Abstract
Introduction:
Scapular fractures are rare injuries and are often an indicator of high-energy trauma. These injuries are rare, and many are managed without surgery. The caveat to this is intra-articular extension into the glenoid when AO Foundation principles of fracture fixation for intra-articular injuries must be adhered to. We report a percutaneous arthroscopically assisted technique for fixation of a scapular fracture with extension into the glenoid fossa in a young male patient.
Case Report:
A 22-year-old Caucasian male presented to the emergency department after a road traffic collision. Primary assessment and secondary surgery demonstrated an isolated shoulder injury involving the glenoid. Three-dimensional imaging was performed and revealed an intra-articular glenoid fracture with the involvement of the superior suspensory apparatus of the shoulder, not fitting into known classification systems. He underwent an arthroscopically assisted percutaneous screw fixation, which resulted in reduction of the suspensory apparatus and the glenoid fossa.
Conclusion:
Intra-articular glenoid involvement in scapular fractures mandates anatomical reduction through internal fixation. We highlight that this technique is of benefit in these injuries and is easy and quick to perform. Validated outcomes, in this case, have been excellent, with no adverse events.
Keywords: Arthroscopic assisted, percutaneous, fixation, glenoid, trauma
Learning Point for the Article:
An arthroscopic assisted, percutaneous technique demonstrates excellent medium term outcomes for intra articulate glenoid.
Introduction
Scapular fractures are rare injuries and typically result from high-energy trauma such as road traffic accidents and falls from height[1]. Accurate classification of these fractures, based on radiological imaging, facilitates optimum management and long-term shoulder function. We present a unique case of scapular fracture which does not fit entirely with any existing classifications. This was treated with a unique arthroscopically assisted, percutaneous fixation technique with excellent post-operative patient-reported outcomes.
Case Report
A 22-year-old male presented to casualty with the left shoulder pain following a road traffic accident. Examination revealed reduced movements of the left shoulder in all planes. Neurovascular examination was unremarkable and no other injuries identified. Radiographs revealed anintra-articular fracture of the left scapula with disruption of the acromioclavicular joint (Fig. 1a). To help further assess the extent of injury, computed tomography with 3D reconstruction was performed which showed a comminuted fracture of the scapula involving the glenoid and body of the scapula (Fig. 1b).
Figure 1.
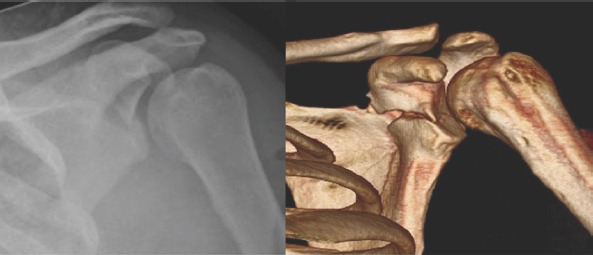
(a)Plain anteroposteriorradiograph illustrating the intra-articular scapular fracture with acromioclavicular joint disruption. (B)3D CT (anterior view) demonstrating a comminuted scapular fracture involving the glenoid.
The patient underwent surgical fixation using a unique technique for repair of an intra-articular glenoid fracture with reduction of an associated acromioclavicular disruption.
Surgical technique
The procedure was performed in the “beach chair” position under general anesthesia. Intravenous antibiotic prophylaxis, as per unit policy, was administered. Standard anterior and posterior arthroscopic port sites allowed for direct visualization of the glenoid and facilitated washout of the fracture hematoma (Fig. 2a and b). Pre-operative concerns were of a capsular tear which would risk fluid extravasation around the brachial plexus. However, at the time of arthroscopy, the capsule was found to be intact. Once the fracture site was thoroughly debrided, a single 2.5mm threaded guidewire was placed in the superior-inferior plane percutaneously to act as a joystick to reduce the large fragment. When the guidewire was in position, two 2mm Kirschner wires were used to hold the fragment in place. Three 4.5mm low profile, partially threaded cannulated screws (Arthrex, FL, USA)were inserted percutaneously. One screw failed at the thread-shaft junction during insertion with the distal part being left in situ, providing compression to the fracture site and restoration of stability. The remaining screws achieved compression at the fracture site, which were visualized simultaneously with the arthroscope, restoring the articular surface and reduction of the acromioclavicular joint (Fig. 2c). Clinical follow-up was performed postoperatively, and validated subjective functional scores completed by one of the authors, either in person or through telephone consultation with the patient. Correlation from time to surgery and outcome scores was recorded and P value calculated for the progression over time. P<0.05 was considered statistically significant.
Figure 2.

(a)Intraoperative arthroscopic image of the glenoid fracture before washout and removal of the fracture hematoma. (b) After washout, the intra-articular fracture of the glenoid can be clearly seen. There is evidence of intra-articular loose bodies (c) Arthroscopic view of the articular surface after reduction with three percutaneous screws.
Discussion
Scapular fractures are uncommon comprising 3–% of shoulder fractures and <1% of all fractures [1]. This is largely due to its mobility on the chest wall, protection provided by muscles, and the surrounding musculoskeletal structures, including the clavicle and acromioclavicular joint, which typically give way first following injury. Fractures of the scapula and glenoid cavity usually require direct high-energy trauma, with road traffic collisions causing more than 60% of these injuries [1]. Not surprisingly, more than 80% of patients with a scapular fracture have associated injuries which may be life-threatening [2, 3]. Only a few classifications exist for scapular fractures, largely due to their infrequent occurrence. Existing classifications typically relate to the anatomical region involved based on radiographic findings. The orthopedic trauma association classification for scapular fractures describes extra-articular, intra-articular, and combined fracture patterns[4]. In addition, Ideberg, Mayo et al., and Goss, each describe intra-art icular scapular fractures[5, 6, 7]. The aforementioned fracture pattern lies somewhere between the Orthopaedic Trauma Association classification 14-C3, Ideberg Type III, and Goss Type III [4, 5, 8]. Goss also introduced the concept of the superior shoulder suspensory complex (SSSC) to help identify patterns of certain shoulder injuries and guide management[6]. The SSSC refers to a ring of bony and soft tissue structures, namely the glenoid, coracoid process, coracoclavicular ligament, distal part of the clavicle, acromioclavicular joint, and acromion process[6]. Goss maintained that disruption of two or more components of the complex would result in an unstable or “floating” shoulder, commonly requiring surgical treatment[6]. However, recent experience suggests that if there is significant displacement of a scapular fracture, particularly the glenoid, surgical management should be considered to help prevent functional disability [6, 9]. In the above case, not only was there an intra-articular fracture of the glenoid, but the patient also had acromioclavicular disruption requiring surgical intervention. Ideberg’s original classification describes a Type III fracture that is an oblique fracture through the glenoid exiting superiorly. It has been modified to include an associated acromioclavicular joint injury in recent years. Ogawa described a Type Icoracoid injury, whereby the fracture is proximal to the coracoclavicular ligament. The injury seen above, in this case, does not conform to either yet bears hallmarks of both. This is the first reported case of a glenoid fracture with associated acromioclavicular joint disruption, both of which were corrected by a percutaneous approach. Open reduction and internal fixation of the scapula is indicated in displaced fractures the extend into the glenoid articular surface if a step of >3mm is encountered, and more than 20% of the joint is involved[10]. Other indications include as follows:
Unstable shoulder girdle based on multiple disruptions of the superior SSSC- the so-called “floating” shoulder.
Medialization>10mm.
Angular deformity of 25–° [6, 11, 12].
Arthroscopic repair of the shoulder joint is commonly described in the surgical treatment of glenoid labrum injuries; however, there have only been small case reports and case series regarding arthroscopic-assisted fixation of scapula fractures. There is a reported case of Kirchner wire fixation of a glenoid fracture[13]. Fewer reports have looked specifically at percutaneous internal fixation of fracture[13, 14, 15, 16, 17]. In a small series of patients, Ideberg Type IA intra-articular glenoid fractures have been repaired by arthroscopy-assisted techniques with excellent results in 70% of individuals, with low complication rates [12]. Arthroscopic-assisted surgical fixation of Ideberg Type III glenoid fractures is reported to be a safe and effective method of treatment, yielding excellent functional results with union of the fractures, with few associated complications as a result of the surgery [17]. A cadaveric study demonstrated that superiorly placed percutaneous fixation, as in this case, represents a safe approach to fixation of the glenoid arthroscopically[18].
Patient outcome
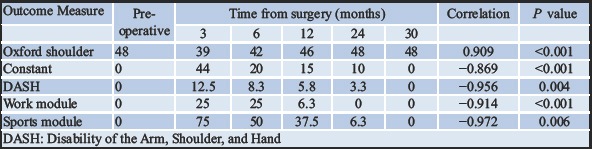
Follow-up of the patient at 3, 6, 12, 24, and 30 months was performed. Functional outcomes scores including constant score, Oxford shoulder, and disability of the arm, shoulder, and hand (DASH) were performed. Radiographs at 3 months and 30 months are shown in Fig. 3. Table 1 summarizes the functional scores over time, which has shown significant improvement during the post-operative period. In the case of negative correlations, this showed that reductions in the difference in DASH scores between shoulders occurred over time, indicating a return of normal function. Currently, the patients have returned to work as a manual shop assistant, plays rugby and cricket, with no pain, functional limitation, or restriction on activities of daily living.
Figure 3.
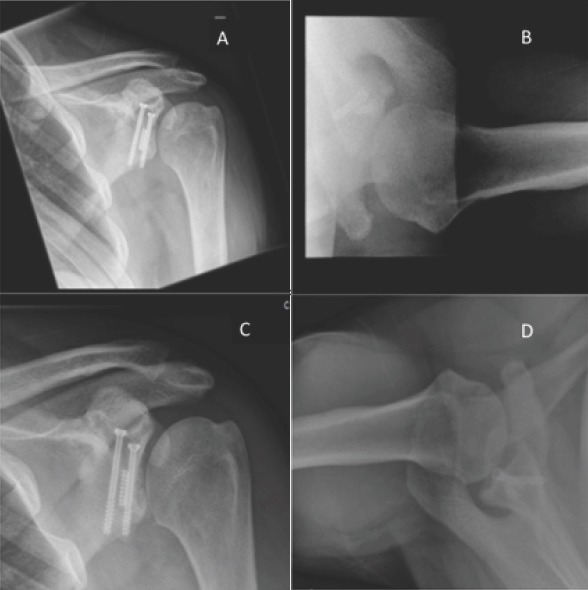
(a and b) Radiographs of the glenohumeral joint anteroposterior (AP) and shoulder axial views at 3 months post-surgery. (candd)Radiographs of the glenohumeral joint AP and shoulder axial views at 30 months post-surgery.
Table 1.
Patient-reported outcome scores for the Oxford shoulder, Constant shoulder score, and DASH
Conclusion
We describe a unique case of an unclassified isolated scapular fracture in a young male, involving the glenoid fossa and associated acromioclavicular joint disruption. This posed a challenge regarding management due to a lack of specific guidelines and available data on functional outcomes. We report the first case involving a unique approach for arthroscopic-assisted repair of an intra-articular glenoid fracture, with subsequent reduction of the acromioclavicular joint, using percutaneous, variable pitched headless screws. While the body of literature available consists of small number case series only, arthroscopic repair of intra-articular glenoid fractures is an effective technique for the experienced surgeon, associated with good functional outcomes. We, therefore, advocate arthroscopic-assisted percutaneous screw fixation for intra-articular glenoid fractures.
Clinical Message
Scapula fractures involving the glenoid require anatomical reduction and fixation in keeping with AO principles. This can be achieved through an arthroscopically assisted technique as described, with excellent medium-term outcomes.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Coimbra R, Conroy C, Tominaga GT, Bansal V, Schwartz A. Causes of scapula fractures differ from other shoulder injuries in occupants seriously injured during motor vehicle crashes. Injury. 2010;41:151–5. doi: 10.1016/j.injury.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Balwin KD, Ohman-Strickland P, Mehta S, Hume E. Scapula fractures:A marker for concomitant injury?A retrospective review of data in the national trauma database. J Trauma. 2008;65:430–5. doi: 10.1097/TA.0b013e31817fd928. [DOI] [PubMed] [Google Scholar]
- 3.Tadros AM, Lunsio K, Czechowski J, Abu-Zidan FM. Multiple-region scapular fractures had more severe chest injury than single-region fractures:A prospective study of 107 blunt trauma patients. J Trauma. 2007;63:889–93. doi: 10.1097/01.ta.0000235876.32569.db. [DOI] [PubMed] [Google Scholar]
- 4.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium - 2007:Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 5.Goss TP. Scapular fractures and dislocations:Diagnosis and treatment. J Am AcadOrthopSurg. 1995;3:22–33. doi: 10.5435/00124635-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7:99–106. doi: 10.1097/00005131-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa. Results of open reduction and internal fixation. ClinOrthopRelat Res. 1998:122–30. [PubMed] [Google Scholar]
- 8.Ideberg R, Grevsten S, Larsson S. Epidemiology of scapular fractures. Incidence and classification of 338 fractures. ActaOrthopScand. 1995;66:395–7. doi: 10.3109/17453679508995571. [DOI] [PubMed] [Google Scholar]
- 9.Herrera DA, Anavian J, Tarkin IS, Armitage BA, Schroder LK, Cole PA, et al. Delayed operative management of fractures of the scapula. J Bone Joint Surg Br. 2009;91:619–26. doi: 10.1302/0301-620X.91B5.22158. [DOI] [PubMed] [Google Scholar]
- 10.Cole PE, Shafiq B. Scapula Fractures:Open Reduction and Internal Fixation in Master Techniques in Orthopaedic Surgery:Fractures. 2nd ed. Ch. 2. Philadelphia, PA: Lippincott Williams and Wilkin; 2006. p. 16. [Google Scholar]
- 11.Cole PA, Gauger EM, Herrera DA, Anavian J, Tarkin IS. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury. 2012;43:327–33. doi: 10.1016/j.injury.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 12.Tauber M, Moursy M, Eppel M, Koller H, Resch H. Arthroscopic screw fixation of large anterior glenoid fractures. Knee Surg Sports TraumatolArthrosc. 2008;16:326–32. doi: 10.1007/s00167-007-0437-2. [DOI] [PubMed] [Google Scholar]
- 13.Carro LP, Nuñez MP, Llata JI. Arthroscopic-assisted reduction and percutaneous external fixation of a displaced intra-articular glenoid fracture. Arthroscopy. 1999;15:211–4. doi: 10.1053/ar.1999.v15.015021. [DOI] [PubMed] [Google Scholar]
- 14.Al-Khateeb H, Edwards A, Goldie B, Ahmed H. Arthroscopy-Assisted Reduction and Percutaneous Fixation of Glenoid Fractures. Vienna: Poster Presented at 10th European Federation of National Association of Orthopaedics and Traumatology (EFORT) Congress; 2009. pp. 3–6. [Google Scholar]
- 15.Gigante A, Marinelli M, Verdenelli A, Lupetti E, Greco F. Arthroscopy-assisted reduction and percutaneous fixation of a multiple glenoid fracture. Knee Surg Sports TraumatolArthrosc. 2003;11:112–5. doi: 10.1007/s00167-002-0340-9. [DOI] [PubMed] [Google Scholar]
- 16.Yallapragada R, Patel K, Davuluri P, Sloan A, Marynissen H. Arthroscopy-assisted percutaneous fixation of glenoid fossa fracture. Int J Shoulder Surg. 2007;1:96–9. [Google Scholar]
- 17.Yang HB, Wang D, He XJ. Arthroscopic-assisted reduction and percutaneous cannulated screw fixation for ideberg Type III glenoid fractures:A minimum 2-year follow-up of 18 cases. Am J Sports Med. 2011;39:1923–8. doi: 10.1177/0363546511408873. [DOI] [PubMed] [Google Scholar]
- 18.Marsland D, Ahmed HA. Arthroscopically assisted fixation of glenoid fractures:A cadaver study to show potential applications of percutaneous screw insertion and anatomic risks. J Shoulder Elbow Surg. 2011;20:481–90. doi: 10.1016/j.jse.2010.08.003. [DOI] [PubMed] [Google Scholar]


