Abstract
Objective:
Attention allocation to threat is perturbed in patients with posttraumatic stress disorder (PTSD), with some studies indicating excess attention to threat and others indicating fluctuations between threat vigilance and threat avoidance. The authors tested the efficacy of two alternative computerized protocols, attention bias modification and attention controltraining, for rectifying threat attendance patterns and reducing PTSD symptoms.
Method:
Two randomized controlled trials compared the efficacy of attention bias modification and attention control training for PTSD: one in Israel Defense Forces veteransand one in U.S. military veterans. Both utilized variants of the dot-probe task, with attention bias modification designed to shift attention away from threat and attention control training balancing attention allocation between threat and neutral stimuli. PTSD symptoms, attention bias, and attention bias variability were measured before and after treatment.
Results:
Both studies indicated significant symptom improvement after treatment, favoring attention control training. Additionally, both studies found that attention control training, but not attention bias modification, significantly reduced attention bias variability. Finally, a combined analysis of the two samples suggested that reductions in attention bias variability partially mediated improvement in PTSD symptoms.
Conclusions:
Attention control training may address aberrant fluctuations in attention allocation in PTSD, thereby reducing PTSD symptoms. Further study of treatment efficacy and its underlying neurocognitive mechanisms is warranted.
ClinicalTrials.gov registration identifiers: NCT01368302, NCT01564667.
Evidence indicates that the attention system of anxious individuals is biased toward threat (1–4). These findings have led to randomized controlled trials of attention bias modification, which showed moderate efficacy for anxiety disorders (5–8). Attention bias modification involves computerized cognitive training strategies designed to alter biases in attention (9–11). For example, in protocols intended to shift attention away from threat, response targets appear more frequently at the screen locations of neutral stimuli than at threat stimuli locations, inducing an implicitly learned association between the neutral stimulus and target location that gradually trains attention away from threat (12–14).
Given the attentional bias toward threat in anxiety disorder patients, attention bias modification for anxiety disorders such as social phobia (15, 16) and generalized anxiety disorder (17) typically trains attention away from threat. However, patterns of threat-related attention in patients with posttraumatic stress disorder (PTSD) are more variable than in anxiety disorders; some studies show a bias toward threat (18–20), whereas others show threat avoidance (21–25). Thus, while threat-related attention biases occur in PTSD, inconsistency in the direction of the findings raises questions about which type of protocol is most appropriate to rectify the observed aberrations—training attention away from threat, training attention toward threat, or applying a training protocol designed to balance fluctuations in threat-related attention bias. Indeed, a tendency for attention to fluctuate between threat vigilance and threat avoidance, called “attention bias variability,” reliably correlates with PTSD symptoms (26, 27). This may reflect a loss of attentional control and aberrant buffering of attention among participants with PTSD symptoms (28, 29).
To our knowledge, only two randomized controlled trials have used attention bias modification in PTSD. Schoorl et al. (30) compared attention bias modification and attention control training and found that the two regimens induced comparable reductions in PTSD symptoms, with no evidence of associations between changes in threat bias and symptoms. Kuckertz and colleagues (31) administered attention bias modification or attention control training in conjunction with cognitive-behavioral therapy and medication to military personnel with PTSD. While participants receiving either training regimen experienced reductions in PTSD symptoms, the group that received attention bias modification had fewer PTSD symptoms at posttreatment than the group that received attention control training. In that study, change in plasticity of attention bias in the attention bias modification group mediated change in PTSD symptoms.
We applied randomized controlled trial designs using variants of the dot-probe task to test the efficacy of attention bias modification versus attention control training in patients with PTSD. We measured changes in symptoms, attention bias, and attention bias variability from pre- to posttreatment. In study 1 we administered four sessions of word-based attention bias modification or attention control training to Israel Defense Forces veterans with PTSD. In study 2 we administered eight sessions of face-based attention bias modification or attention control training to veterans of the U.S. Armed Forces with PTSD.
STUDY 1
This study involved a double-blind randomized controlled trial of attention bias modification versus attention control training for combat-related PTSD in Israel Defense Forces veterans.
Method
Sample.
A CONSORT diagram of participant flow through the study is presented in Figure S1 in the data supplement accompanying the online version of this article. Male combat veterans (N=144) seeking treatment in the Israel Defense Forces‵ Unit for Treatment of Combat-Related PTSD formed the potential pool of participants. Veterans were included if they had PTSD as assessed with the Clinician-Administered PTSD Scale (CAPS) (32). The exclusion criteria were 1) psychotic or bipolar disorder, 2) nonfluent Hebrew, 3) inability to use a computer keyboard, 4) current psychotherapy, and 4) use of psychotropic medication that started within the past year. Candidates were admitted if they had been taking a stable dose of medication for at least 1 year (N=4); participants were removed from the study if their medication had to be changed during the trial. Eighty-seven candidates were excluded for not meeting the study’s inclusion criteria. Five candidates declined participation. The remaining 52 participants enrolled in the study were between the ages of 22 and 65 years (mean=36.05, SD=12.10) and were randomly assigned to the treatment groups. For all participants, PTSD had resulted from combat experiences that occurred at least 3 years prior to the beginning of the study (time from traumatic events ranged from 3 to 40 years, mean=14.14 years, SD=11.46). All participants provided complete pretreatment data (attention bias modification: N=27; attention control training: N=25); 13 participants from the bias modification group and 10 from the attention control group did not provide posttreatment data. All participants were included in an intention-to-treat analysis. The participants who provided full data sets did not differ from those who did not provide full data sets on age, PTSD and depression symptoms, attention bias, and attention bias variability before treatment (p>0.65).
The study was approved by the Israel Defense Forces and Tel Aviv University institutional review boards. Participants provided written informed consent.
Clinical diagnosis.
PTSD was diagnosed by means of the CAPS (32). This is a structured interview used to make a diagnosis of PTSD according to the DSM-IV criteria. It possesses good sensitivity, specificity, retest reliability, and validity (32). Interviews were conducted by four experienced clinicians (two clinical psychologists and two psychiatrists) specializing in diagnosis and treatment of combat-related PTSD. Consistency in diagnoses was ascertained by means of a weekly meeting in which the diagnostic data for each potential participant were discussed by the four independent evaluators. Diagnosis and comorbidity were determined by consensus. The comorbidity distribution is presented in Table S1 in the online data supplement.
Outcome measures.
Self-reported PTSD symptoms were evaluated by using the 17-item National Center for PTSD Checklist of the Department of Veterans Affairs (33–35). Symptoms were related to the participants‵ combat experience. Scores can range from 17 to 85, with higher scores reflecting more PTSD symptoms.
The Patient Health Questionnaire (36–39) is a self-reported depression rating scale consisting of nine items on which the diagnosis of DSM-IV major depression is based. Scores range from 0 to 27, with higher scores reflectingmore depression. Scale reliability and diagnostic validity have been described previously (37, 39).
Threat-related attention assessment.
Patterns of threat-related attention were evaluated by using the dot-probe task (40), with a variant similar to the one used by Bar-Haim et al. (24) and Wald et al. (23). Detailed description of the task is provided in the online supplement.
Two measures were derived from the dot-probe data: threat-related attention bias and attention bias variability. Threat-related attention bias was calculated as the difference between the mean reaction time for trials in which targets appeared at the neutral word location and the mean reaction time for trials in which targets appeared at the location of the threat-related word (i.e., time for neutral location minus time for threat-related location); positive values reflect attention bias toward threat. Attention bias variability was calculated in four steps: 1) a trial-by-trial moving average algorithm computed mean reaction times for all successive 10 neutral trial blocks and all successive 10 threat trial blocks, 2) successive attention bias scores were calculated by subtracting the first threat block average from the first neutral block average, the second threat block average from the second neutral block average, etc., forming a series of consecutive attention bias scores, 3) the standard deviation of these successive bias scores was then calculated, providing an index of variation in attention bias throughout the session, and 4) this standard deviation score was divided by the participant’s mean overall reaction time to control for associations between mean and variance. Attention bias variability reflects the within-session variability in threat-related attention bias, normalized to individual task performance (26, 27, 41).
Attention bias modification and attention control training.
The attention bias modification version of the dot-probe task used the same display characteristics as those used for assessment of threat-related attention, with two important modifications: 1) a different set of threat-neutral word pairs was used, and 2) target probes appeared only at the location previously occupied by neutral words, with the aim of implicitly establishing these as a predictive cue for probe location. The group receiving attention control training received the same number and type of trials as the group assigned to attention bias modification but in a fully counterbalanced manner. Participants received four sessions of attention bias modification or attention control training over 4 weeks while waiting for conventional treatment.
Procedure.
The participants went through the intake protocol of the Israel Defense Forces’ Unit for Treatment of Combat-Related PTSD, including the structured interview and questionnaires. Those meeting inclusion criteria were offered participation. After providing written informed consent, the participants completed the PTSD Checklist, the Patient Health Questionnaire, and the dot-probe assessment task. The participants were then randomly assigned to either attention bias modification or attention control training and completed four sessions—once a week for four weeks. One week following the last training session, the PTSD Checklist, Patient Health Questionnaire, and dot-probe assessment task were again administered.
Data analyses.
The baseline characteristics of the two treatment groups were compared by using independent-samples t tests. Intervention effects were analyzed by using random effects time series models in generalized estimating equations (42, 43). This enabled consideration of correlations between repeated measurements, and it addressed missing data through estimated marginal means relying on the entire sample of randomly assigned participants, taking into account all data collected at anytime point, including missing data. The generalized estimating equation models examined effects of the interaction between time (pretreatment, posttreatment) and treatment group (attention bias modification, attention control training) on attention bias, attention bias variability, and PTSD and depression symptoms. The analyses specified an unstructured correlation matrix to model the correlations between participant-specific intercepts and change slopes in outcomes. The terms for the interactions between time and treatment group (regressed on attention indices or symptoms) reflect the outcomes of interest from intention-to-treat analysis.
Results
Descriptive statistics for all variables are provided in Table 1. The treatment groups did not differ on any of the recorded measures before treatment (in all cases, p>0.10).
TABLE 1.
PTSD and Depression Symptom Scores, Threat-Related Attention Bias, and Attention Bias Variability in 52 Israeli Military Veterans Before and After Treatment With Attention Bias Modification or Attention Control Training (study 1)a
| Attention Bias Modification Training |
Attention Control Training |
|||||||
|---|---|---|---|---|---|---|---|---|
| Pretreatment |
Pretreatment |
Pretreatment |
Pretreatment |
|||||
| Measure | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| PTSD Checklist score | 60.39 | 1.77 | 56.57 | 2.74 | 58.29 | 1.84 | 45.34 | 3.58 |
| Patient Health Questionnaire score | 15.52 | 1.47 | 15.91 | 1.74 | 15.69 | 1.14 | 12.99 | 1.67 |
| Attention bias (ms)b | –3.83 | 6.71 | –1.50 | 6.38 | 18.75 | 10.80 | 8.65 | 6.68 |
| Attention bias variabilityb | 0.09 | 0.01 | 0.09 | 0.01 | 0.10 | 0.01 | 0.08 | 0.01 |
Not all participants provided posttreatment data.
Assessed with the dot-probe task (40). See text for description of measures.
Symptom change.
Generalized estimating equations of PTSD symptom change (measuredwith the PTSD Checklist) revealed a main effect of time (Wald χ2=19.83, df=1, p<0.0001) and a time-by-treatment group interaction effect (Wald χ2=28.22, df=3, p<0.0001). Reduction in PTSD symptoms from pre- to posttreatment was greater for attention control training than for attention bias modification (Figure 1A).
FIGURE 1. PTSD Symptoms and Attention Bias Variabilitya in 52 Israeli Military Veterans Before and After Treatment With Attention Bias Modification or Attention Control Training (study 1)b.
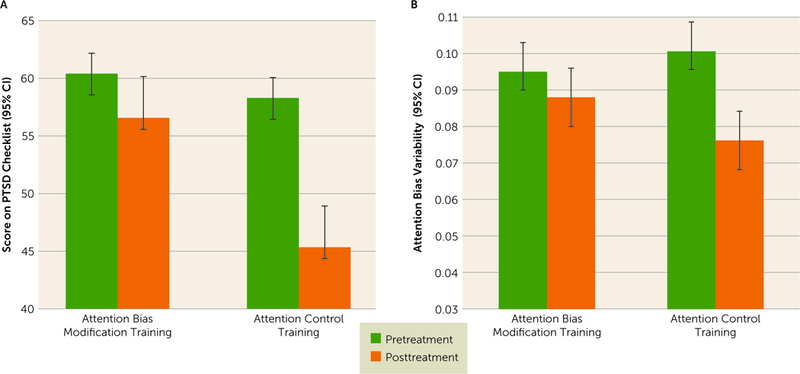
a Attention bias variability was assessed with the dot-probe task (40). See text for description of measures. b Not all participants provided posttreatment data.
The models of change in depression symptoms revealed nonsignificant main effects and a nonsignificant interaction of time and treatment group (p>0.30).
Change in attention bias variability and attention bias.
The models of change in attention bias variability revealed a main effect of time (Wald χ2=6.04, df=1, p<0.02) and a significant time-by-treatment interaction (Wald χ2=9.86, df=3, p=0.02) (Figure 1B). Reduction in attention bias variability from pre- to posttreatment was observed in the attention control training group (p=0.005) but not in the group that received attention bias modification (p=0.43).
The models of change in attention bias scores revealed nonsignificant main effects and time-by-treatment interaction (in all cases, p>0.05).
STUDY 2
This study involved a double-blind randomized controlled trial of attention bias modification versus attention control training for combat-related PTSD in veterans of the U.S. Armed Forces living in the Midwest.
Method
Sample.
A consort diagram is provided in Figure S2 in the online data supplement. A community sample of male U.S. military veterans who served in recent conflicts in Iraq and Afghanistan were recruited through television commercials, social media, and flyers. After verbally consenting, participants were screened for PTSD symptoms by telephone with the PTSD Checklist-Military Version (44). Veterans were eligible for inclusion if they had served in a war zone as part of the U.S. military any time since March 2003. The exclusion criteria were 1) psychotic, bipolar, or obsessive-compulsive disorder; 2) current substance dependence; 3) significant head injury; 4) current psychotherapy; and 5) use of psychotropic medication that started within 6 months prior to study recruitment (39%). Participants were removed from the study if their medication had to be changed during the trial. Of 76 veterans assessed for eligibility, 46 met the inclusion criteria. They ranged in age from 24 to 65 years (mean=32.43, SD=7.93). These veterans were randomly assigned to attention bias modification (N=22) and attention control training (N=24); five participants from the attention bias modification group and nine from the attention control training group did not provide posttreatment data. All participants were included in an intention-to-treat analysis. Participants who provided full data sets did not differ from those who did not on age, PTSD and depression symptoms, attention bias, and attention bias variability before treatment (p>0.16 in all cases).
The study was approved by the Creighton University institutional review board. All participants gave their written informed consent to participate in the trial.
Clinical diagnosis.
As in study 1, PTSD was diagnosed by using the CAPS (32). Diagnostic interviews were conducted by four interviewers: a psychologist specializing in PTSD, a master’s-level clinician with 30 years of experience, and two clinical psychology graduate students. Consistency in diagnoses was achieved by reliability training of the independent evaluators by an experienced psychologist trained in the Department of Veterans Affairs system. Diagnostic data for each participant were reviewed by the expert to validate diagnostic status. Additionally, the Mini International Neuropsychiatric Inventory (45) was used to assess exclusionary diagnoses. The comorbidity distribution is presented in Table S2 in the online data supplement.
Outcome measures.
Pre- and posttreatment scores on the CAPS (clinician-reported) and PTSD Checklist (self-reported) served as PTSD symptom outcomes. Pre- and posttreatment scores on the Patient Health Questionnaire served to measure depressive symptoms. For details, see the description for study 1.
Threat-related attention assessment.
A variant of the dot-probe task was used to assess threat-related attention patterns and to provide training in accordance with the TAU-NIMH Attention Bias Modification Treatment Initiative protocol (http://people.socsci.tau.ac.il/mu/anxietytrauma/research/). This version was based on faces (46), rather than words. A detailed description is presented in the online data supplement. As in study 1, attention bias and attention bias variability were calculated.
Attention bias modification and attention control training.
The attention bias modification version of the dot-probe task used the same display characteristics as those used for attention assessment with three modifications: 1) a different set of face pairs was used, 2) target probes appeared only at the location previously occupied by neutral faces, and 3) 160 rather than 120 trials were presented in each session. The attention control training group received the same number and types of trials as the attention bias modification group but in a fully counterbalanced manner. Participants received eight sessions of attention bias modification or attention control training over 4 weeks.
Procedure.
After meeting preliminary eligibility requirements, participants came to the clinic to discuss participation. Participants who gave their written informed consent completed a clinical interview, the PTSD Checklist and the Patient Health Questionnaire, and the dot-probe measurement task. Participants who met the inclusion criteria were randomly assigned to either attention bias modification or attention control training, and they returned to the clinic for eight training sessions (two sessions per week for 4 weeks). Following training completion, the participants were reassessed with the same measures employed during the pretreatment assessment. The participants were paid up to $285 for their time and travel to the clinic.
Data Analyses.
The analysis strategy was the same as in study 1.
Results
Descriptive statistics for all variables are provided in Table 2. The participants in the two treatment conditions did not differ on any of the collected measures before treatment (p>0.45 in all cases).
TABLE 2.
PTSD and Depression Symptom Scores, Threat-Related Attention Bias, and Attention Bias Variability in 46 U.S. Military Veterans Before and After Treatment With Attention Bias Modification or Attention Control Training (Study 2)a
| Attention Bias Modification Training |
Attention Control Training |
|||||||
|---|---|---|---|---|---|---|---|---|
| Pretreatment |
Pretreatment |
Pretreatment |
Pretreatment |
|||||
| Measure | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Clinician-Administered | 72.18 | 3.53 | 56.19 | 4.90 | 72.33 | 3.00 | 44.13 | 4.92 |
| PTSD Scale score | ||||||||
| PTSD Checklist score | 51.68 | 2.66 | 50.17 | 2.96 | 54.16 | 1.82 | 45.40 | 3.22 |
| Patient Health Questionnaire score | 11.59 | 1.12 | 12.01 | 1.31 | 11.58 | 1.26 | 9.26 | 1.30 |
| Attention bias (ms)b | –1.28 | 5.50 | 6.18 | 5.42 | –1.55 | 6.43 | –2.00 | 5.05 |
| Attention bias variabilityb | 0.06 | 0.01 | 0.06 | 0.01 | 0.06 | 0.01 | 0.04 | 0.00 |
Not all participants provided posttreatment data.
Assessed with the dot-probe task (40). See text for description of measures.
Symptom change.
Generalized estimating equations of PTSD symptom change as measured by the CAPS yielded a main effect of time (Wald χ2=42.15, df=1, p<0.0001) and a time-by-treatment interaction effect (Wald χ2=55.23, df=3, p<0.0001). The decrease in PTSD severity from pre- to posttreatment was greater for attention control training than for attention bias modification (Figure 2A).
FIGURE 2. Clinician- and Self-Reported PTSDSymptoms, DepressionSymptoms, and Attention Bias Variabilitya in 46 U.S. Military Veterans Before and After Treatment With Attention Bias Modification or Attention Control Training (Study 2)b.
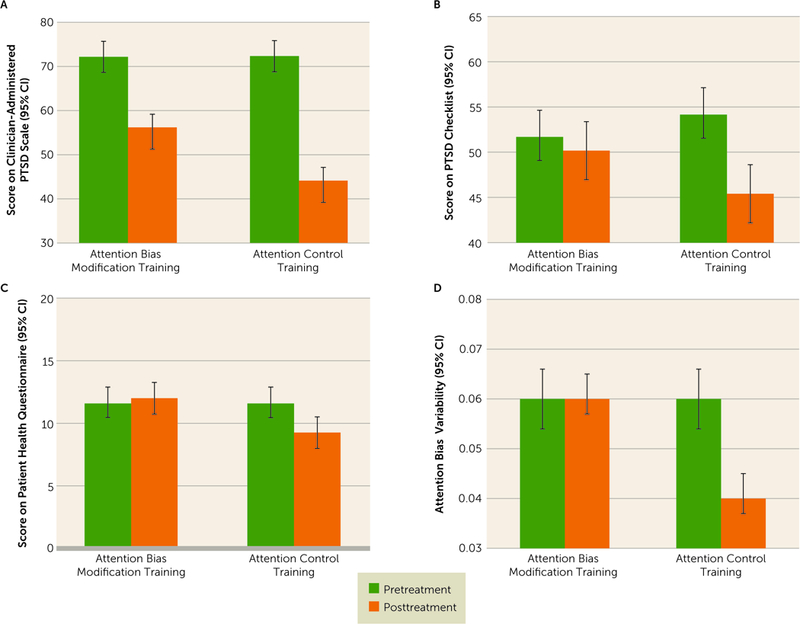
a Attention bias variability was assessed with the dot-probe task (40). See text for description of measures. b Not all participants provided posttreatment data.
The models of PTSD symptom change as measured by the PTSD Checklist also revealed a significant main effect of time (Wald χ2=7.06, df=1, p=0.008) and a significant time-by-treatment interaction effect (Wald χ2=15.30, df=3, p=0.002). A significant reduction in PTSD Checklist scores from pre- to posttreatment was observed in the attention control training group (p<0.0001) and not in the attention bias modification group (p=0.56) (Figure 2B).
Nonsignificant main effects of time and treatment group were found for change in depression symptoms (p>0.35 in both cases). A nonsignificant trend-level interaction between time and treatment group was observed (Wald χ2 =6.58, df=3, p=0.08), with a significant decrease in depression symptoms from pre- to posttreatment in the attention control training group (p=0.02) and not in the attention bias modification group (p=0.79) (Figure 2C).
Change in attention bias variability and attention bias.
Generalized estimating equations of change in attention bias variability revealed a main effect of time (Wald χ2=5.66, df=1, p=0.02) and a time-by-treatment interaction (Wald χ2=19.91, df=3, p<0.0001) (Figure 2D), with a significant decrease in attention bias variability in the attention control training group (p<0.0001) and not in the attention bias modification group (p=0.58). Analyses of change in attention bias scores revealed nonsignificant main effects and time-by-treatment interaction (p>0.53 in all cases).
Mediation of PTSD symptom change by change in attention bias variability.
To test for potential mediation of treatment effects on PTSD symptoms by change in attention bias variability, we used generalized estimating equations to determine whether the mediator-by-treatment interaction was significant (47). To increase analytic power we combined the two samples’ scores on the PTSD Checklist and attention bias variability, which were available in both studies. The three-way interaction of attention bias variability, time, and treatment was significant (Wald χ2=33.87, df=3, p<0.0001). Follow-up simple correlations between change in attention bias variability and change in PTSD Checklist score within each treatment group indicated that in the attention control training group, the decrease in attention bias variability from pre- to posttreatment was marginally correlated with the decrease in PTSD symptoms (r=0.36, N=28, p=0.06). A nonsignificant correlation was found in the attention bias modification group (r=–0.09, N=26, p=0.67) (Figure 3).
FIGURE 3. Relation of Change in PTSD Symptoms to Change in Attention Bias Variabilitya in 52 Israeli and U.S. Military Veterans After Treatment With Attention Bias Modification or Attention Control Training.
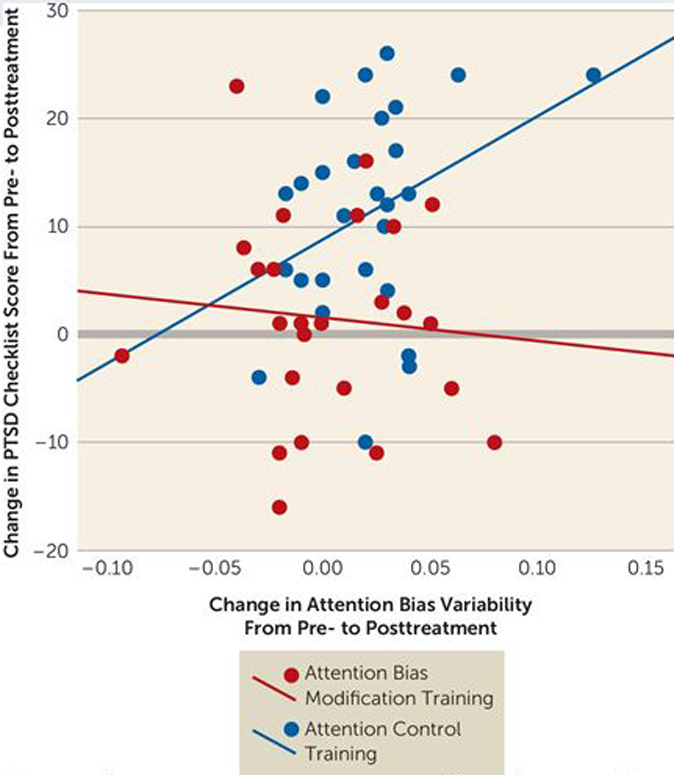
a Attention bias variability was assessed with the dot-probe task (40). See text for description of measures.
DISCUSSION
We conducted two separate randomized controlled trials of attention bias modification versus attention control training delivered as stand-alone treatments for combat-related PTSD. These trials were conducted in different countries (Israel, United States) with different stimuli sets (words, faces) and different treatment requirements (four and eight sessions); however, the results of the two trials were similar. Both trials supported attention control training over attention bias modification as the more efficacious training protocol for PTSD symptom reduction. Attention control training, but not attention bias modification, was associated with a decrease in attention bias variability, which has recently been identified as a core attentional perturbation present in PTSD (26, 27). Combining the two independent samples for mediation analysis revealed that change in attention bias variability mediated the reduction in PTSD symptoms in the attention control training group but not in the attention bias modification group. Neither treatment resulted in change in the classically calculated attention bias score.
The findings in the current study differ markedly from findings in other studies of attention bias modification for non-PTSD anxiety disorders. Whereas attention bias modification typically produces greater effects on symptoms than attention control training for anxiety disorders (8), we found the opposite pattern for PTSD. Whereas findings in non-PTSD anxiety disorders have been consistent, previous research has shown less consistent attention bias patterns in PTSD, with some research supporting attention bias toward threat (18–20) and other studies indicating attention bias away from threat (21–25). These disparate findings are consistent with the diagnostic criteria for PTSD, which include both threat vigilance and threat avoidance symptoms. Attention bias toward threat is the mechanism targeted by traditional attention bias modification for anxiety disorders; however, studies not producing the intended effect on attention bias may not reduce symptoms (11). Although attention bias modification was associated with reduced CAPS scores in study 2 (Figure 2A), neither of the two studies showed a change in threat-related attention bias. Thus, attention training away from threat is unlikely to represent an underlying mechanism of PTSD symptom reduction. Even so, the significant symptom reduction in the attention bias modification group in study 2 does provide some limited evidence that this training regimen might treat PTSD.
The current results support the importance of attention bias variability as a marker of PTSD, and they demonstrate that a reduction in attention bias variability is associated with reduced PTSD severity following attention control training. These findings resonate with recent reports that higher attention bias variability correlates with more severe PTSD (26, 27), and they extend this work by indicating that change in attention bias variability induced through attention control training appears to mediate clinical improvement in PTSD. The current findings also correspond with recent research suggesting that within-trial response variability may be a general marker of executive dysfunction in PTSD (48) and that fluctuations in trial-level bias scores may provide more appropriate expressions of underlying attention bias conceptualizations (49). Consistent with this emerging literature, attention bias variability appears to capture the attentional shifts toward and away from threat in PTSD more accurately than static measures of attention bias.
Recently Kuckertz and colleagues (31) suggested that training direction (toward or away from threat) may be less important than establishing the training contingency between emotional stimuli and task completion, which would require top-down attentional control. However, our results suggest that attention control training may be more effective than attention bias modification designed to train attention away from threat, by enhancing attentional control in PTSD. In attention control training, participants respond to probes appearing equally often after threatening and neutral stimuli, essentially requiring that participants ignore irrelevant threat-related contingencies to most efficiently complete the task at hand. In our trials, attention control training appeared to normalize strong within-task fluctuations in threat-related attention bias, which are typical of patients with PTSD (26,27). In attention control training, participants implicitly learn that the threatening stimuli, which likely deplete attentional resources in PTSD, are irrelevant to task performance. The emergence of this more balanced attention allocation is supported by the reduction in attention bias variability in the attention control training arm of both trials and by the mediation effect of change in attention bias variability on PTSD symptom reduction noted for attention control training but not for attention bias modification. More research is needed to replicate these findings and to clarify the exact cognitive mechanisms underlying reduction in attention bias variability through attention control training. Understanding could be enhanced by neurophysiological research designed to assess the impact of attention control training and attention bias modification on dynamic brain functioning. Testing of attention bias modification designed to train attention toward threat in PTSD is also in order.
The current studies did not reveal therapeutic effects for depression symptoms. This is consistent with the largely inconclusive evidence for threat-related attention bias and efficacy of attention training in depression (7). Such effects, when observed in depression, are usually found with sad rather than angry faces and with longer stimulus presentation durations than used here (50). It is interesting that a previous study found that word-based attention bias modification had no effect on depression, whereas face-based attention bias modification did (51). Here, study 1 applied a word-based task and found no effects on depression, whereas study 2 applied a face-based task and found a trend-level reduction in depression symptoms. Future research could test training variants that may be effective for both PTSD and comorbid depression.
The results of the current studies should be viewed in light of some limitations and opportunities for further research. First, although high dropout rates are common in PTSD treatment research (52), future studies of attention training should explore ways to reduce dropouts (e.g., enhance engagement with the task, enhance the treatment alliance). Concerns regarding generalizability due to large dropout rates are alleviated to an extent by the intention-to-treat analyses and the direct replication in two independent studies. Second, given that attention bias variability has emerged as a partial mediator of the reported therapeutic effect, it would be useful to include measures of general attentional control in future studies.
In summary, traditional attention bias modification is thought to reflect an implicitly learned association between stimulus location and target location (12–14). In the case of attention bias modification for anxiety, this learning targets attention bias toward threat by training attention away from threat (5, 9, 53). However, in PTSD no specific direction of attention bias has been ascertained; rather, PTSD is characterized by fluctuations in attention bias, reflected in high attention bias variability. Attention control training requires equal attention allocation to threatening and neutral stimuli and thus appears to balance moment-to-moment fluctuations in attention bias from threat vigilance to threat avoidance (Table 3). In line with this assumption, our results indicate that attention control training, more so than attention bias modification, not only helps regulate attention bias variability in PTSD patients, but also results in significantly reduced trauma-related distress as assessed by both self- and clinician-reported PTSD severity.
TABLE 3.
Comparison of Attention Bias Modification and Attention Control Training
| Characteristic | Attention Bias Modification Training | Attention Control Training |
|---|---|---|
| Goal | Train attention bias away from threat | Normalize fluctuations in threat-related |
| attention bias | ||
| Training | Over repeated trials patients are taught | Over repeated trials patients are taught |
| to expect targets to appear at the | that emotional or neutral cues do not | |
| location of neutral rather than | predict target location and thus it is | |
| threat-related stimuli | preferable to ignore irrelevant | |
| contingencies | ||
| Evidence of clinical efficacy | Anxiety disorders (e.g., social anxiety disorder, generalized anxiety disorder) | PTSD |
| Effect on attention bias variability | No effect | Decrease |
Supplementary Material
Acknowledgments
Partially supported by a grant from the nonprofit organization At Ease USA. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
All authors report no financial relationships with commercial interests.
REFERENCES
- 1.Bar-Haim Y, Lamy D, Pergamin L, et al. : Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull 2007; 133:1–24 [DOI] [PubMed] [Google Scholar]
- 2.Armstrong T, Olatunji BO: Eye tracking of attention in the affective disorders: a meta-analytic review and synthesis. Clin Psychol Rev 2012; 32:704–723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cisler JM, Koster EHW: Mechanisms of attentional biases towards threat in anxiety disorders: an integrative review. Clin Psychol Rev 2010; 30:203–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yiend J: The effects of emotion on attention: a review of attentional processing of emotional information. Cogn Emotion 2010; 24:3–47 [Google Scholar]
- 5.Hakamata Y, Lissek S, Bar-Haim Y, et al. : Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biol Psychiatry 2010; 68:982–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beard C, Sawyer AT, Hofmann SG: Efficacy of attention bias modification using threat and appetitive stimuli: a meta-analytic review. Behav Ther 2012; 43:724–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hallion LS, Ruscio AM: A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychol Bull 2011; 137: 940–958 [DOI] [PubMed] [Google Scholar]
- 8.Linetzky M, Pergamin-Hight L, Pine DS, et al. : Quantitative evaluation of the clinical efficacy of attention bias modification treatment for anxiety disorders. Depress Anxiety 2015; 32:383–391 [DOI] [PubMed] [Google Scholar]
- 9.Bar-Haim Y: Research review: attention bias modification (ABM): a novel treatment for anxiety disorders. J Child Psychol Psychiatry 2010; 51:859–870 [DOI] [PubMed] [Google Scholar]
- 10.MacLeod C, Koster EHW, Fox E: Whither cognitive bias modification research? commentary on the special section articles. J Abnorm Psychol 2009; 118:89–99 [DOI] [PubMed] [Google Scholar]
- 11.Clarke PJF, Notebaert L, MacLeod C: Absence of evidence or evidence of absence: reflecting on therapeutic implementations of attentional bias modification. BMC Psychiatry 2014; 14:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacLeod C, Mathews A: Cognitive bias modification approaches to anxiety. Annu Rev Clin Psychol 2012; 8:189–217 [DOI] [PubMed] [Google Scholar]
- 13.Abend R, Karni A, Sadeh A, Fox NA, Pine DS, Bar-Haim Y: Learning to attend to threat accelerates and enhances memory consolidation. PloS One 2013; 8(4):e62501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abend R, Pine DS, Fox NA, et al. : Learning and memory consolidation processes of attention bias modification in anxious and non-anxious individuals. Clin Psychol Sci 2014; 2:620–627 [Google Scholar]
- 15.Amir N, Beard C, Taylor CT, et al. : Attention training in individuals with generalized social phobia: a randomized controlled trial. J Consult Clin Psychol 2009; 77:961–973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmidt NB, Richey JA, Buckner JD, et al. : Attention training for generalized social anxiety disorder. J Abnorm Psychol 2009; 118:5–14 [DOI] [PubMed] [Google Scholar]
- 17.Amir N, Beard C, Burns M, et al. : Attention modification program in individuals with generalized anxiety disorder. J Abnorm Psychol 2009; 118:28–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buckley TC, Blanchard EB, Neill WT: Information processing and PTSD: a review of the empirical literature. Clin Psychol Rev 2000; 20:1041–1065 [DOI] [PubMed] [Google Scholar]
- 19.Bryant RA, Harvey AG: Attentional bias in posttraumatic stress disorder. J Trauma Stress 1997; 10:635–644 [DOI] [PubMed] [Google Scholar]
- 20.Fani N, Tone EB, Phifer J, et al. : Attention bias toward threat is associatedwith exaggerated fear expression and impaired extinction in PTSD. Psychol Med 2012; 42:533–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wald I, Degnan KA, Gorodetsky E, et al. : Attention to threats and combat-related posttraumatic stress symptoms: prospective associations and moderation by the serotonin transporter gene. JAMA Psychiatry 2013; 70:401–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beevers CG, Lee HJ, Wells TT, et al. : Association of predeployment gaze bias for emotion stimuli with later symptoms of PTSD and depression in soldiers deployed in Iraq. Am J Psychiatry 2011; 168:735–741 [DOI] [PubMed] [Google Scholar]
- 23.Wald I, Lubin G, Holoshitz Y, et al. : Battlefield-like stress following simulated combat and suppression of attention bias to threat. Psychol Med 2011; 41:699–707 [DOI] [PubMed] [Google Scholar]
- 24.Bar-Haim Y, Holoshitz Y, Eldar S, et al. : Life-threatening danger and suppression of attention bias to threat. Am J Psychiatry 2010; 167: 694–698 [DOI] [PubMed] [Google Scholar]
- 25.Constans JI, McCloskey MS, Vasterling JJ, et al. : Suppression of attentional bias in PTSD. J Abnorm Psychol 2004; 113:315–323 [DOI] [PubMed] [Google Scholar]
- 26.Iacoviello BM, Wu G, Abend R, et al. : Attention bias variability and symptoms of posttraumatic stress disorder. J Trauma Stress 2014; 27: 232–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naim R, Abend R, Wald I, et al. : Threat-related attention bias variability and post traumatic stress. Am J Psychiatry (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schoorl M, Putman P, Van Der Werff S, et al. : Attentional bias and attentional control in posttraumatic stress disorder. J Anxiety Disord 2014; 28:203–210 [DOI] [PubMed] [Google Scholar]
- 29.Bardeen JR, Orcutt HK: Attentional control as a moderator of the relationship between posttraumatic stress symptoms and attentional threat bias. J Anxiety Disord 2011; 25:1008–1018 [DOI] [PubMed] [Google Scholar]
- 30.Schoorl M, Putman P, Van Der Does W:Attentionalbias modification in posttraumatic stress disorder: a randomized controlled trial. Psychother Psychosom 2013; 82:99–105 [DOI] [PubMed] [Google Scholar]
- 31.Kuckertz JM, Amir N, Boffa JW, et al. : The effectiveness of an attention bias modification program as an adjunctive treatment for post-traumatic stress disorder. Behav Res Ther 2014; 63:25–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blake DD, Weathers FW, Nagy LM, et al. : The development of a clinician-administered PTSD scale. J Trauma Stress 1995; 8:75–90 [DOI] [PubMed] [Google Scholar]
- 33.Blanchard EB, Jones-Alexander J, Buckley TC, et al. : Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996; 34: 669–673 [DOI] [PubMed] [Google Scholar]
- 34.Kang HK, Natelson BH, Mahan CM, et al. : Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol 2003; 157:141–148 [DOI] [PubMed] [Google Scholar]
- 35.Hoge CW, Castro CA, Messer SC, et al. : Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351:13–22 [DOI] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL: The PHQ-9:a new depression and diagnostic severity measure. Psychiatr Ann 2002; 32:509–521 [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Löwe B, Kroenke K, Herzog W, et al. : Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord 2004; 81: 61–66 [DOI] [PubMed] [Google Scholar]
- 39.Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 1999; 282:1737–1744 [DOI] [PubMed] [Google Scholar]
- 40.MacLeod C, Mathews A, Tata P: Attentional bias in emotional disorders. J Abnorm Psychol 1986; 95:15–20 [DOI] [PubMed] [Google Scholar]
- 41.Price RB, Kuckertz JM, Siegle GJ, et al. : Empirical recommendations for improving the stability of the dot-probe task in clinical research. Psychol Assess (Epub ahead of print, November 24, 2014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zeger SL, Liang KY: Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986; 42:121–130 [PubMed] [Google Scholar]
- 43.Zeger SL, Liang KY, Albert PS: Models for longitudinal data: a generalized estimating equation approach. Biometrics 1988; 44: 1049–1060 [PubMed] [Google Scholar]
- 44.Weathers FW, Litz BT, Herman DS, et al. : The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. San Antonio, Tex, International Society of Traumatic Stress Studies, 1993. http://www.pdhealth.mil/library/downloads/PCL_sychometrics.doc [Google Scholar]
- 45.Sheehan DV, Lecrubier Y, Sheehan KH, et al. : The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59(suppl 20): 22–33 [PubMed] [Google Scholar]
- 46.Tottenham N, Tanaka JW, Leon AC, et al. : The NimStim set of facial expressions: judgments from untrained research participants. Psychiatry Res 2009; 168:242–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fitzmaurice GM, Laird NM, Ware JH: Applied Longitudinal Analysis. Hoboken, NJ, Wiley, 2004, pp 291–395 [Google Scholar]
- 48.Swick D, Honzel N, Larsen J, et al. : Increased response variability as a marker of executive dysfunction in veterans with post-traumatic stress disorder. Neuropsychologia 2013; 51:3033–3040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zvielli A, Bernstein A, Koster EHW: Dynamics of attentional bias to threat in anxious adults: bias towards and/or away? PLoS One 2014; 9:e104025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gotlib IH, Krasnoperova E, Yue DN, et al. : Attentional biases for negative interpersonal stimuli in clinical depression. J Abnorm Psychol 2004; 113:121–135 [DOI] [PubMed] [Google Scholar]
- 51.Browning M, Holmes EA, Charles M, et al. : Using attentional bias modification as a cognitive vaccine against depression. Biol Psychiatry 2012; 72:572–579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Imel ZE, Laska K, Jakupcak M, et al. : Meta-analysis of dropout in treatments for posttraumatic stress disorder. J Consult Clin Psychol 2013; 81:394–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pine DS, Helfinstein SM, Bar-Haim Y, et al. : Challenges in developing novel treatments for childhood disorders: lessons from research on anxiety. Neuropsychopharmacology 2009; 34:213–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


