Abstract
Introduction:
Many factors influence bone health, but osteoporosis is viewed as a calcium deficiency disorder in which bone is resorbed to maintain the serum calcium levels. Dietary calcium supplements have been recommended for the prevention of osteoporosis in the elderly. Many forms of dietary calcium supplements are widely available in market, but products containing calcium citrate and calcium carbonate are the most common. Calcium lysinate, a new form of calcium preparation, may have a better absorption and can be a better calcium supplement.
Aim:
The aim of this study is to evaluate the efficacy, safety, and bioavailability of calcium lysinate in comparison to other calcium supplements in improving the bone mineral density (BMD) status in osteopenia patients.
Methodology:
A total of 24 osteopenia patients were randomly divided into three groups of eight subjects in each. Anyone of the study drug, namely, calcium lysinate, calcium carbonate, or calcium citrate malate was administered to each group. Blood samples for the determination of serum calcium was taken, based on which the area under the curve (absorption profile) and relative bioavailability were calculated. BMD was assessed on the day 0 and at 8 weeks’ post-treatment.
Results:
The relative oral bioavailability of calcium lysinate was 223.15%. There is a significant improvement in the T-score of BMD in all the groups. It was more significant in calcium lysinate group (P < 0.0004).
Conclusion:
The high oral bioavailability of calcium lysinate, high percentage of calcium content, and a good clinical improvement in the BMD T-scores of osteopenia patients suggest that calcium lysinate will serve as a better dietary calcium supplement.
Keywords: Calcium lysinate, bone mineral density, bioavailability, osteopenia
Learning Point for the Article:
Calcium Lysinate is having better efficacy and bioavailability compared to calcium Citrate malate and calcium carbonate.
Introduction
Osteoporosis is a skeletal disorder characterized by a decrease in bone mass, compromised bone strength, and an increase in bone fragility predisposing to fracture [1]. It is an important health problem in Western and developing countries; in the United States alone, it is estimated that 10 million people have osteoporosis, whereas 18 million people have low bone density (having osteopenia) placing them at risk of this disorder [1, 2]. Osteopenia is characterized by bone loss that is not as severe as osteoporosis. Osteopenia patients land up in osteoporosis sooner or later. If we are able to identify and treat osteopenia at an early stage, we can prevent the complications that occur due to osteoporosis. Many factors influence bone health, but osteoporosis is viewed as a calcium deficiency disorder in which bone is resorbed to maintain the serum calcium levels when the excretion of calcium is not getting balanced by calcium absorption [2, 3, 4]. Calcium from the diet is absorbed primarily in the intestine and is the essential nutrient for attaining the peak bone mass during adolescence and for the prevention and treatment of osteoporosis [1]. Recommendations of daily dietary calcium intake range from 400 to 1200 mg per day depending on age and gender. This has been issued by many governmental and non-governmental organizations in many countries [1, 5]. Since many of the modern diets which we consume do not provide the recommended levels of calcium, dietary calcium supplements have been recommended for the prevention of osteoporosis in the elderly. It is also being recommended for other medical conditions including hypertension, hypercholesterolemia, and cancer [6]. Many forms of dietary calcium supplements are widely available in market, but products containing calcium citrate and calcium carbonate are the most common [5, 6, 7]. Over the past 20 years, the absorption of calcium from various forms of dietary supplements has been studied by various methods. Few studies have shown the more soluble calcium citrate to be better absorbed than the relatively insoluble calcium carbonate, whereas others have shown the opposite result, and still other studies have found no significant difference [8, 9]. The lack of consensus between these two important forms of calcium supplements has been ascribed in part to the differences in study design, differences in the analytical methods, and genetic and other factors that differ between individuals [9, 10]. Calcium lysinate is a chelate of calcium and an amino acid, L-lysine which is an essential amino acid and is actively absorbed from the intestinal tract. The European Food Safety Authority concluded that the use of calcium lysinate used in food supplements as a source of calcium is not of safety concern at the proposed use levels. Calcium lysinate chelate consists of calcium bonded to two molecules of lysine. Calcium lysinate provides the bioavailable calcium higher than the other calcium salts. Certain calcium supplements that are not chelated have been shown to interfere with the absorption of some other minerals, particularly with iron. Unlike these sources of calcium, calcium lysinate does not ionize in the gut, thus eliminating the potential to interfere with iron absorption. L-lysine can both enhance intestinal Ca absorption and improve the renal conservation of the absorbed Ca. The combined effects may contribute to a positive Ca balance, thus suggesting a potential usefulness of L-lysine supplements for both preventive and therapeutic interventions in osteoporosis [11,12]. Therefore, the study aims to compare the relative oral bioavailability of calcium from a single dose of calcium lysinate to that of calcium citrate malate (CCM) and calcium carbonate and to evaluate the efficacy of the different calcium supplements in improving the bone mineral density in osteopenia patients.
Aim and objective
The aim of this study is as follows:
To evaluate the efficacy of calcium lysinate in comparison to other calcium supplements in improving the bone mineral density (BMD) status in osteopenia patients.
To compare the bioavailability and safety of calcium lysinate (CALNIFIT) with that of the standard drugs calcium carbonate (SHELCAL) and CCM.
Hypothesis
Is Calcium lysinate effective, safe, and better absorbed when compared with two other calcium preparations, namely, calcium carbonate (SHELCAL) and CCM?
Methodology
The study was conducted over a duration of 6 months from July 2017 to December 2017 at a Clinical Research Organization (Quest Life Sciences) in Chennai after getting Ethics Committee approval from an Independent Ethics Committee (Ethica Norma). Both male and female subjects with an age group of 40–years, who are diagnosed to have osteopenia using a BMD T-score (score between −1.0 and −2.5), were included in the study. Calcaneal BMD was assessed using CM.200 light instrument. Subjects who had a presence of any other comorbid disease conditions, smoking, and alcohol or drug dependence and subjects who were allergic to any of the calcium supplements such as calcium lysinate, calcium carbonate, and CCM were excluded from the study. A total sample size of 24 (considering this as a pilot phase 2 study) osteopenia patients were enrolled in the study after screening 80 subjects for their BMD scores. Participants who satisfied the inclusion and exclusion criteria underwent general and systemic examination followed by laboratory tests for complete hematological, biochemical, and urine analysis, electrocardiogram, and chest X-ray. Only subjects who were not suffering from any comorbid conditions, with the mentioned normal laboratory test profiles, normal ECG, and chest X-ray were enrolled in the study. Eligible subjects were randomly (computer-generated randomization) divided into three groups of eight subjects in each. We selected subjects of similar age group (30–years range with male and female equally distributed). There was no statistically significant difference in the demographic data between the groups. The study participants were kept in overnight fasting for 10 h on the day 1 of the study. Anyone of the study drug, namely, calcium lysinate (CALNIFIT), calcium carbonate (SHELCAL), and CCM was administered to each subject in the morning at the same time of the day based on the randomization generated along with 240 ml (8 ounces) of water. During the subsequent 4.5 h after tablet ingestion, subjects were allowed water ad libitum, but no other beverage or food was allowed until after the last blood sample was collected. Venous blood samples for the determination of serum calcium were taken immediately before ingestion of the calcium preparations (time 0) and at 30, 60, 90, 135, 180, 225, and 270 min post-dose on the day 1. Blood samples were processed in ERBA CHEM 5, using semi analyzer method to determine the serum calcium levels, based on which the area under the curve (AUC) (absorption profile) and relative bioavailability were calculated. The subjects were then advised to take the respective calcium tablets according to their classified groups on a daily basis for a period of 8 weeks and they were followed up once in every 2 weeks for compliance check. Efficacy was evaluated statistically by assessing the improvement in BMD T-score of osteopenia at the end of 8 weeks, by means of paired student t-test using GraphPad Prism version 5.0. Pharmacokinetic calculations were made using Winnonlin software 6.4 version.
Result
After administration of CCM, serum calcium concentrations rose slowly but steadily reaching a plateau approximately above baseline by 180 min post-dose. At 225 and 270 min post-dose, the increases following CCM were significantly greater like that of calcium carbonate (Table 1). After calcium lysinate administration, the time profile of serum calcium was strikingly different compared with the other two treatment groups (Table 2 and 3). As early as 30 min post-dose, serum calcium had risen by 13%, and by 60 min, it reached a plateau value about 24% above baseline that was maintained from 60 to at least 180 min post-dose, after which there was a rise in serum calcium which again came back to a plateau around 225 and 270 min post-dose (Fig. 1). The relative oral bioavailability of the test when compared with the reference SHELCAL was calculated using the formula: F= AUC T *Dose R/AUC R * Dose T (F=43.9 * 500/39.3 * 250). Relative Bioavailability, F=223.15% (Table 4). Error! Not a valid link. Paired t-test (two tailed) was applied between pre- and post-BMD of calcium lysinate group. P < 0.0004, which is highly significant*** (t = 6.381 df = 7), (Table 5). P < 0.0042 for calcium carbonate group which is also statistically significant **(t = 4.161 df = 7). P < 0.0069 for CCM group which is also statistically significant *(t = 3.776 df = 7). There is a significant improvement in the T-score of BMD in all the groups. It was more significant in calcium lysinate group (Fig. 2). Five subjects reported symptoms of abdominal bloating and belching during the 1st week of the study period, which resolved on its own. Of the five subjects, three belonged to calcium carbonate group and one each belonged to calcium lysinate and CCM group.
Table 1.
Mean serum calcium values of different calcium supplements
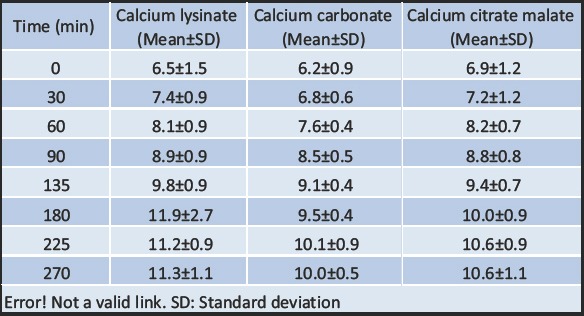
Table 2.
The pharmacokinetic parameters derived for the increments in serum calcium concentration (i.e., the change from zero time baseline values) observed in this study
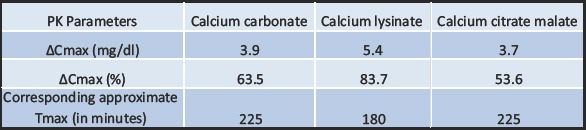
Table 3.
The percentage increment in the mean serum calcium concentration (i.e., the changes from zero time baseline values)
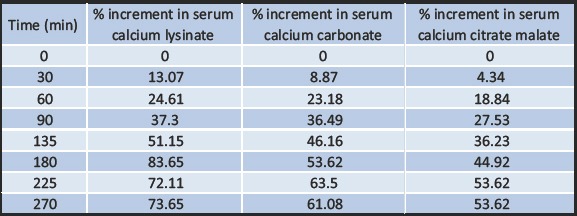
Figure 1.
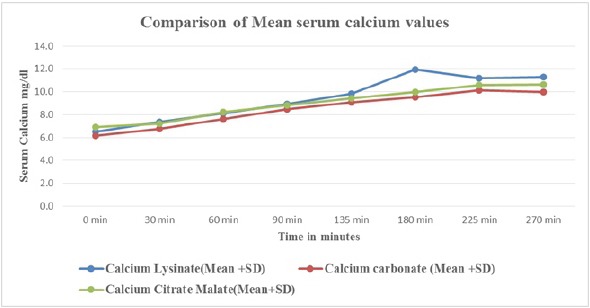
The comparison of the mean serum calcium levels of different calcium supplements.
Table 4.
Elemental calcium and absorption percentage of calcium lysinate
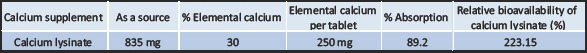
Table 5.
Bone mineral density (T-Score) - pre- and post-study comparison

Figure 2.
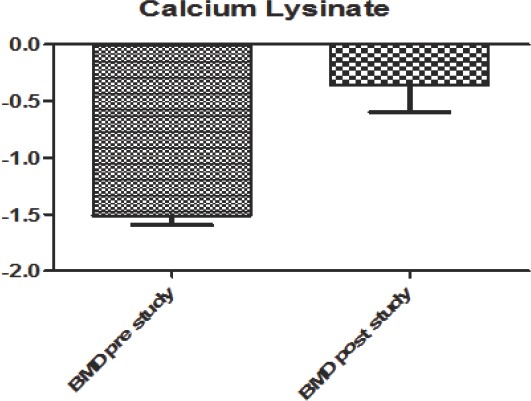
Comparison of pre- and post-study bone mineral density score of calcium lysinate group showed high significance of improvement in T score.
Discussion
In this study, calcium lysinate was clearly superior to both calcium carbonate and CCM in ability to deliver calcium to the bloodstream after oral administration and calcium lysinate may offer significant advantages as a dietary calcium supplement. The time course and percentage of calcium absorption are being affected by a number of variables including dose size, rate of gastric emptying, and the rate of disintegration and dissolution of the dosage form to release the absorbable amount of calcium. In addition, the results might also be influenced by length of time post dosing and the number of observations made across the time period. Heaney et al. [13] compared the serum calcium concentration versus time curves (0–h) after administration of two forms of calcium carbonate, one form of calcium citrate, or a placebo to a group of 24 postmenopausal women. In their results, the pharmacokinetic data showed no significant differences among the three calcium preparations in terms of ΔCmax, tmax, ΔAUC (0–or 0–h) or the bioavailability of calcium. In this study, serum calcium concentrations rose by 5–% within 3 h, remained constant from 3 to 5 h, and then decreased. Heller et al. [8] also used another pharmacokinetic approach to investigate the relative bioavailability of calcium from calcium carbonate and calcium citrate in 18 healthy women but found a greater bioavailability of calcium from that of calcium citrate than from the calcium carbonate. In another study, Heaney [14] administered 300–-mg doses of precipitated calcium carbonate to 12 healthy men. A serum calcium concentration versus time profile similar to that of his earlier study in women [13] was observed. Significantly, the absorption fraction (determined from the 5 h specific activity of serum 45Ca) was strongly and linearly correlated to the ΔAUC for serum calcium increment integrated out to 24 h when the absorption phase would certainly have been completed. In our study, though the length of the observation period of calcium sampling was probably not sufficient to capture the entire absorption profile of each calcium supplement, it was more than adequate to demonstrate a significant difference in absorption rate and the net calcemic response (assessed using the relative bioavailability results) between calcium lysinate and the other two supplements, namely, calcium carbonate and CCM. The bioavailability of an orally administered exogenous compound is defined as the fraction of the dose that reaches the systemic circulation. Bioavailability is often determined pharmacokinetically by comparing the dose-normalized AUC, an oral versus an intravenous dose, i.e., F= (AUCpo/Dosepo)/(AUCiv/Doseiv). For calcium, which is an endogenous substance, measurement of absolute bioavailability of an oral dose requires the use of isotopic methods, but for assessing relative oral bioavailability, the pharmacokinetic method is a convenient and acceptable tool. Hence, the same was applied here. Relative bioavailability with reference to SHELCAL (Calnifit/SHELCAL) = 223.15%. The literature reference shows that absorption of calcium carbonate is 22% [15] and that of CCM is 42% [16], considering its elemental calcium of 40% and 24%, respectively. A study done by Bristow et al. showed that calcium citrate and calcium carbonate have equivalent efficacy in suppressing bone turnover [17]. Moreover, it has also been shown that hydroxyl apatite complexes are better when compared to different calcium supplements, as it is also having analgesic properties in osteopenic perimenopausal women [18]. In case of calcium lysinate which is having an elemental calcium of 30% amounting to 250 mg per tablet, has shown a marked increase in the rate of absorption when compared with that of calcium carbonate. When the bioavailability of calcium lysinate was compared with that of calcium carbonate, we found that it was 223.15%, which amounts to 89.2% of calcium absorption. The benefits of calcium supplements to bone strength and health are thought to derive from the increased availability of serum calcium for bone deposition. In our study, there is a significant improvement in the BMD scores, in all the three formulations. It is showing a significant improvement in SHELCAL and CCM group. However, it is showing high significance of improvement in calnifit group. Thus, of the three formulations, calcium lysinate is showing a better improvement in BMD T-score when compared with calcium carbonate and CCM.
Conclusion
Dietary supplementation with calcium may be necessary for the good health of individuals and is also widely practiced. The fact that calcium lysinate gave substantially significant increase in serum calcium concentration, higher AUC for the mean serum calcium concentration, and a significant improvement in the BMD T-scores than the other form of calcium supplements such as calcium carbonate or CCM suggests that calcium lysinate may have considerable promise for use as a new dietary calcium supplement.
Clinical Message
Calcium lysinate was clearly superior to both calcium carbonate and CCM in its ability to deliver calcium to the bloodstream and to improve the BMD T-score after oral administration. The high oral bioavailability of calcium lysinate, high percentage of calcium content, and a good clinical improvement in the BMD T-scores of osteopenia patients suggest that calcium lysinate will serve as a better dietary calcium supplement.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.NIH consensus development panel on osteoporosis prevention, diagnosis, and therapy, march 7-29 2000:Highlights of the conference. South Med J. 2001;94:569–73. [PubMed] [Google Scholar]
- 2.Charles P. Calcium absorption and calcium bioavailability. J Intern Med. 1992;231:161–8. doi: 10.1111/j.1365-2796.1992.tb00519.x. [DOI] [PubMed] [Google Scholar]
- 3.Reginster JY, Denis D, Bartsch V, Deroisy R, Zegels B, Franchimont P, et al. Acute biochemical variations induced by four different calcium salts in healthy male volunteers. Osteoporos Int. 1993;3:271–5. doi: 10.1007/BF01623832. [DOI] [PubMed] [Google Scholar]
- 4.Wood RJ, Martini L. Reply to R. P. Heaney. Am J Clin Nutr. 2003;78:493–494. [Google Scholar]
- 5.Levenson DI, Bockman RS. A review of calcium preparations. Nutr Rev. 1994;52:221–32. doi: 10.1111/j.1753-4887.1994.tb01427.x. [DOI] [PubMed] [Google Scholar]
- 6.Porter C. Vitamin and mineral supplements:Part 1. Rx Consultant. 2003;12:1–8. [Google Scholar]
- 7.Sakhaee K, Bhuket T, Adams-Huet B, Rao DS. Meta-analysis of calcium bioavailability:A comparison of calcium citrate with calcium carbonate. Am J Ther. 1999;6:313–21. doi: 10.1097/00045391-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Heller HJ, Stewart A, Haynes S, Pak CY. Pharmacokinetics of calcium absorption from two commercial calcium supplements. J Clin Pharmacol. 1999;39:1151–4. [PubMed] [Google Scholar]
- 9.Heaney RP. Factors influencing the measurement of bioavailability, taking calcium as a model. J Nutr. 2001;131:S1334–48. doi: 10.1093/jn/131.4.1344S. [DOI] [PubMed] [Google Scholar]
- 10.Abrams SA, Copeland KC, Gunn SK, Gundberg CM, Klein KO, Ellis KJ. Calcium Absorption, Bone Mass Accumulation, and Kinetics Increase during Early Pubertal Development in Girls. The Journal of Clinical Endocrinology &Metabolism, Volume 85, Issue 5, 1 May. 2000:1805. doi: 10.1210/jcem.85.5.6508. [DOI] [PubMed] [Google Scholar]
- 11.Aguiar F, Autrup H, Barlow S, Castle L, Crebelli R, Dekant W, et al. Opinion on certain lysinates as sources for magnesium, calcium and zinc. EFSA J. 2008;261:2–11. [Google Scholar]
- 12.Civitelli R, Villareal DT, Agnusdei D, Nardi P, Avioli LV, Gennari C. Dietary L-lysine and calcium metabolism in humans. Nutrition. 1992;8:400–5. [PubMed] [Google Scholar]
- 13.Heaney RP, Dowell MS, Bierman J, Hale CA, Bendich A. Absorbability and cost effectiveness in calcium supplementation. J Am Coll Nutr. 2001;20:239–46. doi: 10.1080/07315724.2001.10719038. [DOI] [PubMed] [Google Scholar]
- 14.Heaney RP. Quantifying human calcium absorption using pharmacokinetic methods. J Nutr. 2003;133:1224–6. doi: 10.1093/jn/133.4.1224. [DOI] [PubMed] [Google Scholar]
- 15.Recker RR, Bammi A, Barger-Lux MJ, Heaney RP. Calcium absorbability from milk products, an imitation milk, and calcium carbonate. Am J Clin Nutr. 1988;47:93–5. doi: 10.1093/ajcn/47.1.93. [DOI] [PubMed] [Google Scholar]
- 16.Andon MB, Peacock M, Kanerva RL, DeCastro JA. Calcium absorption from apple and orange juice fortified with calcium citrate malate (CCM) J Am Coll Nutr. 1996;15:313–6. doi: 10.1080/07315724.1996.10718604. [DOI] [PubMed] [Google Scholar]
- 17.Bristow SM, Gamble GD, Stewart A, Horne L, House ME, Aati O, et al. Acute and 3-month effects of microcrystalline hydroxyapatite, calcium citrate and calcium carbonate on serum calcium and markers of bone turnover:A randomised controlled trial in postmenopausal women. Br J Nutr. 2014;112:1611–20. doi: 10.1017/S0007114514002785. [DOI] [PubMed] [Google Scholar]
- 18.Castelo-Branco C, Dávila J, Alvarez L, Balasch J, et al. Comparison of the effects of calcium carbonate and ossein-hydroxyapatite complex on back and knee pain and quality of life in osteopenic perimenopausal women. Maturitas. 2015;81:76–82. doi: 10.1016/j.maturitas.2015.02.265. [DOI] [PubMed] [Google Scholar]


