Abstract
Exposure to trauma is consistently associated with co-occurrence of behavioral health disorders. Primary care settings are opportune places to screen for traumatic experiences and symptoms, as they are often the initial point of care for behavioral health concerns by the Alaska Native and American Indian (AN/AI) population. In this case study, we examine results dissemination activities at the SCF Research Department-hosted 2016 Alaska Native Health Research Forum (Forum) of a pilot study of a trauma-focused screening, brief intervention, and referral to treatment (T-SBIRT) process for AN/AI adults in primary care. Feedback included audience responses to the presentation delivered at the Forum and recommendations to guide future community dissemination of T-SBIRT results. Attendees (N = 31) found the presentation clear, interesting, and included the right amount of detail. Four broad dissemination themes were identified in discussion groups: 1) share results with everyone; 2) share results in ways that reach all AN audiences; 3) provide a summarized status update at each stage of the study; and 4) use results to improve care for trauma and related symptoms.
INTRODUCTION
Exposure to trauma is consistently associated with co-occurrence of behavioral health disorders, suicidal behaviors, chronic disease risk factors, and an increase in health care service utilization (Beals et al., 2005; Goldstein et al., 2016; LeBouthillier, McMillan, Thibodeau, & Asmundson, 2015; Neria, Nandi, & Galea, 2008; Schnurr, 2015). AN/AI people experience higher rates of intergenerational trauma, interpersonal violence (Duran et al., 2004; Duran et al., 2009; Ehlers, Gizer, Gilder, & Yehuda, 2013; Evans-Campbell, Lindhorst, Huang, & Walters, 2006; Libby et al., 2005; Malcoe, Duran, & Montgomery, 2004; Manson, Beals, Klein, Croy, & Team, 2005; Saylors & Daliparthy, 2006; Wood & Magen, 2009), and unintentional injury than their non-AN/AI counterparts (Castrodale, 2007; Centers for Disease Control and Prevention, 2013; Edelman, Cook, & Saffle, 2010; Pollack, Frattaroli, Young, Dana-Sacco, & Gielen, 2012). Elevated prevalence leads to higher rates of individuals experiencing multiple traumas, which in turn increases the likelihood of lifetime risks for associated disorders (Beals et al., 2005). To improve trauma-informed care and prognosis is to detect traumatic experiences and post-traumatic stress disorder (PTSD) earlier (Substance Abuse and Mental Health Service Administration, 2014; Ursano et al., 2004). Primary care settings are opportune places to screen for PTSD symptoms given the relationship between traumatic experiences and medical and/or behavioral health problems. These settings also often serve as the initial point of entry for behavioral health care services.
Trauma Screening, Brief Intervention, and Referral to Treatment
In 2012, the University of Colorado Denver (UCD), SCF, and Cherokee Nation Health Services (CNHS) joined in a research partnership to 1) work with key stakeholders to expand current primary care efforts to include trauma-focused screening, brief intervention, and referral to treatment (T-SBIRT) in their respective health care settings and 2) to test the acceptability and feasibility of this new T-SBIRT process. The Center for American Indian and Alaska Native Health at UCD coordinated the study. SCF’s Anchorage Native Primary Care Clinic and CNHS’s W.W. Hastings Hospital in Tahlequah, Oklahoma were the primary care clinics. Combined, these sites serve nearly 200,000 AN/AI people.
A steering committee of key representatives from each site (two or more clinical providers and one administrator/program director) guided all stages of the research process. The steering committee developed mutually agreed upon guiding principles to: 1) build on the strengths of AN/AI cultures and communities; 2) use a collaborative, inclusive investigative approach; and 3) do no harm and use research as a positive change agent. Operating by these principles, the research team used an iterative research process commonly used in community-based participatory research (CBPR) projects with the following five distinct steps: 1) identify cycle goals, 2) develop measure/material, 3) collect data, 4) manage and analyze data, and 5) interpret results.
Process Development and Pilot Study
The research team met with stakeholders to develop a screening, brief intervention, and referral process for trauma among AN/AI adults at SCF and CNHS. The steering committee identified three stakeholder groups for primary data collection: health care providers in primary care and behavioral health clinics; administrative, clinical, and tribal leaders; and patients/customer-owners. SCF uses the term “customer-owner” to reflect how tribal members who receive health care services are also owners of the health care system (Gottlieb, 2013; Gottlieb, Sylvester, & Eby, 2008). Recruitment began in January 2013. Trained qualitative researchers completed 24, one-hour individual semi-structured interviews with providers and leaders and a two-hour focus group with 13 patients and customer-owners. The first round of interviews and focus groups included a combined SCF/CNHS sample of 37 participants; the second round included 33, with four lost to follow-up. In the first round, we asked about the types of trauma experienced in the community, the barriers to healing from trauma, personal and community aspects of strength and resilience, and existing services to treat individuals with symptoms related to trauma. In the second round, we presented participants with T-SBIRT pilot options and asked for recommendations about who should conduct trauma screenings, what questions should be asked in screenings, and ways to provide brief intervention and referral to care for those who need it. Data from each round of data collection were analyzed using a thematic network approach (Attride-Stirling, 2001) by researchers from each partnering organization. Using NVivo 9 (QSR International), three researchers coded one transcript to determine agreement on a priori codes based on question constructs then coded the remaining transcripts, meeting to discuss the coding schema, and later developing summaries from coded transcripts.
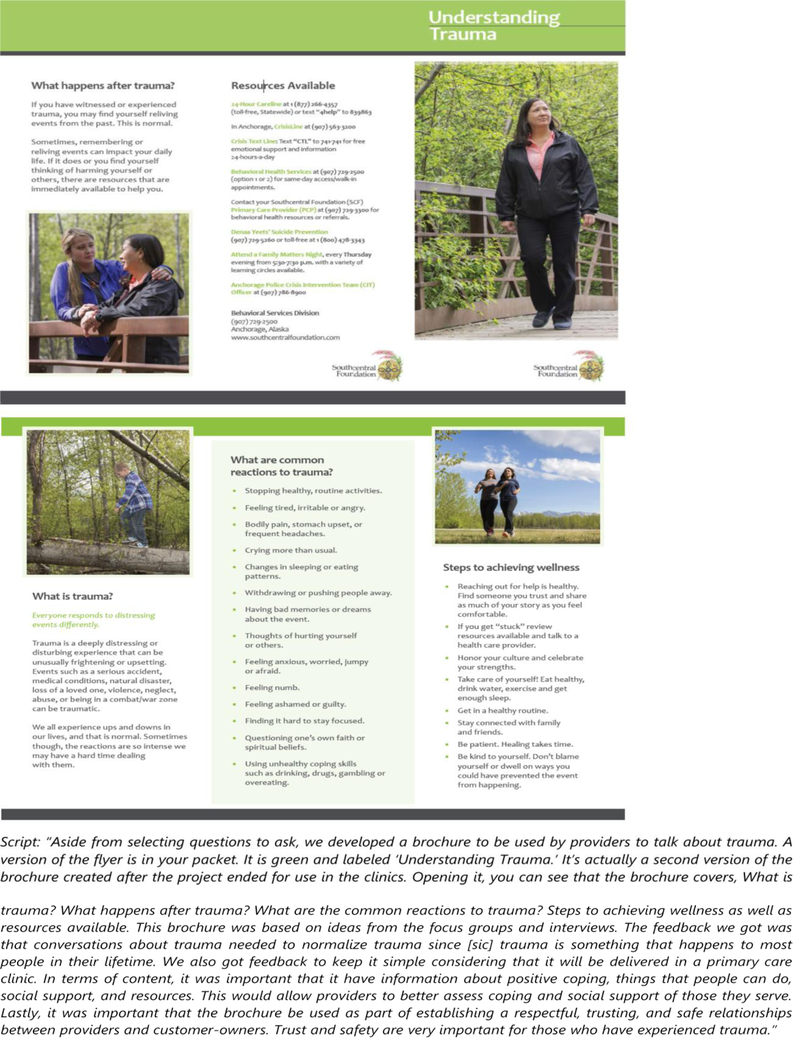
Four major themes emerged from the first round of data collection: 1) the nature of trauma in AN/AI communities, 2) barriers to healing from trauma, 3) trauma screening concerns, and 4) screening and brief intervention preferences. In the second round, we identified preferences for a trauma-screening instrument and screening process, and four themes for the development of the brief intervention brochure and process emerged: 1) normalization, 2) simplicity, 3) education/resource sharing, and 4) resiliency.
Researchers used this information to select screening questions, draft an intervention brochure, and create a T-SBIRT process in primary care. SCF and CNHS routinely conduct behavioral health screening in primary care for depression and substance use disorders. These screenings are conducted by trained certified medical assistants at SCF and by nurses at CNHS before the scheduled primary care provider visits. Both systems have behavioral health consultants (BHCs) integrated into primary care clinics to provide brief intervention and referral to additional treatment services such as behavioral health urgent response teams, behavioral health specialty care, and various wellness programs.
A pilot of the T-SBIRT process was completed at SCF and CNHS with a combined sample of 99 primary care outpatients. AN/AI adults who came to the clinic for regular provider appointments were invited to participate. If they agreed, after their appointment, they were asked the four-item Primary Care Posttraumatic Stress Disorder (PC-PTSD) Screen about trauma symptoms by a BHC. The BHC (SCF) or primary care provider (CNHS) reviewed the brief intervention brochure with participants, even those who had screened negative in case a family member had experienced trauma, or they were to experience trauma in the future. BHCs and primary care providers tailored the depth of their review of the brochure to participant responses to the screener or interest.
After reviewing the brochure, the BHC referred the participant to additional behavioral health services or scheduled a follow-up appointment, if needed. To determine the acceptability and feasibility of the T-SBIRT pilot process, researchers collected satisfaction surveys from all participants, conducted a medical records review of participant diagnoses and health service utilization in the one year before and three months after screening. A subsample of 41 participants completed a full 90-minute clinical interview (Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition) and a 36-item quality-of-life survey (World Health Organization Disability Assessment Schedule 2.0) to explore the diagnostic and predictive validity of the screening process.
Dissemination of Research Activities and Results
The steering committee guided dissemination efforts to customer-owners/patients; clinicians; and clinical, administrative, and tribal leaders. Tribal review bodies at SCF and CNHS approved all dissemination activities. An 18-page report of T-SBIRT development findings, along with the interview and focus group guides, were provided to tribal leadership at SCF in January 2014. Formal dissemination of the T-SBIRT development at CNHS has been limited to progress reports to the Cherokee Nation IRB and informal personal communication with interested providers and leaders. Posters on the development of the T-SBIRT process were presented at the 4th Alaska Native Health Research Conference in March 2014 in Anchorage, Alaska, and the 16th International Congress on Circumpolar Health in June 2015 in Oulu, Finland. Full findings of development efforts were published by Hiratsuka et al. (2016) in The Journal of Behavioral Health Services & Research.
Following the pilot, a one-page summary of preliminary information and actionable results were presented to SCF vice presidents and providers. The tri-fold brochure used in the pilot’s brief intervention was presented to an administrative quality improvement committee at SCF that focuses on trauma-informed services. That committee later adapted the tri-fold brochure for use in SCF’s health care system to bolster trauma-related services.
CASE STUDY
Event Overview
The purpose of the Forum was to: 1) provide an overview of health research among Alaska Native people; 2) obtain feedback on outreach and dissemination strategies used by the Alaska Native health system to communicate with community members on tribal health issues and events; and 3) engage in an open dialogue with the community through a showcase of three current health research projects conducted by the SCF Research Department. A total of 31 AN/AI adults attended the 3.5-hour Forum. A thorough description of the Forum, recruitment, attendee eligibility, registration, Forum activities, the audience response system (ARS), data collection, and data analysis are available in this special issue (see Hiratsuka et al., 2018, “Approach and Methods”).
Designing a T-SBIRT Presentation for a Community Audience
The iterative process of designing, drafting, and revising the T-SBIRT presentation for a community audience was extensive, considering the shortened length of the presentation. The presentation was initially drafted to be a 15–20 minute traditional academic presentation to a non-scientific community audience, or as a shortened version of a conference presentation, educational seminar, or colloquium. This type of presentation would allow for comparison of presentation styles with two other topics presented at the Forum. However, because the presentation was reviewed and revised by the SCF study team, most of whom are SCF customer-owners, it was clear that the traditional presentation was too long, not likely to be engaging, and too technical. Thus, the presentation was edited to target a community audience. The number of PowerPoint slides was reduced from 22, to 19, then to 15, and ultimately to 12 slides (Figure 1). Language about “screening, intervention, and treatment” was reduced and, in some instances, replaced with language such as “screen and care for people” to simplify language, to keep the presentation conversational, and to reflect the setting and use of the findings within the AN/AI health care setting.
Figure 1.
Example Slide with Presenter Script
As the presentation was revised with the customer-owner audience in mind, fewer direct results of the focus groups and interviews were included; rather, staff presented the end result of the qualitative inquiry—the methods of the pilot. Staff did not discuss the research project linearly, as one might present a traditional research project in a conference or academic setting; SCF staff changed the order of the presentation so that the final products of the pilot process (e.g., screening questions, the brochure as an intervention material, and evaluation method) were shown after the description of the problem, leaving the remainder of the presentation to tell the story of how the researchers came to those final products.
Information about the effectiveness of the PC-PTSD and the T-SBIRT process, the predictive validity regarding quality of life, and the clinical utility of the process of engaging people in additional services was not presented because the analysis was still underway and had not yet been approved by the SCF Board of Directors.
Final T-SBIRT Presentation Overview
The final presentation included a description of each research team member with pictures; descriptions of trauma; paraphrased goals of the study; research partners, roles, and a map of data collection sites; steps in the iterative development of the T-SBIRT pilot process (with clip art); an overview of the pilot process and experience of study participants; four PC-PTSD screening questions; review of the development and final content of a tri-fold brochure (Figure 2); data collection methods that examined the acceptability, feasibility, and validity of the process; and preliminary satisfaction data of participants involved in the study (verbal only).
Figure 2.
Intervention Brochure with Presenter Script
A local, non-AN/AI (White) study team member (JPA) delivered the presentation to the AN/AI audience. The SCF Research Department had identified in multiple previous projects that community audiences prefer to know more about the background of research team members. Thus, after describing the topic of the presentation, but before describing the study team, the presenter briefly described his personal/educational background, his history at SCF, and what drew him to work in this tribal health setting and on this trauma project.
RESULTS
Quantitative Results
Attendees responded that the presentation was clear (92%), the amount of information was about right (78%), and the results were presented in an interesting way (93%; Table 1).
Table 1.
Research Forum T-SBIRT Presentation Survey Responses
| Survey Response | N | % |
|---|---|---|
| The presentation about the results was clear. | ||
| Strongly disagree | 1 | 4% |
| Disagree | 1 | 4% |
| Agree | 14 | 54% |
| Strongly agree | 10 | 39% |
| Amount of information was about right. | ||
| Strongly disagree | 1 | 3% |
| Disagree | 6 | 19% |
| Agree | 18 | 58% |
| Strongly agree | 6 | 19% |
| The results were presented in an interesting way. | ||
| Strongly disagree | 0 | 0% |
| Disagree | 2 | 7% |
| Agree | 19 | 63% |
| Strongly agree | 9 | 30% |
Qualitative Results
Four broad themes were identified from the discussion groups with community members in direct response to the trauma presentation: 1) share results with everyone; 2) share results in ways that reach all AN audiences; 3) provide a status update in summary form at each stage of the study; and 4) use results to improve care for trauma and related symptoms. Although these themes were in direct result to the trauma presentation, it is believed that some individual responses apply more generally to research in a tribal health setting as attendees may have also been responding to the preceding presentation that addressed tribal oversight in research.
Share Results with Everyone
Attendees reported that they felt that everyone—tribal communities and the “general public”—should hear the results. This theme was near universal. Although everyone should hear results, participants identified key audiences: customer-owners of SCF, SCF providers, tribal partners, and elders and youth in rural tribal communities. The public, AN/AI and local non-Native, was viewed as a good “check and balance” of validity and applicability of research results.
Dissemination of broad themes was recommended with detailed information available for those with questions. For example, research activities and results of research occurring in Anchorage may be of interest to individuals in rural tribal communities because so many travel to Anchorage. Research products, such as the brochure, were seen as potentially helpful for the members of the general public, both AN and non-Native.
Share Results in Ways that Reach all AN Audiences
Research results should be shared in multiple ways to reach all AN audiences. Additionally, dissemination products should incorporate AN/AI languages and values, contain “flashy” graphics or videos, use large print, and have contact information to solicit more information.
Attendees suggested urban audiences might be easiest to reach on the Alaska Native Tribal Health campus using electronic educational panels located in the lobbies of clinics, home screens on public computers, and print media like posters, banners, and tri-fold brochures on display in waiting areas. They also suggested posting dissemination materials in waiting areas specific to the project, such as those for primary care or behavioral health services. Overall, attendees wanted to see more fliers in more locations in the clinic. Another suggestion of a convenient way to reach urban audiences was employee picnics and community events in which large numbers of AN/AI people gather.
Attendees wanted to make sure that research results were distributed to residents of rural AN villages. They suggested advertising in major television news or print news that can be seen and heard by village audiences, most notably by elders without computer access. Attendees indicated Anchorage-based print, television, and radio news are often distributed or rebroadcast in rural village communities. Specific venues could be larger in-state newspapers, television, and radio; tribal and village newspapers; or paid media-based advertising. The sentiment of attendees was that earned media (i.e., media coverage not paid for or owned) by non-tribal organizations may not necessarily be the best venue, but that paid advertisements containing tribal news were an acceptable way to capitalize on the reach of these non-tribal media sources. These avenues were seen as acceptable, even on the topic of trauma. Lastly, attendees wanted research activities and results disseminated through electronic sources that can be easily shared, such as social media (Facebook and Twitter) and electronic newsletters. Attendees said they felt that all forms of results (Anchorage Native News articles, handouts, brochures, PowerPoints, peer-reviewed publications, etc.) should be shared on the SCF website.
Provide a Summarized Status Update at Each Stage of the Study
Attendees wanted additional research project summaries like the T-SBIRT PowerPoint. However, they also requested that more information about the number of AN/AI participants who were involved in the development and pilot of the T-SBIRT be more clearly presented. Attendees stated that a summary would suffice for most people and those who wanted more could contact the SCF Research Department to ask questions or to acquire more detailed information. Attendees anticipated that community members would want to know more about the research process and data analysis. Attendees also wanted a summary of all current research activities at SCF.
Second to having information shared in different levels of detail, attendees expected research activities be shared before, during, and after active data collection. All forms of dissemination were seen as useful, but if budget only accommodated one form of dissemination, attendees preferred to wait until the end of the study or when results prompted changes to the health care system.
Use Results to Improve Care for Trauma and Related Symptoms
Trauma was regarded as having wide-ranging impacts on the AN/AI community. Attendees reported that they felt providers, specifically behavioral health providers and tribal doctors, should know about the results of SCF research projects, because research should enable providers to improve care for people with trauma. Results should be shared with providers to increase communication about trauma and related behavioral health services between providers. SCF and the statewide tribal health organization, the Alaska Native Tribal Health Consortium, were seen as having the funding, resources, and unique responsibility to conduct research to improve health outcomes of AN/AI people and to make these research efforts public.
DISCUSSION
The Alaska Native Health Research Forum format, T-SBIRT presentation, ARS, and discussion groups were well received by Forum attendees. This positive reception is consistent with the preference for transparent communication identified in the SCF community (Avey et al., 2016; Hiratsuka, Brown, Hoeft, & Dillard, 2012; Shaw, Robinson, Starks, Burke, & Dillard, 2013) and with the preference for open-house style events identified in other indigenous populations in the circumpolar north (Pufall et al., 2011).
However, unlike many other community-based dissemination efforts by academic researchers who partnered with AN communities to co-develop culturally relevant formats (Boyer, Mohatt, Pasker, Drew, & McGlone, 2007), Forum feedback suggested that the PowerPoint presented by our staff was a clear and interesting form of dissemination in this tribal health setting. The effectiveness of the PowerPoint presentation may be due, in part, to the forming of the presentation by a group of indigenous researchers specifically for a non-scientific population, limiting the presentation to 15 minutes, not including data tables or graphs in the presentation, the English speaking audience, and the near verbatim script to eliminate non-meaningful utterances. Still, the audience may have also simply responded in a desirable way as the presenter asked the rating questions immediately after the presentation, the audience may have been comprised of people who possessed a greater interest in research than the community as a whole, or had been exposed to more research studies.
Attendees described ways that owned media (i.e., those controlled by the organization) or tribally controlled news formats were preferred to earned media by national non-AN/AI sources (e.g., The New York Times) for disseminating results of tribal research. This preference is consistent with the literature, which indicates that results should be usable by the community involved in the study and that findings should be controlled by tribal organizations maintaining tribal sovereignty of intellectual property, including dissemination products (Harding et al., 2012). Interestingly, although providers at SCF and Elders in rural tribal communities were identified as key audiences, tribal and institutional leadership within SCF were not described as key audiences of the results of the study. However, it is likely that attendees were prompted to focus on the needs of their rural counterparts as the first presentation of the Forum, delivered by a SCF board member, reviewed the research process at SCF and heavily emphasized the oversight provided by tribal and institutional leadership. Similarly, although there were sentiments about the unique responsibility of tribal health organizations to conduct research, there appeared to be a clear lack of distinction between differing tribal entities among many attendees. Again, the first presentation may have played a role in this as it stressed the more recent shift to research conducted by AN people for AN people. Since the Forum, research staff have continued to analyze data and participate in a special SCF quality-improvement workgroup that addresses trauma-related services at SCF. Research staff have begun to draft a final results manuscript to complement a published manuscript on the T-SBIRT development (Hiratsuka et al., 2016).
Research staff also received permission from the SCF Board of Directors and Cherokee Nation IRB to disseminate updated results at two conferences intended to reach AN/AI researchers, clinicians, and health service administrators. The first presentation was a PowerPoint delivered at the Indian Health Services Division of Behavioral Health Conference. These results included additional technical information about the focus groups and interviews and the development of the T-SBIRT, the T-SBIRT process as tested, the usability and acceptability results of the pilot, the sensitivity and specificity of the PC-PTSD, and predictive validity related to quality of life. Audience members expressed satisfaction with the presentation, described it as one of the most data driven of the conference, and wanted to know more about the process so they could implement similar procedures at their institutions. The second presentation was a round-table discussion with similar talking points but that emphasized the clinical utility of the T-SBIRT. Because of the Alaska Native Health Research Forum, community dissemination efforts are planned for tribal news sources following SCF and CNHS Tribal Leadership approval.
Future Research
Future research should explore differences in dissemination strategies between academic CBPR partnerships and tribally-driven research located within the tribal health setting. Future research may also examine differences in perceptions of trustworthiness between research communicated at an open-house style event and public events in other settings. Research on dissemination efforts in large tribal health service areas may explore the reach of urban media syndication services to rural villages or dissemination to tribal partners, such as the Association of Village Council Presidents. Lastly, although attendees of this Forum preferred to receive overviews of research activities, researchers who produce electronic dissemination products should explore the liberal use of hyperlink references to ongoing and past local efforts, so those who want more information can click to the original sources.
Lessons Learned
Even among organizations, such as SCF, which are committed to conducting research using a CBPR process, the timing of disseminating results can be challenging and remains an area for improvement. For instance, community stakeholders may desire preliminary results; however, in many settings, such as SCF, all research results must first be reviewed by tribal leadership and authorized for distribution to the community. Yet, it remains critical for researchers to be cognizant to provide ongoing communication within each stakeholder group because this is crucial to conducting CBPR. Adequate tracking of tribal approval authorizing dissemination of incremental results, coordinating with external partners, and tailoring research dissemination products requires attention to detail, persistent effort, reporting infrastructure, and considerable reflection of context. In disseminating research results to community stakeholders, researchers may find it helpful to distinguish between research processes, research results, and the use of results to improve care. Distinct from research results and improvements to clinical care, types of research process information appropriate to share with stakeholders may include newly awarded funding, developed partnerships, or added faculty/researchers. In regards to dissemination, this community sample was interested in hearing about research results first and then the methods and rationale underlying their discovery.
ACKNOWLEDGEMENTS
This study was funded in part from the National Center on Minority Health and Health Disparities of the National Institutes of Health (grant number 2P60MD000507), the Indian Health Service/National Institute of General Medical Sciences (grant number U261IHS0079), and the National Institute of General Medical Sciences (grant number 1U54GM115371).
Footnotes
The purpose of this case study was to closely examine how to disseminate findings from a pilot test of a T-SBIRT (i.e., trauma-focused screening, brief intervention, and referral to treatment) process at Southcentral Foundation (SCF) to an Alaska Native and American Indian community audience. The current article first describes the pilot test and then focuses on a case study of the dissemination activities at the 2016 Alaska Native Health Research Forum, including the process of tailoring dissemination products for this community audience, the audience’s response to the delivered presentation, and audience feedback about future dissemination of T-SBIRT results.
Contributor Information
Dr. Jaedon P. Avey, Research Department at Southcentral Foundation in Anchorage.
Dr. Vanessa Y. Hiratsuka, Research Department at Southcentral Foundation.
Lisa G. Dirks, Research Department at Southcentral Foundation.
Laurie A. Moore, Centers for American Indian and Alaska Native Health at the University of Colorado Denver in Aurora, Colorado.
Barbara Beach, W.W. Hastings Hospital Behavior Health in Talequah, Oklahoma.
Dr. Douglas K. Novins, Division of Child and Adolescent Psychiatry, Department of Psychiatry at the University of Colorado School of Medicine in Aurora, Colorado.
Karen Caindec, Board of Directors for Southcentral Foundation.
Dr. Denise A. Dillard, Research Department at Southcentral Foundation.
REFERENCES
- Attride-Stirling J (2001). Thematic networks: An analytical tool for qualitative research. Qualitative Research, 1(3), 385–405. 10.1177/146879410100100307 [DOI] [Google Scholar]
- Avey JP, Hiratsuka VY, Beans JA, Trinidad SB, Tyndale RF, & Robinson RF (2016). Perceptions of pharmacogenetic research to guide tobacco cessation by patients, providers and leaders in a tribal healthcare setting. Pharmacogenomics, 17(4), 405–415. 10.2217/pgs.15.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, & Mitchell CM (2005). Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Archives of General Psychiatry, 62(1), 99–108. 10.1001/archpsyc.62.1.99 [DOI] [PubMed] [Google Scholar]
- Boyer BB, Mohatt GV, Pasker RL, Drew EM, & McGlone KK (2007). Sharing results from complex disease genetics studies: A community based participatory research approach. International Journal of Circumpolar Health, 66(1), 19–30. 10.3402/ijch.v66i1.18221 [DOI] [PubMed] [Google Scholar]
- Castrodale L (2007). Hospitalizations resulting from dog bite injuries -- Alaska, 1991–2002. International Journal of Circumpolar Health, 66(4), 320–327. 10.3402/ijch.v66i4.18273 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2013). Motor vehicle traffic-related pedestrian deaths - United States, 2001–2010. Morbidity and Mortality Weekly Report (MMWR), 62(15), 277–282. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6215a1.htm [PMC free article] [PubMed] [Google Scholar]
- Duran B, Malcoe LH, Sanders M, Waitzkin H, Skipper B, & Yager J (2004). Child maltreatment prevalence and mental disorders outcomes among American Indian women in primary care. Child Abuse & Neglect, 28(2), 131–145. 10.1016/j.chiabu.2003.06.005 [DOI] [PubMed] [Google Scholar]
- Duran B, Oetzel J, Parker T, Malcoe LH, Lucero J, & Jiang Y (2009). Intimate partner violence and alcohol, drug, and mental disorders among American Indian women in primary care. American Indian and Alaska Native Mental Health Research, 16(2), 11–27. 10.5820/aian.1602.2009.11 [DOI] [PubMed] [Google Scholar]
- Edelman LS, Cook LJ, & Saffle JR (2010). Burn injury in Utah: Demographic and geographic risks. Journal of Burn Care & Research, 31(3), 375–384. 10.1097/BCR.0b013e3181db51b0 [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Gilder DA, & Yehuda R (2013). Lifetime history of traumatic events in an American Indian community sample: Heritability and relation to substance dependence, affective disorder, conduct disorder and PTSD. Journal of Psychiatric Resesarch, 47(2), 155–161. 10.1016/j.jpsychires.2012.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T, Lindhorst T, Huang B, & Walters KL (2006). Interpersonal violence in the lives of urban American Indian and Alaska Native women: Implications for health, mental health, and help-seeking. American Journal of Public Health, 96(8), 1416–1422. 10.2105/AJPH.2004.054213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, … Grant BF (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. 10.1007/s00127-016-1208-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb K (2013). The Nuka System of Care: improving health through ownership and relationships. International Journal of Circumpolar Health, 72(1), 1–6. 10.3402/ijch.v72i0.21118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb K, Sylvester I, & Eby D (2008). Transforming your practice: what matters most. Family Practice Management, 15(1), 32–38. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/18277759 [PubMed] [Google Scholar]
- Harding A, Harper B, Stone D, O’Neill C, Berger P, Harris S, & Donatuto J (2012). Conducting research with tribal communities: Sovereignty, ethics, and data-sharing issues. Environmental Health Perspectives, 120(1), 6–10. 10.1289/ehp.1103904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiratsuka VY, Avey JP, Beans JA, Dirks LG, Caindec K, & Dillard DA (2018). Approach and methods of the 2016 Alaska Native Health Research Forum. American Indian and Alaska Native Mental Health Research, 25(1). 19–29. 10.5820/aian.2501.2018.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiratsuka VY, Brown JK, Hoeft TJ, & Dillard DA (2012). Alaska Native people’s perceptions, understandings, and expectations for research involving biological specimens. International Journal of Circumpolar Health, 71, 18642 10.3402/ijch.v71i0.18642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiratsuka VY, Moore L, Dillard DA, Avey JP, Dirks LG, … & Novins D (2016). Development of a screening and brief intervention process for symptoms of psychological trauma among primary care patients of two American Indian and Alaska Native health systems. The Journal of Behavioral Health Services & Research, 44(2), 224–241. 10.1007/s11414-016-9519-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBouthillier DM, McMillan KA, Thibodeau MA, & Asmundson GJ (2015). Types and number oftTraumas associated with suicidal ideation and suicide attempts in PTSD: Findings from a U.S. nationally representative sample. Journal of Traumatic Stress, 28(3), 183–190. 10.1002/jts.22010 [DOI] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Novins DK, Beals J, & Manson SM (2005). Childhood physical and sexual abuse and subsequent depressive and anxiety disorders for two American Indian tribes. Psychological Medicine, 35(3), 329–340. 10.1017/s0033291704003599 [DOI] [PubMed] [Google Scholar]
- Malcoe LH, Duran BM, & Montgomery JM (2004). Socioeconomic disparities in intimate partner violence against Native American women: A cross-sectional study. BMC Medicine, 2(20), 1–14. 10.1186/1741-7015-2-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD, & Team A-S (2005). Social epidemiology of trauma among 2 American Indian reservation populations. American Journal of Public Health, 95(5), 851–859. 10.2105/AJPH.2004.054171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Nandi A, & Galea S (2008). Post-traumatic stress disorder following disasters: A systematic review. Psychological Medicine, 38(4), 467–480. 10.1017/s0033291707001353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack KM, Frattaroli S, Young JL, Dana-Sacco G, & Gielen AC (2012). Motor vehicle deaths among American Indian and Alaska Native populations. Epidemiologic Reviews, 34(1), 73–88. 10.1093/epirev/mxr019 [DOI] [PubMed] [Google Scholar]
- Pufall EL, Jones AQ, McEwen SA, Lyall C, Peregrine AS, & Edge VL (2011). Community-derived research dissemination strategies in an Inuit community. International Journal of Circumpolar Health, 70(5), 532–541. 10.3402/ijch.v70i5.17860 [DOI] [PubMed] [Google Scholar]
- Saylors K, & Daliparthy N (2006). Violence against Native women in substance abuse treatment. American Indian and Alaska Native Mental Health Research, 13(1), 32–51. 10.5820/aian.1301.2006.32 [DOI] [PubMed] [Google Scholar]
- Schnurr PP (2015). Understanding pathways from traumatic exposure to physical health. In Schnyder U & Cloitre M (Eds.), Evidence Based Treatments for Trauma-Related Psychological Disorders: A Practical Guide for Clinicians (pp. 87–103). Cham: Springer International Publishing. [Google Scholar]
- Shaw JL, Robinson R, Starks H, Burke W, & Dillard DA (2013). Risk, reward, and the double-edged sword: Perspectives on pharmacogenetic research and clinical testing among Alaska Native people. American Journal of Public Health, 103(12), 2220–2225. 10.2105/AJPH.2013.301596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Service Administration. (2014). Trauma-Informed Care in Behavioral Health Services: TIP 57 Retrieved from http://store.samhsa.gov/product/TIP-57-Trauma-Informed-Care-in-Behavioral-Health-Services/SMA14-4816 [PubMed]
- Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, … Yager J (2004). Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. American Journal of Psychiatry, 161(11 Suppl), 3–31. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15617511 [PubMed] [Google Scholar]
- Wood DS, & Magen RH (2009). Intimate partner violence against Athabaskan women residing in interior Alaska: Results of a victimization survey. Violence Against Women, 15(4), 497–507. 10.1177/1077801208331245 [DOI] [PubMed] [Google Scholar]