mental patient’”-subtheme-labeling.
Patient 12# “He (husband) was ill before marriage, but was not receiving any treatment. I never knew that ‘mental patients’ behave so”-subtheme-labeling.
Patient-related factors
Underlying premorbid personality
Another finding which was evident in the category of patient-related factors for delay in treatment seeking was the underlying personality of the patient before the illness. Family members confused the symptoms with premorbid traits of personality leading to delay in identification of symptoms and treatment.
Patient 8# “At that time he used to beat everyone in the house. As he was ‘angry’ by nature from childhood, we thought it's just an exaggeration of the same”-subtheme-normalcy.
Patient 22# “He (husband) started to remain irritated at work place and would complain about the happenings there. We thought that some of his colleagues might have done something or scolded him for not working. So we didn’t pay much heed to his complaints”-subtheme-psychopathology related to patient's sociocultural background.
Symptoms at the onset
It was reported by few of the family members that when the patient had predominant negative symptoms at the onset of illness or in the prodromal phase, they were likely to be neglected leading to delay in the treatment.
Patient 5# “We never knew that this was an illness. We took her to various faith healers to get rid of the ‘evil’ inside her…. She used to sit alone, wouldn’t disturb anyone, neither would interact with us. It was easy to manage her at home. Doctor we didn’t get her treated for 2 ½ years into her illness”-subtheme-absence of positive symptoms/aggression and illness not intruding other's life.
Patient 24# “When her illness began she used to stay quiet and self-absorbed. She used to sit alone throughout the day. We tried to console her, reassure and counsel her. But nothing worked. But 1 day all of a sudden she consumed pesticide and tried to commit suicide. Then we admitted her in a hospital, where a psychiatrist saw her and told us that she has ‘mental illness’”-subtheme-absence of danger to self.
Onset along with life events
One caregiver opined that they had assumed that the symptoms were the result of a significant life event.
Patient 18# “We started him on treatment after 2–3 months of his illness. Because we didn’t understand what that was all about. And around the same time he took his retirement, so we thought that he was feeling lonely and that's why behaving so”-subtheme-normal life course.
Poor insight/uncooperative patient
Another important finding from our study with respect to patient-related factors for delay in treatment was patient's poor insight and uncooperativeness for treatment. Poor insight about illness is not only responsible for poor treatment adherence but also delays treatment seeking as elicited.
Patient 7# “We kept taking him to different faith-healers thinking that he is under the influence of a spirit. His anger was so severe that it was difficult for us to take him for treatment.”
Patient 21# “How would we know initially about what happened to him. How could we take him to a doctor, he would resist anything said and would try to beat everyone.”
Patient 25# “We wanted to take her (wife) to the doctor but she was never willing to come. She always said she has no illness. Used to tell us that am fine. She never could be convinced for a visit to a doctor. Today we have called few of our relatives and forced her, so she couldn’t resist.”
Impaired functioning
Most patients of psychosis develop impaired functioning sooner or later in the course of illness. As seen from the sample below if the patient continues to function normally, especially in the earlier stages of illness, it is likely that the symptoms are often ignored leading to delay in treatment seeking.
Patient 8# “…Apart from that he used to do all the work allotted to him so we never bothered to get him treated. But since when he stopped working then we thought that something is wrong with him. Then we took him to a local doctor.”
Family-related factors
Shared societal beliefs
If the explanatory models of illness assumed by family members are also shared by the society they live in, it gives much strength to their beliefs and guides the pathway to care. From the samples provided below, we can surmise that shared beliefs about illness and various magico-religious attributions are reasons for delay in a few instances.
Patient 6# “Our neighbors gave suggestions that someone did black magic on her and guided us as to who will be the correct faith healer. I (husband) kept taking her from one faith healer to the other depending upon their advise. And this process continued for few months”-subtheme-interdependence.
Patient 17# “…Because he was turning weak and fragile and my (mother's) daughter also started to get weak. Her daughter also fell ill at that same time in the house. They visited my house after several years. Immediately after coming, all of them fell ill. So I thought it might be the effect of the evil eye of our neighbors as they were jealous about my family.”
Patient 3# “…We thought that he has been possessed by an ‘evil spirit’, because we didn’t know about this problem. We took him to Baba, because even our neighbors have confirmed this belief of ours”--subtheme-interdependence.
Cultural constraints
Cultural factors not only help in differentiating normal patterns of thought and behavior from psychopathology but also can cause hindrance in seeking treatment for mental illnesses. This is illustrated by the following transcript.
Patient 10# “But because we belong to “Marwadi” background, I was not allowed to get out of home, neither was I permitted to remove the veil. Till the time my mother in law survived I couldn’t take him out for treatment.”
Lack of support from significant others or poor social support
Social support is needed for patients with psychiatric illness from the very first stage of their illness till the stage of recovery and reintegration. In the samples provided below, caregivers mentioned that lack of social support, particularly lack of paternal support, and being the sole caregiver were significant factors responsible for delayed treatment.
Patient 13# (sister) “….We don’t have father, lost him at very young age, mother works to earn the expenses. So we couldn’t afford to take her by ourselves for treatment”-subtheme-loss of parent.
Patient 21# “….There was no one at home to come along with us. His father expired several years ago. With much difficulty I took him to railway station, then he ran away from there”-subtheme-loss of parent.
Patient 4# “…. Since 1992 she has been troubling me (father). She had 4 children by that time. There was no one else to take care of her. I had to take care of the children. Look after their studies, food and everything. There was no support from her in-laws side.”
Patient 6# “There was no improvement with faith healing. Then I accepted my failure and sat at home, because I was alone and had to look after the kids too. The kids are also very small. Entire family depends upon my earnings acquired on a daily basis”-subtheme-sole caregiver.
Treatment-related factors
Poor knowledge of general physicians about psychiatric disorders and poor referral
In the samples below, we can see that doctors apart from psychiatrists due to their own belief in magico-religious proceedings and unawareness of psychiatric illness combined with poor referral lead to delay in treatment seeking in some of our patients.
Patient 20# “One doctor near our home also told us that it's the effect of black magic and asked us to continue with the religious proceedings.”
Patient 22# “But when he started to hurl abuses, use foul language at family members we thought there was something wrong. We took him to a general physician for 2–3 times, but he couldn’t find out what's wrong with the patient.”
Patient 4# “When the symptoms worsened and it was difficult to manage her, I took her to a doctor. Then he told us to get scan of the brain and told it's a neurological illness. But she didn’t improve.”
Misconceptions about the effects of medication
Another factor that was found to be responsible for treatment delay was the patients’ misconceptions about medications.
Patient 12# “We were afraid that the medicines you give might cause side effects and might be habit forming. But as his symptoms continued we had to visit a doctor.”
Others
Financial constraints
Many caregivers/family members told us that their poor financial status was a significant contributor of delay particularly if the patients had negative symptoms. This was because they had to choose a priority between running the family and getting the patient treated.
Patient 11# “Though some of our neighbours told us to seek treatment from the doctor, we couldn’t do that for quite some time because we were running short of money. Her husband didn’t take initiative to get her treated, he left her with me (father).”
Patient 3# “Also we had financial problems at that time because of which we couldn’t afford him to take to a doctor.”
Patient 4# “I had to look after her and her children and bear all the expenses. It was difficult for me to get her treated in that situation. When the symptoms worsened and it was difficult to manage her, I took her to a doctor.”
Patient 5# “We took her to various faith healers to get rid of the ‘evil’ inside her. There was not much of improvement. Our family was in huge financial crisis at that time when she fell ill. It was easy to manage her at home.”
Patient 6# “Entire family depends upon my earnings acquired on a daily basis. I had no money and was not guided properly neither supported by anyone. Then one of my neighbor told me about your hospital. Also that the treatment will be free of charge, so I gained courage and brought her (wife) here.”
DISCUSSION
This study tried to identify the various factors responsible for treatment delay in patients with psychosis. Keeping in view of the sociocultural background of people from Central India where the belief systems and pathways of care are centered around the explanatory models and shared beliefs, we thought of determining all the factors behind treatment delay in order to design intervention strategies accordingly. We found out that factors responsible for delay can be categorized as patient-related factors, illness-related factors, treatment-related factors, family-related factors, and other factors.
We found out that the most common cause of delay was unawareness about the illness, its causes, and treatment. This was in line with the handful of qualitative studies done in India on this subject.[9,10]
Another important and commonly found reason was the shared beliefs/supernatural causation of illness which was in line with current studies.[11,12,13,14] The result was expected considering the background of the area in which the study took place. However, one surprising result we found was that few of the family members also had biological explanation to the patient's symptoms. This result was in sharp contrast to that of a recent study conducted in Bilaspur where supernatural causations for mental illness were more prevalent.[15] Hence, it can be stated that there is a slow but gradual change in belief systems of the population.
Other causes found were stigma about being labeled or social isolation with respect to mental illness. This finding of stigma being responsible for treatment delay and nonadherence has been replicated in number of earlier studies.[1,7,11,16,17,18] Lack of social support was also related to delay in help-seeking. However, this became a significant problem if the family member was the sole caregiver or patients had lost their fathers early.
Symptoms at the onset of illness and premorbid personality were the patient-related factors associated with treatment delay found in our study. Although negative symptoms and absence of violence at the onset have been shown to be factors responsible for delay in help-seeking in earlier studies,[19] the association with premorbid personality was a novel finding. To our knowledge, this is the first study where we found out that if the patient's personality presents in an exaggerated way, it is difficult to figure out the change as a means of illness. Another interesting finding in this area is if the patient's psychopathology is in line with the sociocultural background, it might lead to delay in identification. Patient's poor insight/uncooperativeness along with preserved functioning in the initial stages might lead to delay in care. Although the former finding about patient's poor insight and uncooperativeness was found by many studies in the existing literature, preserved functioning is another of our novel findings.
In the current study, we found that financial burden is one another factor which strongly influences the treatment seeking particularly of psychiatric disorders.[19,20] This finding has also been replicated in few studies. The last step for delay lies at the level of general physicians and other practitioners because of their poor knowledge and reluctance to refer patients to psychiatrists.
Our study was not without limitations. The predominantly rural background of the population might have affected the findings. Hence, the family members included in our study might not be representative of the whole population of family members with psychosis. As our center treats patients free of cost, it is highly likely that patients with preexisting financial burden might have turned up, leading to over-representation of this aspect in the factors responsible for treatment delay. Not all the patients included were of first-episode psychosis leading to retrospective recall bias in few of them.
The current study has identified various reasons responsible for prolonged DUP in patients. Although these reasons seem to be separate, they are interdependent and they interact in a complex way leading to the delay in treatment seeking. Interventions focused at each and every step need to be devised in further studies in order to overcome the barriers found. However, such interventions need to be individually tailored and culturally congruent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We sincerely acknowledge the patients and family members who participated in the study and provided us with their valuable inputs.
REFERENCES
- 1.Franz L, Carter T, Leiner AS, Bergner E, Thompson NJ, Compton MT, et al. Stigma and treatment delay in first-episode psychosis: A grounded theory study. Early Interv Psychiatry. 2010;4:47–56. doi: 10.1111/j.1751-7893.2009.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Judge AM, Perkins DO, Nieri J, Penn DL. Pathways to care in first episode psychosis: A pilot study on help-seeking precipitants and barriers to care. J Ment Health. 2005;14:465–9. [Google Scholar]
- 3.Norman RM, Malla AK, Verdi MB, Hassall LD, Fazekas C. Understanding delay in treatment for first-episode psychosis. Psychol Med. 2004;34:255–66. doi: 10.1017/s0033291703001119. [DOI] [PubMed] [Google Scholar]
- 4.Wrigley S, Jackson H, Judd F, Komiti A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Aust N Z J Psychiatry. 2005;39:514–21. doi: 10.1080/j.1440-1614.2005.01612.x. [DOI] [PubMed] [Google Scholar]
- 5.Grover S, Davuluri T, Chakrabarti S. Religion, spirituality, and schizophrenia: A review. Indian J Psychol Med. 2014;36:119–24. doi: 10.4103/0253-7176.130962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhikha AG, Farooq S, Chaudhry N, Husain N. A systematic review of explanatory models of illness for psychosis in developing countries. Int Rev Psychiatry. 2012;24:450–62. doi: 10.3109/09540261.2012.711746. [DOI] [PubMed] [Google Scholar]
- 7.Sadath A, Muralidhar D, Varambally S, Jose JP, Gangadhar BN. Caregiving and help seeking in first episode psychosis: A qualitative study. J Psychosoc Rehabil Ment Health. 2014;1:47–53. [Google Scholar]
- 8.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 9.Hasan AA, Musleh M. Barriers to seeking early psychiatric treatment amongst first-episode psychosis patients: A qualitative study. Issues Ment Health Nurs. 2017;38:669–77. doi: 10.1080/01612840.2017.1317307. [DOI] [PubMed] [Google Scholar]
- 10.Nallapaneni N, Lanka U, Paritala C. A cross sectional study of factors influencing duration of untreated psychosis in a tertiary mental health care institute. Int J Innov Res Dev. 2015;4:191–7. [Google Scholar]
- 11.Saravanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS, et al. Belief models in first episode schizophrenia in South India. Soc Psychiatry Psychiatr Epidemiol. 2007;42:446–51. doi: 10.1007/s00127-007-0186-z. [DOI] [PubMed] [Google Scholar]
- 12.Chadda RK, Agarwal V, Singh MC, Raheja D. Help seeking behaviour of psychiatric patients before seeking care at a mental hospital. Int J Soc Psychiatry. 2001;47:71–8. doi: 10.1177/002076400104700406. [DOI] [PubMed] [Google Scholar]
- 13.Grover S, Patra BN, Aggarwal M, Avasthi A, Chakrabarti S, Malhotra S, et al. Relationship of supernatural beliefs and first treatment contact in patients with obsessive compulsive disorder: An exploratory study from India. Int J Soc Psychiatry. 2014;60:818–27. doi: 10.1177/0020764014527266. [DOI] [PubMed] [Google Scholar]
- 14.Lahariya C, Singhal S, Gupta S, Mishra A. Pathway of care among psychiatric patients attending a mental health institution in central India. Indian J Psychiatry. 2010;52:333–8. doi: 10.4103/0019-5545.74308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naik SK, Pattanayak S, Gupta CS, Pattanayak RD. Help-seeking behaviors among caregivers of schizophrenia and other psychotic patients: A hospital-based study in two geographically and culturally distinct Indian cities. Indian J Psychol Med. 2012;34:338–45. doi: 10.4103/0253-7176.108214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanskanen S, Morant N, Hinton M, Lloyd-Evans B, Crosby M, Killaspy H, et al. Service user and carer experiences of seeking help for a first episode of psychosis: A UK qualitative study. BMC Psychiatry. 2011;11:157. doi: 10.1186/1471-244X-11-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCann TV, Lubman DI, Clark E. Responding to stigma: First-time caregivers of young people with first-episode psychosis. Psychiatr Serv. 2011;62:548–50. doi: 10.1176/ps.62.5.pss6205_0548. [DOI] [PubMed] [Google Scholar]
- 18.Iyer SN, Loohuis H, Pawliuk N, Joober R, Malla AK. Concerns reported by family members of individuals with first-episode psychosis. Early Interv Psychiatry. 2011;5:163–7. doi: 10.1111/j.1751-7893.2011.00265.x. [DOI] [PubMed] [Google Scholar]
- 19.Marthoenis M, Aichberger MC, Schouler-Ocak M. Patterns and determinants of treatment seeking among previously untreated psychotic patients in Aceh province, Indonesia: A qualitative study. Scientifica (Cairo) 2016. 2016 doi: 10.1155/2016/9136079. 9136079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grover S, Avasthi A, Chakrabarti S, Bhansali A, Kulhara P. Cost of care of schizophrenia: A study of Indian out-patient attenders. Acta Psychiatr Scand. 2005;112:54–63. doi: 10.1111/j.1600-0447.2005.00512.x. [DOI] [PubMed] [Google Scholar]


