Abstract
Coronary high-intensity plaques (HIPs) visualized by non-contrast T1-weighted imaging (T1WI) in cardiac magnetic resonance (CMR) are associated with slow-flow phenomena during percutaneous coronary intervention (PCI). We report a case of a 52-year-old man who had undergone left anterior descending artery stent implantation for unstable angina 5 years previously. He underwent CMR imaging for screening of vulnerable plaques. A lesion in the proximal right coronary artery showed HIP on non-contrast T1WI. Invasive coronary angiography showed progressive stenosis and PCI was performed. Non-contrast T1WI indicated a high risk for a slow-flow phenomenon. A distal protection device (Parachute™ (Tri-Med, Osaka, Japan)) was deployed at the distal site of the lesion. Following balloon dilation, a filter no-reflow phenomenon developed. Coronary flow was improved with removal of the Parachute™ after debris aspiration. Histological examination revealed aspirated debris composed of white thrombi, foamy macrophages, and cholesterol crystals.
<Learning objective: Although optimal medical therapy has improved the prognosis of patients with acute coronary syndrome, recurrent major adverse cardiovascular events occur in a substantial proportion of patients. Non-contrast T1-weighted imaging is a valuable tool for use in screening of vulnerable plaque and prediction of slow-flow phenomenon during percutaneous coronary intervention.>
Keywords: Non-contrast T1-weighted imaging, High-intensity plaque, Screening of vulnerable plaque, Slow-flow phenomenon
Introduction
Recent studies have shown that coronary high-intensity plaques (HIPs) visualized by non-contrast T1-weighted imaging (T1WI) in cardiac magnetic resonance (CMR) were associated with coronary events and percutaneous coronary intervention-related myocardial injury [1], [2], [3]. Despite successful revascularization and implementation of secondary prevention strategies, major adverse cardiovascular events (MACE) still occur in approximately one-quarter of patients with acute coronary syndrome (ACS) [4]. We report a case by which non-contrast T1WI was useful in the screening of vulnerable plaque and in the strategy of percutaneous coronary intervention (PCI).
Case report
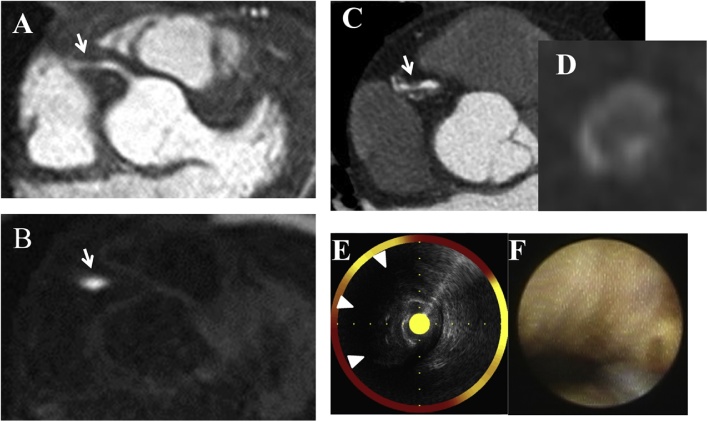
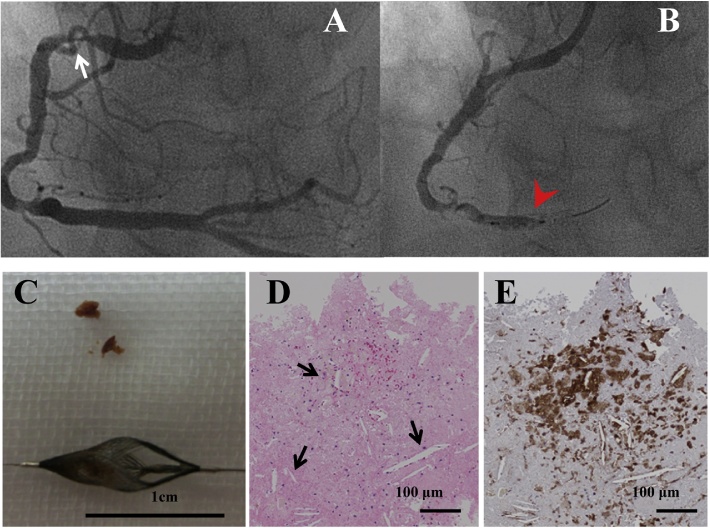
The present case involved a 52-year-old man who underwent left anterior descending artery stent implantation for unstable angina 5 years previously and CMR imaging for screening of vulnerable plaques without chest pain. Whole-heart coronary magnetic resonance (MR) angiography using a 1.5-T MR imager (Magnetom Aera, Siemens Healthcare, Munich, Germany), showed moderate stenosis in the proximal right coronary artery (RCA) (Fig. 1A). The procedures used to acquire MR images have been previously described [5]. The signal intensity of coronary plaque to muscle ratio (PMR) was calculated (PMR was defined as the signal intensity of the coronary plaque divided by the signal intensity of the left ventricular muscle near the coronary plaque). Moderate stenosis in the RCA showed HIP (PMR = 4.1) on non-contrast T1WI (Fig. 1B). Coronary computed tomography (CT) showed significant stenosis with napkin-ring sign plaque (Fig. 1C and D). Invasive coronary angiography (CAG) showed progressive severe stenosis compared to that 5 years previously (Fig. 2A). He continued to take aspirin, angiotensin II receptor blocker, β-blocker, statin, and ezetimibe. His low-density lipoprotein cholesterol was 45 mg/dl. Despite optimal medical therapy and cardiac rehabilitation, the lesion had progressed. An exercise electrocardiogram revealed significant ST-segment depression on treadmill stress test and PCI was performed. Coronary angioscopy revealed yellow plaque without red thrombus (Fig. 1F). Near-infrared spectroscopy intravascular ultrasonography (NIRS-IVUS) revealed attenuated plaques composed of thrombus and lipid components (Fig. 1E). The lesion had a maximum lipid-core burden index on NIRS-IVUS of 583. Non-contrast T1WI and NIRS-IVUS findings indicated a high risk for slow-flow phenomenon. After pre-dilation using 2.0 × 15 mm balloon catheter, a distal protection device (Parachute™ (Tri-Med, Osaka, Japan)) was deployed at the distal site of the lesion. Following balloon dilation using Lacrosse® NSE 3.5 × 13 mm (Goodman, Japan), filter no-reflow phenomenon developed (Fig. 2B). Coronary flow improved by removing the Parachute™ after thrombus aspiration, and Synergy™ 3.5 × 16 mm (Boston Scientific; Natick, Massachusetts, United States) stent implantation was performed. Finally, thrombolysis in myocardial infarction flow grade 3 was achieved. Histological examination revealed aspirated debris (Fig. 2C) composed of white thrombi, foamy macrophages, and cholesterol crystals (Fig. 2D and E).
Fig. 1.
(A) Whole-heart coronary magnetic resonance angiography showed moderate stenosis (arrow). (B) Plaque-to-myocardium signal intensity ratio of 4.1 on T1-weighted imaging was apparent (arrow). (C) Coronary computed tomography (CT) showed significant stenosis with positive vessel remodeling (arrow). (D) Cross-sectional CT showed napkin-ring sign plaque. (E) Near-infrared spectroscopy intravascular ultrasonography revealed attenuated plaque (arrowhead). (F) Angioscopy revealed dense yellow plaque without red thrombus.
Fig. 2.
(A) Invasive coronary angiography showed severe stenosis. (B) Filter no-reflow phenomenon developed. (C) Retrieved debris was yellowish brown. (D) Hematoxylin-eosin staining showed numerous cholesterol clefts (arrow). (E) Immunohistochemistry showed extensive infiltration of CD68 + macrophages.
Discussion
Although optimal medical therapy has improved the prognosis of patients with acute coronary syndrome, recurrent MACE occur in a substantial proportion of patients [4]. Follow-up studies using intravascular imaging techniques in patients with ACS have shown that a substantial number of second events arise from these non-culprit plaques [6]. Coronary CT angiography study has shown that a quarter of patients with ACS experienced a second event arising from a non-culprit plaque during 5-year follow-up [7]. We were able to detect a new vulnerable plaque by using non-contrast T1WI in a patient who had experienced ACS 5 years before. Non-contrast T1WI noninvasively enables the detection of the vulnerable plaque leading to ACS and aids in carrying out PCI strategy.
The presence of HIP on non-contrast T1WI has the potential to predict a PCI-related myocardial injury, which is associated with worse short-term and long-term clinical outcomes [2], [3]. Slow-flow or no-reflow phenomenon is one of the serious complications of PCI and is an independent predictor of myocardial infarction and in-hospital and long-term mortality [8], [9]. Plaque imaging information obtained before PCI may allow preparation for the appropriate distal protection device to prevent complications. However, the incidence of no-reflow phenomenon in elective PCI varies between 2% and 5% [10], therefore, we usually do not prepare for the treatment of no-reflow phenomenon in elective cases. In this case, since the PMR of the lesion was very high, we could avoid no-reflow phenomenon with the distal protection device before balloon dilation. Non-contrast T1WI is a valuable tool for use in screening of vulnerable plaque and prediction of slow-flow phenomenon.
Conflict of interest
There is no conflict of interest to declare.
References
- 1.Noguchi T., Kawasaki T., Tananka A., Yasuda S., Goto Y., Ishihara M. High-intensity signals in coronary plaques on noncontrast T1-weighted magnetic resonance imaging as a novel determinant of coronary events. J Am Coll Cardiol. 2014;63:989–999. doi: 10.1016/j.jacc.2013.11.034. [DOI] [PubMed] [Google Scholar]
- 2.Hoshi T., Sato A., Akiyama D., Hiraya D., Sakai S., Shindo M. Coronary high-intensity plaque on T1-weighted magnetic resonance imaging and its association with myocardial injury after percutaneous coronary intervention. Eur Heart J. 2015;36:1913–1922. doi: 10.1093/eurheartj/ehv187. [DOI] [PubMed] [Google Scholar]
- 3.Asaumi Y., Noguchi T., Morita Y., Fujiwara R., Kanaya T., Matsuyama T.A. High-intensity plaques on noncontrast T1-weighted imaging as a predictor of periprocedural myocardial injury. J Am Coll Cardiol. 2015;8:741–743. doi: 10.1016/j.jcmg.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Cannon C.P., Braunwald E., McCabe C.H., Rader D.J., Rouleau J.L., Belder R. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–1504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- 5.Oshita A., Kawakami H., Miyoshi T., Seike F., Matsuoka H. Characterization of high-intensity plaques on noncontrast T1-weighted magnetic resonance imaging by coronaryangioscopy. J Cardiol. 2017;70:520–523. doi: 10.1016/j.jjcc.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Stone G.W., Maehara A., Lansky A.J., de Bruyne B., Cristea E., Mintz G.S. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–235. doi: 10.1056/NEJMoa1002358. [DOI] [PubMed] [Google Scholar]
- 7.Dedic A., Kurata A., Lubbers M., Meijboom W.B., van Dalen B.M., Snelder S. Prognostic implications of non-culprit plaques in acute coronary syndrome: non-invasive assessment with coronary CT angiography. Eur Heart J Cardiovasc Imaging. 2016;17:1231–1237. doi: 10.1093/ehjci/jew002. [DOI] [PubMed] [Google Scholar]
- 8.Brosh D., Assali A.R., Mager A., Porter A., Hasdai D., Teplitsky I. Effect of no-reflow during primary percutaneous coronary intervention for acute myocardial infarction on six-month mortality. Am J Cardiol. 2007;99:442–445. doi: 10.1016/j.amjcard.2006.08.054. [DOI] [PubMed] [Google Scholar]
- 9.Resnic F.S., Wainstein M., Lee M.K., Behrendt D., Wainstein R.V., Ohno-Machado L. No-reflow is an independent predictor of death and myocardial infarction after percutaneous coronary intervention. Am Heart J. 2003;145:42–46. doi: 10.1067/mhj.2003.36. [DOI] [PubMed] [Google Scholar]
- 10.Salinas P., Jimenez-Valero S., Moreno R., Sanchez-Recalde A., Galeote G., Calvo L. Update in pharmacological management of coronary no-reflow phenomenon. Cardiovasc Hematol Agents Med Chem. 2012;10:256–264. doi: 10.2174/187152512802651024. [DOI] [PubMed] [Google Scholar]