Abstract
Background
Patients with acute coronary syndrome (ACS), including ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation (NSTE)-ACS have a significant risk of morbidity and mortality. This study evaluated the practice patterns of ACS care in Taiwan from 2005 to 2018.
Methods
Data from two nationwide ACS registries (2008-2010 and 2012-2015) were used. ACS patients who received percutaneous coronary interventions (PCIs) during admission were compared between the two registries.
Results
In STEMI, the door-to-balloon time for primary PCI decreased by 25 min from a median of 96 to 71 min (p < 0.0001) from the first to second registry. More complex PCI procedures and drug-eluting stents were used for ACS. However, the onset-to-door time was still long for both STEMI and NSTE-ACS. The D2B time for NSTE-ACS was long, especially in the elderly and female patients. Although the prescription rate of secondary preventive medications for ACS increased, it was still relatively low compared with Western data, especially in NSTE-ACS.
Conclusions
The registry data showed that ACS care quality has improved in Taiwan. However, areas including onset-to-door time and use of secondary preventive medications still need further improvements.
Keywords: Acute coronary syndromes, Quality, Taiwan
INTRODUCTION
Despite recent advances, acute coronary syndrome (ACS) still carries significant morbidity and mortality. In Taiwan, the overall incidence of acute myocardial infarction (MI) increased from 30 to 42 per 100,000 population from 1997 to 2011, mainly due to increases in non-ST segment elevation (NSTE) MI.1,2 Rapid diagnosis, timely percutaneous coronary intervention (PCI) and adequate pharmacological therapies are the mainstays of treatment for ACS. Current evidence favors using rapid primary PCI as the initial reperfusion strategy for acute ST segment elevation MI (STEMI). Secondary preventive medications for ACS, including dual antiplatelet therapy (DAPT), beta blockers, angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) and statins have been proved to decrease morbidity and mortality. All of these treatments are recommended in the clinical guidelines3-5 and form the standard of care for ACS. However, a significant gap exists between the guideline recommendations and real-world practice for ACS treatment due to substantial variations in health care systems and spending around the world. In the United States, health care is provided by many different public or private organizations, and only about 64% of the costs were paid by the government in 2013.6 The health care system in Taiwan (the National Health Insurance program) is a single-payer compulsory insurance plan which is administered by the Ministry of Health and Welfare of the Taiwanese government for all hospitals, and covers almost all of the 23 million people in this country. The average cost of each hospitalization for acute MI in Taiwan is only about one third of that in the United States.7,8 Revascularization is increasingly used for ACS treatment in Taiwan. Overall, fibrinolysis is given to only 0.3% of the patients with STEMI, and the rate of PCI has increased markedly from 23% in 1997 to 82% in 2011 for STEMI treatment in Taiwan.2 For patients with NSTEMI, revascularization procedures have also increased from 10% in 1997 to 56% in 2011.2 In Taiwan, the crude in-hospital mortality rate from acute MI gradually improved from 9.1% in 1997 to 6.5% in 2011, but there was no further reduction in mortality after 2004.2 From 2008 to 2009, the prescription rate of secondary preventive medications after MI was also low in Taiwan.9 The Taiwanese government initiated a national audit project from 2009 to evaluate the care quality of ACS in hospitals. In order to understand the practice patterns of ACS in Taiwan, the Taiwan Society of Cardiology established two nationwide ACS registries in different time periods. The purpose of the present study was to evaluate the changes in in-hospital ACS management between the two ACS registries. The performance indicators of ACS treatment were specifically compared.
METHODS
Study population
Two nationwide ACS registries were established in Taiwan by the Taiwan Society of Cardiology. The first registry covered the period from October 2008 to January 2010 and included 39 major hospitals around the country.9,10 Adult ACS patients (age ≥ 20 years old) who presented with ACS symptoms and were admitted within 24 hours to the participating hospitals were included. The diagnosis of ACS depended on the clinical symptoms, electrocardiography (ECG) and changes in cardiac markers. Creatine kinase (CK) MB and cardiac troponin are the most commonly used cardiac markers in Taiwan. STEMI was diagnosed if the patients had ischemic symptoms, ST segment elevation on ECG and increased cardiac markers. All of the other ACS patients including those with NSTEMI and unstable angina were categorized as having NSTE-ACS in this study. The diagnoses were made by the in-charge cardiologists at each participating site according to the appropriate guidelines.3-5 Trauma or procedure-induced cardiac injury and patients enrolled in other investigational drug clinical trials were not included. The second registry covered the period from April 2012 to December 2015 and included 24 hospitals which participated in the first registry. The inclusion criteria were the same as the first registry except that only ACS patients who received PCI with stent implantation during hospitalization were included in the second registry. In the two registries, the clinical data including age, gender, vascular risk factors, previous disease history, clinical presentations, laboratory data, medications and procedures used during the index admission were collected for each patient. The onset-to-door time, door-to-ECG time and door-to-balloon (D2B) time were recorded in each patient. Onset-to-door time was defined as the time between first symptom onset described by the patients or families and the patients’ arrival at the participating hospital that recruited the case. Door-to-ECG time was defined as the time between the patients’ arrival at the hospital and initial ECG acquisition. D2B time was defined as the time between the patients’ arrival at the hospital and balloon inflation during PCI. In subgroup analysis, elderly patients were defined as those aged ≥ 75 years. Anterior MI was diagnosed by the in-charge cardiologists according to clinical pictures and ECG changes. The study protocol was approved by the institutional ethics committee at each participating hospital. The study was carried out in accordance with local regulatory guidelines as well as international guidelines for Good Epidemiological Practice.
Statistical analysis
Continuous and categorical variables were presented with medians (interquartile ranges), means (standard deviations) or numbers (percentages), respectively. Comparisons were performed using the unpaired Student t test or Wilcoxon rank sum test for continuous variables, and the chi-square or Fisher’s exact test for categorical variables as appropriate. Significance was set at p < 0.05 (2-tailed). SAS statistical software (version 9.2 for Windows; SAS Institute, Cary, NC, USA) was used for all analyses.
RESULTS
Overall, the first registry enrolled 3183 ACS patients, of whom 2399 underwent PCI with stent implantation during hospitalization. These 2399 patients (STEMI, n = 1424, NSTE-ACS, n = 975) were compared with 2357 patients (STEMI, n = 1295, NSTE-ACS, n = 1062) recruited in the second registry.
STEMI patients
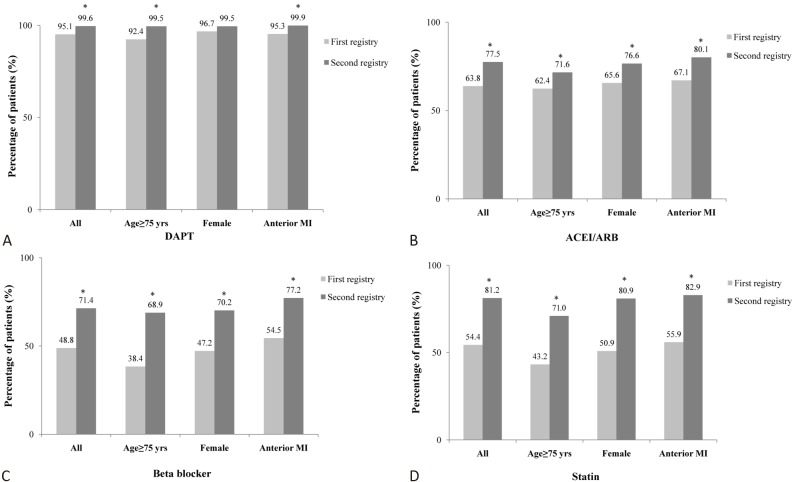
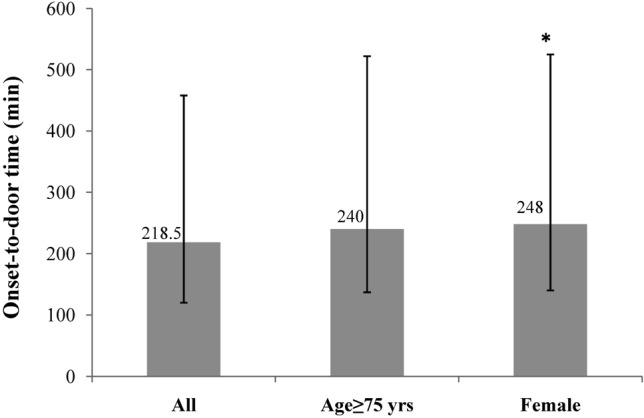
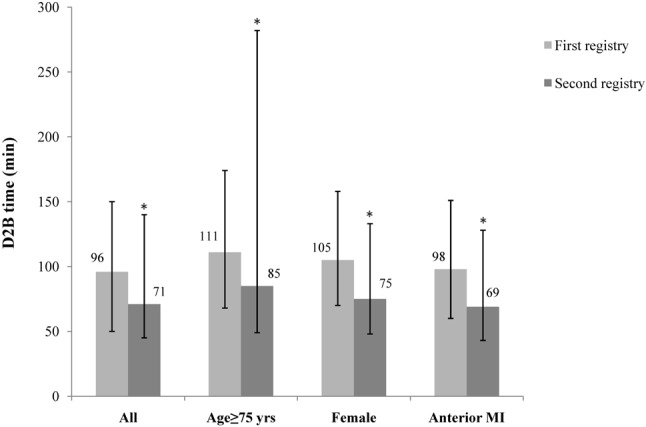
Table 1 shows the clinical characteristics of the STEMI patients in the two registries. Age, gender and risk factors were similar between the two registries, except that there was a higher rate of hyperlipidemia and a higher baseline level of low density lipoprotein cholesterol in the second registry. The patients in the second registry also had a higher rate of prior stroke, higher left ventricular ejection fraction, lower creatinine level, and shorter duration of admission. The onset-to-door time in the STEMI patients was long, with median times of 266 min and 172 min, respectively, (p < 0.0001) in the two registries. In all STEMI patients in both registries, the median onset-to-door time was 218.5 min, and there was a trend of a longer onset-to-door time in the elderly patients (240 min; p = 0.093) and women (248 min; p = 0.046) compared to the STEMI patients overall (Figure 1). Overall, only 10.6% of the STEMI patients had an onset-to-door time < 60 min. Table 2 shows the in-hospital management of the STEMI patients. The percentage of STEMI patients with a door-to-ECG time < 10 min increased from 54% to 61.2% (p = 0.0018) from the first to second registry. The median D2B time decreased by 25 min from 96 min in the first registry to 71 min in the second registry (p < 0.0001) with a corresponding increase in the percentage of patients with D2B < 90 min (46.7% to 63.3%, p < 0.0001). Between the two registries, decreases in D2B time were also observed in the elderly patients (median 111 to 85 min, p = 0.0051; percentage of D2B < 90 min 40.1% to 55%, p = 0.0051), women (105 to 75 min, p = 0.0041; 43.3% to 60.9%, p = 0.0013), and those with anterior MI (98 to 69 min, p = 0.0001; 47.3% to 64.8%, p < 0.0001) (Figure 2). The median D2B time was the longest in the elderly patients in both registries (Figure 2). Overall, drug-eluting stents (DESs) were used during primary PCI in 21.6% and 41% of cases in the first and second registry, respectively. Interventions in the left main coronary artery and for multiple lesions both increased. We further stratified D2B time according to onset-to-door time in all STEMI patients in both registries. Table 3 shows that the patients with the longest onset-to-door time (> 6 hours) also had the longest D2B time regardless of age and gender. In pharmacological therapies, the in-hospital use of DAPT (95.1% to 99.6%), ACEIs or ARBs (63.8% to 77.5%), beta blockers (48.8% to 71.4%), and statins (54.4% to 81.2%) all increased significantly (all p < 0.0001) between the two registries (Table 2). The use of these secondary preventive medications also increased among the elderly patients, women and those with anterior MI between the two registries (Figure 3). The elderly patients in both registries had the lowest treatment rate of ACEIs/ARBs, beta blockers and statins (Figure 3).
Table 1. Clinical characteristics of STEMI patients.
| Registry 1 (2008-2010) | Registry 2 (2012-2015) | p value | |
| (n = 1424) | (n = 1295) | ||
| Age (years) | 60.8 ± 13.5 | 60.0 ± 12.7 | 0.1409 |
| Women | 14.9% | 14.5% | 0.7854 |
| BMI (kg/m2) | 25.4 ± 3.8 | 25.5 ± 3.6 | 0.2468 |
| Cardiovascular risk factor | |||
| Current smoker | 52.7% | 52.1% | 0.7503 |
| Hypertension | 55.4% | 56.4% | 0.5725 |
| Diabetes | 28.9% | 28.4% | 0.7556 |
| Hyperlipidemia | 32.9% | 38.6% | 0.0021 |
| Medical history | |||
| Prior stroke | 2.9% | 4.9% | 0.0074 |
| Prior MI | 5.2% | 6.6% | 0.1363 |
| Prior PCI | 8.3% | 8.5% | 0.8583 |
| Prior CABG | 0.8% | 0.4% | 0.1414 |
| Prior HF | 1.5% | 2.3% | 0.1423 |
| PAD | 1.0% | 0.6% | 0.2906 |
| AF | 1.5% | 2.2% | 0.1792 |
| Clinical presentation | |||
| Onset-to-door time (min) | 266 (155-525) | 172 (85-370) | < 0.0001 |
| Transferred in | 30.4% | 29.0% | 0.4319 |
| Cardiac arrest | 1.9% | 2.8% | 0.1183 |
| Killip > 2 | 18.7% | 17.7% | 0.109 |
| Anterior wall | 51.0% | 52.0% | 0.5908 |
| LVEF | 53% | 56% | 0.0019 |
| Laboratory data | |||
| Creatinine (mg/dL) | 1.4 ± 1.5 | 1.2 ± 1.2 | < 0.0001 |
| Cholesterol (mg/dL) | 181.3 ± 46.0 | 180.7 ± 42.8 | 0.6954 |
| Triglyceride (mg/dL) | 138.3 ± 104.5 | 136.6 ± 115.5 | 0.7037 |
| LDL-C (mg/dL) | 116.6 ± 37.5 | 120.5 ± 41.4 | 0.0182 |
| HDL-C (mg/dL) | 39.9 ± 27.6 | 41.1 ± 10.5 | 0.1610 |
| CK (U/L) | 169 (95-448) | 188 (99-650) | 0.0115 |
| CK MB (U/L) | 14 (5.8-34) | 17.1 (4.7-47) | 0.0116 |
| Troponin I | 0.2 (0-2.7) | 0.2 (0-2.8) | 0.7314 |
| Admission days | 6.0 (4-7) | 5.0 (4-6) | < 0.0001 |
The data were presented with medians (interquartile ranges), means ± standard deviations or percentages (%).
AF, atrial fibrillation; BMI, body mass index; CABG, coronary artery bypass grafting; CK, creatine kinase; HDL-C, high density lipoprotein cholesterol; HF, heart failure; LDL-C, low density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PAD, peripheral arterial disease; PCI, percutaneous coronary intervention.
Figure 1.
The median onset-to-door time in all STEMI patients, elderly patients (age ≥ 75 years) and female patients. * p < 0.05 compared with all STEMI patients. STEMI, ST segment elevation myocardial infarction.
Table 2. Interventional and pharmacological therapies during hospitalization of STEMI patients.
| Registry 1 (2008-2010) | Registry 2 (2012-2015) | p value | |
| (n = 1424) | (n = 1295) | ||
| Interventional therapies | |||
| Door to ECG time (min) | 8.0 (4-16) | 6.0 (4-19) | 0.0173 |
| First ECG within 10 min | 54.0% | 61.2% | 0.0018 |
| D2B time (min) | 96 (61-150) | 71 (44-135) | < 0.0001 |
| D2B time < 90 min | 46.7% | 63.3% | < 0.0001 |
| Left main intervention | 1.5% | 2.7% | 0.0243 |
| No. of lesion treated > 2 | 4.9% | 11.9% | < 0.0001 |
| DES | 21.6% | 41.0% | < 0.0001 |
| CABG | 0.1% | 0.2% | 0.9105 |
| Pharmacological therapies | |||
| Aspirin | 95.9% | 99.8% | < 0.0001 |
| Clopidogrel | 98.5% | 99.8% | < 0.0001 |
| Dual antiplatelet therapy | 95.1% | 99.6% | < 0.0001 |
| GP 2b3a inhibitor | 25.4% | 28.7% | 0.0526 |
| Heparin | 85.3% | 93.4% | < 0.0001 |
| ACEI/ARB | 63.8% | 77.5% | < 0.0001 |
| Beta blocker | 48.8% | 71.4% | < 0.0001 |
| Statin | 54.4% | 81.2% | < 0.0001 |
| Calcium channel antagonist | 5.3% | 10.4% | < 0.0001 |
| Nitrate | 62.4% | 51.5% | < 0.0001 |
| Oral anticoagulant | 0.7% | 2.2% | 0.0008 |
The data were presented with medians (interquartile ranges) or percentages (%).
ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; CABG, coronary artery bypass grafting; DES, drug eluting stent; D2B, door-to-balloon; ECG, electrocardiogram; GP, glycoprotein.
Figure 2.
The median D2B time in all STEMI patients, elderly patients (age ≥ 75 years), female patients and anterior MI patients in the first and second registry. * p < 0.05 compared with the first registry. D2B, door-to-balloon; MI, myocardial infarction; STEMI, ST segment elevation myocardial infarction.
Table 3. Door-to-balloon time according to onset-to-door time by sex and age of all STEMI patients in the 2 registries.
| Door-to-balloon time (min) | |||||
| Onset-to-door time (min) | Whole cohort | Men | Women | Age < 75 yrs | Age ≥ 75 yrs |
| < 60 min | 76.5 (53-123) | 76 (53-123) | 91 (61-204) | 76 (52-121) | 98.5 (64-161) |
| 61-180 min | 70 (45-106) | 69 (44-103) | 76 (55-125) | 69 (44-105) | 76 (49-123) |
| 181-360 min | 84 (53-148) | 84.5 (53-145) | 84 (56-152) | 84 (53-138) | 101 (59-174) |
| > 360 min | 113 (62-242) | 113 (62-262) | 96 (63-178) | 109 (60-241) | 123.5 (73-246) |
| p value | < 0.0001 | < 0.0001 | 0.0845 | < 0.0001 | 0.0015 |
The data were presented with medians (interquartile ranges). The p values indicated the comparison of door-to-balloon time in different onset-to-door time groups among whole STEMI patients, men, women and patients with age < or ≥ 75 yrs.
Figure 3.
The percentage of STEMI patients that received DAPT (A), ACEI or ARB (B), beta blocker (C) and statin (D) during hospitalization in the first and second registry. * p < 0.05 compared with the first registry. ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; DAPT, dual antiplatelet therapy; STEMI, ST segment elevation myocardial infarction.
NSTE-ACS patients
Table 4 shows the clinical characteristics of the NSTE-ACS patients. Age and risk factors were similar between the two registries except that there were fewer female patients in the second registry. The second registry also had more patients with prior stroke, peripheral arterial disease and fewer patients with Killip > 2. The duration of admission was also shorter in the second registry. Although there were improvements, the onset-to-door times were long in the NSTE-ACS patients, with medians of 550 and 391 min, respectively, (p < 0.0001) in the two registries, which were much longer than those for the STEMI patients. Table 5 shows the in-hospital management of the NSTE-ACS patients. The percentage of NSTE-ACS patients with a door-to-ECG time < 10 min increased from 35.9% to 48.5% (p < 0.0001). The median D2B times of the NSTE-ACS patients were 2534 min (42.2 hours) and 2003 min (33.4 hours), respectively, in the two registries (p = 0.0048). The median D2B time was longer in the patients aged ≥ 75 years, and there was no improvement between the two registries (55.1 to 46.0 hours, p = 0.2239). For male patients, the D2B time improved from 39.2 hours to 31.4 hours (p = 0.0026), but for female patients, the D2B time was longer than that in the male patients, and there was no significant difference between the two registries (48.4 to 43.2 hours, p = 0.2639). PCIs for left main and multiple lesions increased significantly. The percentages of patients receiving DESs during PCI were 35.1% and 62.9%, respectively, in the two registries. The in-hospital use of DAPT (85.5% to 99.0%), ACEIs or ARBs (58.3% to 67.6%), beta blockers (43.3% to 64.4%) and statins (48.0% to 78.8%) all increased significantly (all p < 0.0001). Compared with the patients with STEMI, those with NSTE-ACS received fewer ACEIs/ARBs (67.6% vs. 77.5%, p < 0.0001) and beta blockers (64.4% vs. 71.4%, p = 0.0003) in the second registry.
Table 4. Clinical characteristics of NSTE-ACS patients.
| Registry 1 (2008-2010) | Registry 2 (2012-2015) | p value | |
| (n = 975) | (n = 1062) | ||
| Age (years) | 64.9 ± 12.8 | 64.0 ± 13.0 | 0.1165 |
| Women | 26.5% | 21.7% | 0.0112 |
| BMI (kg/m2) | 25.7 ± 3.9 | 25.8 ± 4.0 | 0.7766 |
| Cardiovascular risk factor | |||
| Current smoker | 34.8% | 37.4% | 0.2146 |
| Hypertension | 71.0% | 72.7% | 0.5604 |
| Diabetes | 41.4% | 41.6% | 0.9339 |
| Hyperlipidemia | 48.8% | 51.8% | 0.1714 |
| Medical history | |||
| Prior stroke | 5.4% | 7.6% | 0.0441 |
| Prior MI | 12.2% | 12.1% | 0.9524 |
| Prior PCI | 24.5% | 24.6% | 0.9412 |
| Prior CABG | 4.6% | 3.3% | 0.1419 |
| Prior HF | 7.3% | 9.4% | 0.0805 |
| PAD | 2.7% | 4.5% | 0.0247 |
| AF | 3.9% | 4.3% | 0.6195 |
| Clinical presentation | |||
| Onset-to-door time (min) | 550 (279-986) | 391 (133-830) | < 0.0001 |
| Transferred in | 18.4% | 16.9% | 0.3890 |
| Cardiac arrest | 0.8% | 0.7% | 0.6534 |
| Killip > 2 | 22.0% | 14.4% | 0.0022 |
| Anterior wall | 33.5% | 34.0% | 0.8513 |
| LVEF | 56.0 ± 13.2 | 57.4 ± 13.2 | 0.0441 |
| Laboratory data | |||
| Creatinine (mg/dL) | 1.8 ± 2.1 | 1.9 ± 5.3 | 0.7029 |
| Cholesterol (mg/dL) | 180.9 ± 47.8 | 176.5 ± 46.5 | 0.0511 |
| Triglyceride (mg/dL) | 154.6 ± 115.2 | 158.8 ± 197.5 | 0.5790 |
| LDL-C (mg/dL) | 112.4 ± 38.3 | 112.7 ± 39.7 | 0.9033 |
| HDL-C (mg/dL) | 38.5 ± 11.0 | 40.0 ± 10.9 | 0.0088 |
| Peak CK (U/L) | 143 (81-314) | 155 (90-327) | 0.0790 |
| Peak CK MB (U/L) | 13 (5-26) | 12 (3.5-25) | 0.0320 |
| Peak troponin I | 0.3 (0.1-2.1) | 0.4 (0.1-2.4) | 0.3947 |
| Admission days | 5.0 (4-8) | 5.0 (3-7) | < 0.0001 |
Abbreviations as the Table 1.
Table 5. Interventional and pharmacological therapies during hospitalization of NSTE-ACS patients.
| Registry 1 (2008-2010) | Registry 2 (2012-2015) | p value | |
| (n = 975) | (n = 1062) | ||
| Interventional therapies | |||
| Door to ECG time (min) | 13 (7-31) | 9 (5-75) | 0.4834 |
| First ECG within 10 min | 35.9% | 48.5% | < 0.0001 |
| D2B time (min) | 2534 (260-3367) | 2003 (1016-4167) | 0.0048 |
| Left main intervention | 3.8% | 5.6% | 0.0496 |
| No. of lesion treated > 2 | 12.6% | 22.2% | < 0.0001 |
| DES | 35.1% | 62.9% | < 0.0001 |
| CABG | 0.9% | 0.3% | 0.0598 |
| Pharmacological therapies | |||
| Aspirin | 89.7% | 99.3% | < 0.0001 |
| Clopidogrel | 93.3% | 99.6% | < 0.0001 |
| Dual antiplatelet therapy | 85.5% | 99.0% | < 0.0001 |
| GP 2b3a inhibitor | 9.1% | 8.5% | 0.6027 |
| Heparin | 65.5% | 85.5% | < 0.0001 |
| ACEI/ARB | 58.3% | 67.6% | < 0.0001 |
| Beta blocker | 43.3% | 64.4% | < 0.0001 |
| Statin | 48.0% | 78.8% | < 0.0001 |
| Calcium channel antagonist | 15.3% | 26.2% | < 0.0001 |
| Nitrate | 69.3% | 59.8% | < 0.0001 |
| Oral anticoagulant | 0.6% | 3.7% | < 0.0001 |
Abbreviations as the Table 2.
DISCUSSION
The major findings of this study are: (1) The care quality for ACS, including primary PCI for STEMI and pharmacological therapies for ACS, has improved in Taiwan. (2) Elderly STEMI patients had longer onset-to-door and D2B times, and were less likely to receive secondary preventive medications. (3) The onset-to-door time was longer in the patients with NSTE-ACS than in those with STEMI, and the D2B time in the patients with NSTE-ACS was long, especially in the elderly and female patients. (4) In addition, secondary preventive medications for ACS were underused except for DAPT, and ACEIs/ARBs and beta blockers were less likely to be used in the NSTE-ACS than in the STEMI patients.
PCI is the major revascularization strategy for ACS in Taiwan. In the first registry, PCI was performed in 97% of the STEMI cases and 75% of the NSTE-ACS cases.9 For STEMI, the D2B time of primary PCI was long, with a median time of 96 min in the first registry. Several strategies to shorten D2B time have been developed in Taiwan among different hospitals since 2009.11-14 The D2B time fell to 71 min in the second registry. In the United States, the median D2B time in 2010 was 64 min and 91% patients had a D2B time < 90 min in primary PCI.15 Previous studies have reported that benefits of a shorter D2B time were only observed in patients with early hospital presentation.16-18 This is probably the reason why patients with the longest onset-to-door time usually also have the longest D2B time in Taiwan. However, recent studies have shown that, at an individual patient level, a shorter D2B time was still associated with lower in-hospital and long-term mortality.19,20 In addition to D2B time, shortening the onset-to-door time is another important task for quality improvement of ACS in Taiwan. In the second registry, the onset-to-door time (172 min) of STEMI was much longer than that reported from Korea (150 min) and Japan (135 min).21,22 Our NSTE-ACS patients had an even longer onset-to-door time. This was most likely due to the higher percentage of female and diabetic patients in our NSTE-ACS group who usually had atypical presentations of ACS. Increased public awareness of ACS through educational interventions has not been proven to reduce prehospital delay effectively.23,24 Other novel strategies are needed in Taiwan to reduce the onset-to-door time for ACS patients. For NSTE-ACS, the D2B time was quite long with median times of 42.2 and 33.4 hours, respectively, in the two registries. Although D2B time for NSTE-ACS is not a performance indicator, current evidence favors an early invasive strategy for NSTE-ACS, especially for high-risk features. Early coronary angiography can identify coronary anatomy, stratify the patient’s risk and establish the indication for PCI or surgery. In the Timing of Intervention in Acute Coronary Syndromes (TIMACS) trial, an early invasive strategy (coronary angiography < 24 hours) lowered the risk of death, MI or stroke in high-risk NSTE-ACS patients compared with delayed interventions.25 In the ACUITY trial for NSTE-ACS, a delayed strategy of PCI > 24 hours was an independent predictor of 30-day and 1-year mortality.26 In the NSTE-ACS patients in our first registry, analysis showed that the high-risk patients who received PCI after 72 hours had worse clinical outcomes than those who underwent PCI within 24-72 hours.27 More aggressive treatment with a shorter D2B time is therefore necessary for NSTE-ACS in Taiwan.
Another weak point of our ACS care is the underuse of DESs, which is now a standard treatment during PCI. DESs were used in only about 40-60% in our ACS patients in the second registry. New generations of DESs have been associated with lower incidence rates of stent thrombosis and target vessel revascularization compared to bare metal stents in ACS patients.28,29 However, DESs are not completely reimbursed by the National Health Insurance in Taiwan, and the economic burden is probably the major reason for the low rate of DES use in our study. In pharmacological therapy, we found that secondary preventive medications for ACS were underused in our patients. Although there was an improvement between the two registries, ACEIs/ARBs and beta blockers were only prescribed in about 70% of the STEMI patients and 60% of the NSTE-ACS patients in the second registry. The prescription rates of these drugs in Asian-American acute MI patients have been reported to be higher than 90%.30 In Taiwan, the clinical benefits of secondary preventive medications after MI have been demonstrated in clinical studies and they are recommended in local guidelines.1,5 The prescription rate of these drugs should be increased to further improve the patients’ prognosis in Taiwan.
This study is an observational and non-randomized registry which is the major limitation. Patient entry into the registry may not have been strictly monitored as those in randomized trials. Selection bias of the included patients may also have influenced the study results. However, registry studies are typically more generalizable to real-world practice and may truly reflect the current conditions of ACS treatment in Taiwan. Our data clearly indicated the treatment gap between real-world practice and guideline recommendations. Novel strategies are necessary in Taiwan to further improve the care quality of ACS. Another limitation is that we did not know the reasons for a prehospital delay and underutilization of secondary preventive medications in the current study. The treatment side effects of ACEIs/ARBs and beta blockers, such as hypotension, bradycardia and renal dysfunction are the major concerns for Asian patients.31,32 Potential associations could be generated from an observational study, however the true causality needs further studies.
CONCLUSIONS
In conclusion, the two nationwide ACS registries from 2008 to 2015 in Taiwan showed that the ACS care quality improved significantly. The registry results also revealed some weak points that need to be improved for ACS care in Taiwan.
Acknowledgments
We would like to express our gratitude and appreciation to the physicians participating in the registry.
Principal investigators (by alphabetical order): Chien-Cheng Chen, Show Chwan Memorial Hospital; Zhih-Cherng Chen, Chi-Mei Hospital; Shu-Meng Cheng, Tri-Service General Hospital; Ching-Chang Fang, Tainan Municipal Hospital; Chih-Neng Hsu, National Taiwan University Hospital, Yun-Lin Branch; Kwan-Lih Hsu, E-Da Hospital; Eng-Thiam Ong, Cathay General Hospital; Chun-Ming Shih, Taipei Medical University Hospital; Ji-Hung Wang, Hualien Tzu Chi General Hospital; Chiung-Jen Wu, Kaohsiung Chang Gung Memorial Hospital; Wei-Hsian Yin, Cheng-Hsin General Hospital.
SOURCES OF FUNDING
This study was supported by the Taiwan Society of Cardiology and sponsored by Sanofi Taiwan Co. Ltd.
DISCLOSURES
None.
REFERENCES
- 1.Lee CH, Cheng CL, Yang YH, et al. Trends in the incidence and management of acute myocardial infarction from 1999 to 2008: get with the guidelines performance measures in Taiwan. J Am Heart Assoc. 2014;3:e001066. doi: 10.1161/JAHA.114.001066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yin WH, Lu TH, Chen KC, et al. The temporal trends of incidence, treatment, and in-hospital mortality of acute myocardial infarction over 15 years in a Taiwanese population. Int J Cardiol. 2016;209:103–113. doi: 10.1016/j.ijcard.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 3.O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139–e228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 5.Li YH, Yeh HI, Tsai CT, et al. 2012 guidelines of the Taiwan Society of Cardiology for the management of ST-segment elevation myocardial infarction. Acta Cardiol Sin. 2012;28:63–89. doi: 10.6515/ACS.202007_36(4).20200619A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Himmelstein DU, Woolhandler S. The current and projected taxpayer shares of US health costs. Am J Public Health. 2016;106:449–452. doi: 10.2105/AJPH.2015.302997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen CS, Liu TC, Chiu WT, Lin HC. Impact of hospital and physician characteristics on medical expenditures for acute myocardial infarction hospitalization. Int J Cardiol. 2007;121:127–129. doi: 10.1016/j.ijcard.2006.08.058. [DOI] [PubMed] [Google Scholar]
- 8.Kauf TL, Velazquez EJ, Crosslin DR, et al. The cost of acute myocardial infarction in the new millennium: evidence from a multinational registry. Am Heart J. 2006;151:206–212. doi: 10.1016/j.ahj.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 9.Shyu KG, Wu CJ, Mar GY, et al. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome – observations from the Taiwan ACS Full Spectrum Registry. Acta Cardiol Sin. 2011;27:135–144. [Google Scholar]
- 10.Chu CY, Lin TH, Lai WT. The management and prognostic factors of acute coronary syndrome: evidence from the Taiwan Acute Coronary Syndrome Full Spectrum Registry. Acta Cardiol Sin. 2017;33:329–338. doi: 10.6515/ACS20161205A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuo FY, Huang WC, Chiou KR, et al. The effect of failure mode and effect analysis on reducing percutaneous coronary intervention hospital door-to-balloon time and mortality in ST segment elevation myocardial infarction. BMJ Qual Saf. 2013;22:626–638. doi: 10.1136/bmjqs-2012-001288. [DOI] [PubMed] [Google Scholar]
- 12.Wang YC, Lo PH, Chang SS, et al. Reduced door-to-balloon times in acute ST-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. Int J Clin Pract. 2012;66:69–76. doi: 10.1111/j.1742-1241.2011.02775.x. [DOI] [PubMed] [Google Scholar]
- 13.Chen KC, Yen DH, Chen CD, et al. Effect of emergency department in-hospital tele-electrocardiographic triage and interventional cardiologist activation of the infarct team on door-to-balloon times in ST-segment-elevation acute myocardial infarction. Am J Cardiol. 2011;107:1430–1435. doi: 10.1016/j.amjcard.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Pan MW, Chen SY, Chen CC, et al. Implementation of multiple strategies for improved door-to-balloon time in patients with ST-segment elevation myocardial infarction. Heart Vessels. 2014;29:142–148. doi: 10.1007/s00380-013-0336-z. [DOI] [PubMed] [Google Scholar]
- 15.Krumholz HM, Herrin J, Miller LE, et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124:1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menees DS, Peterson ED, Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 17.Brodie BR, Gersh BJ, Stuckey T, et al. When is door-to-balloon time critical? Analysis from the HORIZONS-AMI (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction) and CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications) trials. J Am Coll Cardiol. 2010;56:407–413. doi: 10.1016/j.jacc.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 18.Shiomi H, Nakagawa Y, Morimoto T, et al. CREDO-Kyoto AMI investigators. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;344:e3257. doi: 10.1136/bmj.e3257. [DOI] [PubMed] [Google Scholar]
- 19.Nallamothu BK, Normand SL, Wang Y, et al. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385:1114–1122. doi: 10.1016/S0140-6736(14)61932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bucholz EM, Butala NM, Normand SL, et al. Association of guideline-based admission treatments and life expectancy after myocardial infarction in elderly medicare beneficiaries. J Am Coll Cardiol. 2016;67:2378–2391. doi: 10.1016/j.jacc.2016.03.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakamura M, Yamagishi M, Ueno T, et al. Current treatment of ST elevation acute myocardial infarction in Japan: door-to-balloon time and total ischemic time from the J-AMI registry. Cardiovasc Interv Ther. 2013;28:30–36. doi: 10.1007/s12928-012-0128-x. [DOI] [PubMed] [Google Scholar]
- 22.Park YH, Kang GH, Song BG, et al. Factors related to prehospital time delay in acute ST-segment elevation myocardial infarction. J Korean Med Sci. 2012;27:864–869. doi: 10.3346/jkms.2012.27.8.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dracup K, McKinley S, Riegel B, et al. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circ Cardiovasc Qual Outcomes. 2009;2:524–532. doi: 10.1161/CIRCOUTCOMES.109.852608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 25.Mehta SR, Granger CB, Boden WE, et al. TIMACS Investigators. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med. 2009;360:2165–2175. doi: 10.1056/NEJMoa0807986. [DOI] [PubMed] [Google Scholar]
- 26.Sorajja P, Gersh BJ, Cox DA, et al. Impact of delay to angioplasty in patients with acute coronary syndromes undergoing invasive management: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) trial. J Am Coll Cardiol. 2010;55:1416–1424. doi: 10.1016/j.jacc.2009.11.063. [DOI] [PubMed] [Google Scholar]
- 27.Wei CC, Shyu KG, Cheng JJ, et al. The relation between the timing of percutaneous coronary intervention and outcomes in patients with acute coronary syndrome with routine invasive strategy - Data from Taiwan Acute Coronary Syndrome Full Spectrum Data Registry. Acta Cardiol Sin. 2016;32:39–48. doi: 10.6515/ACS20150722A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palmerini T, Biondi-Zoccai G, Della Riva D, et al. Clinical outcomes with drug-eluting and bare-metal stents in patients with ST-segment elevation myocardial infarction: evidence from a comprehensive network meta-analysis. J Am Coll Cardiol. 2013;62:496–504. doi: 10.1016/j.jacc.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 29.Sabaté M, Räber L, Heg D, et al. Comparison of newer-generation drug-eluting with bare-metal stents in patients with acute ST-segment elevation myocardial infarction: a pooled analysis of the EXAMINATION (clinical Evaluation of the Xience-V stent in Acute Myocardial INfArcTION) and COMFORTABLE-AMI (Comparison of Biolimus Eluted from an Erodible Stent Coating with Bare Metal Stents in Acute ST-Elevation Myocardial Infarction) trials. JACC Cardiovasc Interv. 2014;7:55–63. doi: 10.1016/j.jcin.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 30.Qian F, Ling FS, Deedwania P, et al. Get With The Guidelines Steering Committee and Investigators. Care and outcomes of Asian-American acute myocardial infarction patients: findings from the American Heart Association Get With The Guidelines-Coronary Artery Disease program. Circ Cardiovasc Qual Outcomes. 2012;5:126–133. doi: 10.1161/CIRCOUTCOMES.111.961987. [DOI] [PubMed] [Google Scholar]
- 31.Lee JH, Yang DH, Park HS, et al. Korea Acute Myocardial Infarction Registry Investigators. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010;159:1012–1019. doi: 10.1016/j.ahj.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 32.Lee PT, Chao TH, Huang YL, et al. Analysis of the clinical characteristics, management, and causes of death in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention from 2005 to 2014. Int Heart J. 2016;57:541–546. doi: 10.1536/ihj.15-454. [DOI] [PubMed] [Google Scholar]