Abstract
PURPOSE
Ultrasound examinations are currently being implemented in general practice. This study aimed to systematically review the literature on the training in and use of point-of-care ultrasound (POCUS) by general practitioners.
METHODS
We followed the Cochrane guidelines for conduct and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting. We searched the databases MEDLINE (via PubMed), EMBASE, CINAHL, Web of Science, and Cochrane Central Register of Controlled Trials using the key words ultrasonography and general practice in combination and using thesaurus terms. Two reviewers independently screened articles for inclusion, extracted data, and assessed the quality of included studies using an established checklist.
RESULTS
We included in our review a total of 51 full-text articles. POCUS was applied for a variety of purposes, with the majority of scans focused on abdominal and obstetric indications. The length of training programs varied from 2 to 320 hours. Competence in some types of focused ultrasound scans could be attained with only few hours of training. Focused POCUS scans were reported to have a higher diagnostic accuracy and be associated with less harm than more comprehensive scans or screening scans. The included studies were of a low quality, however, mainly because of issues with design and reporting.
CONCLUSIONS
POCUS has the potential to be an important tool for the general practitioner and may possibly reduce health care costs. Future research should aim to assess the quality of ultrasound scans in broader groups of general practitioners, further explore how these clinicians should be trained, and evaluate the clinical course of patients who undergo scanning by general practitioners.
Key words: ultrasonography, diagnostic imaging, screening, general practice, point-of-care testing, primary care, practice-based research
INTRODUCTION
Point-of-care ultrasound (POCUS) is described as the stethoscope of the future1 and is being implemented across the medical field by clinicians for bedside examination of patients.1–3 Evidence supports the idea that adding POCUS to the examination of selected patients leads to improved and earlier diagnosis in a hospital setting.4–7 As a result, POCUS has been integrated into the curriculum in several medical schools8,9 and medical specialist training programs.10,11
General practitioners are increasingly using POCUS in patient care.11–13 Evidence from hospital settings cannot be directly transferred to general practice because of differences in the patient population and disease prevalence, and the limited time for consultations in general practice.14,15 The use of ultrasonography is user dependent and requires appropriate training and quality assurance to ensure safety. Misinterpretations may lead to flawed diagnoses that could raise unnecessary concern in patients, and potentially delay proper treatment if a serious condition is overlooked. Currently, there is a lack of any systematic synthesis of evidence in the literature on POCUS use among general practitioners.
The primary objective of this study was to systematically review and synthesize the published literature regarding the use of ultrasonography by general practitioners and their training in its use. We aimed to identify which medical indications ultrasonography was used for, general practitioners’ training, the quality of the scans performed, the frequency of use, the time required, potential harms, patient satisfaction, and financial costs associated with ultrasonography performed by general practitioners in practice or in training.
METHODS
The reporting of this study follows PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). The review was prospectively registered in the PROSPERO international prospective register of systematic reviews (CRD42016038302).
Search Strategy
The literature search was conducted in May 2016 and updated in August 2017 by a medical librarian in 5 databases: MEDLINE via PubMed, EMBASE via OVID, CINAHL via Ebsco, Web of Science, and Cochrane Central Register of Controlled Trials (CENTRAL).
We used the key words ultrasonography and general practice and synonyms in combination (Supplemental Appendix 1, available at http://www.AnnFamMed.org/content/17/1/61/suppl/DC1/). We made no restrictions regarding the year of publication, publication type, setting, or patient population.
Inclusion Criteria
To be included, studies had to describe ultrasound examinations performed by general practitioners or general practitioners in training. General practitioners were defined as medical doctors working in hospitals or outpatient settings as general practitioners, family physicians, or primary care doctors. General practitioners in training were defined as postgraduate medical doctors working as residents in the field of family medicine.
No restrictions were made on setting or patient population. Articles describing referrals for ultrasound examination or thermal therapeutic ultrasound, and articles describing ultrasound without production of an image for the clinician to view were all excluded. Articles not published in Danish, English, Norwegian, or Swedish were also excluded.
If it was unclear from the full-text review who performed the ultrasound, we contacted the author. When there was no reply, the article was excluded.
Data Extraction and Synthesis
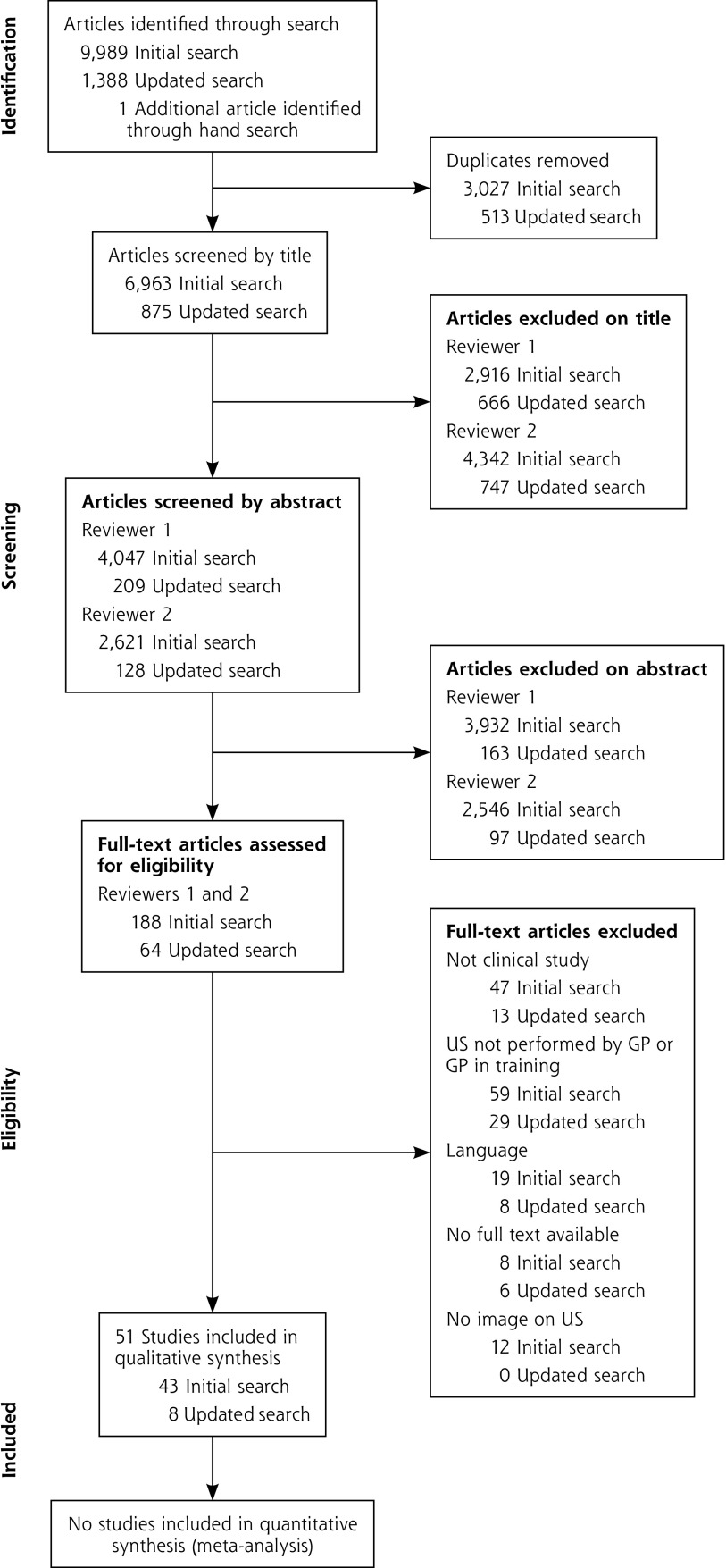
Two reviewers (C.A.A. and S.H. in the original search; C.A.A. and M.B.J. in the updated search) independently screened the articles (Figure 1). Any conflicts were discussed, and a third reviewer (M.B.J.; S.H.) was available in cases where consensus on inclusion could not be reached. Data were independently extracted and quality was assessed by 2 reviewers (C.A.A. and Dr Pia Sterling Haugen; C.A.A. and M.B.J.) using an adapted version of the Cochrane data extraction form (Supplemental Appendix 2, available at http://www.AnnFamMed.org/content/17/1/61/suppl/DC1) and the quality assessment checklist of Downs and Black,16 respectively. As the included studies were noninterventional, items 19, 21 to 24, and 27 were excluded from the checklist, leaving a scale from 1 to 21. Inconsistencies were resolved through discussions involving 2 extra reviewers (S.H. and M.S.R.).
Figure 1.
PRISMA flow diagram.
GP = general practitioner; PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses; US = ultrasound.
The results were synthesized narratively because we expected considerable heterogeneity among the included studies.
RESULTS
The initial literature search identified 6,963 nonduplicate articles and the updated search identified another 875 articles (Figure 1). Ultimately, 51 articles17–67 were included.
The articles originated from 18 countries, with 16 publications from the United States and 10 from Norway. (See Supplemental Appendix 3, available at http://www.AnnFamMed.org/content/17/1/61/suppl/DC1, for details on the included articles.) Only 18 of the 51 articles were less than 10 years old. Nearly all studies were observational, with only 1 randomized controlled trial among them. The studies included 1 to 180 general practitioners, 1 to 90 clinics, and 3 to 9,959 patients. The quality of the articles varied from 5 to 20 points on the 21-point checklist modified from Downs and Black,16 with a mean of 11.9 points (Supplemental Appendix 3). The main problems with quality were design issues and poor reporting.
Use of Ultrasonography
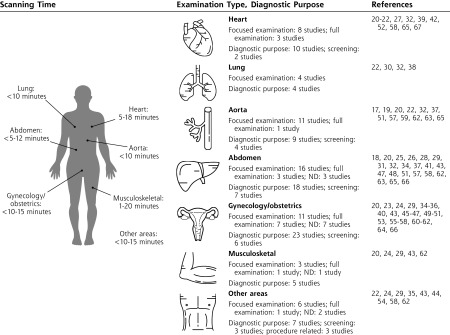
Ultrasonography was used for diagnostic purposes (43 studies); procedure-related purposes, such as aspiration (3 studies); and screening, for example, during general health check-ups (16 studies). Figure 2 shows the examined anatomic areas, whereas Supplemental Appendix 4 (available at http://www.AnnFamMed.org/content/17/1/61/suppl/DC1) provides a full description of the organs scanned. Abdominal, obstetric, and heart examinations were the most common. Only 41 articles provided a detailed description of the scanning procedure: 31 described a focused POCUS, for example, an examination for a specific condition, and 10 described full, detailed examinations. Consequently, there were notable variations in the time used for the ultrasound examination (Figure 2). Detailed ultrasound examinations were reported to last up to 5 minutes longer than focused POCUS (Supplemental Appendix 4). Still, most articles reported a procedure duration of less than 10 minutes.
Figure 2.
Use of ultrasound examinations by anatomic area.
ND = not described.
Note: Icons made by Freepik from www.flaticon.com.
Frequency of Use
Five articles provided an estimation of the frequency of ultrasonography use for broad application in a general practice setting.24,29,43,62,66 These estimations ranged from 131 to 601 ultrasound examinations per general practitioner annually. For obstetric use only, the frequency was described as 72 scans,36 99 scans,45 and 133 scans56 per general practitioner annually. For abdominal,37 urinary tract,48 and broad screening58 examinations, the frequencies were 58 scans, 100 scans, and 43 scans per general practitioner annually, respectively.
Training in Use
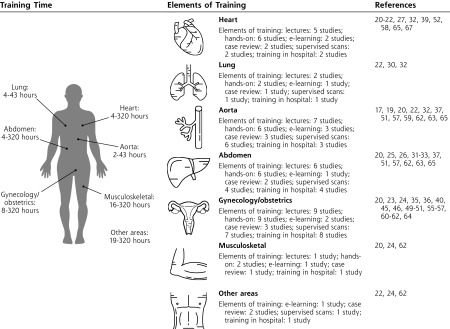
Training of general practitioners in ultrasound examinations was described in 33 out of the 51 articles. Typically, training programs included several elements, such as theoretical sessions, hands-on practice, and supervised scans (Figure 3). These elements varied extensively in time and scope between studies.
Figure 3.
Training in ultrasound examinations by anatomic area.
Note: Icons made by Freepik from www.flaticon.com.
When ultrasonography was applied for more than 1 anatomic area,* the training time varied from 4 to 320 hours depending on the level of detail of the examinations. For focused POCUS examinations, practitioners received 2.3 to 31 hours of training.
Quality of Scans
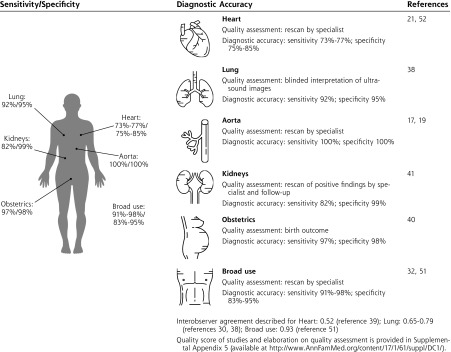
Scanning proficiency after training was assessed by supervision in 12 studies,† by a review of still pictures or video sequences in 2 studies,19,51 and by an examination or certification in 12 studies.‡ An evaluation of the quality of general practitioners’ ultrasound scans was described in 38 publications. Only 28 of these provided an estimate of scan quality, however (Supplemental Appendix 5, available at http://www.AnnFamMed.org/content/17/1/61/suppl/DC1). Nine articles estimated the diagnostic accuracy of ultrasonography in the hands of general practitioners in practice or in training (Figure 4). Ultrasonography used for examining the aorta or lungs, or for obstetric conditions had a higher diagnostic accuracy than ultrasonography used for heart or abdominal examinations. The quality estimate was higher in stud ies with focused abdominal POCUS scans (ie, scans limited to answering specific clinical questions,32,51 such as whether ascites was present) than in studies entailing more explorative examinations.47,57,58 Limited cardiac examinations20,52 also had a higher quality estimate than more extensive examinations.27,39,67 Several articles17,63,64 have reported an improvement in diagnostic accuracy of ultrasonography with training, but we found no overall association between the amount of training and diagnostic accuracy (Supplemental Appendix 5).
Figure 4.
Diagnostic accuracy of ultrasound examinations by anatomic area.
Note: Icons made by Freepik from www.flaticon.com.
Harms
Diagnoses of conditions not actually present (false-positives) were reported in 9 studies and reported to occur in 4.0% to 33.3% of all cardiac examinations,27,39,67 in 0.7% to 3.2% of obstetric examinations,23,45,50 and in 0.5% to 9.9% of abdominal examinations.26,32,37 Higher proportions of false-positive findings were found in screening studies of the carotid artery (18.0%)54 and aorta (21.4%),59 and in broad health-check screenings (9.7% to 12.1%).57,58 Additionally, a screening study for renal cell carcinoma found 93% of detected cases to be falsely positive.41
Nine articles* reported incidental findings on abdominal ultrasonography. Overall, the rate varied widely. The lowest rate (0.05%) was seen in an article describing focused POCUS in symptomatic patients,32 whereas the highest rates (18.1% to 25.7%) were seen in studies screening asymptomatic patients.41,57,58 Additionally, 1 article describing obstetric ultrasonography reported incidental findings in 1.2% of cases.40
Seven studies26,32,41,55–58 described overlooked conditions (false-negatives), with the rate ranging from 0.02% to 2.3%. One study, however, described a false-negative rate of 8.7% in cardiac examinations.39
Patient Perspective
Five articles37,43,47,57,66 reported results regarding the patient perspective. In a study using telemedicine with ultrasonography, the investigators reported, “The patients found the interaction pleasant, innovative and useful. Most would have had no reservations about undergoing the same procedure again and saw benefits to them in terms of quicker treatment and access to additional expertise.”47 In a screening study for abdominal pathology, the investigators reported that no patients found ultrasonography time-consuming, stressful, uncomfortable, or embarrassing; 69% were satisfied or very satisfied with the procedure, and 56% reported that the screening gave them a sense of security about their health.57 Sixty-six percent felt that it should be performed during routine physical examination.
Two studies37,66 undertaken in rural areas found that patients preferred having ultrasonography locally, rather than traveling to a specialist. Another article, however, found that patients, more often than general practitioners, reported that ultrasound examinations had led to unnecessary worries, and 29% of patients said that doctors generally emphasized technology too much.43
Financial Aspects
Three studies45,58,66 performed limited economic evaluations and found health care costs were lower with ultrasound use in general practice vs secondary care. Two articles reported that with use of POCUS in primary care, 65.6% of scans32 and 32.1% of scans39 eliminated need for further testing. One study found that 83% of patients were willing to pay extra to have an ultrasound examination performed by the general practitioner.43
DISCUSSION
Findings in Context
This is the first comprehensive systematic review of the use of ultrasonography by general practitioners and general practitioners in training. Our review shows that these physicians use ultrasonography for a variety of conditions, in agreement with a previous review limited to the Polish literature.12 In studies assessing quality, the general practitioners typically scanned with a satisfactory level of accuracy, a finding also reported in a previous scoping review11 and in a recent study regarding deep vein thrombosis.68 We found that quality depended on the extent of the examination and the anatomic area being scanned. Some focused scans had higher levels of diagnostic accuracy, required less training, and were associated with less potential harm, whereas more extensive examinations were associated with lower scan quality and more potential harm. This knowledge is important for determining the curriculum for POCUS in general practice and a corresponding educational program for general practitioners.
A previous review found a range of ultrasonography courses available for general practitioners, butno nationwide tailored ultrasonography training programs.11 Since then, the American Academy of Family Physicians (AAFP) has released a recommended curriculum guideline for developing training programs for family medicine.69 This guideline was developed primarily based on existing evidence from hospital settings and included only a few of the studies described in this review. The AAFP guideline outlines a more extensive curriculum than that described by the studies reviewed here, but limits ultrasonography in family medicine to a focused rule-in test in patients with a high pretest probability of having a specific condition. Our findings support the recommendation for focused examinations.
The AAFP guideline recommends that training programs include didactic education combined with hands-on practice and supervised scans followed by knowledge and skill assessments. It also recommends that training programs quantify the number of POCUS needed before competency is assessed. A great variety of pedagogic approaches were used by studies in our review, including e-learning, lectures, and hands-on teaching (Figure 3). As these methods have not been compared in any studies, strong recommendations for how to train general practitioners to obtain sufficient skills in using POCUS cannot be made. It appears, however, that general practitioners can be trained to do focused scans in selected anatomic areas (eg, the aorta) with a high level of competence after just a few hours of training.17 Other areas (eg, heart and abdominal organs) may require more extensive training (Supplemental Appendix 5 and Figure 3). The quality of ultrasonography performed by general practitioners seems to depend on the type of examination being undertaken rather than the hours of training involved. The extent of training programs must therefore be adapted to the type of examination being taught, and consequently, the number of required ultrasound scans needed to obtain competency will depend on the anatomic area being scanned.
Limitations
We followed Cochrane recommendations for systematic reviews and included all published studies regardless of quality to provide a complete overview of the available literature. As a result, we included only a few high-quality studies. Generally, there was wide variation in the information regarding general practitioners’ training, and lack of detail explicitly describing how organs were scanned. Outcome measures and quality indicators varied considerably, which limited ability to aggregate data.
We systematically examined the literature captured in 5 major databases, which would be expected to include most studies in the field. We included only publications in Danish, English, Norwegian, and Swedish, however (Figure 1). It is therefore possible that we missed some important studies published in other languages.12,70
Most included articles were more than 10 years old, and with advances in technology, the results reported longer than a decade ago may not be applicable today.27,52 Furthermore, there were 2 chronologic periods of interest: one in the 1980s and 1990s, regarding mainly obstetric ultrasound examinations,* and one more recent describing POCUS with portable ultrasound technology.† A large number of articles reported results with only a single or a few general practitioners using ultrasonography. Those results are prone to low external validity, as these dedicated users may not be representative of most general practitioners. Furthermore, many articles described the use of ultrasonography in settings other than general practice, which makes it difficult to transfer the results to the working situation of most general practitioners.
Implications for Practice
Point-of-care ultrasound will probably be increasingly important for general practitioners to augment diagnostics, to choose treatments, and to make decisions about referral. It can be used by general practitioners in practice and in training, but there is an urgent need for further knowledge on how these clinicians should use POCUS in terms of which types of examinations to perform and how to proceed after the scan. A range of examinations were performed in the studies reviewed, and the AAFP guidelines69 suggested even more applications, but not all applications of POCUS can be expected to improve patient care. As this review has shown, some applications require more training than others. Ultrasound is a user-dependent technology, and an unskilled examiner may misinterpret the images obtained, leading to mistreatment. Sufficient training for each application is therefore paramount.
Moreover, some examinations may be associated with more potential harm than others. An increased use of ultrasound imaging may lead to overdiagnosis,71 spurious findings, or detection of clinically unimportant conditions. How to proceed after having scanned a patient is a challenge for general practitioners using POCUS. In this review, misdiagnoses in terms of false-positives and false-negatives were described in 17% and 16% of included studies, respectively, and incidental findings were described in 20%. Misinterpretations or incidental findings may cause anxiety for patients and the need for further examinations, and if POCUS is to replace more extensive examinations in secondary care, there is the risk that overlooked conditions may delay proper treatment. This review indicates that focused examinations may minimize these harms.
Existing POCUS guidelines are based mainly on hospitalized patients and may not apply to general practice.69,72,73 This review suggests that focused examinations within selected anatomic areas are within reach for general practitioners and may reduce health care costs, but to maximize benefits and avoid unnecessary harm, guidelines founded in general practice are needed. Development of future guidelines might benefit from collaborative efforts between general practice associations and associations for specialists such as radiologists.
In sum, ultrasonography is used for many purposes in general practice, obstetrical and abdominal examinations being most frequent. Scan quality seems to depend on anatomic area and extent of the examination. Focused POCUS scans had higher diagnostic accuracy, were associated with less harm, and required less training. The studies reviewed here were of low quality, however. Hence, there is an essential need for further research.
Acknowledgments
We would like to thank Pia Sterling Haugen for assisting with the first data extraction.
Footnotes
Conflicts of interest: authors report none.
To read or post commentaries in response to this article, see it online at http://www.AnnFamMed.org/content/17/1/61.
Funding support: The study is internally funded by the Research Unit for General Practice in Aalborg, Denmark.
Previous presentation: The 20th Nordic Congress of General Practice, June 14-16, 2017; Reykjavík, Iceland.
Supplemental Materials: Available at http://www.AnnFamMed.org/content/17/1/61/suppl/DC1/.
References
- 1.Moore CLCJ, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011; 364(8): 749–757. [DOI] [PubMed] [Google Scholar]
- 2.Dietrich CF, Goudie A, Chiorean L, et al. Point of care ultrasound: A WFUMB position paper. Ultrasound Med Biol. 2017; 43(1): 49–58. [DOI] [PubMed] [Google Scholar]
- 3.Frederiksen CA, Juhl-Olsen P, Sloth E. Advances in imaging: ultrasound in every physician’s pocket. Expert Opin Med Diagn. 2012; 6(3): 167–170. [DOI] [PubMed] [Google Scholar]
- 4.Bhagra A, Tierney DM, Sekiguchi H, Soni NJ. Point-of-care ultrasonography for primary care physicians and general internists. Mayo Clin Proc. 2016; 91(12): 1811–1827. [DOI] [PubMed] [Google Scholar]
- 5.Diprose W, Verster F, Schauer C. Re-examining physical findings with point-of-care ultrasound: a narrative review. N Z Med J. 2017; 130(1449): 46–51. [PubMed] [Google Scholar]
- 6.Chavez MA, Shams N, Ellington LE, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res. 2014; 15: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laursen CB, Sloth E, Lassen AT, et al. Point-of-care ultrasonography in patients admitted with respiratory symptoms: a single-blind, randomised controlled trial. Lancet Respir Med. 2014; 2(8): 638–646. [DOI] [PubMed] [Google Scholar]
- 8.Baltarowich OH, Di Salvo DN, Scoutt LM, et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014; 30(1): 13–19. [DOI] [PubMed] [Google Scholar]
- 9.Galusko V, Khanji MY, Bodger O, Weston C, Chambers J, Ionescu A. Hand-held ultrasound scanners in medical education: A systematic review. J Cardiovasc Ultrasound. 2017; 25(3): 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atkinson P, Bowra J, Lambert M, Lamprecht H, Noble V, Jarman B. International Federation for Emergency Medicine point of care ultrasound curriculum. CJEM. 2015; 17(2): 161–170. [DOI] [PubMed] [Google Scholar]
- 11.Steinmetz P, Oleskevich S. The benefits of doing ultrasound exams in your office. J Fam Pract. 2016; 65(8): 517–523. [PubMed] [Google Scholar]
- 12.Genc A, Ryk M, Suwała M, Zurakowska T, Kosiak W. Ultrasound imaging in the general practitioner’s office – a literature review. J Ultrason. 2016; 16(64): 78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mengel-Jørgensen T, Jensen MB. Variation in the use of point-of-care ultrasound in general practice in various European countries. Results of a survey among experts. Eur J Gen Pract. 2016; 22(4): 274–277. [DOI] [PubMed] [Google Scholar]
- 14.van de Laar FA, Bor H, van de Lisdonk EH. Prevalence of zebras in general practice: Data from the Continuous Morbidity Registration Nijmegen. Eur J Gen Pract. 2008; 14(Suppl 1): 44–46. [DOI] [PubMed] [Google Scholar]
- 15.Irving G, Neves AL, Dambha-Miller H, et al. International variations in primary care physician consultation time: A systematic review of 67 countries. BMJ Open. 2017; 7(10): e017902-2017–017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998; 52(6): 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bailey RP, Ault M, Greengold NL, Rosendahl T, Cossman D. Ultrasonography performed by primary care residents for abdominal aortic aneurysm screening. J Gen Intern Med. 2001; 16(12): 845–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barabas G, Mölstad S. No association between elevated post-void residual volume and bacteriuria in residents of nursing homes. Scand J Prim Health Care. 2005; 23(1): 52–56. [DOI] [PubMed] [Google Scholar]
- 19.Blois B. Office-based ultrasound screening for abdominal aortic aneurysm. Can Fam Physician. 2012; 58(3): e172–e178. [PMC free article] [PubMed] [Google Scholar]
- 20.Bornemann P, Bornemann G. Military family physicians’ perceptions of a pocket point-of-care ultrasound device in clinical practice. Mil Med. 2014; 179(12): 1474–1477. [DOI] [PubMed] [Google Scholar]
- 21.Bornemann P, Johnson J, Tiglao S, et al. Assessment of primary care physicians’ use of a pocket ultrasound device to measure left ventricular mass in patients with hypertension. J Am Board Fam Med. 2015; 28(6): 706–712. [DOI] [PubMed] [Google Scholar]
- 22.Bornemann P. Assessment of a novel point-of-care ultrasound curriculum’s effect on competency measures in family medicine graduate medical education. J Ultrasound Med. 2017; 36(6): 1205–1211. [DOI] [PubMed] [Google Scholar]
- 23.Bratland SZ, Eik-Nes SH. Ultrasonic diagnosis of pregnant women in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 1985; 105(28): 1940–1946. [PubMed] [Google Scholar]
- 24.Bratland SZ, Bjørnstad PG. Ultrasonic diagnosis used in general practice. A summarized evaluation [in Norwegian]. Tidsskr Nor Laegeforen. 1985; 105(28): 1954–1955. [PubMed] [Google Scholar]
- 25.Bratland SZ, Nordshus T. Ultrasonography of the gallbladder in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 1985; 105(28): 1946–1948. [PubMed] [Google Scholar]
- 26.Bratland SZ, Nordshus T. Ultrasonography of the urinary tract in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 1985; 105(28): 1948–1950. [PubMed] [Google Scholar]
- 27.Bratland SZ. Assessment of echocardiography used in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 1985; 105(28): 1988–1990. [Google Scholar]
- 28.Busse R, Hoopmann M, Schwartz FW. Which factors determine the use of diagnostic imaging technologies for gastrointestinal complaints in general medical practice? Int J Technol Assess Health Care. 1999; 15(4): 629–637. [PubMed] [Google Scholar]
- 29.Chan VSP, Piterman L, McCall L. Use of clinical ultrasonography in an Australian suburban family practice: Its indications and findings. Hong Kong Practitioner. 1999; 21(9): 405–415. [Google Scholar]
- 30.Chavez MA, Naithani N, Gilman RH, et al. Agreement between the World Health Organization algorithm and lung consolidation identified using point-of-care ultrasound for the diagnosis of childhood pneumonia by general practitioners. Lung. 2015; 193(4): 531–538. [DOI] [PubMed] [Google Scholar]
- 31.Chebli H, Laamrani El Idrissi A, Benazzouz M, et al. Human cystic echinococcosis in Morocco: Ultrasound screening in the Mid Atlas through an Italian-Moroccan partnership. PLoS Negl Trop Dis. 2017; 11(3): e0005384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Colli A, Prati D, Fraquelli M, et al. The use of a pocket-sized ultrasound device improves physical examination: results of an in- and outpatient cohort study. PLoS One. 2015; 10(3): e0122181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Del Carpio M, Mercapide CH, Salvitti JC, et al. Early diagnosis, treatment and follow-up of cystic echinococcosis in remote rural areas in Patagonia: impact of ultrasound training of non-specialists. PLoS Negl Trop Dis. 2012; 6(1): e1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deutchman ME, Connor P, Hahn RG, Rodney WM. Maternal gallbladder assessment during obstetric ultrasound: results, significance, and technique. J Fam Pract. 1994; 39(1): 33–37. [PubMed] [Google Scholar]
- 35.Dingwall DW, Hogg BS, Knox JD. A portable ultrasound device in general practice—a pilot study. Health Bull (Edinb). 1979; 37(2): 63–66. [PubMed] [Google Scholar]
- 36.Eggebø TM, Dalaker K. Ultrasonic diagnosis of pregnant women performed in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 1989; 109(29): 2979–2981. [PubMed] [Google Scholar]
- 37.Eggebø TM, Sørvang S, Dalaker K. Ultrasonic diagnosis of the upper abdomen performed in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 1990; 110(9): 1096–1098. [PubMed] [Google Scholar]
- 38.Ellington LE, Gilman RH, Chavez MA, et al. ; Lung Ultrasound for Pneumonia Assessment (LUPA) Study Investigators. Lung ultrasound as a diagnostic tool for radiographically-confirmed pneumonia in low resource settings. Respir Med. 2017; 128: 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Evangelista A, Galuppo V, Méndez J, et al. Hand-held cardiac ultrasound screening performed by family doctors with remote expert support interpretation. Heart. 2016; 102(5): 376–382. [DOI] [PubMed] [Google Scholar]
- 40.Everett CB, Preece E. Women with bleeding in the first 20 weeks of pregnancy: value of general practice ultrasound in detecting fetal heart movement. Br J Gen Pract. 1996; 46(402): 7–9. [PMC free article] [PubMed] [Google Scholar]
- 41.Filipas D, Spix C, Schulz-Lampel D, et al. Screening for renal cell carcinoma using ultrasonography: a feasibility study. BJU Int. 2003; 91(7): 595–599. [DOI] [PubMed] [Google Scholar]
- 42.Gillespie ND, Pringle S. A pilot study of the role of echocardiography in primary care. Br J Gen Pract. 1998; 48(429): 1182. [PMC free article] [PubMed] [Google Scholar]
- 43.Glasø M, Mediås IB, Straand J. Diagnostic ultrasound in general practice [in Norwegian]. Tidsskr Nor Laegeforen. 2007; 127(15): 1924–1927. [PubMed] [Google Scholar]
- 44.Greenlund LJS, Merry SP, Thacher TD, Ward WJ. Primary care management of skin abscesses guided by ultrasound. Am J Med. 2017; 130(5): e191–e193. [DOI] [PubMed] [Google Scholar]
- 45.Hahn RG, Ho S, Roi LD, Bugarin-Viera M, Davies TC, Rodney WM. Cost-effectiveness of office obstetrical ultrasound in family practice: preliminary considerations. J Am Board Fam Pract. 1988; 1(1): 33–38. [PubMed] [Google Scholar]
- 46.Hahn RG, Roi LD, Ornstein SM, et al. Obstetric ultrasound training for family physicians. Results from a multi-site study. J Fam Pract. 1988; 26(5): 553–558. [PubMed] [Google Scholar]
- 47.Hussain P, Melville D, Mannings R, Curry D, Kay D, Ford P. Evaluation of a training and diagnostic ultrasound service for general practitioners using narrowband ISDN. J Telemed Telecare. 1999; 5(Suppl 1): S95–S99. [DOI] [PubMed] [Google Scholar]
- 48.Hussain P, Deshpande A, Shridhar P, Saini G, Kay D. The feasibility of telemedicine for the training and supervision of general practitioners performing ultrasound examinations of patients with urinary tract symptoms. J Telemed Telecare. 2004; 10(3): 180–182. [DOI] [PubMed] [Google Scholar]
- 49.Johansen I, Grimsmo A, Nakling J. Ultrasonography in primary health care—experiences within obstetrics 1983-99 [in Norwegian]. Tidsskr Nor Laegeforen. 2002; 122(20): 1995–1998. [PubMed] [Google Scholar]
- 50.Keith R, Frisch L. Fetal biometry: a comparison of family physicians and radiologists. Fam Med. 2001; 33(2): 111–114. [PubMed] [Google Scholar]
- 51.Lindgaard K, Riisgaard L. ‘Validation of ultrasound examinations performed by general practitioners’. Scand J Prim Health Care. 2017; 35(3): 256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mjølstad OC, Snare SR, Folkvord L, et al. Assessment of left ventricular function by GPs using pocket-sized ultrasound. Fam Pract. 2012; 29(5): 534–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morgan WC, Rodney WM, Hahn R, Garr D. Ultrasound for the primary care physician. Applications in family-centered obstetrics. Postgrad Med. 1988; 83(2): 103–107. [DOI] [PubMed] [Google Scholar]
- 54.Okahara A, Sadamatsu K, Matsuura T, Koga Y, Mine D, Yoshida K. Coronary artery disease screening with carotid ultrasound examination by a primary care physician. Cardiol Res. 2016; 7(1): 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ornstein SM, Smith MA, Peggs J, Garr D, Gonzales J. Obstetric ultrasound by family physicians. Adequacy as assessed by pregnancy outcome. J Fam Pract. 1990; 30(4): 403–408. [PubMed] [Google Scholar]
- 56.Rodney WM, Prislin MD, Orientale E, McConnell M, Hahn RG. Family practice obstetric ultrasound in an urban community health center. Birth outcomes and examination accuracy of the initial 227 cases. J Fam Pract. 1990; 30(2): 163–168. [PubMed] [Google Scholar]
- 57.Rosenthal TC, Siepel T, Zubler J, Horwitz M. The use of ultrasonography to scan the abdomen of patients presenting for routine physical examinations. J Fam Pract. 1994; 38(4): 380–385. [PubMed] [Google Scholar]
- 58.Siepel T, Clifford DS, James PA, Cowan TM. The ultrasound-assisted physical examination in the periodic health evaluation of the elderly. J Fam Pract. 2000; 49(7): 628–632. [PubMed] [Google Scholar]
- 59.Sisó-Almirall A, Kostov B, Navarro González M, et al. Abdominal aortic aneurysm screening program using hand-held ultrasound in primary healthcare. PLoS One. 2017; 12(4): e0176877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smith CB, Sakornbut EL, Dickinson LC, Bullock GL. Quantification of training in obstetrical ultrasound: a study of family practice residents. J Clin Ultrasound. 1991; 19(8): 479–483. [DOI] [PubMed] [Google Scholar]
- 61.Strasser RP, Bass MJ. Obstetric ultrasound in family practice: the effect of on-site ultrasound facilities. Can Fam Physician. 1987; 33: 2505–2508. [PMC free article] [PubMed] [Google Scholar]
- 62.Szwamel K, Polanski P, Kurpas D. Experiences of family physicians after a CME ultrasound course. Fam Med Prim Care Rev. 2017; 19(1): 62–69. [Google Scholar]
- 63.Todsen T, Jensen ML, Tolsgaard MG, et al. Transfer from point-of-care ultrasonography training to diagnostic performance on patients—a randomized controlled trial. Am J Surg. 2016; 211(1): 40–45. [DOI] [PubMed] [Google Scholar]
- 64.Weerasinghe S, Mirghani H, Revel A, Abu-Zidan FM. Cumulative sum (CUSUM) analysis in the assessment of trainee competence in fetal biometry measurement. Ultrasound Obstet Gynecol. 2006; 28(2): 199–203. [DOI] [PubMed] [Google Scholar]
- 65.Wong F, Franco Z, Phelan MB, Lam C, David A. Development of a pilot family medicine hand-carried ultrasound course. WMJ. 2013; 112(6): 257–261. [PubMed] [Google Scholar]
- 66.Wordsworth S, Scott A. Ultrasound scanning by general practitioners: is it worthwhile? J Public Health Med. 2002; 24(2): 88–94. [DOI] [PubMed] [Google Scholar]
- 67.Zamorano JL, Moreno R, Alburquerque C. Echocardiography performed by physicians outside of echo-labs – is it possible? Eur Heart J. 2002; 23(11): 908–909. [DOI] [PubMed] [Google Scholar]
- 68.Mumoli N, Vitale J, Giorgi-Pierfranceschi M, et al. ; PRACTICUS Study Investigators. General practitioner-performed compression ultrasonography for diagnosis of deep vein thrombosis of the leg: A multicenter, prospective cohort study. Ann Fam Med. 2017;15(6):535–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.American Academy of Family Physicians. Recommended curriculum guidelines for family medicine residents: point of care ultrasound. AAFP Reprint No. 290D https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf. Published Dec 2016 Accessed Apr 27, 2018.
- 70.Reports from the Spanish Agency for Health Technology Assessment (AETS). Ultrasonography in primary health care. Int J Technol Assess Health Care. 1999; 15(4): 773–777. [PubMed] [Google Scholar]
- 71.Shabanzadeh DM, Sørensen LT, Jørgensen T. A prediction rule for risk stratification of incidentally discovered gallstones: Results from a large cohort study. Gastroenterology. 2016; 150(1): 156–167.e1. [DOI] [PubMed] [Google Scholar]
- 72.Volpicelli G, Elbarbary M, Blaivas M, et al. ; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38(4): 577–591. [DOI] [PubMed] [Google Scholar]
- 73.Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013; 26(6): 567–581. [DOI] [PubMed] [Google Scholar]