Abstract
Background:
The US Preventive Services Task Force recommends biennial screening mammography for average-risk women aged 50 to 74 years. County-level information on population measures of mammography use can inform targeted intervention to reduce geographic disparities in mammography use. County-level estimates for mammography use nationwide are rarely presented.
Methods:
We used data from the 2014 Behavioral Risk Factor Surveillance System (BRFSS) (n=130,289 women), linked it to the American Community Survey poverty data, and fitted multilevel logistic regression models with two outcomes: mammography within the past 2 years (up-to-date); and most recent mammography 5 or more years ago or never (rarely/never). We post-stratified the data with US Census population counts to run Monte Carlo simulations. We generated county-level estimates nationally and by urban-rural county classifications. County-level prevalence estimates were aggregated into state and national estimates. We validated internal consistency between our model-based state-specific estimates and urban-rural estimates with BRFSS direct estimates using Spearman correlation coefficients and mean absolute differences.
Results:
Correlation coefficients were 0.94 or larger. Mean absolute differences for the 2 outcomes ranged from 0.79 to 1.03. Although 78.45% (95% CI: 77.95%—78.92%) of women nationally were up-to-date with mammography, more than half of the states had counties with >15% of women rarely/never using a mammogram, many in rural areas.
Conclusions:
We provided estimates for all U.S. counties and identified marked variations in mammography use. Many states and counties were far from the 2020 target (81.1%).
Impact:
Our results suggest a need for planning and resource allocation on a local level to increase mammography uptake.
Keywords: multilevel small area estimation, county-level estimates, mammography, internal consistency, rural populations
Introduction
In 2016, the U.S. Preventive Services Task Force (USPSTF) updated its recommendations on breast cancer screening after concluding that a net benefit to screening exists. The USPSTF recommended screening every 2 years for average-risk women aged 50 to 74 years (1).
One of the Department of Health and Human Services’ Healthy People objectives was to increase the prevalence of breast cancer screening as recommended to 81.1% by 2020 (2). Analysis of data from the National Health Interview Survey in 2015 showed that 71.5% of women aged 50–74 years reported having had a mammogram in the past two years—nearly 10% below the Healthy People 2020 target—and this proportion has been stable for 15 years (3). Underlying this national estimate is considerable variability in screening prevalence by race/ethnicity, income, education, and insurance status (3). Furthermore, variability in these characteristics occurs at finer geographic scales such as the state or county levels.
State-level cancer screening use is often estimated using data from the Behavioral Risk Factor Surveillance System (BRFSS) (4). However, differences in mammography screening estimates among states do not provide information about the variations within individual states. Local communities may also have substantial variations in mammography use due to diversity in social and economic status, healthcare and cultural characteristics, which can be masked by state-level analysis.
Recent estimates of mammography prevalence for US counties have utilized BRFSS data from 2012 or earlier. These estimates focused only on the distribution of women with recent mammography and have compared prevalence estimates with older USPSTF recommendations that have since been revised (5–7). A publication of state and county-level mammography prevalence within 2 years among women aged 40 or older by the National Cancer Institute found that between 2008 and 2010, there were large geographical variations among states (57.5%−81.9%) and counties (30.69%−94.66%) (8).
Data from small area analysis, such as county-level analysis, can be useful for describing local variations of mammography use and highlight disparity among counties. County-level mammography screening data could inform state and local public health decision makers about public health resource allocation in counties with low mammography uptake by utilizing state programs funding, such as the CDC National Breast and Cervical Cancer Early Detection Programs (NBCCEDP). Because some survey samples are insufficiently large to yield stable estimates for some areas, small area estimates can be generated using models that combine county-level data from different sources, such as the U.S. Census. Using census population data for post-stratification allows states to generate estimates for all counties including counties for which no direct estimates are available from BRFSS.
The goal of our study is to apply multilevel small area estimation (SAE) to obtain county-level prevalence estimates of 1) women who had a mammogram within 2 years (defined as up-to-date) according to the USPSTF recommendations; and 2) women who had their most recent mammogram 5 or more years before the survey interview or never had one (defined as rarely or never).
Examining small-area differences in mammography use among the group of women who rarely or never had a mammogram is of utmost importance because women who are not screened are more likely to have more advanced disease. In a recent systematic review and meta-analysis, the authors concluded that advanced cancer is reduced with screening for women aged 50 years or older (9). A different systematic review and meta-analysis comparing mammographic screening attendance between immigrant and minority women to that of other women indicated a lower attendance among immigrants and minorities, who are more often diagnosed with advance breast cancer (10). Our estimates of proportions of women up-to-date with mammography or those who never had a mammogram can potentially reduce geographic disparities in mammography use and reduce late-stage diagnosis.
Material and Methods
We used data from the 2014 BRFSS, a state-based, cross-sectional, random-digit-dial phone survey administered annually by CDC in collaboration with state health departments and the District of Columbia to non-institutionalized adults aged 18 years or older. In 2014, the survey’s combined landline and cell phone response rates ranged from 60.1% in South Dakota to 25.1% in California, with a median rate of 47%. Further information about the survey can be found on the BRFSS website (4).
Women aged 40 years and older were asked “Have you ever had a mammogram?” and those who answered “No” were assigned as never having had a mammogram. Women who answered “Yes” were asked “How long it has been since you had your last mammogram?” We examined 2 outcomes based on responses to a question about time since their last mammogram: being up-to-date with mammography (most recent mammogram <2 years ago); and rarely or never having had a mammogram (most recent mammogram 5 or more years ago, or never). Our analysis included women aged 50–74 years who answered these questions, consistent with the current USPSTF recommendation for breast cancer screening. For women aged 40 to 49 years, the USPSTF stated the decision to start screening was a personal one, and for those aged 75 years or older, no recommendation was issued (1). Women who did not know, were not sure, or refused to answer, were excluded.
Because the BRFSS questions did not include details on whether the mammogram was for screening or diagnosis, we consider these questions a general measure of mammography use for all purposes.
Statistical analysis
We linked BRFSS individual-level data with county-of-residence from the 2014 BRFSS restricted data set by adding the state and county information to each record of the BRFSS data (n=130,289 women age 50–74 years, representing 44.1 million women) after excluding missing mammography information (n=8,442). We then linked the combined data to the 5-year (2010–2014) county-level poverty estimates from the American Community Survey (11). Using these data, we fitted multilevel logistic regression models (12) with fixed effects including age group (50–54, 55–59, 60–64, 65–69, 70–74), race/ethnicity (non-Hispanic (NH) white, NH black, NH American Indian/Alaska Native (AIAN), NH Asian, NH other (Pacific Islander, other one race, and 2 or more races), and Hispanic), county-level poverty (≤150% of the federal poverty rate), and state- and county-level random effects. The results from each model included parameters for each fixed and random effects. Because estimates of random effects were not available for some counties which did not have BRFSS samples for analysis, we used a local spatial smoothing algorithm, namely a smoothed average of the adjacent counties random effects, to approximate the county random effect of each county without BRFSS respondents (12). We then linked the newly created random effects with the county random effects list. We chose to use a flexible spatial smoothing method to avoid over-smoothing health behavior outcome variations in adjacent counties and by BRFSS data, where direct calculations for some counties were limited (13, 14). Also, a county random effect specifies the local contextual influence on health outcomes and likely would be more similar to its adjacent counties. We post-stratified the BRFSS data with US census county population counts (15) and used them with the updated random effects list in newly developed Monte Carlo simulation models. Our models predicted the individual-level expected probability of being up-to-date with mammography use, or rarely or never having had a mammogram, and generated their county-level prevalence estimates and their standard errors.
Our regression models followed the generalized linear mixed models general formula (12,16):
yijcs is the self-reported mammography use by an individual in age group i, i=1 to 5, and race/ethnicity group j, j=1 to 6, from county c in state s, and their respective regression coefficients. xc is a vector of county-level poverty status covariates and η is a vector of their respective regression coefficients. The prediction model included their product x’cη. μc and ѵs are the county- and state-level random effects, which were assumed to be independent and normally distributed.
Each simulation included 1,000 randomly drawn samples for each of the parameters and their standard errors. We used the respective simulation results to summarize the estimated proportions for each outcome by county, state, and the entire United States, and generated predicted mean values, their standard errors, and 95% confidence intervals. The prevalence calculations used the county population counts from the Census as weights.
In an additional analysis, we linked our post-stratified data (with 2142 counties) with the 2013 National Center for Health Statistics (NCHS) urban-rural area classification scheme for counties (here after urban-rural area) (17) after excluding 5 counties that were not on the list of the 2014 BRFSS counties. The NCHS urban-rural areas file included 4 metropolitan area categories: area 1 - counties of Metropolitan Statistical Areas (MSAs) of ≥1 million (large central metro); area 2 - counties with population ≥1 million (large fringe metro); area 3 - counties within MSAs of 250,000–999,999 population (medium metro); area 4 - counties within MSAs of 50,000–249,999 population (small metro), and 2 nonmetropolitan areas: area 5 - counties in micropolitan statistical areas with a city of 10,000 or more population; area 6 – noncore counties not within micropolitan statistical areas (without a city of 10,000 or more population). Linking the urban-rural area classification scheme to the post-stratified BRFSS data enabled us to point out the difference in mammography screening uptake among the 6 area classifications.
We repeated the simulation process described above for the counties in each urban-rural area to generate overall and county-level estimates. We also linked the BRFSS county-level data with the above urban-rural areas by state and county codes and presented the overall direct estimates of our BRFSS outcomes for each urban-rural area by demographic characteristics in the supplemental data section. For this analysis, we collapsed the metropolitan areas to 2 areas based on population size: 1) areas 1 (large central metro) and area 2 (large fringe metro); and 2) areas 3 (medium metro) and area 4 (small metro). Areas 5 and 6 remained the same.
Because the BRFSS is a state-based survey, we evaluated the internal consistency of our model-based state-specific estimates with BRFSS direct state estimates and the 6 model-based urban-rural area estimates with the corresponding BRFSS direct urban-rural area estimates, using both Spearman correlation coefficients and the mean absolute differences between the model-based and BRFSS estimates. Further details about our methodology are presented by Berkowitz et al (16).
We fitted the BRFSS multilevel logistic regression models with unweighted data using the SAS GLIMMIX procedure, SAS Version 9.3 (SAS Institute, Inc., Cary, NC). The exclusion of weights was based on 2 validation studies showing that an unweighted model generated more accurate small area estimates (18, 19). Post-stratification is a weighting process in our modeling approach for small area estimation. We used ArcGIS (Esri, Redlands, CA) to separately map the model-based county estimates and their standard errors by deciles. We calculated direct BRFSS estimates with SAS-callable SUDAAN (Research Triangle Institute, Research Triangle Park, NC).
Results
Our BRFSS data analysis found 93 counties for which random effects were not available. Over 70% of these counties were in the non-core area classification and their mean and median poverty rates among women aged 50–74 were estimated by the American Community Survey at 30%.
Our post stratification file included data from all 3,142 counties. The national 2014 model-based SAE prevalence estimate for up-to-date with mammography was 78.45%, (95% confidence interval (CI), 77.95%―78.92%), the same as the direct 2014 BRFSS estimate: 78.45%, (95% CI, 78.00%―78.90%). The model-based prevalence estimate for rarely or never had a mammogram was 11.19%, (95% CI, 10.91%―11.45%) while the direct 2014 BRFSS estimate was 11.02%, (95% CI. 10.70%―11.36%).
Spearman correlation coefficients between our state-level model-based SAE estimates and the BRFSS direct state estimates were 0.98 for up-to-date with mammography and 0.95 for rarely or never had a mammogram, indicating high state-level internal consistency (Table 1). Spearman correlation coefficients for both outcomes for the urban-rural area analysis were 0.94. The means of the absolute differences between both the model-based state-estimates and the NCHS rural-urban area estimates and the respective BRFSS direct estimates for the 2 outcomes ranged from 0.79 to 1.03. The differences between the model-based mean and median estimates and the BRFSS direct estimates were <0.5% (Table 1).
Table 1.
Correlation coefficients and mean absolute differences between model-based state estimates and NCHS urban-rural area estimates, and BRFSS direct state estimates, by test type.
| Up-to-date with mammographya | Rarely or never had a mammogramb | |||||
|---|---|---|---|---|---|---|
| Test | Test estimate | Mean (%) | Median (%) | Test estimate | Mean (%) | Median (%) |
| Spearman correlation coefficient | State estimates (n=51) | |||||
| Model-Based | 0.98 | 77.66 | 78.44 | 0.95 | 11.56 | 11.27 |
| BRFSS | 77.58 | 78.10 | 11.60 | 11.17 | ||
| Mean absolute differences | 0.79 | 0.95 | ||||
| Spearman correlation coefficient | NCHS urban-rural stimatesc (n=6) | |||||
| Model-Based | 0.94 | 77.72 | 77.72 | 0.94 | 11.68 | 11.73 |
| BRFSS | 77.43 | 78.09 | 11.91 | 11.70 | ||
| Mean absolute differences | 1.03 | 0.92 | ||||
Notes: NCHS=National Center for Health Statistics
Up-to-date = having had the most recent mammogram within 2 years;
Rarely or never = having had the most recent mammogram ≥5 years before the survey interview or never.
Metropolitan and nonmetropolitan areas were based on the 2013 6 categories of NCHS urban-rural classification Scheme for counties.
BRFSS percentages are weighted to the study population
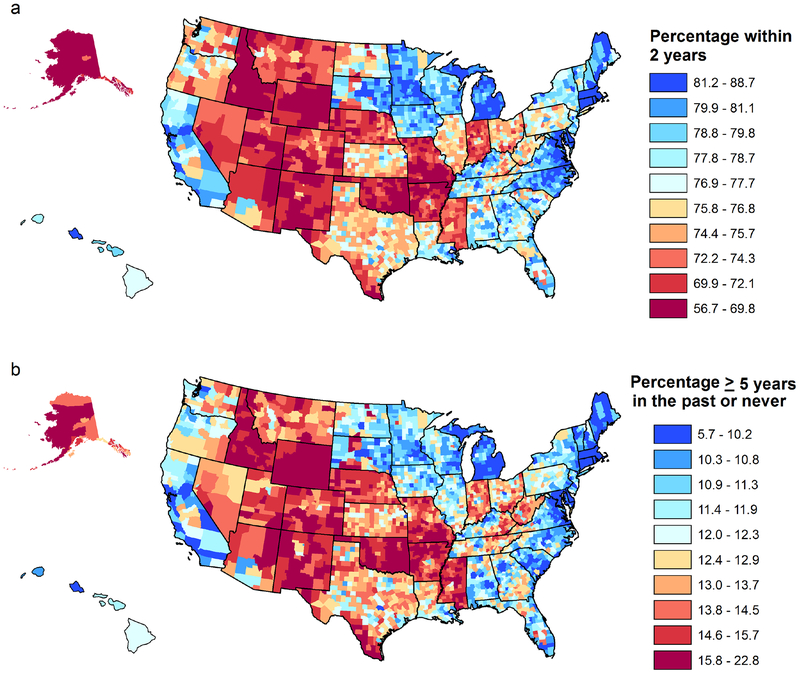
Although the majority of women were up-to-date with mammography in 2014, our findings showed large variations in mammography use among states and counties (Table 2, Figure 1a). The mean estimate for being up-to-date with mammography use by state ranged from 68.72% in Idaho to 87.17% in Massachusetts. States with the highest proportions of up-to-date mammography (>80%) were mostly in New England, and the northern, eastern, and western U.S. The 7 states with the highest estimates of being up-to-date with mammography, along with New Hampshire, and DC, had the lowest proportion of women (<10%) who rarely or never had a mammogram. The largest differences (ranges) in estimates for being up-to-date with mammography use across counties within a state ranged from a low of 1.42% in Delaware to a high of 17.19% in Alaska. Alaska also had the lowest up-to-date county estimate (56.67%). Large differences in county estimates (>13.5%) were also observed in Nebraska, Missouri, Idaho, and Arkansas (Figure 1a).
Table 2.
Model-based SAE state mean estimate (%) and county statistics summarized by state for up-to-date with mammography and rarely or never had a mammograma
| Up-to-date with mammographyb | Rarely or never had a mammogramc | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| State | State Mean | County summary statistic | State Mean | County summary statistic | ||||||||||||
| Min | Q1 | Mean | Median | Q3 | Max | Ranged | Min | Q1 | Mean | Median | Q3 | Max | Ranged | |||
| Massachusetts | 87.17 | 85.03 | 86.16 | 86.73 | 86.80 | 87.22 | 88.75 | 3.72 | 6.50 | 5.67 | 6.41 | 6.82 | 6.74 | 7.31 | 8.00 | 2.32 |
| Rhode Island | 84.65 | 83.51 | 84.03 | 84.44 | 84.63 | 84.69 | 85.32 | 1.81 | 6.92 | 6.70 | 6.73 | 6.94 | 6.89 | 7.13 | 7.25 | 0.55 |
| Delaware | 84.20 | 83.71 | 83.71 | 84.37 | 84.27 | 85.13 | 85.13 | 1.42 | 8.05 | 7.98 | 7.98 | 8.04 | 8.06 | 8.07 | 8.07 | 0.09 |
| Maryland | 83.41 | 75.69 | 80.88 | 82.26 | 82.58 | 84.05 | 85.71 | 10.02 | 8.57 | 7.54 | 8.35 | 9.15 | 8.84 | 9.90 | 11.76 | 4.23 |
| Connecticut | 83.04 | 81.50 | 82.96 | 83.50 | 83.39 | 84.44 | 84.94 | 3.45 | 8.23 | 7.69 | 7.84 | 8.12 | 7.92 | 8.43 | 8.94 | 1.25 |
| Michigan | 82.17 | 78.64 | 80.56 | 81.62 | 81.78 | 82.48 | 84.90 | 6.26 | 9.19 | 8.02 | 9.47 | 9.91 | 9.82 | 10.50 | 11.93 | 3.91 |
| Maine | 81.97 | 76.89 | 79.13 | 80.74 | 80.95 | 82.39 | 83.91 | 7.02 | 8.74 | 7.76 | 8.62 | 9.33 | 9.05 | 10.14 | 11.17 | 3.41 |
| Minnesota | 81.43 | 75.75 | 79.93 | 80.62 | 80.67 | 81.39 | 83.90 | 8.15 | 10.46 | 9.14 | 10.44 | 10.90 | 10.89 | 11.28 | 14.77 | 5.63 |
| Virginia | 81.11 | 73.32 | 78.49 | 79.96 | 80.11 | 81.46 | 83.32 | 10.11 | 10.16 | 8.79 | 9.96 | 11.01 | 10.86 | 11.85 | 15.92 | 7.13 |
| DC | 80.91 | 7.80 | ||||||||||||||
| North Carolina | 80.87 | 77.48 | 79.49 | 80.53 | 80.68 | 81.45 | 84.02 | 6.55 | 10.77 | 9.15 | 10.44 | 11.12 | 10.92 | 11.92 | 13.66 | 4.52 |
| New Hampshire | 80.75 | 78.54 | 78.74 | 79.81 | 79.04 | 81.24 | 82.60 | 4.05 | 9.71 | 8.90 | 9.35 | 10.35 | 10.44 | 10.94 | 12.04 | 3.13 |
| Hawaii | 80.57 | 77.39 | 77.72 | 78.85 | 78.15 | 79.19 | 81.80 | 4.40 | 10.46 | 9.93 | 10.67 | 11.21 | 11.09 | 12.09 | 12.29 | 2.37 |
| California | 80.29 | 75.21 | 78.23 | 79.49 | 79.68 | 80.84 | 82.77 | 7.56 | 10.22 | 8.79 | 9.91 | 10.85 | 10.77 | 11.85 | 13.21 | 4.43 |
| Iowa | 80.21 | 76.19 | 78.62 | 79.45 | 79.42 | 80.21 | 83.85 | 7.66 | 11.30 | 9.45 | 11.02 | 11.55 | 11.52 | 12.02 | 13.63 | 4.17 |
| Wisconsin | 80.19 | 74.75 | 78.63 | 79.49 | 79.66 | 80.39 | 83.67 | 8.91 | 10.64 | 8.92 | 10.50 | 11.05 | 11.02 | 11.50 | 14.47 | 5.56 |
| Kentucky | 71.95 | 11.46 | 8.63 | 11.93 | 13.32 | 16.30 | 7.67 | |||||||||
| 79.58 | 76.42 | 78.12 | 78.63 | 79.80 | 83.41 | 11.27 | 11.13 | 12.24 | ||||||||
| Georgia | 79.57 | 74.01 | 77.14 | 78.39 | 78.35 | 79.59 | 82.45 | 8.45 | 10.81 | 8.96 | 10.92 | 11.80 | 11.88 | 12.68 | 15.39 | 6.43 |
| South Dakota | 79.55 | 71.05 | 78.53 | 79.21 | 79.79 | 81.13 | 84.10 | 13.05 | 11.16 | 9.00 | 10.31 | 11.63 | 11.01 | 11.87 | 19.31 | 10.32 |
| Louisiana | 79.18 | 74.23 | 76.69 | 77.79 | 77.79 | 78.65 | 82.86 | 8.63 | 11.44 | 9.48 | 11.66 | 12.30 | 12.41 | 13.03 | 15.19 | 5.71 |
| Tennessee | 79.08 | 73.58 | 76.31 | 77.60 | 77.60 | 78.60 | 81.49 | 7.91 | 11.69 | 9.29 | 11.92 | 12.67 | 12.73 | 13.48 | 15.76 | 6.46 |
| Vermont | 79.01 | 75.88 | 77.36 | 78.49 | 78.57 | 78.94 | 81.81 | 5.93 | 10.31 | 9.34 | 10.11 | 10.54 | 10.27 | 11.23 | 12.05 | 2.71 |
| Florida | 78.98 | 73.09 | 76,79 | 78.03 | 78.01 | 79.46 | 82.80 | 9.71 | 10.92 | 9.56 | 10.79 | 11.63 | 11.48 | 12.22 | 14.69 | 5.13 |
| Alabama | 78.72 | 73.43 | 76.94 | 77.89 | 77.72 | 79.19 | 81.41 | 7.98 | 11.03 | 9.45 | 10.73 | 11.40 | 11.38 | 12.01 | 13.46 | 4.00 |
| New York | 78.61 | 76.02 | 77.64 | 78.47 | 78.53 | 79.07 | 81.52 | 5.50 | 10.85 | 9.57 | 10.71 | 11.17 | 11.05 | 11.67 | 12.54 | 2.97 |
| New Jersey | 78.44 | 74.86 | 77.54 | 78.41 | 78.52 | 79.41 | 81.55 | 7.00 | 11.13 | 9.81 | 10.92 | 11.24 | 11.18 | 11.64 | 12.61 | 2.80 |
| South Carolina | 77.96 | 73.21 | 76.00 | 77.44 | 77.47 | 79.05 | 81.93 | 8.72 | 10.39 | 8.12 | 10.07 | 10.69 | 10.73 | 11.27 | 12.60 | 4.48 |
| Oregon | 77.67 | 70.80 | 74.99 | 76.22 | 76.15 | 77.15 | 80.99 | 10.19 | 11.41 | 10.25 | 11.37 | 11.97 | 12.01 | 12.48 | 14.04 | 3.79 |
| Washington | 77.65 | 70.63 | 74.25 | 75.66 | 75.58 | 77.64 | 81.20 | 10.57 | 11.18 | 9.76 | 11.54 | 12.24 | 12.24 | 12.86 | 14.74 | 4.98 |
| Pennsylvania | 77.56 | 73.18 | 76.10 | 76.97 | 76.96 | 77.90 | 80.85 | 7.67 | 11.27 | 9.81 | 11.29 | 11.73 | 11.84 | 12.27 | 13.18 | 3.37 |
| Kansas | 77.48 | 72.43 | 74.91 | 75.91 | 75.88 | 77.13 | 82.54 | 10.10 | 12.62 | 10.06 | 12.61 | 13.34 | 13.39 | 14.14 | 15.82 | 5.76 |
| North Dakota | 77.26 | 67.73 | 75.61 | 76.14 | 76.55 | 77.70 | 79.72 | 12.00 | 11.58 | 10.14 | 11.15 | 12.05 | 11.75 | 12.41 | 17.84 | 7.70 |
| Illinois | 77.21 | 71.63 | 75.10 | 75.90 | 75.96 | 77.00 | 78.97 | 7.33 | 10.83 | 9.78 | 11.18 | 11.83 | 11.76 | 12.34 | 15.10 | 5.32 |
| West Virginia | 77.07 | 73.13 | 75.46 | 76.40 | 76.22 | 77.44 | 80.10 | 6.97 | 12.98 | 11.05 | 12.89 | 13.49 | 13.50 | 14.05 | 16.37 | 5.32 |
| Texas | 77.03 | 67.75 | 74.53 | 75.43 | 75.57 | 76.70 | 80.64 | 12.89 | 12.44 | 10.05 | 12.35 | 13.25 | 13.17 | 13.95 | 18.98 | 8.93 |
| Arizona | 76.68 | 66.2 | 70.04 | 72.02 | 71.36 | 75.05 | 79.04 | 12.62 | 11.60 | 10.23 | 12.95 | 14.33 | 14.08 | 15.73 | 18.17 | 7.95 |
| Ohio | 69.82 | 9.59 | 10.04 | 12.94 | 15.90 | 5.86 | ||||||||||
| 76.15 | 74.58 | 75.29 | 75.28 | 76.60 | 79.41 | 12.31 | 12.12 | 12.95 | 13.64 | |||||||
| Nebraska | 74.36 | 61.67 | 70.08 | 71.54 | 71.54 | 72.94 | 77.59 | 15.92 | 13.09 | 10.66 | 14.13 | 14.77 | 14.62 | 15.40 | 21.40 | 10.74 |
| Colorado | 73.92 | 64.49 | 69.08 | 71.29 | 71.51 | 73.18 | 76.38 | 11.89 | 13.92 | 12.14 | 14.14 | 15.36 | 15.16 | 16.71 | 19.72 | 7.58 |
| Utah | 73.43 | 63.82 | 69.57 | 71.21 | 71.25 | 73.16 | 75.35 | 11.53 | 13.42 | 11.78 | 13.04 | 14.35 | 14.09 | 15.19 | 19.21 | 7.43 |
| Mississippi | 73.08 | 69.94 | 71.53 | 72.49 | 72.28 | 73.20 | 76.56 | 6.62 | 14.88 | 12.06 | 14.70 | 15.32 | 15.41 | 15.93 | 17.53 | 5.46 |
| Missouri | 73.07 | 63.71 | 68.76 | 70.17 | 70.01 | 71.58 | 78.30 | 14.59 | 13.33 | 10.70 | 14.07 | 14.92 | 15.06 | 15.93 | 18.56 | 7.87 |
| Nevada | 73.06 | 66.42 | 71.36 | 71.80 | 72.20 | 73.02 | 74.40 | 7.97 | 13.67 | 11.82 | 13.28 | 13.81 | 13.73 | 14.06 | 17.94 | 6.12 |
| Indiana | 72.74 | 68.67 | 70.60 | 72.14 | 71.91 | 73.00 | 78.04 | 9.37 | 13.24 | 10.40 | 12.95 | 13.63 | 13.73 | 14.50 | 15.55 | 5.15 |
| Montana | 72.60 | 64.03 | 71.06 | 71.84 | 72.13 | 73.31 | 76.92 | 12.89 | 13.94 | 11.86 | 13.39 | 14.26 | 13.98 | 14.71 | 18.75 | 6.88 |
| New Mexico | 72.11 | 64.99 | 68.72 | 70.21 | 70.41 | 71.31 | 76.51 | 11.52 | 14.37 | 10.76 | 14.62 | 15.41 | 15.62 | 16.26 | 17.96 | 7.20 |
| Arkansas | 71.71 | 64.19 | 68.80 | 70.17 | 70.06 | 71.57 | 77.78 | 13.59 | 14.73 | 11.30 | 14.58 | 15.43 | 15.43 | 16.39 | 18.21 | 6.91 |
| Oklahoma | 69.79 | 63.54 | 67.41 | 68.87 | 68.74 | 70.37 | 72.81 | 9.26 | 16.18 | 13.48 | 15.68 | 16.70 | 16.74 | 17.68 | 20.03 | 6.54 |
| Alaska | 69.52 | 56.67 | 65.75 | 67.32 | 67.84 | 69.08 | 73.89 | 17.19 | 14.11 | 11.76 | 13.48 | 15.09 | 14.49 | 16.27 | 21.65 | 9.89 |
| Wyoming | 69.39 | 64.41 | 65.46 | 68.33 | 68.38 | 70.72 | 73.83 | 9.42 | 17.41 | 15.06 | 16.04 | 17.55 | 17.71 | 18.38 | 21.35 | 6.28 |
| Idaho | 68.72 | 58.80 | 64.34 | 66.10 | 66.29 | 68.14 | 72.87 | 14.08 | 16.17 | 14.70 | 15.84 | 17.10 | 16.70 | 17.99 | 22.79 | 8.09 |
Notes: Q1=Lower quartile; Q3=upper quartile
Percentages are in decreasing order of state prevalence for up-to-date mammography. Percentages for rarely or never match by state.
Up-to-date = having had the most recent mammogram within 2 years;
Rarely or never = having had the most recent mammogram ≥5 years before the survey interview or never.
Ranges with percentages ≥10% are highlighted.
Figure 1.
Model-based County-level mean estimates (%) maps of 2 outcomes of mammography use: a. up-to-date (<2 years). b. rarely or never had a mammogram (most recent mammogram ≥5 years before the survey interview or never). The County percentage-ranges shown on the right of each map differ by map. Percentage-ranges for up-to-date mammography are in decreasing order. Percentage-ranges for rarely or never are in increasing order. County-level mean estimates were aggregated by deciles, and a different color was assigned in the legend to each decile.
At least 10% of women rarely or never had a mammogram in most states; Wyoming had the highest state mean estimate, 17.41% (Table 2). Counties where ≥15% of women rarely or never had a mammogram existed in more than half of the states and in 5 states this percentage exceeded 20% (Nebraska, Oklahoma, Alaska, Idaho and Wyoming, Figure 1b). Nebraska and South Dakota had the largest within-state differences in county estimates of women who rarely or never had a mammogram (10.74% and 10.32% respectively).
Of the 50 counties with the lowest mean estimates of being up-to-date with mammography, nearly half also had the highest mean estimates (>=18%) of women who rarely or never had a mammogram. These counties were in Alaska, Idaho, Montana, Wyoming, Colorado, Nebraska, Oklahoma, Arkansas, Missouri, and Utah. Although not among the above mentioned states Texas had 6 counties where 18% to 19% of women rarely or never had a mammogram.
Additional details about the predicted standard errors of county estimates for being up-to-date with mammography and for rarely or never having had a mammogram are presented in the supplementary Fig. S1a and S1b.
Findings from our model-based urban-rural analysis indicate an approximately 4% difference in the overall mean estimate of up-to-date mammography use between metropolitan areas with population ≥1 million (areas 1 and 2) and the noncore area (area 6, Table 3a). The total range in county estimates was twice as large in the noncore area as in the large central metro area (area 1). Conversely, the lowest mean estimate for rarely or never mammography use was observed in the largest metropolitan areas (areas 1 and 2) and the highest in the noncore area (Table 3b). The overall county range was also twice as large in the noncore area as in the large central metro area (area 1). BRFSS direct estimates were similar to our model-based estimates and their 95% CIs largely overlapped.
Table 3.
Model-based small area estimation summary statistics (%) and BRFSS direct estimates for up-to-date mammography use and rarely or never had a mammogram by NCHS metropolitan and nonmetropolitan county population size
| NCHS categorya | No of counties | Mean | 95% CI | Min | Lower quartile | Median | Upper quartile | Max | Inter-quartile range | Overall Range | BRFSSb | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| mean | 95% CI | |||||||||||
| Up-to-date | ||||||||||||
| 1 (overall) | 79.47 | 78.36–80.52 | 80.94 | 79.89–81.94 | ||||||||
| Counties | 68 | 79.72 | 71.69 | 78.26 | 80.20 | 81.35 | 87.23 | 3.08 | 15.54 | |||
| 2 (overall) | 79.67 | 79.00–80.33 | 78.92 | 77.98–79.82 | ||||||||
| Counties | 368 | 78.55 | 67.57 | 76.43 | 79.02 | 81.08 | 88.7 | 4.65 | 21.16 | |||
| 3 (overall) | 78.02 | 77.39–78.67 | 78.53 | 77.65–79.39 | ||||||||
| Counties | 372 | 77.32 | 61.02 | 75.59 | 77.91 | 80.09 | 87.02 | 4.50 | 26.00 | |||
| 4 (overall) | 77.41 | 76.81–78.07 | 77.65 | 76.36–78.88 | ||||||||
| Counties | 358 | 77.00 | 66.13 | 75.08 | 77.43 | 79.73 | 86.73 | 4.64 | 20.59 | |||
| 5 (overall) | 76.02 | 75.49–76.52 | 75.95 | 74.82–77.04 | ||||||||
| Counties | 641 | 75.39 | 61.36 | 72.30 | 75.86 | 78.49 | 86.53 | 6.20 | 25.17 | |||
| 6 (overall) | 75.64 | 75.14–76.11 | 72.61 | 71.34–73.83 | ||||||||
| Counties | 1335 | 74.90 | 56.60 | 71.67 | 75.68 | 78.27 | 86.77 | 6.61 | 30.17 | |||
| Rarely or never | ||||||||||||
| 1 (overall) | 10.58 | 9.99–11.18 | 8.88 | 8.20–9.62 | ||||||||
| Counties | 68 | 10.60 | 6.77 | 9.86 | 10.47 | 11.20 | 15.04 | 1.34 | 8.27 | |||
| 2 (overall) | 10.29 | 9.94–10.67 | 10.40 | 9.75–11.08 | ||||||||
| Counties | 368 | 11.03 | 5.66 | 9.98 | 10.86 | 12.13 | 17.33 | 2.15 | 11.67 | |||
| 3 (overall) | 11.50 | 11.13–11.87 | 11.13 | 10.50–11.80 | ||||||||
| Counties | 372 | 11.96 | 6.26 | 10.70 | 11.47 | 12.98 | 20.16 | 2.28 | 13.90 | |||
| 4 (overall) | 11.95 | 11.62–12.34 | 12.26 | 11.22–13.34 | ||||||||
| Counties | 358 | 12.22 | 6.41 | 10.94 | 11.97 | 13.32 | 18.38 | 2.38 | 11.96 | |||
| 5 (overall) | 12.74 | 12.44–13.04 | 13.42 | 12.57–14.33 | ||||||||
| Counties | 641 | 13.09 | 7.07 | 11.58 | 12.78 | 14.47 | 21.58 | 2.88 | 14.51 | |||
| 6 (overall) | 13.01 | 12.71–13.29 | 15.36 | 14.38–16.39 | ||||||||
| Counties | 1335 | 13.39 | 6.66 | 11.76 | 13.09 | 14.78 | 22.72 | 3.02 | 16.06 | |||
Notes:
Metropolitan and nonmetropolitan areas were based on the 2013 6 categories of NCHS urban-rural classification Scheme for counties (12).
Large central Metropolitan Statistical Areas (MSA) with population ≥1 million.
Large fringe MSA with population ≥1 million.
Medium metropolitan counties within MSAs of 250,000–999,999 population.
Small metropolitan counties within MSAs of 50,000–249,999 population (small metro).
Micropolitan counties with a city of 10,000 or more population).
Non-core (non-micropolitan) counties without a city of 10,000 or more population
Up-to-date = having had the most recent mammogram within 2 years; Rarely or never = having had the most recent mammogram ≥5 years before the survey interview or never.
The total number of counties in these areas is 3142 after deleting 5 counties to reflect the number of counties in the 2014 BRFSS survey.
BRFSS percentages are weighted to the study population
A decreasing trend was also observed in BRFSS-NCHS urban-rural linked data, where the overall estimated percentage of up-to-date mammography use was highest in the large central and fringe metro areas (79.97%) and lowest in the noncore area (72.61%, Supplemental Table S1). A similar trend was also observed across age groups in metropolitan and nonmetropolitan areas. A corresponding trend was observed for the percentage of women who rarely or never had a mammogram, with overall estimate of 9.61% in the large central and fringe metro areas and 15.36% in the noncore area (Supplemental Table S2). An increasing trend in the estimate was also observed across age groups.
Discussion
Between states and within states, our results show large variations in the estimated proportions of women up-to-date with mammography and women who rarely or never had a mammogram. Over three quarters of women were up-to-date with mammography. Fifteen states and the District of Colombia had an estimated mean of 80% or more of women who were up-to-date with mammography and 21 states were within 5% of the 2020 goal of 81.1%. However, many counties were far below 80%. Additionally, a large number of states had counties with many women who rarely or never had a mammogram. Overall, we found that 1 in 9 women (approximately 4.9 million) rarely or never had a mammogram, and in some states, this ratio was as high as 1 in 7. This proportion, when applied to the population eligible for mammography, translates into a large number of women.
The county maps’ deciles highlight the disparity among counties. Many counties with both the lowest estimated proportion up-to-date with mammography and substantial proportions of women who rarely or never had a mammogram were in rural areas. A recent CDC analysis of invasive cancer incidence and mortality over time showed that nonmetropolitan counties had persistently lower incidence rates of breast cancer and late-stage breast cancer among women. However, death rates for breast cancer were higher in nonmetropolitan rural areas than in metropolitan areas with <1 million population (20). A county-level analysis of access to screening mammography across the US from 2003 to 2009 found that more than 27% of counties had no mammography capacity—a finding that was strongly associated with low population density, low primary care physician density, and low percentage of insured residents compared with counties with one or more mammography machines (21, 22). A longitudinal assessment study of geographic disparities in mammography capacity in the south found that in 2008, Texas contributed the largest percentage of women (44%) living in poor mammography capacity areas, including many rural areas (23). Inadequate health services and low mammography capacity might have decreased the likelihood of women receiving screening mammograms and increased the likelihood of late-stage diagnoses among women with breast cancer (21, 24).
Addressing the challenges of lower mammography use in rural communities requires a multifocal approach. Adults living in rural areas are more likely to have lower educational attainment, lower income, have limited employment, and to be uninsured than those living in urban areas (25–27). In addition, many people in rural areas may have cultural and language challenges which can contribute to low screening uptake (28). To reduce disparity in mammography uptake between rural and urban areas, evidence-based multifaceted interventions designed to address the needs and concerns of the local populations are needed (29).
In an effort to increase information about small geographical areas, and to plan localized interventions, the CDC, in collaboration with the Robert Wood Johnson Foundation and the CDC Foundation, launched the 500 Cities Project in 2015 (30). Using small area estimation methods, this project provides estimates of chronic disease measures, unhealthy behaviors, and prevention practices including mammography use at the city and census tract levels. Although the 500 Cities project covers 33% of the population, it does not include rural areas and cities (except for WY, WV, and VT) with populations <66,000. Thus, our county-level mammography estimates fill a critical data need for rural areas and smaller cities, which represent two-thirds of the total US population.
Our analysis suggests new avenues of research into geographical and sociodemographic barriers to screening. County-level estimates can help with planning and resource allocation at the local level, by identifying areas that might be targeted for interventions to increase screening use. States lacking high quality county estimates can use our small area estimation method to generate their own county-level estimates by only including county random effects and excluding the state random effect. Census population data for post-stratification, can provide information to generate estimates for all counties in each state, including counties for which no direct estimates are available from BRFSS.
Limitations and strengths
We acknowledge several limitations. First, the results of our study are based on self-reported information without medical record validation. Second, the data is cross-sectional, and does not help determine cause and effect relationship between the covariates and the outcome. Third, although there is a possibility of over-reporting mammography use which can vary by demographic characteristics and may result in misclassification, our internal validation confirmed that the model-based estimates are consistent with the BRFSS estimates. Fourth, our unit-level multilevel model did not incorporate state-level and county-level structured spatial random effects. As a result, the predicted standard errors of our model-based small area estimates tend to be underestimated. Although our multilevel regression and post-stratification (MRP) approach for small area estimation has been validated internally and externally for county-level small area estimation (18), further research is needed to explore spatial structure effects on small area estimates in terms of bias and precision. Fifth, because mammography use included diagnostic and follow-up tests, we were not able to tell whether mammograms were specifically for screening (31). Finally, our predicted percentages of being current with mammography use might be more appropriate for program planning than for program evaluation because we do not include a variable for local interventions in our model.
Despite the limitations, our method provides more current estimates for all US counties. Although a more complex model might have fitted the data better, the results would not necessarily translate into better prediction. Our current model might not be the best model for prediction, but our internal validation confirmed that our models were appropriate to produce small area estimates, when aggregated, consistent with reliable direct survey estimates. Our national estimates were very similar to the BRFSS estimates and their 95% CIs largely overlapped. Furthermore, a recent study confirmed that unit-level multilevel models consistently perform better than area-level models in the context of small area estimation (32).
In conclusion, using data from a nationwide large survey with a linkage to census and the American Community Survey county-level data, our analysis found large variability in the prevalence of mammography use within many of the 50 states. This county-level variability cannot be captured by national or state-level analyses. Our method, which generated estimates for all the counties, identified many counties far below state-specific and national averages for mammography use. These estimates could be used to target interventions to overcome barriers to mammography in counties with low mammography use.
Supplementary Material
Acknowledgments
Financial disclosure: All authors are employees of the federal government and the work was performed as part of their official duties.
Footnotes
Conflict of interest: No potential conflicts of interest exist
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Economic Research Service, U.S. Department of Agriculture
References
- 1.Clinical Summary: breast cancer; screening. U.S. Preventive Services Task Force; January 2016. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/breast-cancer-screening. Accessed August 14, 2018. [Google Scholar]
- 2.Healthy people 2020. Office of Disease Prevention and Health Promotion. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/cancer/objectives. Accessed August 14, 2018.
- 3.White A, Thompson TD, White MC, Sabatino SA, deMoor J, Doria-Rose PV, Geiger AM, Richardson LC. Cancer screening test use—United States, 2015. MMWR 2017;66(8):201–206. DOI: 10.15585/mmwr.mm6608a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office of Surveillance, Epidemiology and Laboratory Services. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: 2014 Summary Data Quality Report. Atlanta, GA: Centers for Disease Control and Prevention; 2014. Available at: http://www.cdc.gov/brfss/annual_data/annual_2014.html. Accessed August 14, 2018. [Google Scholar]
- 5.Raghunathan TE, Xie D, Schenker N, Parsons V, Davis WW, Dodd KW, Feuer EJ. Combining Information from Two Surveys to Estimate County Level Prevalence Rates of Cancer Risk Factors & Screening. J Am Stat Assoc June 2007;102(478):474–86 [Google Scholar]
- 6.Feng X, Tan X, Alenzi EO, Rai P, Chang J. Spatial and temporal variations of screening for breast and colorectal cancer in the United States, 2008 to 2012. Medicine (Baltimore). 2016. December;95(51):e5656. doi: 10.1097/MD.0000000000005656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schneider KL, Lapane KL, Clark MA, Rakowski W. Using small-area estimation to describe county-level disparities in mammography. Prev Chronic Dis. 2009. October;6(4):A125. [PMC free article] [PubMed] [Google Scholar]
- 8.Mammography Prevalence within 2 Two Years (Age 40+). Maps and Data of Model-Based Small Area Estimates. Small Area Estimates for Cancer-Related Measures. National Cancer Institute, DCCPS, Statistical Research & Applications Branch, released October 2016 (sae.cancer.gov). Underlying data provided by Behavioral Risk Factor Surveillance System (http://www.cdc.gov/brfss/) and National Health Interview Survey (http://www.cdc.gov/nchs/nhis.htm)
- 9.Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L. Effectiveness of Breast Cancer Screening: Systematic Review and Meta-analysis to Update the 2009 U.S. Preventive Services Task Force Recommendation. Ann Intern Med. 2016. February 16;164(4):244–55. Accessed August 14, 2018. [DOI] [PubMed] [Google Scholar]
- 10.Bhargava S, Moen K, Qureshi SA, Hofvind S. Mammographic screening attendance among immigrant and minority women: a systematic review and meta-analysis. Acta Radiol. 2018. January 1:284185118758132. doi: 10.1177/0284185118758132. [DOI] [PubMed] [Google Scholar]
- 11.United States Census Bureau. American Community survey 2010 – 2014 state level estimation details. Available at: https://www.census.gov/programs-surveys/acs/data/summary-file.html Accessed August 14, 2018.
- 12.Zhang X, Holt JB, Lu H, Wheaton AG, Ford ES, Greenlund KJ, et al. Multilevel regression and post stratification for small-area estimation population health outcomes: A case study of chronic obstructive pulmonary disease prevalence using the Behavioral Risk Factor Surveillance System. Am J Epidemiol. 2014;179:1025–1033. [DOI] [PubMed] [Google Scholar]
- 13.Ryan Louise. Spatial Epidemiology: Some Pitfalls and Opportunities. Epidemiology. 2009;20(2):242–4. [DOI] [PubMed] [Google Scholar]
- 14.Condon P. Mixture of spatial and unstructured effects for spatially discontinuous health outcomes. Computational Statistics & data analysis. 2007:51;3197–212. [Google Scholar]
- 15.United States Census Bureau. Population Division. Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States, States, and Counties: April 1, 2010 to July 1, 2014. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed August 14, 2018.
- 16.Berkowitz Z, Zhang X, Richards TB, Nadel M, Peipins LA, Holt J. Multilevel small-area estimation of colorectal cancer screening in the United States. Cancer Epidemiology, Biomarkers and Prevention. Cancer Epidemiol Biomarkers and Prev. 2018;28(3): 245–253. Doi: 10.1158/1055-9965.EPI-17-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NCHS urban-rural classification scheme for counties. Data file documentation. Available at: https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf. Accessed August 14, 2018.
- 18.Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the Behavioral Risk Factor Surveillance System. Am J Epidemiol. 2015;182:127–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Y, Holt JB, Zhang X, Lu H, Shah SN, Dooley DP, et al. Comparison of methods for estimating prevalence of chronic diseases and health behaviors for small geographic areas: Boston validation study, 2013. Prev Chronic Dis 2017;14:170281 DOI: 10.5888/pcd14.170281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker K, Richardson LC. Invasive cancer incidence, 2004–2013, and death, 2006–2015, in nonmetropolitan and metropolitan counties-United States. MMWR Surveill Summ 2017:66(No. SS-14):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peipins LA, Miller J, Richards TB, Bobo JK, Liy T, White MC et al. Characteristics of US counties with no mammography capacity. J Community Health. 2012;37:1239–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.James CV, Moonesinghe R, Wilson-Frederick SM, Hall JE, Penman-Aguilar A, Bouye K. Racial/Ethnic Health Disparities Among Rural Adults — United States, 2012–2015. MMWR Surveill Summ 2017;66 (No. SS-23):1–9. DOI: 10.15585/mmwr.ss6623a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eberth JM, Eschbach K, Morris JS, Nguyen HT, Hossain MM, Elting LS. Geographic disparities in mammography capacity in the south: a longitudinal assessment of supply and demand. Health Serv Res. 2014;49:171–185. doi: 10.1111/1475-6773.12081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mammography use from 2000 to 2006: state-level trends with corresponding breast cancer incidence rates. Miller JW, King JB, Ryerson AB, Eheman CR, White MC. AJR Am J Roentgenol. 2009. February;192(2):352–60. doi: 10.2214/AJR.08.1757 [DOI] [PubMed] [Google Scholar]
- 25.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004;94(10):1682–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marré A. Rural Education at a Glance, 2017 Edition. US Department of Agriculture, Economic Research Service, Economic Information Bulletin 171; April 2017. Available at: https://www.ers.usda.gov/webdocs/publications/83078/eib-171.pdf?v=42830. Accessed August 14, 2018. [Google Scholar]
- 27.Hertz T. Rural Employment and Unemployment. US Department of Agriculture, Economic Research Service; 2017. Available at: https://www.ers.usda.gov/topics/rural-economy-population/employment-education/rural-employment-and-unemployment/. Updated July 6, 2017. Accessed August 14, 2018. [Google Scholar]
- 28.Alexandraki I, Mooradian AD. Barriers related to mammography use for breast cancer screening among minority women. Journal of the National Medical Association 2010; 102(3): 206–18. [DOI] [PubMed] [Google Scholar]
- 29.Wheeler SB, Davis MM. Commentary. “Taking the bull by the horns”: Four principles to align public health primary care, and community efforts to improve rural cancer control. The Journal of Rural Health. 2017;00:1–5. doi: 10.1111/jrh.12263.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. 500 Cities Project Data [online]. 2016. URL https://www.cdc.gov/500cities. Accessed August 14, 2018.
- 31.Miller JW, King JB, Joseph DA, Richardson LC. Breast Cancer Screening Among Adult Women — Behavioral Risk Factor Surveillance System, United States, 2010. Morbidity and Mortality Weekly Report (MMWR). Supplements. June 15, 2012. / 61(02);46–50. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/su6102a8.htm. Accessed August 14, 2018. [PubMed] [Google Scholar]
- 32.Hidiroglou MA, You Y. Comparison of unit level and area level small area estimators, Survey Methodology, 2016;42(1): 41–61. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.