ABSTRACT
Migrants may experience immunisation inequities compared with the host population related to barriers with accessing immunisations in their home countries, while migrating and/or post-arrival. This retrospective cohort study explored vaccination rates among migrant and non-migrant children in New Zealand (NZ). Linked de-identified data from various government sources from 1 January 2006 to 31 December 2015 were analysed using Statistic NZ’s Integrated Data Infrastructure. Vaccination rates were compared between three cohorts of children aged up to 5 years: foreign-born children who migrated to NZ; children born in NZ of migrant mothers; and a comparator group of children born in NZ to non-migrant mothers. Less than half of foreign-born children (46%) had a record in the NZ National Immunisation Register compared with 95% and 96% among migrant and non-migrant NZ-born children, respectively. Foreign-born migrant children had lower age-appropriate reported vaccination rates by vaccine of interest, ethnicity and visa category compared with NZ-born children. Migrant children from Pacific ethnicities had lower reported coverage than other ethnicities. High rates of not age-appropriately vaccinated were noted among foreign-born children on refugee, Pacific and humanitarian visa schemes. This study highlights possible shortfalls around immunisation data, particularly about recording vaccinations given overseas for foreign-born children, and potential challenges around engagement with immunisation services for migrant children. However, results highlight the successful engagement of quota refugee children as part of NZ’s refugee orientation programme. It is important to monitor vaccination coverage by migrant and refugee background to inform improvements to policy and practice for wider population health benefits.
Keywords: Immunisation, inequity, child, data-linking, migrant, refugee, New Zealand
Introduction
Increased international migration has resulted in an unprecedented number of migrants and refugees.1–3 Migrants are those who reside outside their country of birth irrespective of the reason for migration while refugees are those who have been forcibly displaced outside their native country due to fear of persecution.4,5 Migration to New Zealand (NZ) has been steadily increasing; migrants now represent almost a quarter of NZ’s total population.6,7 In accordance with NZ’s human rights framework, approximately 750 refugees, known as quota refugees, are resettled every year and additional refugees are accepted under various humanitarian and family reunification schemes.8 Children make up approximately half of the refugee intake in Australia and NZ and are arguably the most vulnerable subgroup.9,10
International outbreaks of vaccine-preventable diseases (VPDs) have been linked to under-immunised migrant populations.11,12 Migrant and refugee children are noted to be particularly at risk of VPDs as many have incomplete or unknown immunisation status and few have serological immunity against some VPDs.13,14 Arriving migrants may be under-immunised due to multiple factors, such as coming from resource poor countries with suboptimal immunisation coverage and facing interruptions of routine vaccinations while migrating.11 Post-arrival, migrants may experience barriers with receiving immunisations attributed to socio-cultural differences, difficulties accessing health services, economic troubles, limited language proficiency and health literacy, and/or inadequate medical information and advice.11,13,15
To provide optimal protection against VPDs and prevent against disease outbreaks, it is important for children to receive timely childhood vaccinations. In NZ, all children under the age of 18 years are eligible to receive publicly funded National Immunisation Schedule (NIS) vaccines, regardless of their immigration and citizenship status.16 No specific immunisation data focusing on migrant and refugee children are currently available. Although national vaccination coverage rates are high overall, these may mask substantial shortfalls among migrant and refugee children. The aim of this study was to use de-identified linked datasets with immigration information to examine if there were differences in age-appropriate immunisation coverage rates among children with and without migrant backgrounds.
Results
Description of cohorts
Figure 1 shows the number of children included in each cohort after applying the exclusions. Of the total study population, 10.9% were foreign-born migrants (Cohort A), 7.2%were NZ-born migrants (Cohort B), and 81.9% were NZ-born non-migrants (Cohort C). Among Cohort A (N = 75,375), the largest group of foreign-born migrants were of European ethnicity with 21.7% identifying as European and 8.8% as NZ European. Other large migrant groups were those of Indian (5.6%) and Chinese (4.2%) ethnicity. Of those with visa data (54.2%), the combined categories of work, visitor and student visas were the most common (37.0%). Small numbers arrived on refugee-related visas, with only approximately 1% on convention, quota, family and humanitarian visas. Regarding the longest length of time spent in NZ, more than half of Cohort A (68.0%) had been in NZ for more than 1 year.
Figure 1.
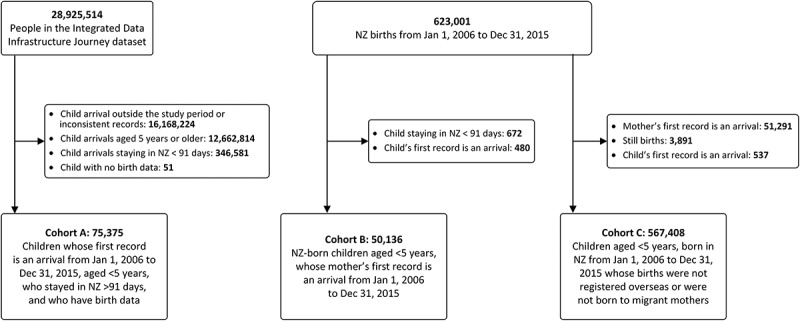
Participant flow chart of children for Cohorts A, B and C and exclusions (some children were counted in multiple exclusion categories). Note it is the policy of Statistics New Zealand that counts are randomly rounded to a number divisible by 3 in order to protect privacy; thus, the numbers of inclusions and exclusions will not reconcile precisely.
Among Cohort B, NZ-born migrant children (N = 50,136), just above a quarter identified as European or NZ European (28.3%). The combined Asian ethnic group was the largest (48.9%) with high representation from Indian (19.7%) and Chinese (11.3%) sub-groups. Of those with visa data (92.1%), most children were born to migrant mothers who first came to NZ during the study period on work, visitor or student visas (44.6%). A small proportion of NZ-born children had mothers with refugee backgrounds (3.6%). More than half of the NZ-born non-migrant children in Cohort C (N = 567,408) identified as having European or NZ European ethnicity (54.1%); other large ethnic groups were NZ Māori (25.0%) and Pacific (10.6%).
Recorded vaccination status
The majority of NZ-born children in Cohorts B (N = 48,177, 96.1%) and C (N = 536,805, 94.6%) had an enrolment record or at least one recorded vaccination event in the National Immunisation Register (NIR). Among Cohort A, less than half (N = 34,599, 45.9%) of eligible children had a record in the NIR. The likelihood of foreign-born migrant children having a record in the NIR increased with time spent in NZ. Only 12% of children who stayed in NZ for up to 6 months had a record in the NIR, while 60% of those who stayed in NZ for 2 or more years were included in the NIR.
Of all the vaccines included in this analysis, the highest age-appropriate vaccination coverage was for MMR and pertussis-containing vaccines across all cohorts (Table 1). Low age-appropriate coverage rates were noted for the rotavirus vaccine; this is likely to be because it was introduced to the NIS in 2014. Most children were age-appropriately vaccinated for each vaccine of interest, except within Cohort A for PCV and rotavirus where most children were unvaccinated. NZ-born children of recent migrant mothers (Cohort B) and of non-migrant mothers (Cohort C) had higher recorded age-appropriate vaccination rates for all antigens of interest compared with foreign-born migrant children (Cohort A). For all of the vaccines of interest, children in Cohort A generally had higher proportions of delayed and partial vaccinations compared to children in Cohorts B and C.
Table 1.
Recorded vaccination status by vaccine for each cohort from January 1, 2006 to December 31, 2015, New Zealand. ‘Out of range’ = MMR vaccine given before 12 months old or possibly indicates a data error (e.g., vaccine recorded as given prior to birth) for the other vaccines.
| Cohort A |
Cohort B |
Cohort C |
||||
|---|---|---|---|---|---|---|
| N = 75,375 |
N = 50,136 |
N = 567,408 |
||||
| Total number in cohort | n | (%) | n | % | n | % |
| Measles, mumps and rubella | ||||||
| Vaccinated-on time | 23,703 | (68.5) | 39,372 | (81.7) | 444,633 | (82.8) |
| Vaccinated-delayed | 3,042 | (8.8) | 2,385 | (5.0) | 37,797 | (7.0) |
| Vaccinated-partial | 5,835 | (16.9) | 2,025 | (4.2) | 26,466 | (4.9) |
| Unvaccinated | 936 | (2.7) | 4,254 | (8.8) | 26,490 | (4.9) |
| Out of range | 1,083 | (3.1) | 141 | (0.3) | 1,416 | (0.3) |
| Total | 34,599 | 48,177 | 536,805 | |||
| Pneumococcal conjugate vaccine† | ||||||
| Vaccinated-on time | 7,239 | (20.9) | 33,129 | (68.8) | 282,951 | (52.7) |
| Vaccinated-delayed | 5,361 | (15.5) | 4,419 | (9.2) | 83,025 | (15.5) |
| Vaccinated-partial | 9,033 | (26.1) | 2,724 | (5.7) | 23,568 | (4.4) |
| Unvaccinated | 12,774 | (36.9) | 7,872 | (16.3) | 147,036 | (27.4) |
| Out of range | 192 | (0.6) | 30 | (0.1) | 225 | (< 0.1) |
| Total | 34,599 | 48,177 | 536,805 | |||
| Pertussis | ||||||
| Vaccinated-on time | 18,201 | (52.6) | 37,524 | (77.9) | 432,528 | (80.6) |
| Vaccinated-delayed | 3,264 | (9.4) | 2,157 | (4.5) | 38,367 | (7.1) |
| Vaccinated-partial | 12,033 | (34.8) | 3,936 | (8.2) | 44,607 | (8.3) |
| Unvaccinated | 837 | (2.4) | 4,536 | (9.4) | 21,096 | (3.9) |
| Out of range | 261 | (0.8) | 24 | (0.0) | 207 | (< 0.1) |
| Total | 34,599 | 48,177 | 536,805 | |||
| Rotavirus* | N = 3,204 | N = 17,733 | N = 97,578 | |||
| Vaccinated-on time | 327 | (24.3) | 8,448 | (49.0) | 42,123 | (45.2) |
| Vaccinated-delayed | 333 | (24.7) | 1,347 | (7.8) | 11,631 | (12.5) |
| Vaccinated-partial | 120 | (8.9) | 324 | (1.9) | 1,773 | (1.9) |
| Unvaccinated | 558 | (41.4) | 7,104 | (41.2) | 37,656 | (40.4) |
| Out of range | 6 | (0.4) | 12 | (0.1) | 39 | (< 0.1) |
| Total | 1,347 | 17,238 | 93,222 | |||
*Introduced in 2014; hence total cohort only includes children born in 2014 and 2015.
†Introduced in 2008
Note: ‘Total’ = children in each cohort with an enrolment record or at least one record in the National Immunisation Register. ‘Vaccinated-on time’ = complete and timely vaccination. ‘Vaccinated-delayed’ = vaccinations given > 1 month after the scheduled date for the 6-week, and 3-, 5- and 15-month vaccinations, and > 6 months after for the 4-year vaccinations. In a multi-dose series, it was considered delayed if any one dose was given late. ‘Vaccinated-partial’ = less than the scheduled doses were received based on the child’s age. ‘Unvaccinated’ = no record on the NIR for the particular vaccine or actively declined vaccination. ‘Out of range’ for MMR = vaccines given before 12 months old or possibly indicates a data error (e.g., vaccine recorded as given prior to birth) for the other vaccines.
Children in Cohort B had the highest recorded age-appropriate vaccination rates compared to those in Cohorts A and C across all ethnicities, with the exception of Niuean and ‘Other’ ethnicities where those in Cohort C had higher rates (Table 2). Within each cohort, there were differences in age-appropriate vaccination rates by ethnicity, grouped by Statistics NZ Level 1 categories. NZ Māori (13.6%) had the highest age-appropriate vaccination rates in Cohort A, while those of Asian ethnicity (62.8%) in Cohort B and those of Asian (53.2%) and Other ethnicity (53.5%) in Cohort C had the highest rates. Children from many Pacific Island ethnicities had lower reported coverage than other ethnicities. Within Cohort A, although numbers are low, children of Pacific Realm Countries (i.e., Tokelau, Niue, Cook Islands) had higher age-appropriate vaccination rates compared to other Pacific Island ethnicities. Across cohorts, those of NZ Māori ethnicity had the highest rates of not age-appropriately vaccinated and those of Other ethnicity had the highest rates of Unknown vaccination status, meaning that they did not have a record in the NIR.
Table 2.
Recorded complete and timely vaccination status for selected vaccines for Cohorts A, B and C by ethnicity, grouped by Statistics NZ categories, from January 1, 2006 to December 31, 2015, New Zealand.
| Cohort A |
Cohort B |
Cohort C |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total number in cohort | N = 75,375 | N = 50,136 | N = 567,408 | |||||||||||||||
| Ethnicity | Yes | (%) | No | (%) | Unkn | (%) | Yes | (%) | No | (%) | Unkn | (%) | Yes | (%) | No | (%) | Unkn | (%) |
| European | 2,877 | (12.6) | 12,378 | (54.2) | 7,584 | (33.2) | 7,410 | (52.7) | 5,859 | (41.7) | 798 | (5.7) | 147,891 | (48.7) | 140,973 | (46.5) | 14,625 | (4.8) |
| European (nfd) | 1,719 | (10.6) | 8,421 | (51.7) | 6,135 | (37.7) | 4,551 | (52.1) | 3,708 | (42.4) | 483 | (5.5) | 10,935 | (45.2) | 11,700 | (48.3) | 1,575 | (6.5) |
| NZ European | 1,158 | (17.6) | 3,957 | (60.3) | 1,452 | (22.1) | 2,859 | (53.7) | 2,151 | (40.4) | 315 | (5.9) | 136,956 | (49.0) | 129,273 | (46.3) | 13,047 | (4.7) |
| NZ Māori | 504 | (13.6) | 2,280 | (61.3) | 933 | (25.1) | 390 | (41.0) | 516 | (54.3) | 45 | (4.7) | 49,491 | (35.4) | 85,116 | (60.9) | 5,139 | (3.7) |
| Pacific Island | 432 | (6.2) | 4,176 | (60.0) | 2,355 | (33.8) | 3,399 | (53.4) | 2,865 | (45.0) | 99 | (1.6) | 23,694 | (40.1) | 34,119 | (57.7) | 1,314 | (2.2) |
| Pacific Island (nfd) | 12 | (10.0) | 60 | (50.0) | 48 | (40.0) | 42 | (48.3) | 45 | (50.0) | S | S | 228 | (36.5) | 375 | (60.1) | 21 | (3.4) |
| Samoan | 186 | (5.8) | 1,944 | (60.8) | 1,065 | (33.3) | 1,281 | (47.1) | 1,401 | (51.5) | 39 | (1.4) | 9,942 | (39.5) | 14,637 | (58.1) | 600 | (2.4) |
| Cook Island Māori | 60 | (9.8) | 384 | (62.4) | 171 | (27.8) | 102 | (49.3) | 96 | (46.4) | 9 | (4.3) | 3,669 | (38.4) | 5,652 | (59.1) | 237 | (2.5) |
| Tongan | 78 | (5.9) | 792 | (60.1) | 447 | (33.9) | 804 | (57.4) | 576 | (41.1) | 21 | (1.5) | 5,529 | (39.8) | 8,124 | (58.5) | 234 | (1.7) |
| Niuean | 9 | (10.7) | 48 | (57.1) | 27 | (32.1) | 9 | (21.4) | 27 | (64.3) | 6 | (14.3) | 1,563 | (42.0) | 2,088 | (56.1) | 72 | (1.9) |
| Tokelauan | 9 | (11.5) | 42 | (53.8) | 27 | (34.6) | 18 | (46.2) | S | S | S | S | 531 | (40.9) | 747 | (57.5) | 21 | (1.6) |
| Fijian | 60 | (5.1) | 717 | (60.4) | 411 | (34.6) | 927 | (63.1) | 522 | (35.5) | 21 | (1.4) | 1,491 | (48.2) | 1,545 | (49.9) | 60 | (1.9) |
| Other Pacific Island | 15 | (4.2) | 189 | (52.5) | 156 | (43.3) | 216 | (54.1) | S | S | S | S | 741 | (42.2) | 948 | (53.9) | 69 | (3.9) |
| Asian | 1,413 | (9.9) | 8,484 | (59.2) | 4,425 | (30.9) | 15,258 | (62.8) | 8,793 | (36.2) | 240 | (1.0) | 25,254 | (53.2) | 21,375 | (45.0) | 849 | (1.8) |
| Asian (nfd) | 69 | (5.9) | 603 | (51.5) | 498 | (42.6) | 663 | (63.1) | 366 | (34.9) | 21 | (2.0) | 888 | (48.8) | 885 | (48.6) | 48 | (2.6) |
| Southeast Asian | 150 | (6.9) | 1,350 | (62.4) | 663 | (30.7) | 2,184 | (64.4) | 1,158 | (34.1) | 51 | (1.5) | 2,340 | (54.6) | 1,857 | (43.3) | 87 | (2.0) |
| Chinese | 369 | (11.9) | 1,920 | (61.8) | 816 | (26.3) | 3,456 | (61.6) | 2,109 | (37.6) | 42 | (0.7) | 10,893 | (56.5) | 8,067 | (41.9) | 306 | (1.6) |
| Indian | 453 | (10.8) | 2,526 | (60.1) | 1,224 | (29.1) | 6,135 | (62.8) | 3,570 | (36.5) | 63 | (0.6) | 6,732 | (50.0) | 6,525 | (48.4) | 216 | (1.6) |
| Other Asian | 372 | (10.1) | 2,088 | (56.6) | 1,230 | (33.3) | 2,820 | (63.0) | 1,590 | (35.5) | 63 | (1.4) | 4,401 | (51.0) | 4,041 | (46.8) | 189 | (2.2) |
| MELAA | 237 | (9.9) | 1,416 | (59.0) | 747 | (31.1) | 2,025 | (58.5) | 1,368 | (39.5) | 66 | (1.9) | 2,844 | (42.6) | 3,591 | (53.8) | 237 | (3.6) |
| Middle Eastern | 87 | (10.9) | 480 | (59.9) | 234 | (29.2) | 681 | (57.2) | 489 | (41.1) | 21 | (1.8) | 1,272 | (44.2) | 1,500 | (52.1) | 105 | (3.6) |
| Latin American/Hispanic | 75 | (12.6) | 339 | (57.1) | 180 | (30.3) | 639 | (58.5) | 423 | (38.7) | 30 | (2.7) | 612 | (46.7) | 624 | (47.6) | 75 | (5.7) |
| African | 75 | (7.5) | 597 | (59.4) | 333 | (33.1) | 705 | (59.9) | 456 | (38.8) | 15 | (1.3) | 960 | (38.6) | 1,467 | (59.1) | 57 | (2.3) |
| Other | 12 | (6.5) | 108 | (58.1) | 66 | (35.5) | 69 | (48.9) | 63 | (44.7) | 9 | (6.4) | 162 | (53.5) | 120 | (39.6) | 21 | (6.9) |
| Missing | 27 | (0.1) | 252 | (1.0) | 24,291 | (98.9) | 90 | (26.8) | 78 | (23.2) | 168 | (50.0) | 846 | (23.7) | 1,332 | (37.2) | 1,398 | (39.1) |
| Total | 5,502 | (7.3) | 29,097 | (38.8) | 40,404 | (53.9) | 28,641 | (57.7) | 19,536 | (39.4) | 1,425 | (2.9) | 250,176 | (44.6) | 286,629 | (51.1) | 23,583 | (4.2) |
Note: ‘Yes’ = complete and timely vaccination of MMR, PCV and DTP vaccines. Rotavirus vaccine was not included; ‘No’ = not complete and timely vaccination, includes children who are partially vaccinated, received delayed vaccinations or declined vaccinations; ‘Unkn’ = children without a record on the NIR; Ethnicity is self-defined as per the National Health Index and grouped according to ethnic categories as per Statistics NZ (italicised); S = values suppressed (fewer than 6) to protect privacy; nfd = not further defined
Among migrant children, those who were NZ-born had higher recorded age-appropriate vaccination rates than those who were foreign-born across all visa groups (Table 3). The highest rates of the foreign-born migrant children not age-appropriately vaccinated were noted among those on refugee, Pacific and humanitarian visa schemes, indicating that many children were either partially vaccinated or received late vaccinations. Within Cohort A, children generally had high Unknown vaccination rates, most notably for those children who accompanied parents on work, student and visitor visas for whom Unknown rates ranged from 55.2% to 69.7%, while only 10.1% of quota refugees had an Unknown vaccination status.
Table 3.
Recorded complete and timely vaccination status for selected vaccines of Cohorts A and B by visa group from January 1, 2006 to December 31, 2015, New Zealand.
| Cohort A (child’s visa) |
Cohort B (mother’s visa) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total number in cohort |
N = 75,375 |
N = 50,136 |
||||||||||
| Visa group | Yes | (%) | No | (%) | Unknown | (%) | Yes | (%) | No | (%) | Unknown | (%) |
| Refugee (quota)1 | 9 | (2.8) | 285 | (87.2) | 33 | (10.1) | 135 | (62.5) | 81 | (37.5) | - | - |
| Pacific | 63 | (3.8) | 1,098 | (65.9) | 504 | (30.3) | 480 | (51.6) | 441 | (47.4) | 9 | (1.0) |
| International (non-Pacific)/Refugee (non-quota) | 33 | (6.5) | 387 | (75.9) | 90 | (17.6) | 456 | (67.3) | 222 | (32.7) | S | S |
| Convention refugee & Humanitarian2 | 27 | (6.6) | 312 | (75.9) | 72 | (17.5) | - | - | - | - | - | - |
| Humanitarian | - | - | - | - | - | - | 36 | (47.8) | 33 | (52.2) | S | S |
| Convention refugee1 | - | - | - | - | - | - | 348 | (69.5) | 153 | (30.5) | - | - |
| Refugee family | 6 | (6.1) | 75 | (75.8) | 18 | (18.2) | 72 | (33.3) | 36 | (66.7) | S | S |
| Residence | 381 | (7.4) | 2,658 | (51.7) | 2,100 | (40.9) | 2,961 | (59.2) | 1,902 | (38.0) | 138 | (2.8) |
| Family | 207 | (11.6) | 1,104 | (62.1) | 468 | (26.3) | 3,099 | (61.1) | 1,845 | (36.4) | 129 | (2.5) |
| Adopted child3 | S | S | S | S | 105 | (67.3) | - | - | - | - | - | - |
| Child of citizen or resident | 258 | (15.7) | 909 | (55.4) | 474 | (28.9) | 24 | (53.3) | S | S | S | S |
| Work4 | - | - | - | - | - | - | 9,507 | (58.8) | 6,252 | (38.6) | 417 | (2.6) |
| Work & student | 66 | (2.6) | 813 | (32.3) | 1,638 | (65.1) | 120 | (54.8) | S | S | S | S |
| Work & visitor | 969 | (5.8) | 6,519 | (39.0) | 9,243 | (55.2) | 348 | (54.5) | 270 | (42.3) | 21 | (3.3) |
| Visitor | 267 | (3.1) | 2,316 | (27.1) | 5,952 | (69.7) | 2,688 | (57.0) | 1,893 | (40.2) | 132 | (2.8) |
| Overstay | 18 | (4.0) | 165 | (36.9) | 264 | (59.1) | 486 | (54.7) | 375 | (42.2) | 27 | (3.0) |
| Medical treatment | S | S | 12 | (14.3) | 72 | (85.7) | 6 | (66.7) | S | S | S | S |
| Seasonal work4 | - | - | - | - | - | - | 42 | (60.9) | S | S | S | S |
| Working holiday4 | - | - | - | - | - | - | 585 | (51.7) | 477 | (42.2) | 69 | (6.1) |
| Student parent4 | - | - | - | - | - | - | 1,077 | (54.1) | 870 | (43.7) | 45 | (2.3) |
| Other | 63 | (6.0) | 432 | (41.3) | 552 | (52.7) | 4,959 | (62.7) | 2,751 | (34.8) | 195 | (2.5) |
| Visa not required or missing5 | 3,153 | (9.2) | 12,330 | (35.9) | 18,897 | (55.0) | 1,662 | (42.5) | 2,016 | (51.6) | 231 | (5.9) |
| Total | 5,502 | (7.3) | 29,100 | (38.8) | 40,401 | (53.9) | 28,641 | (57.7) | 19,536 | (39.4) | 1,425 | (2.9) |
Note: ‘Yes’ = complete and timely vaccination of MMR, PCV and DTP vaccines. Rotavirus vaccine was not included; ‘No’ = not complete and timely vaccination, includes children who are partially vaccinated, received delayed vaccinations or declined vaccinations; ‘Unkn’ = children without a record on the NIR; Total N by International (non-Pacific)/Refugee (non-quota) grouping is italicised; S = values suppressed (fewer than 6) to protect privacy.
1 No and Unknown were aggregated for Cohort B
2Aggregated because of low numbers for Cohort A
3 Visa category not applicable for Cohort B
4 Visa category not applicable for Cohort A
5 The majority of this group included migrants from countries where a visa for New Zealand is not needed (e.g., Australia)
Discussion
To our knowledge, this is the first national study to explore immunisation inequities between migrant and non-migrant children in NZ. Our study revealed that all three cohorts of children had suboptimal age-appropriate vaccination rates for all of the vaccines of interest. It is important to note that our definition of vaccine timeliness was stricter than that used for national reporting, which is the percentage of 8-month olds who are fully immunised over a 3-month reporting period. As such, our reported vaccination rates were lower than the national reported averages.17 In our study, foreign-born children had lower recorded age-appropriate vaccination rates for all of the included vaccines compared with NZ-born migrant and non-migrant children. This finding supports childhood vaccination coverage disparities observed in foreign-born migrant children in other countries, including the United States,18,19 Europe,20,21 and Australia13. These studies indicate that nativity has a strong effect on recorded immunisation coverage with foreign-born status being a risk factor for being under-immunised.19
While the majority of NZ-born children had a record in the NIR, less than half of the foreign-born children did. For the latter group, this improved with time spent in NZ; however, even after being in NZ for 2 or more years, still only 60% had a NIR record. We were unable to establish the vaccination status of those children with no NIR record. Newly arrived migrant and refugee children are advised to register with a general practice for their documented vaccination status (if available) to be assessed and recorded in the NIR, and to be given appropriate immunisation catch-up programmes.16 Thus, our results likely reflect issues of limited engagement with immunisation services and/or challenges with recording vaccinations given prior to arrival in NZ on the NIR.
The finding that foreign-born migrant children were under-immunised relative to NZ-born children may be attributed to a number of factors. First, the finding may be indicative of suboptimal provision of vaccines in their countries of origin and/or interruptions to routine vaccinations while migrating.11 Second, children vaccinated according to the schedule of their country of origin may not be classified as age-appropriately vaccinated according to the NZ schedule, if the schedules do not align. Furthermore, challenges with translating different immunisation schedules may lead to inaccurate recording in the NIR. Thus, the reported vaccination rates among foreign-born children may be an underestimation of the ‘true’ coverage rate. Third, this finding may reflect gaps in immunisation service delivery and barriers to accessing immunisations among migrant children post-arrival. A previous study reported that parental ethnicity, culture, and immigration status can influence the vaccination status of their children.19 Another study found that missed vaccination opportunities post-arrival are likely to contribute to low vaccination rates among migrant children.13
Although variations were observed, generally, children of Asian ethnicity in our study had the highest rates of age-appropriate vaccination rates among NZ-born migrant and non-migrant children. Across all cohorts, children of NZ Māori and Pacific Island ethnicities had lower rates of age-appropriate vaccination, generally. Immunisation inequities between ethnicities have been previously noted and attributed to differing vaccination practices and experiences. For instance, pro-immunisation attitudes and perceived easy access to immunisations have been reported among Asian peoples.22 Immunisation rates for Pacific Peoples have been steadily improving in NZ due to numerous targeted strategies;23 however, our study highlights that children of Pacific ethnicity, particularly those who are foreign-born, appear more at risk of being under-immunised than other groups.
There was substantial variation in vaccination rates among children with migrant backgrounds, depending on their visa category. Generally, high numbers of children accompanied by parents on work, student and/or visitor visas had no record in the NIR. Parents of these children may not have not engaged with immunisation services due to a low awareness of the NZ health services available for children. The variation among children with refugee backgrounds likely reflects the differential engagement with immunisation services based on the scheme within which they were accepted into NZ. For instance, the Unknown vaccination rates for quota refugees were slightly lower than those of refugees entering on other (i.e., family reunification, asylum seekers, etc.) schemes. Only quota refugee children spend their first 6 weeks in NZ at the Mangere Refugee Resettlement Centre completing an orientation and comprehensive health screening programme, which includes the recording of their overseas vaccinations in the NIR and being offered appropriate catch-up immunisation schedules.9,14,24
Immunisation policy and practice implications
This study has important implications for immunisation policy and practice in NZ. The NIR is the key tool used to identify and respond to the underimmunised, so it is important that NIR data are accurate. Importantly, the proportion of foreign-born children who did not have a record in the NIR signals a need for prompt enrolment of foreign-born children in the NIR and accurate entry of vaccinations administered overseas for migrant children. Recorded immunisation rates among foreign-born migrant children by vaccine, ethnicity and visa category were consistently low and this finding warrants concern. It is unclear if this finding reflects inaccurate recording of vaccinations and/or issues with access and uptake of immunisations among migrant children. While vaccination interventions aimed at the general population, such as reminder/recall messages, parent-centred information, and immunisation policies have been shown to be effective to improve rates,25 further targeted strategies for migrant children are also needed. For instance, interventions that reduce barriers to accessing immunisation services and facilitate catch-up immunisations post-arrival, along with improving the availability of culturally- and linguistically-appropriate immunisation services may be helpful. Moreover, efforts should focus on improving awareness among healthcare professionals about the specific needs of migrant patients given the important role that they play in terms of influencing the vaccine decision-making of migrant mothers.26 Further support may be needed to assist healthcare professionals with translating international vaccination schedules across to the NIR and planning appropriate catch-up immunisation schedules.
Study strengths and limitations
The employed methods were only possible due to NZ’s unique health care structure and existing data collection capabilities that support robust data linkage across various databases for a national sample of children. Despite this, there are several important limitations. Existing administrative data used for this study were originally collected for a different purpose so a number of assumptions were made. We were not able to control the variables available or the value categories within them; thus, some inaccuracies may have been introduced. Whilst we have data for most of the NZ population, there are some groups (e.g., certain nationalities or ethnicities) that have small numbers, which limits the conclusions we can make.
Certain variables of interest were selected to maintain the focus of this study; however, further analyses would be possible and that could yield helpful information. For this study, only the most recent visa held by the migrant child or his/her migrant parent was used and transition through different visa categories was not examined. Patterns of travel, transition to residency and length of time spent in NZ could be investigated further to tease out how this may impact immunisation uptake. Future work is required to understand the factors contributing to the low recorded vaccination rates reported among migrant children in our study. One area of focus could relate to the accuracy of data reported on the NIR for migrant children who may have been vaccinated overseas.
Conclusion
Foreign-born migrant children living in NZ represent a diverse range of ethnicities and backgrounds, and, overall, are reported to have lower age-appropriate vaccination rates than NZ-born children. Additional efforts are needed to improve the accuracy of immunisation data in the NIR and develop targeted campaigns to increase access and uptake of immunisation services for migrant children to reduce immunisation inequities in NZ. This study also highlights the importance of having better national surveillance and migrant-specific data related to vaccination coverage to help uncover health inequities among children living in NZ and inform immunisation policy and practice.
Materials and methods
Study design and population
This study is part of a larger retrospective cohort study that examined immunisation coverage and VPD burden among three cohorts of children in NZ from 1 January 2006 and 31 December 2015, using linked government administrative data. Cohort A (foreign-born migrants) consisted of foreign-born children aged up to 5 years who arrived in NZ prior to their fifth birthday within the study period. Cohort B (NZ-born migrants) consisted of children aged up to 5 years who were born in NZ to women who migrated to NZ during the study period. Cohort C (NZ-born non-migrants, the comparator group) consisted of all children aged up to 5 years who were born in NZ without a migration background during the study period. Exclusions were all children who stayed less than 3 months in NZ and children with logical data inconsistencies (e.g., a birth date occurring after a travel date).
Data sources and variables of interest
De-identified data were retrieved and linked from multiple sources using Statistics NZ’s Integrated Data Infrastructure (IDI). Data were collected from government administrative datasets: Ministry of Health’s National Health Index (NHI) for demographic data; Ministry of Business, Innovation and Employment and NZ Customs Journey datasets for immigration and travel data; Department of Internal Affairs for life event data; and the National Immunisation Register (NIR) for immunisation data. Data for the following variables were obtained including: date of birth, date of death, sex, ethnicity, nationality (i.e., country that issued their passport), visa type, time spent in NZ, and immunisation status for select NIS vaccines. For individuals who had multiple nationalities, the non-NZ nationality was reported if NZ was one of the nationalities. For individuals that had multiple nationalities and no NZ nationality, the earliest recorded nationality was reported. Ethnicity was self-reported by the parents, and based on that recorded in the NHI dataset (as it provides more detail) and grouped according to the six Statistics NZ Level 1 ethnicity classifications. The September 2016 refresh version of the IDI was used for all data except for the NIR data, which used the version uploaded to the IDI ‘sandpit’ in January 2017 to allow for the most complete vaccination records for the cohorts to be included.
A NHI number is assigned to all people who are born in NZ or allocated to foreign-born individuals the first time they access health and disability support services. NHI numbers enabled deterministic linkage across health-related data sources. Linking the NIR with the NHI dataset was done using the encrypted NHI index (snz_moh_uid). Data that did not have a standard identifier, such as immigration and travel data, were linked to the health datasets and life events datasets using probabilistic linking originally by Statistics NZ, who assigned an encrypted identifier that was then used in this study (snz_uid) to link the data.
The primary outcome measure was vaccination status. The NIR records the administration date of every vaccine given as per the NIS (Table 4). Four vaccines were selected for this study: measles, mumps and rubella (MMR) vaccine (2 doses), pneumococcal conjugate vaccine (PCV) (3 primary doses and a booster), pertussis-containing vaccine (3 primary doses and a booster) and the rotavirus vaccine (3 doses). Vaccination status is reported in two ways. Detailed vaccination status is reported for each vaccine or antigen group as either: vaccinated – on time (received all scheduled doses on time); vaccinated – delayed (received vaccine dose beyond 1 month after the scheduled date for the 6-week and 3-, 5- and 15-month vaccinations, and beyond 6 months after for the 4-year vaccinations); vaccinated – partial (received some of the scheduled doses based on their age); out of range (received or reported a dose given too early for the recommended age); or unvaccinated (did not have a record on the NIR for the particular vaccine or actively declined vaccination). Vaccination status is also reported according to whether or not the child was fully vaccinated on time for all of the vaccines of interest. Thus, those classified as ‘yes’ indicates age-appropriately vaccinated, ‘no’ indicates not age-appropriately vaccinated, and ‘unknown’ indicates no record on the NIR.
Table 4.
Schedule of vaccines as per the New Zealand National Immunisation Schedule during the study period from 1 January 2006 to 31 December 2015.
| Milestoneage | Rotavirus* | PCV† | DTaP-IPV-Hep B-Hib | Hib | DTaP-IPV | MMR |
|---|---|---|---|---|---|---|
| 6 weeks | Dose 1 | Dose 1 | Dose 1 | – | – | – |
| 3 months | Dose 2 | Dose 2 | Dose 2 | – | – | – |
| 5 months | Dose 3 | Dose 3 | Dose 3 | – | – | – |
| 15 months | – | Dose 4† | – | Dose 4‡ | – | Dose 1 |
| 4 years | – | – | – | – | Dose 4‡ | Dose 2 |
*Introduced in 2014
†Introduced in 2008
‡Booster dose
PCV = Pneumococcal conjugate vaccine; DTaP-IPV-Hep B-Hib = Diphtheria-tetanus-pertussis-polio-hepatitis B-Haemophilus influenzae type b; Hib = Haemophilus influenzae type b; DTaP-IPV = Diphtheria-tetanus-pertussis-polio; MMR = Measles-mumps-rubella
Statistical analysis
Selection of subsets of relevant data from the IDI, linkage of data (via the Statistics NZ identifier or the MOH identifier) and recoding of variables were done using SAS Enterprise Guide 7.1. Each cohort is described and compared using counts and percentages summarising each variable of interest, including ethnicity, nationality, visa category, longest time spent in NZ, and vaccination status. In order to meet the privacy protection requirements of Statistics New Zealand each count (both population and numbers of cases) has been randomly rounded to a base of 3.
Ethical approval to conduct this study was granted by the University of Auckland Human Participants Ethics Committee (UAHPEC, reference number: 017200).
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
Funding Statement
This work was supported by the Ministry of Business, Innovation and Employment [UOAX1512]. MBIE was provided the opportunity to review a preliminary version of this manuscript for factual accuracy but the authors are solely responsible for final content and interpretation. The authors received no financial support or other form of compensation related to the development of the manuscript.
Acknowledgments
This study was conducted in collaboration with Statistics New Zealand and within the confines of the Statistics Act 1975. We would like to thank members of The Monarch Collaboration (http://monarchcollaboration.org/) for their support of this study.
Summary Statistics New Zealand Security Statement
The presented Red Knot (Huahou) Study is a study of the immunisation coverage among migrant and refugee children in New Zealand, based on the integration of anonymised population census data from Statistics New Zealand and mortality data from the New Zealand Health Information Service. This project was approved by Statistics New Zealand as a Data Laboratory project under the Microdata Access Protocols in 1997. The datasets created by the integration process are covered by the Statistics Act 1975 and can be used for statistical purposes only. Only approved researchers who have signed Statistics New Zealand’s declaration of secrecy can access the integrated data in the Data Laboratory. For further information about confidentiality matters in regard to this study please contact Statistics New Zealand.
References
- 1.Castles S. International migration at the beginning of the 21st century. ISSJ. 2000;52(165):269–281. [Google Scholar]
- 2.Abel G, Sander N. Quantifying global international migration flows. Science. 2014;343(6178):1520–1522. doi: 10.1126/science.1248676. [DOI] [PubMed] [Google Scholar]
- 3.Beine M, Parsons C. Climatic factors as determinants of international migration. Scand J Econ. 2015;117(2):723–767. doi: 10.1111/sjoe.12098. [DOI] [Google Scholar]
- 4.Perruchoud R, Redpath-Cross J, International Organization for Migration (IOM) . Glossary on migration. Geneva, Switzerland: International Organization for Migration; 2011. [Google Scholar]
- 5.United Nations High Commissioner for Refugees (UNHCR) The 1951 Convention relating to the status of refugees and its 1967 protocol. Geneva, Switzerland: UN High Commissioner for Refugees; 2011. [Google Scholar]
- 6.Merwood P. Labour market outcomes of recent migrants to New Zealand. Wellington, New Zealand: Ministry of Business, Innovation and Employment; 2013. [Google Scholar]
- 7.Statistics New Zealand (2016). International Travel and Migration: 2016 July Available from: http://www.stats.govt.nz/browse_for_stats/population/Migration/IntTravelAndMigration_HOTPJul16.aspx.
- 8.Immigration New Zealand (2017). New Zealand Refugee Quota Programme 2017. Available from: https://www.immigration.govt.nz/about-us/what-we-do/our-strategies-and-projects/supporting-refugees-and-asylum-seekers/refugee-and-protection-unit/new-zealand-refugee-quota-programme.
- 9.McLeod A, Reeve M. The health status of quota refugees screened by New Zealand’s Auckland public health service between 1995 and 2000. NZMJ. 2005;118(1224):U1702. [PubMed] [Google Scholar]
- 10.Zwi K, Raman S, Burgner D, Faniran S, Voss L, Blick D, Osborn M, Borg C, Smith M. Royal Australasian College of Physicians. Towards Better Health for Refugee Children and Young People in Australia and New Zealand: the Royal Australasian College of Physicians Perspective. JPCH.. 2007;43(7–8):522–526. [DOI] [PubMed] [Google Scholar]
- 11.Lam E, Diaz M, Maina AG, Brennan M. Displaced populations due to humanitarian emergencies and its impact on global eradication and elimination of vaccine-preventable diseases. Confl Health. 2015;10(1):27. doi: 10.1186/s13031-016-0094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams GA, Bacci S, Shadwick R, Tillman T, Rechel B, Noori T, Suk JE, Odone A, Ingleby JD, Mladovsky P, et al. Measles among migrants in the European Union and the European Economic Area. Scand J Public Health. 2015;44(1):6–13. doi: 10.1177/1403494815610182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paxton GA, Rice J, Davie G, Carapetis JR, Skull SA. East African immigrant children in Australia have poor immunisation coverage. JPCH. 2011;47(12):888–892. [DOI] [PubMed] [Google Scholar]
- 14.Rungan S, Reeve AM, Reed PW, Voss L. Health needs of refugee children younger than 5 years arriving in New Zealand. Pediatr Infect Dis J. 2013;32(12):432–436. doi: 10.1097/INF.0b013e3182a11526. [DOI] [PubMed] [Google Scholar]
- 15.Morris MD, Popper ST, Rodwell TC, Brodine SK, Brouwer KC. Healthcare barriers of refugees post-resettlement. J Community Health. 2009;34(6):529–538. doi: 10.1007/s10900-009-9175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of Health Immunisation Handbook 2017. Wellington, New Zealand: Ministry of Health; 2017. [Google Scholar]
- 17.Ministry of Health (2018). National and DHB immunisation data. Available from: https://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/immunisation-coverage/national-and-dhb-immunisation-data.
- 18.Strine TW, Barker LE, Mokdad AH, Luman ET, Sutter RW, Chu SY. Vaccination coverage of foreign-born children 19 to 35 months of age: findings from the National Immunization Survey, 1999-2000. Pediatrics. 2002;110(2 Pt 1):e15. doi: 10.1542/peds.110.2.e15. [DOI] [PubMed] [Google Scholar]
- 19.Varan AK, Rodriguez-Lainz A, Hill HA, Elam-Evans LD, Yankey D, Li Q. Vaccination coverage disparities between foreign-born and U.S.-born children aged 19–35 months, United States, 2010–2012. J Immigr Minor Health. 2017;19(4):779–789. doi: 10.1007/s10903-016-0465-4. [DOI] [PubMed] [Google Scholar]
- 20.Poethko-Müller C, Ellert U, Kuhnert R, Neuhauser H, Schlaud M, Schenk L. Vaccination coverage against measles in German-born and foreign-born children and identification of unvaccinated subgroups in Germany. Vaccine. 2009;27(19):2563–2569. doi: 10.1016/j.vaccine.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Chiaradia G, Gualano MR, Di Thiene D, Galli L, Glacchino R, Gattinara GC, Veneruso G, Ricciardi W, La Torre G. Health status of immigrant children: an epidemiological survey among Italian paediatricians. Italian Journal of Public Health. 2011;8(3):268–274. [Google Scholar]
- 22.Pal M, Goodyear-Smith F, Exeter D. Factors contributing to high immunisation coverage among New Zealand Asians. J Prim Health Care. 2014;6(4):304–311. [PubMed] [Google Scholar]
- 23.Paterson J, Schulter P, Percival T, Carter S. Immunisation of a cohort Pacific children living in New Zealand over the first 2 years of life. Vaccine. 2006;24(22):4883–4889. doi: 10.1016/j.vaccine.2006.02.050. [DOI] [PubMed] [Google Scholar]
- 24.Saunders H. Meeting the health needs of newly arrived refugees. NZMJ. 2015;128(1423):89–90. [PubMed] [Google Scholar]
- 25.Briss PA, Rodewald LE, Hinman AR, Shefer AM, Strikas RA, Bernier RR, Carande-Kulis VG, Yusuf HR, Ndiaye SM, Williams SM. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med. 2000;18(1S):97–140. doi: 10.1016/S0749-3797(99)00118-X. [DOI] [PubMed] [Google Scholar]
- 26.Kowal SP, Jardine CG, Bubela TM. “If they tell me to get it, I’ll get it . If They Don’t….”: Immunization Decision-Making Processes of Immigrant Mothers. Can J Public Health. 2015;106(4):e230–235. [DOI] [PMC free article] [PubMed] [Google Scholar]


