Bicuspid aortic valve (BiAV) has been considered a relative contraindication for transcatheter aortic valve replacement (TAVR) because the calcific raphe increases the risk of malapposition, paravalvular leak, annular rupture, and asymmetric expansion of the transcatheter heart valve. Asymmetric expansion can be a mechanism for premature valve degeneration due to severe distortion of the valve leaflets (1–3), and may even be related to lower early survival in patients with BiAV post-TAVR (2). We recently developed the technique of bioprosthetic or native aortic scallop intentional laceration to prevent iatrogenic coronary artery obstruction (BASILICA) during TAVR (4), in which transcatheter electrosurgery splits leaflets that may otherwise occlude the coronary ostia during TAVR. Here, we describe an application of the same technique to avert complications of TAVR for BiAV.
In April 2018, we evaluated a 52-year-old woman for worsening dyspnea and severe aortic insufficiency due to a BiAV. Multidetector computed tomography (MDCT) revealed Sievers type-1 bicuspid morphology (fusion of left and right coronary cusps), annular area of 500 mm2, long aortic leaflets (fused leaflet length 15 mm, left coronary height 12 mm) with short distance of the virtual valve to coronary artery (2.8 mm) (Figure 1A). Our strategy for TAVR in noncalcific aortic insufficiency is to oversize the annulus (29-mm SAPIEN3 [Edwards Lifesciences, Irvine, California] in this anatomy). Given the proposed strategy and the MDCT findings, the heart team was concerned about coronary obstruction. The multidisciplinary heart team determined the patient was at excessive risk for surgical aortic valve replacement secondary to severe comorbidity (STS 4.0% with severe chronic obstructive pulmonary disease). The heart team, however, was also concerned that the bicuspid valve morphology risked noncircular expansion of the transcatheter heart valve, as well as paravalvular leak and left coronary artery obstruction after TAVR. Therefore, the patient was offered bicuspid scallop intentional laceration to induce circularization of the annulus (Bicuspid Scallop Intentional Laceration to Induce Circularization of the Aortic Implant [BI-SILICA])-facilitated TAVR, an alternative application of BASILICA (4).
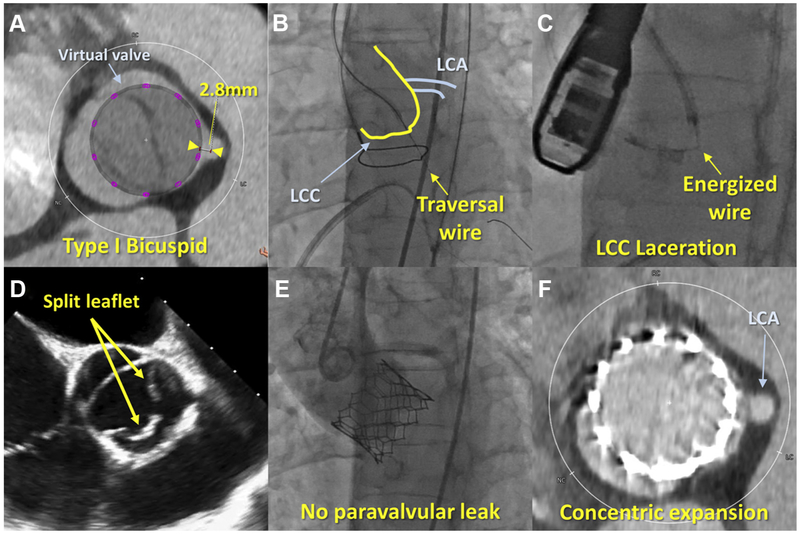
FIGURE 1. BI-SILICA During TAVR for BiAV.
(A) Sievers type-1 bicuspid morphology (fusion of left and right coronary cusps), with short distance of the virtual valve to coronary artery (2.8 mm). (B) An energized Astato XS20 guidewire traversed the left coronary cusp (LCC). (C) The energized guidewire lacerated the LCC. (D) Split leaflet after BI-SILCA was confirmed by transesophageal echocardiography. (E) Final aortography showed no paravalvular leak. (F) Post-procedural computer tomography revealed circular expansion of the balloon-expandable transcatheter heart valve and patent LCA. BiAV = bicuspid aortic valve; BI-SILICA = bicuspid scallop intentional laceration to induce circularization of the annulus; LCA = left coronary artery.
After appropriate informed consent, the procedure was performed in the catheterization laboratory under general anesthesia. An AL-3 Launcher guiding catheter (Medtronic, Minneapolis, Minnesota) was positioned against the nadir of the largest (left) coronary cusp, adjacent to the raphe. The electro-surgical system (coaxial Astato XS20 guidewire [Asahi Intecc, Tustin, California] inside an insulating PiggyBack wire converter [Teleflex, Morrisville, North Carolina]) (Figure 1B) was advanced inside the AL-3 catheter, energized at 50 W to traverse the leaflet, and directed into a loop snare pre-positioned in the left ventricular outflow tract. The central portion of the guidewire was kinked and denuded in a “flying V” configuration (Figure 1C) to lacerate the left coronary cusp during monopolar “cutting” electrification at 50 W and infusion of nonconductive 5% dextrose to displace blood. Laceration of the LCC was confirmed by echo (Figure 1D) and exacerbated aortic insufficiency without acute hemodynamic deterioration. A 29-mm Sapien-3 valve was implanted at the annulus and then uniformly and completely expanded during rapid pacing. The final angiogram showed neither aortic insufficiency (Figure 1E) nor obstruction of the left coronary artery. Post-procedural MDCT showed concentric (eccentricity = 1.02) and complete expansion (outer diameter 29 mm/area 660 mm2) of the Sapien-3 valve (Figure 1F); the stent frame was < 2.5 mm from the left coronary ostium. The patient required a permanent pacemaker for complete heart block and was asymptomatic upon discharge on postprocedure day 3.
In this initial clinical experience, BI-SILICA achieved complete and concentric expansion of a large (29-mm) Sapien-3 valve implanted into a Sievers type-1 BiAV. Compared with supra-annular implantation strategies (5), adjunctive leaflet laceration with BI-SILICA may allow a larger implant because resistance from the fused leaflets against the transcatheter valve is mitigated. More systematic evaluation is warranted to determine the value of BI-SILICA in different BiAV morphologies (e.g., BiAV type, differing amounts and distribution of calcification, stenosis, and regurgitation) to prevent short-term complications and optimize long-term outcomes as well as the influence of the aggressive oversizing strategy on the conduction disturbance during TAVR for aortic insufficiency.
Acknowledgments
Please note: This work was supported using intramural funds, Emory Structural Heart and Valve Center, and by National Institutes of Health grant Z01-HL006040-7. Dr. Lerakis has been a consultant for Edwards Lifesciences and Abbott Vascular. Dr. Grubb has been a speaker, proctor, and advisory board member for Medtronic and Boston Scientific. Dr. Guyton has served as the national principal investigator on the Edwards Lifesciences TMVR early feasibility trial. Dr. Leshnower has served on the speakers bureau for Medtronic. Dr. Greenbaum has been a proctor for Edwards Lifesciences and Abbott Vascular. Dr. Babaliaros has been a consultant for and received research grant support from Abbott Vascular and Edwards Lifesciences. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
REFERENCES
- 1.Zegdi R, Ciobotaru V, Noghin M, et al. Is it reasonable to treat all calcified stenotic aortic valves with a valved stent? Results from a human anatomic study in adults. J Am Coll Cardiol 2008;51:579–84. [DOI] [PubMed] [Google Scholar]
- 2.Costopoulos C, Latib A, Maisano F, et al. Comparison of results of transcatheter aortic valve implantation in patients with severely stenotic bicuspid versus tricuspid or nonbicuspid valves. Am J Cardiol 2014;113: 1390–3. [DOI] [PubMed] [Google Scholar]
- 3.Jilaihawi H, Chen M, Webb J, et al. A bicuspid aortic valve imaging classification for the TAVR Era. J Am Coll Cardiol Img 2016;9: 1145–58. [DOI] [PubMed] [Google Scholar]
- 4.Khan JM, Dvir D, Greenbaum AB, et al. Transcatheter Laceration of aortic Leaflets to prevent coronary obstruction during transcatheter aortic valve replacement: concept to first-in-human. J Am Coll Cardiol Intv 2018;11: 677–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu X, He Y, Zhu Q, et al. Supra-annular structure assessment for selfexpanding transcatheter heart valve size selection in patients with bicuspid aortic valve. Catheter Cardiovasc Interv 2018;91:986–94. [DOI] [PMC free article] [PubMed] [Google Scholar]