Abstract
Background and Purpose
Data for a relationship between salt intake and stroke have been inconsistent. This inconstancy could be due to that the majority of studies evaluated salt intake at a single time point, which may be insufficient to accurately characterize salt intake throughout the observation period.
Methods
Included were 77,605 participants from the Kailuan Study. We assessed perceived salt intake via questionnaire in 2006, 2008, and 2010. Salt intake trajectories during 2006 to 2010 were identified using latent mixture models. Incident stroke cases were identified during 2010 to 2015 and confirmed by review of medical records. Cox proportional hazards model was used to examine the association between salt intake trajectories and stroke risk, after adjusting for possible confounders, including age, sex, lifestyle, social economic status, body mass index, use of medicines, blood pressure and lipoprotein profiles.
Results
Identified were 5 distinct salt intake trajectories: moderate-stable (n=59,241), moderate-decreasing (n=9,268), moderate-increasing (n=2,975), low-increasing (n=2,879) and high-decreasing (n=3,242). During the 5 year follow-up period there were 1,564 incident strokes cases. Compared with individuals with the moderate-stable salt intake trajectory, individuals with moderate-decreasing salt intake trajectory had significantly lower cerebral infarction stroke risk (adjusted HR: 0.77; 95%CI: 0.62–0.95), but not intracerebral hemorrhage risk (adjusted HR: 0.84; 95%CI: 0.55–1.29). Further adjustment for 2006 or 2010 perceived salt intakes generated similar results. When baseline perceived salt intake only was used as the exposure, a significant dose-response relation between higher perceived salt intake and higher stroke risk was observed (P-trend=0.006).
Conclusion
Change in salt intake was associated with the stroke risk. These data support the dietary recommendation to reduction of salt intake.
Keywords: salt eating habit, salt intake, stroke, trajectory, perceive
Although during the past decade there has been a small decline, the burden of stroke remains enormous. Globally, stroke is the second leading cause of mortality 1 and disability 2. According to data from 2016, in the US stroke was the fourth leading cause of mortality 1 and eighth leading cause of morbidity in 20162. During the same year, in China stroke was the first leading cause of mortality1 and morbidity2.
Extensive studies have documented a positive association between salt intake and both stroke risk and other cardiovascular events 3–6. Consequently, population-wide approaches to reduce salt intake have been recommended 7–9. However, several recent studies have raised questions about potential adverse effects associated with low salt intake and cardiovascular events 10–13, 15. In a review paper, Whelton and his colleagues identified several methodological concerns of these studies14. For example, some studies13,15 were conducted in patients at high risk for cardiovascular diseases and stroke, which limits the generalizability of their results to general population.
Another potential reason for the mixed results is that the majority of studies evaluated salt intake at a single time point, usually at baseline, which may inaccurately characterize salt intake throughout the observation period. Change in salt intake in response to public health campaigns and changes in the food supply over time may be an important factor in accurately predicting risk, and could be a critical factor in the future development of evidence-based guidelines for stroke prevention and treatment. We, thus, examined whether salt intake trajectories during a 4-year period were associated with subsequent stroke risk in approximately 77,000 Chinese adults.
Methods
De-identified data are available to researchers upon request by contacting with Dr Shouling Wu or Dr Xiang Gao.
Participants
The current analysis was based on the Kailuan Study, an ongoing community-based longitudinal cohort started in 2006, as detailed elsewhere16–18. Briefly, in 2006–2007, 101,510 participants (81,110 men and 20,400 women, aged 18–98) underwent a comprehensive survey, including questionnaire (e.g., demographic characteristics, medical co-morbidities, medication use, and lifestyle factors), physical examination and laboratory tests. The follow-up survey has been conducted biennially.
In the current study, 8,873 participants were excluded due to a diagnosis of myocardial infarction, stroke and cancer during or prior to 2010 (baseline of this analysis), and 15,032 participants were excluded due to missing perceived salt intake data in the 2006 or 2008/2010 surveys. In total, 77,605 participants were included in the analysis (Supplemental Figure I, online-only Data Supplement). Compare to participants with missing perceived salt intake data, the participants included in the analysis were younger (53.6 vs 62.5 years), and more likely to be women (22.2% vs 13.7%), and had higher prevalence of CVD risk factors (e.g., smoking, physical inactivity, higher concentrations of hs-CRP and LDL-C, and lower concentrations of HDL-C) (Supplemental Table I, online-only Data Supplement). However, we did not observe significant difference in stroke risk between these two groups (Supplemental Table I, online-only Data Supplement).
This investigation was approved by the Ethics Committee of the Kailuan General Hospital. All participants gave their written informed consent. This manuscript adheres to the AHA Journals’ implementation of the Transparency and Openness Promotion (TOP) Guidelines.
Assessment of stroke
The outcome was the first incident stroke, either fatal or nonfatal. Assessments of stroke incidence were conducted once a year during the follow-up period, from 2010 to 2015. Identification of incident stroke was described previously 17,19. In brief, potential stroke incidence was ascertained from 4 complementary sources: (1) Municipal Social Insurance Institution which covered all study participants, (2) Hospital Discharge Register centers, (3) death certificates, and (4) questionnaire survey (biennially since 2006). Potential stroke cases included those who were identified by the ninth and tenth revision of International Classification of Diseases based on the first three sources or those who self-reported in questionnaire survey. According to the World Health Organization criteria combined with a brain computed tomography or magnetic resonance imaging scans, three cardiologist and neurologists reviewed the medical records to confirm the stroke diagnosis. Nonfatal strokes were defined as the sudden onset of focal neurological deficit with vascular mechanism lasting >24 hours. Fatal stroke cases were confirmed by medical records, autopsy reports or death certificates, with stroke as the underlying cause of death. In the current study, only included were cerebral infarction and intracerebral hemorrhage, and not included were epidural, subdural, or subarachnoid hemorrhage.
Assessment of salt intake and covariates
Perceived salt intake was assessed in 2006, 2008 and 2010 by asking participants to rate their habitual daily salt intake as “low”, “medium” or “high”. Low was defined as <6 gram/day (<2400 mg/d sodium intake), medium as 6–10 gram/day (2400–4000 mg/d sodium intake) and high as >10 gram/day (>4000 mg/d sodium intake), as described elsewhere16. Although <6 gram/day of salt is higher than the recommended salt intake (<5 gram/day) by WHO, the categorization is consistent low according to habitual intakes in China.
In 2012, random spot urine samples were collected from 231 Kailuan study participants with hypertension who were not treated with antihypertensive drugs. Higher perceived salt intake was positively associated with estimated 24-hour urinary sodium excretion 20. Average 24-hour urinary sodium excretion was 3,745 mg/d, 3,930 mg/d, and 3,958 mg/d, respectively, across three perceived salt intake groups (P-trend<0.001), after adjustment for age, sex, and blood pressure.
Data on age, sex, smoking, alcohol intake, physical activity, education level, monthly income, and former medical history (e.g., hypertension, diabetes, cancer and active treatments such as hypoglycemic, antihypertensive and lipid-lowering medications) were collected by self-reported questionnaire. Height, weight, and blood pressure (BP) were assessed by trained nurses during the surveys, as detailed previously 17,21. Body mass index (BMI) was calculated as weight (kilogram)/height (meter)2.
Fasting (>12 hour) blood samples were collected into EDTA (ethylene diamine tetra acetic acid) containing vacuum tubes. The plasma glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), creatinine, and high sensitivity C-reactive protein (hs-CRP) were measured by auto analyzer (Hitachi 747; Hitachi, Tokyo, Japan) at the central laboratory at Kailuan general hospital. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration creatinine equation.
Statistical analysis
All analyses were conducted using SAS 9.3 (SAS Institute, Inc, NC). Two-sided P<0.05 was considered statistically significant.
Means and standard deviations were calculated for normally distributed variables; median and interquartile range (IQR) were calculated for non-normally distributed data; percentages were calculated for categorical data. The person-time of follow-up for each participant was determined from the completion date of the 2010 survey to either the date of the first occurrence of stroke, death, lost to follow-up (n=4,869, 6.27%), or the end of follow-up (December 31, 2015), whichever came first.
The primary exposure of this analysis is the longitudinal change in perceived salt intake during 2006 to 2010. Based on study data, latent mixture modeling, within the PROC TRAJ procedure, was used to identify a posteriori trajectories that share the similar underlying perceived salt intake change 22,23. Censored normal appropriate for scaled data was used. Initially, a model with 1 trajectory pattern was used and then with 2, 3, 4 and up to 5 trajectory patterns were added. Model fit was assessed using the Bayesian Information Criterion (BIC), the best fit model is the one with the smallest negative number.
Cox proportional hazards model was used to investigate the association between salt intake trajectories and risk of developing stroke after adjustment for potential confounders including age, sex, smoking, alcohol intake, education, physical activity, average monthly income, systolic blood pressure, diastolic blood pressure, estimated glomerular filtration rate, average concentration of triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, high sensitivity C-reactive protein, fasting blood glucose and body mass index, updated use of antihypertensive, hypoglycemic, and lipid-lowering medications during 2006 to 2010. The moderate-stable pattern with the most participants (76.3%) was set as reference group. The proportional-hazards assumption was satisfied.
To examine whether the potential association between salt intake trajectories and stroke risk could be explained by salt intake at any one time point, further adjusts were made for 2006 or 2010 perceived salt intake, one at a time. In the secondary analysis, also examined was whether baseline perceived salt intake, based on a single assessment in 2010, was associated with future stroke risk.
We explored potential interaction between salt intake trajectories and age (<60 years versus ≥ 60 years), sex, hypertension status (yes versus no) and kidney function (eGFR<60 mL/min/1.73m2 versus eGFR≥ 60 mL/min/1.73m2), in relation to stroke risk, with adjustment for aforementioned covariates.
Results
In our study, the model with 5 trajectories based on perceived salt intake level and changing pattern from 2006 to 2010 was identified as the best fit by comparing the BIC (Table 1). Overall, 76.3% of participants had a maintained moderate salt intake level (all perceived salt intake levels were ‘moderate’ in 2006, 2008 and 2010 surveys, respectively, referred to as ‘moderate-stable trajectory’), 11.9% of the participants who started with moderate salt intake level changed to lower salt intake (perceived salt intake level was ‘moderate’ in 2006, and ‘low’ in 2008 and 2010 surveys, respectively, referred to as ‘moderate-decreasing trajectory’), 3.8% of the participants who started with moderate salt intake level changed to higher salt intake (perceived salt intake level was ‘moderate’ in 2006, and ‘high’ in 2008 and 2010 surveys, respectively, referred to as ‘moderate-increasing trajectory’), 3.7% of the participants who started with low salt intake level changed to moderate salt intake (perceived salt intake level was ‘low’ in 2006, and ‘moderate’ in 2008 and 2010 surveys, respectively, referred to as ‘low-increasing trajectory’), 4.2% of the participants who started with high salt intake level changed to moderate salt intake (perceived salt intake levels were ‘high’ in 2006, and ‘moderate’ in 2008 and 2010 surveys, referred as ‘high-decreasing trajectory’). Individuals with the moderate-decreasing trajectory were more likely to be younger, non-smokers and non-drinkers, had lower total cholesterol and systolic blood pressure, relative to other groups (Table 2).
TABLE 1.
Trajectories of salt intake during 2006–2010
| Trajectory patterns | n | % | Salt Intake
|
||
|---|---|---|---|---|---|
| 2006 | 2008 | 2010 | |||
| Moderate- Stable | 59241 | 76.3 | Moderate | Moderate | Moderate |
| Moderate- Decreasing | 9268 | 11.9 | Moderate | Low | Low |
| Moderate- Increasing | 2975 | 3.8 | Moderate | High | High |
| Low- Increasing | 2879 | 3.7 | Low | Moderate | Moderate |
| High- Decreasing | 3242 | 4.2 | High | Moderate | Moderate |
TABLE 2.
Basic characteristics according to the salt intake trajectory patterns during 2006 to 2010, among 77,605 Kailuan participants
| Moderate- Stable |
Moderate- Decreasing |
Moderate- Increasing |
Low- Increasing |
High- Decreasing |
P value | |
|---|---|---|---|---|---|---|
| N (%) | 59241(76.3) | 9268(11.9) | 2975(3.8) | 2879(3.7) | 3242(4.2) | |
| Age, year | 53.9±11.9 | 51.9±11.5 | 54.5±11.8 | 53.7±12.8 | 52.2±12.4 | <0.001 |
| Women, % | 22.9 | 22.6 | 15.4 | 23.8 | 13.4 | <0.001 |
| Smoking status, % | <0.001 | |||||
| Never | 62.1 | 62.7 | 54.1 | 49.1 | 32.4 | |
| Past | 4.9 | 4.7 | 5.1 | 8.6 | 6.8 | |
| Current | 33.0 | 32.6 | 40.8 | 42.3 | 60.8 | |
| Alcohol intake, % | <0.001 | |||||
| Never | 67.4 | 68.1 | 62.3 | 47.6 | 35.6 | |
| Past | 3.4 | 3.5 | 3.7 | 5.7 | 5.1 | |
| Light* | 6.2 | 6.5 | 6.8 | 11.2 | 11.3 | |
| Moderate* | 4.3 | 4.1 | 4.9 | 7.3 | 6.8 | |
| Heavy* | 18.7 | 17.8 | 22.3 | 28.2 | 41.2 | |
| Physical activity, % | <0.001 | |||||
| 3+ times/week | 13.6 | 15.1 | 13.3 | 29.0 | 24.0 | |
| 1–2 times/week | 77.9 | 75.9 | 78.7 | 56.6 | 58.2 | |
| Never | 8.5 | 9.0 | 8.0 | 14.4 | 17.8 | |
| Education, % | <0.001 | |||||
| College /university | 7.1 | 7.3 | 6.0 | 13.7 | 13.0 | |
| Middle school | 84.3 | 84.6 | 84.4 | 76.4 | 75.8 | |
| Illiteracy or elementary school | 8.6 | 8.1 | 9.6 | 9.9 | 11.2 | |
| Average income, % | <0.001 | |||||
| ≥¥3000/ month | 6.4 | 6.3 | 5.9 | 12.5 | 10.6 | |
| ¥500 to ¥2999/ month | 65.6 | 62.3 | 67.0 | 50.0 | 49.3 | |
| <¥500/month | 28.0 | 31.4 | 27.1 | 37.4 | 40.1 | |
| Use of antihypertensive agent†, % | 16.0 | 16.1 | 19.2 | 19.3 | 22.9 | <0.001 |
| Use of lipid-lowering agents†, % | 1.7 | 2.0 | 1.7 | 2.6 | 2.9 | <0.001 |
| Use of hypoglycemic agents†, % | 4.5 | 4.8 | 4.8 | 5.7 | 5.2 | 0.006 |
| Body mass index, kg/m2 | 25.0±3.4 | 24.9±3.4 | 25.2±3.6 | 24.7±3.4 | 25.5±3.5 | <0.001 |
| hs-CRP †,‡, mg/mL | 1.35(1.95) | 1.40(1.99) | 1.31(1.72) | 1.19(1.63) | 1.26(1.69) | <0.001 |
| Fasting blood glucose†, mmol/L | 5.56±1.36 | 5.54±1.32 | 5.61±1.53 | 5.54±1.38 | 5.59±1.43 | 0.14 |
| Total cholesterol †, mmol/L | 4.98±0.89 | 4.91±0.84 | 5.00±0.93 | 4.99±0.92 | 5.06±0.92 | <0.001 |
| Triglycerides †,‡, mmol/L | 1.32(0.96) | 1.32(0.93) | 1.38(1.07) | 1.32(1.01) | 1.42(1.17) | <0.001 |
| HDL-C†, mmol/L | 1.53±0.33 | 1.54±0.31 | 1.52±0.35 | 1.54±0.34 | 1.52±0.32 | 0.002 |
| LDL-C†, mmol/L | 2.52±0.37 | 2.52±0.65 | 2.52±0.67 | 2.58±0.68 | 2.61±0.67 | <0.001 |
| Systolic blood pressure†, mmHg | 130.6±17.6 | 129.3±16.9 | 132.1±18.2 | 129.4±17.5 | 130.6±17.8 | <0.001 |
| Diastolic blood pressure†, mmHg | 84.0±9.6 | 83.7±9.4 | 84.9±9.9 | 83.0±9.4 | 84.4±9.9 | <0.001 |
| eGFR2, mL/min/1.73m2 | 84.9±17.1 | 86.8±17.0 | 87.3±16.5 | 86.7±16.6 | 89.0±16.8 | <0.001 |
Light drinker: 0.1–0.4 servings/day for women and 0.1–0.9 serving/day for men; moderate: 0.5–1.5 servings/day for women and 1–2 serving/day for men; heavy: >1.5 servings/day for women and >2 serving/day for men; based on 15g of alcohol per day.
Average values based on measurements in 2006, 2008, and 2010.
Median (interquartile range).
Hs-CRP, high sensitivity C-reactive protein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate.
During 5 years of follow-up (2010–2015), 1564 incident strokes cases (1362 cerebral infarction cases and 202 intracerebral hemorrhage cases) were identified. Compared with individuals with moderate-stable salt intake trajectory, individuals with the moderate-decreasing salt intake trajectory had significantly lower stroke risk, with adjusted hazard ratio of 0.77 and 95% confidence interval of 0.64–0.91. When the stroke subtype was considered, we observed a significant association between the moderate-decreasing salt intake trajectory and cerebral infarction (adjusted hazard ratio was 0.76, 95% confidence interval was 0.63 to 0.92). We found a similar trend for risk of intracerebral hemorrhage, the association, however, was not significant (adjusted hazard ratio was 0.84, 95% confidence interval was 0.55 to 1.29).
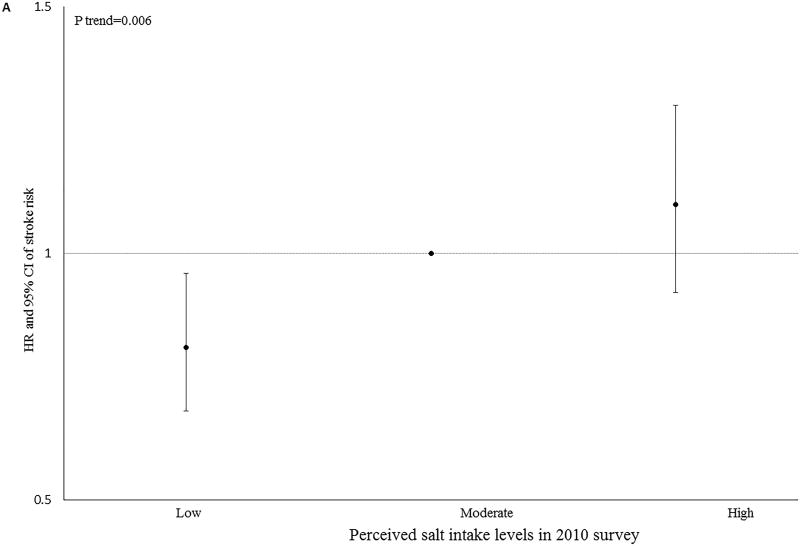
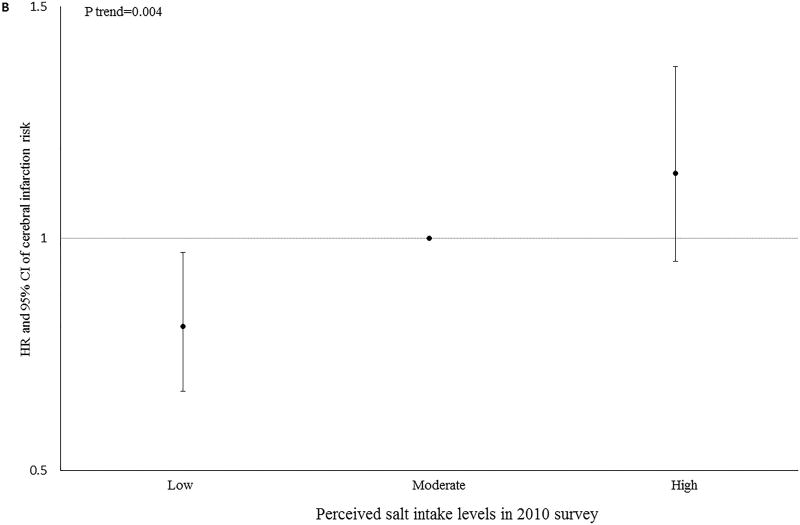
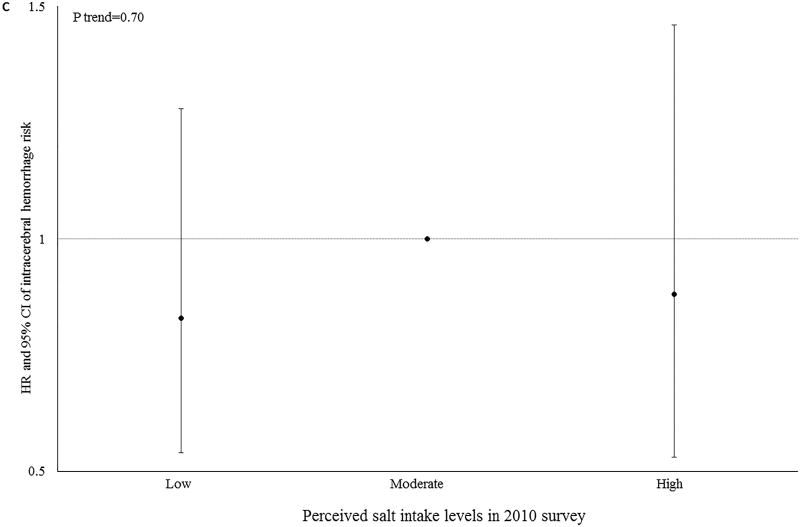
Further adjustment for 2006 perceived salt intake or 2010 perceived salt intake generated similar results (Table 3). We did not find any significant interactions between salt intake trajectories and sex, age, hypertension status and kidney function in relation to stroke (all P-interaction >0.05, Supplemental Table I, online-only Data Supplement). Consistently, we observed a significant dose-response relationship between a single assessment of salt intake at the baseline and future stroke risk (P-trend=0.006) (Figure 1).
TABLE 3.
Adjusted Hazard Ratios and 95% confidence intervals for risk of stroke, according to the salt intake trajectory patterns during 2006 to 2010, among 77,605 Kailuan participants
| Moderate- Stable N=59241 |
Moderate- Decreasing N=9268 |
Moderate- Increasing N=2975 |
Low- Increasing N=2879 |
High- Decreasing N=3242 |
|
|---|---|---|---|---|---|
| Stroke | |||||
| Case # | 1225 | 141 | 72 | 54 | 72 |
| Incidence/ 1000 person year | 4.29 | 3.07 | 5.04 | 3.92 | 4.64 |
| Age and sex adjusted | 1.00 | 0.80(0.67,0.95) | 1.09(0.86,1.38) | 0.89(0.68,1.17) | 1.12(0.88,1.41) |
| Fully adjusted model* | 1.00 | 0.77(0.64,0.91) | 1.04(0.82,1.32) | 0.92(0.70,1.22) | 1.01(0.79,1.28) |
| Further adjusted of perceived salt intake in 2006* | 1.00 | 0.77(0.64,0.91) | 1.04(0.82,1.32) | 0.99(0.70,1.39) | 0.99(0.74,1.32) |
| Further adjusted of perceived salt intake in 2010* | 1.00 | 0.77(0.64,0.95) | 1.00(0.77,1.29) | 0.93(0.71,1.23) | 0.98(0.77,1.26) |
| Cerebral infarction | |||||
| Case # | 1062 | 120 | 68 | 47 | 65 |
| Incidence/ 1000 person year | 3.72 | 2.62 | 4.76 | 3.41 | 4.19 |
| Age and sex adjusted | 1.00 | 0.79(0.65,0.95) | 1.19(0.93,1.53) | 0.91(0.68,1.21) | 1.18(0.92,1.52) |
| Fully adjusted model* | 1.00 | 0.76(0.63,0.92) | 1.14(0.89,1.46) | 0.92(0.69,1.24) | 1.04(0.81,1.34) |
| Further adjusted of perceived salt intake in 2006* | 1.00 | 0.75(0.62,0.91) | 1.15(0.90,1.47) | 0.96(0.66,1.38) | 1.00(0.74,1.36) |
| Further adjusted of perceived salt intake in 2010* | 1.00 | 0.77(0.62,0.95) | 1.09(0.84,1.43) | 0.93(0.69,1.26) | 1.02(0.79,1.32) |
| Intracerebral hemorrhage | |||||
| Case # | 163 | 21 | 4 | 7 | 7 |
| Incidence/ 1000 person year | 0.57 | 0.46 | 0.28 | 0.51 | 0.45 |
| Age and sex adjusted | 1.00 | 0.86(0.56,1.32) | 0.50(0.21,1.22) | 0.78(0.37,1.65) | 0.71(0.33,1.50) |
| Fully adjusted model* | 1.00 | 0.84(0.55,1.29) | 0.47(0.19,1.14) | 0.84(0.39,1.79) | 0.71(0.33,1.52) |
| Further adjusted of perceived salt intake in 2006* | 1.00 | 0.85(0.55,1.30) | 0.46(0.19,1.12) | 1.09(0.41,2.87) | 0.85(0.34,2.10) |
| Further adjusted of perceived salt intake in 2010* | 1.00 | 0.79(0.48,1.29) | 0.44(0.17,1.12) | 0.82(0.38,1.76) | 0.70(0.33,1.52) |
Adjusted for age, sex, smoking (current, past, or never), alcohol intake (never, past, light, moderate, or heavy), education (illiteracy or elementary school, middle school, or college/university), physical activity (never, sometimes, or active), average monthly income of each family member (<¥500, ¥500 to ¥3000, or≥¥3000), systolic blood pressure (≤120, 121–139, ≥140 mmHg), diastolic blood pressure (≤80, 81–89, ≥90 mmHg), estimated glomerular filtration rate(≤30, 31–59, 60–89, ≥90 mL/min/1.73m2), average concentration of triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, high sensitivity C-reactive protein, fasting blood glucose and body mass index, use of antihypertensive, hypoglycemic, and lipid-lowering medications (yes/no for each).
FIGURE 1.
Adjusted Hazard Ratios and 95% confidence intervals for risk of stroke (A), cerebral infarction (B) or intracerebral hemorrhage (C) according to perceived salt intake in 2010, adjusted for age, sex, smoking (current, past, or never), alcohol intake (never, past, light, moderate, or heavy), education (illiteracy or elementary school, middle school, or college/university), physical activity (never, sometimes, or active), average monthly income of each family member (<¥500, ¥500 to ¥3000, or≥¥3000), systolic blood pressure (≤120, 121–139, ≥140 mmHg), diastolic blood pressure (≤80, 81–89, ≥90 mmHg), estimated glomerular filtration rate(≤30, 31–59, 60–89, ≥90 mL/min/1.73m2), average concentration of triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, high sensitivity C-reactive protein, fasting blood glucose and body mass index, use of antihypertensive, hypoglycemic, and lipid-lowering medications (yes/no for each).
Discussion
In this large-scale prospective population-based cohort, perceived reductions in salt intake from moderate (2400–4000 mg/d sodium intake) to low (<2400 mg/d sodium intake) was associated with 23% lower risk of stroke, independent of a single assessment of perceived salt intake and other known risk factors for stroke including blood pressure. When a single assessment of perceived salt intake at baseline was used as exposure, we observed similar results – lower perceived salt intake was associated with lower future stroke risk. Our results provide further evidence to support the notion that reducing salt intake is beneficial, which contributes our understanding of stroke prevention.
The average sodium intakes exceed the WHO recommended levels in almost all countries globally 24. In China, average sodium intake was high, at about 4,830 mg /d 24, which was more than twice the recommended intake levels (2,000 mg /d) by WHO. Consistently, in the current study, more than 75% of the participants had a maintained moderate salt intake level (2400–4000 mg/d sodium intake) during a 4-year period. We observed a significant association between the moderate-decreasing salt intake trajectory and lower further stroke risk, which has important public health implications. In a recent analysis based on the National Health and Nutrition Examination Survey, excess sodium intake (>2000 mg/d) was found to be the leading dietary factor associated with cardiometabolic mortality in the US 25. Specifically, high sodium intake was associated with 10.7% of deaths due to stroke 25.
Most research studies to date have focused on the health effects of salt intakes based on a single assessment, while little information is available on the health effect of salt intake changes over time. Interestingly, sodium intake in the US adult population did not decrease during past 5 decades26. Although no published studies were identified that assessed the association between salt intake change over time and risk of stroke, studies concluding that salt/sodium intake is positively associated with stroke risk 27,28 and cardiovascular events (including stroke) 7,29 have appeared, consistent with our observations. In contrast, a limited number of studies have suggested an increased stroke or cardiovascular events risk with low salt intakes. In an analysis based on 101,945 participants of the Prospective Urban Rural Epidemiology (PURE) study, an estimated sodium excretion below 3000 mg per day was associated with an increased risk of cardiovascular events, including stroke (adjusted hazard ratio was 1.27), compared with an estimated sodium excretion of 4000 to 5999 mg per day 11. This association was not modified by hypertension status 10. One possible reason for these conflicting results is we focused on change in salt intake over time rather than absolute salt intake at baseline and subsequent stroke risk. In addition, different methods were used to estimate sodium intake in the two studies. In the PURE study, salt intake was assessed using spot urine samples. In the Kailuan study perceived salt intake was assessed by questionnaire. Of note, given the limitations of our dataset we could not assess the association between sodium intake <3000 mg/d and stroke.
A potential mechanism to explain the association between moderate-decreasing salt intake trajectory and lower stroke risk is the well documented association between higher salt intakes and higher blood pressure 30, a major risk factor of stroke 17,31. However, in the current study, perceived salt intake was associated with stroke even after adjustment for hypertension status. Additionally, a recent study reported that high salt intake could result in endothelial dysfunction and arterial stiffness, followed by fibrosis and decreased elasticity of large arteries. These changes are associated with an exacerbation of hypertension, hence increased stroke risk 32. Low salt intakes may decrease systemic oxidative stress 33, another risk factor for stroke 34.
We did not identify a trajectory with consistently high salt intake during 2006 to 2010 and thus cannot examine the potential harmful effects due to long-term high salt consumption. Interestingly, we did not observe significantly altered risk in the other trajectory patterns, which could be due to no actual relationship or lack of statistical power – there were only ~ 4% of participants in each of the patterns. If the former, the findings could have important implications for clinical recommendations.
A major limitation of the study is the use of self-report of salt intake, rather than 24-hour urine sodium excretion, to estimate the daily salt intake. For large-scale cohort studies, as the Kailuan study, such measures are not feasible. In a validation study, we found a significant dose-response association between perceived salt intake and estimated 24-hour urine sodium excretion, which is consistent with previous findings 35,36. Therefore, although imperfect, self-reported salt intake, as a surrogate of habitual salt intake, appears to be a feasible method to rank individuals according their relative average salt intake, compare extremes in a large population, and predict risk of relevant health outcomes. The possibility of residual confounding could not be ruled out, although we controlled a wide range of biologically relevant potential confounders. For example, detailed dietary intake data were not available; thus, adjust for potential dietary confounders such as total energy or saturated fat intake could not be factored into the analyses. The model did include adjustment for obesity, fasting glucose concentration and lipid profile (e.g., triglyceride, HDL-C, and LDL-C), which were associated with dietary intake. Also unavailable are data on the reasons for changes in salt intake, which could confound the observed association between salt intake trajectories and stroke risk. Participants might have reduced salt intake due to the diagnosis of hypertension or other cardiovascular disease-related conditions. However, in that case, an increased risk of stroke may have been expected in those who decreased their salt intake. In contrast, lower stroke risk was observed in the moderate-decreasing pattern, relative to the moderate-stable pattern. The possibility of indication confounding cannot be excluded because significant results were only observed in participants with hypertension, but not in those with normal blood pressure, although the difference between these groups was not statistically significant (P-interaction =0.08). In addition, all participants in our study were residents in the Kailuan community, Tangshan city, and most were men (77.8%), therefore, the observed results may not be generalizable. However, similar relations between lower salt intake and lower subsequent stroke risk have been consistently observed in different ethnic groups and in those with different cultural backgrounds and dietary patterns 5,27. Finally, we did not collect the information on the different subtype of cerebral infarction and we thus cannot further explore the potential effect of salt intake on different subtypes of ischemic stroke.
Conclusions
Our findings provide preliminary evidence identifying the importance of salt intake changes over time and stroke risk. Our study should be interpreted with caution due to the possibility of misclassification of exposure and presence of residual confounding. Further studies with precise assessment of salt intake are warranted to replicate the findings.
Supplementary Material
Acknowledgments
Sources of Funding
Supported by the by NIH/National Institute of Neurological Disorders and Stroke (grant 5R21NS087235-02).
Footnotes
Disclosures
None.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260–1344. doi: 10.1016/S0140-6736(17)32130-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makin SDJ, Mubki GF, Doubal FN, Shuler K, Staals J, Dennis MS, et al. Small Vessel Disease and Dietary Salt Intake: Cross-Sectional Study and Systematic Review. J Stroke Cerebrovasc Dis. 2017:30414–7. doi: 10.1016/j.jstrokecerebrovasdis.2017.08.004. S1052–3057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okayama A, Okuda N, Miura K, Okamura T, Hayakawa T, Akasaka H, et al. Dietary sodium-to-potassium ratio as a risk factor for stroke, cardiovascular disease and all-cause mortality in Japan: the NIPPON DATA80 cohort study. BMJ Open. 2016;6:e011632. doi: 10.1136/bmjopen-2016-011632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–34. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 6.Turlova E, Feng ZP. Dietary salt intake and stroke. Acta Pharmacol Sin. 2013;34:8–9. doi: 10.1038/aps.2012.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and reduced cardiovascular risk. Circulation. 2014;129:981–9. doi: 10.1161/CIRCULATIONAHA.113.006032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Appel LJ. Reducing sodium intake to prevent stroke: time for action, not hesitation. Stroke. 2014;45:909–11. doi: 10.1161/STROKEAHA.113.002870. [DOI] [PubMed] [Google Scholar]
- 9.Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S76–99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- 10.Mente A, O’Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388:465–75. doi: 10.1016/S0140-6736(16)30467-6. [DOI] [PubMed] [Google Scholar]
- 11.O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–23. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 12.Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerova J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–85. doi: 10.1001/jama.2011.574. [DOI] [PubMed] [Google Scholar]
- 13.O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–38. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]
- 14.Whelton PK, Appel LJ, Sacco RL, Anderson CA, Antman EM, Campbell N, et al. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012;126:2880–9. doi: 10.1161/CIR.0b013e318279acbf. [DOI] [PubMed] [Google Scholar]
- 15.Thomas MC, Moran J, Forsblom C, Harjutsalo V, Thorn L, Ahola A, et al. The association between dietary sodium intake, ESRD, and all-cause mortality in patients with type 1 diabetes. Diabetes Care. 2011;34:861–6. doi: 10.2337/dc10-1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Q, Zhou Y, Gao X, Wang C, Zhang S, Wang A, et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke. 2013;44:2451–6. doi: 10.1161/STROKEAHA.113.678839. [DOI] [PubMed] [Google Scholar]
- 17.Li W, Jin C, Vaidya A, Wu Y, Rexrode K, Zheng X, et al. Blood Pressure Trajectories and the Risk of Intracerebral Hemorrhage and Cerebral Infarction: A Prospective Study. Hypertension. 2017;70:508–514. doi: 10.1161/HYPERTENSIONAHA.117.09479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang S, Li J, Shearer GC, Lichtenstein AH, Zheng X, Wu Y, et al. Longitudinal study of alcohol consumption and HDL concentrations: a community-based study. Am J Clin Nutr. 2017;105:905–912. doi: 10.3945/ajcn.116.144832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma C, Pavlova M, Liu Y, Liu Y, Huangfu C, Wu S, et al. Probable REM sleep behavior disorder and risk of stroke: A prospective study. Neurology. 2017;88:1849–1855. doi: 10.1212/WNL.0000000000003902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103. doi: 10.1038/sj.jhh.1001307. [DOI] [PubMed] [Google Scholar]
- 21.Wu Z, Jin C, Vaidya A, Jin W, Huang Z, Wu S, et al. Longitudinal Patterns of Blood Pressure, Incident Cardiovascular Events, and All-Cause Mortality in Normotensive Diabetic People. Hypertension. 2016;68:71–7. doi: 10.1161/HYPERTENSIONAHA.116.07381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berlin KS, Parra GR, Williams NA. An Introduction to Latent Variable Mixture Modeling (Part 2): Longitudinal Latent Class Growth Analysis and Growth Mixture Models. Journal of Pediatric Psychology. 2014;39:188–203. doi: 10.1093/jpepsy/jst085. [DOI] [PubMed] [Google Scholar]
- 23.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods & Research. 2007;35:542–571. doi: 10.1177/0049124106292364. [DOI] [Google Scholar]
- 24.Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733. doi: 10.1136/bmjopen-2013-003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Micha R, Penalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association Between Dietary Factors and Mortality From Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA. 2017;317:912–924. doi: 10.1001/jama.2017.0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernstein AM, Willett WC. Trends in 24-h urinary sodium excretion in the United States, 1957–2003: a systematic review. Am J Clin Nutr. 2010;92:1172–80. doi: 10.3945/ajcn.2010.29367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014;4:e004549. doi: 10.1136/bmjopen-2013-004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. doi: 10.1136/bmj.f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mills KT, Chen J, Yang W, Appel LJ, Kusek JW, Alper A, et al. Sodium Excretion and the Risk of Cardiovascular Disease in Patients With Chronic Kidney Disease. JAMA. 2016;315:2200–10. doi: 10.1001/jama.2016.4447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–11. doi: 10.1056/NEJMoa1311989. [DOI] [PubMed] [Google Scholar]
- 31.Zhang FL, Guo ZN, Wu YH, Liu HY, Luo Y, Sun MS, et al. Prevalence of stroke and associated risk factors: a population based cross sectional study from northeast China. BMJ Open. 2017;7:e015758. doi: 10.1136/bmjopen-2016-015758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clark JL, Rech L, Chaity N, Sihag J, Taylor CG, Aliani M. Possible deleterious hormonal changes associated with low-sodium diets. Nutr Rev. 2015;73:22–35. doi: 10.1093/nutrit/nuu003. [DOI] [PubMed] [Google Scholar]
- 33.Hummel SL, Seymour EM, Brook RD, Kolias TJ, Sheth SS, Rosenblum HR, et al. Low-sodium dietary approaches to stop hypertension diet reduces blood pressure, arterial stiffness, and oxidative stress in hypertensive heart failure with preserved ejection fraction. Hypertension. 2012;60:1200–6. doi: 10.1161/HYPERTENSIONAHA.112.202705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jain S, Khera R, Corrales-Medina VF, Townsend RR, Chirinos JA. “Inflammation and arterial stiffness in humans”. Atherosclerosis. 2014;237:381–90. doi: 10.1016/j.atherosclerosis.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Lee H, Cho HJ, Bae E, Kim YC, Kim S, Chin HJ. Not salt taste perception but self-reported salt eating habit predicts actual salt intake. J Korean Med Sci. 2014;29(Suppl 2):S91–6. doi: 10.3346/jkms.2014.29.S2.S91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Inaba Y, et al. Salt preference and mortality from stroke and coronary heart disease for Japanese men and women: the JACC study. Prev Med. 2012;54:32–7. doi: 10.1016/j.ypmed.2011.10.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.