ABSTRACT
Background: Vaccination of healthcare providers (HCPs) against seasonal influenza has been consistently recommended worldwide. Despite that, healthcare providers (HCPs) globally and in other Middle Eastern countries continue to have a low rate of influenza vaccination due to various reasons. No data are available from our country, United Arab Emirates.
Objectives: To identify the percentage of vaccinated HCPs, identify the most common reason for receiving the vaccine or not and to identify the level of HCPs knowledge towards the influenza vaccine itself.
Methods: Using a cross-sectional study design, anonymous 18-item self-administered questionnaires were distributed among healthcare providers in the 11 primary healthcare centers of Dubai Health Authority over a period of 5 months.
Results: Of the 431 participants who completed the questionnaires, 53.4% reported getting vaccinated. The difference in the vaccine uptake between the different professional categories was significant [P value < .000].The most common reason reported by HCPs for getting the vaccine was to protect themselves (94.8%). Of the 46.6% who did not accept the vaccine, the most common reason for not being vaccinated was their belief of not being at high risk to contract influenza (39.8%). Despite fairly good knowledge (63.3%), healthcare providers continue to have their reservations with regards to the yearly influenza vaccination.
Conclusion: Although our HCPs attitude towards vaccine uptake, knowledge and practice were positive; the misconception about the vaccine remains the main reason for not being vaccinated as per our study findings. Overall, the study results raise hope of prospective increase in vaccination through educational and technical interventions and by increasing physician involvement. One suggested method would be to apply mandatory vaccination policies since voluntary vaccinations have shown lesser than satisfactory results and to be integrated in the online staff file system to be able to verify the uptake, in addition to provide easily accessible vaccine centers, during the season in order to facilitate tracking and verification of the vaccination status & to encourage staff compliance.
Keywords: vaccination, healthcare providers, seasonal influenza, knowledge, attitude and practice, United Arab Emirates, Dubai
Introduction
Seasonal influenza is the most common cause of acute respiratory illness worldwide. Influenza infection is a highly transmissible infection of the respiratory system. It can lead to wide range of mild to severe illness. Serious outcomes of flu infection can even result in death. Since the virus is known for its high rates of mutation, compromising the ability of the immune system to protect against new variants. Hence, there are new vaccines that are being produced every year to cover the new strains to the existing vaccines. Vaccinating healthcare providers against influenza is an approved infection control method. The Advisory Committee On Immunization Practice (ACIP) recommends vaccination of healthcare providers because they care for persons at high risk for influenza-related complications.1 Influenza vaccination of healthcare providers reduces illness and mortality among patients and is associated with lower staff absenteeism during influenza season.2 It also provides protection to the healthcare workers who may be more likely to develop influenza infection because of the regular close contact with infected patients. In addition, perception of and attitudes to influenza vaccination by HCPs may influence their recommendations to patients and may be a marker for the evaluation of occupational risks. Healthcare providers appear to have many of the same misconceptions about influenza and influenza vaccine as patients. A high incidence of influenza infection is being reported in the United Arab Emirates as summer transitions to winter.3 Despite that, in our region few studies have addressed similar issues and the results showed low percentage of HCPs being vaccinated against influenza vaccine and inadequate knowledge towards influenza infection.4–6 Addressing the situation in United Arab Emirates, to date, there have been no clear, published guidelines for HCPs influenza vaccination in healthcare setting. In addition, there is a lack of any published studies that shows HCPs attitude, practice and knowledge towards the influenza vaccination. Therefore, this study conducted in Dubai Health Authority, a governmental sector in Duba, aimed to investigate the knowledge, practice and attitude of HCPs towards influenza vaccination, estimate the percentage of vaccinated HCPs, identify the most common reason for receiving the vaccine or not and to identify the level of HCPs knowledge towards the influenza vaccine itself.
Methods
Study design
A cross sectional study design was used to conduct the study, as it was important for us to assess the knowledge and contribution of our existing staff at Dubai Health Authority’s 11 primary health centers in promoting and utilizing the influenza vaccine amongst themselves and within the society.
Study tool
An 18-item self-administered questionnaire was distributed manually by all research members among our target population.
First a pilot study was performed on 30 health care providers to validate our questionnaire as it was adopted from the existing literature tackling the same research question in other regions 7
The questionnaire included 3 sections:
A demographic section detailing the educational level of the participant and their position in the PHC.
Another section included a few questions about the participant’s personal experience with the vaccine.
The remaining sections of the questionnaire assessed the participant’s knowledge of the latest guidelines and recommendations with regards to influenza vaccine, practices and the highly recommended recipients of it.
Our expected response rate was 70%, allowing a 30% drop off rate, taking into account the unavailability of all staff due to absences and annual leaves; and the possibility of incomplete submitted forms. 7
Study sample
Our target population consisted of 700 individuals. We calculated our sample size using standard online tools through the following formula (n = (Z2 x P(1 x P))/e2) where: Z = value from standard normal distribution corresponding to desired confidence level (Z = 1.96 for 95% CI), P is expected true proportion, and e is desired precision (half desired CI width) with 95% confidence, the suggested sample was 254 however we opted to double that number to increase the strength of our study therefore a sample size of 500 was used 8 including family medicine physicians, residents, nurses, and dentists in all primary healthcare centers under DHA, with the exception of rural areas (Hatta and Al-Lusaili) for logistic purposes.
The inclusion criterion set out for the study was:
All primary healthcare providers in the listed primary healthcare centers under DHA.
While the exclusion criteria for participation included:
Primary healthcare providers with contraindications to influenza vaccinations, such as severe allergic reactions to the contents of influenza vaccination.
Primary healthcare providers in rural PHC (Hatta and Al-Lusaili health centers due to logistic reasons as they are not accessible to us)
Over a period of 5 months, between May and September 2017, we succeeded in collecting 431 completed questionnaires from our calculated sample size.
Our study did not involve any tissue/fluid sample collection. There were no incentives or rewards provided and there was no risk imposed on the participants. All questionnaires were submitted anonymously. Participation was voluntary and acceptance in the participation in the study with a returned and completed questionnaire was taken as consent. All healthcare providers who had not completed the questionnaire in the given time period were considered non-respondents. Ethical approval was obtained from the Dubai Scientific Research Ethics Committee.
Study analysis
Upon completion, all the questionnaires were numbered and their data were coded and entered into an excel spreadsheet. An SPSS program version 23was then used for analysis and to compute our results. A descriptive analysis was generated using frequencies, and cross tabulation. Chi square test was also used where appropriate. Our standard was set at 95% with p value of < 0.05 indicating statistical significance of the results.
Results
Of the 431 HCPs that submitted completed questionnaires as shown in Table 1; 53.4% of them had received the vaccine, while 46.6% did not. Almost 40% of those vaccinated, received the vaccine in the month October 2015. The primary reasons given by the respondents for being vaccinated were to protect themselves (94.8%) and/or their patients (62.6%) from illness. Other reasons chosen included protecting household contacts (53.5%), to comply with public health recommendations (45.2%), to comply with DHA recommendations (43.5%), and lastly, because the season was expected to be severe (29.1%) as shown in Figure 1.
Table 1.
Demographics and characteristics of our respondents.
| Characteristics | Total number (n = 431) | Percentage % |
|---|---|---|
| Gender | ||
| female | 367 | 85.2% |
| Male | 64 | 14.8% |
| Specialty | ||
| Medical | 197 | 45.7% |
| nursing | 156 | 36.2% |
| Dental | 78 | 18.1% |
| Co-morbidities | ||
| Diabetes mellitus | 43 | 10% |
| Bronchial asthma | 33 | 7.7% |
| Pneumonia | 1 | 0.2% |
| Obesity | 50 | 11.6% |
| CVD | 11 | 2.6% |
Table 1 shows the demographics and characteristics of the total number of health care providers who responded to our questionnaire
Figure 1.
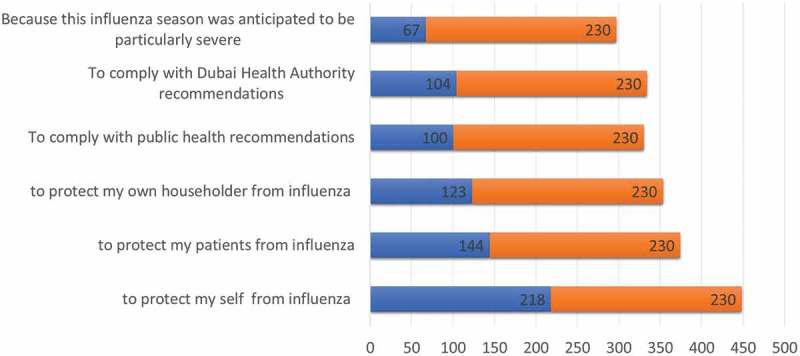
Reasons for accepting the influenza vaccine: this figure demonstrates the reasons for accepting the influenza vaccine as cited by respondents in absolute numbers.
On the other hand, 46.6% of the respondents had never received the vaccine; the most common reason cited for not taking the vaccine was their belief of not being at high risk to contract influenza (39.8%). While the second most frequently cited reason was the lack of time to take the vaccine (28.9%) as shown in Figure 2.
Figure 2.

Reasons for not receiving the influenza vaccine: this figure demonstrates the reasons for not accepting the influenza vaccine as cited by respondents in percentages.
Moreover, out of the total number who received the vaccine, 46% of them were physicians, 42% were nurses, and 12% were from the dental department. The difference in the vaccine uptake between the different professional categories was significant [P value < .000]. The majority of the vaccinated group (85.1%) received the vaccine from the governmental sector, which is also their workplace. In addition, 43.9% of participants who have received the vaccine were having co-morbidities. Those with diabetes, bronchial asthma and obesity had increase acceptance of influenza vaccine which was significant (P < .001). 25.2% of respondents who received the vaccine stated that they experienced adverse effects with it; most common of which, was flu-like illness (58.6%). The mean duration of symptoms experienced following influenza vaccine was 2–3 days (65.5%).
Out of the total sample, 55% HCPs declared they intend to receive the influenza vaccine during the next season out of whom 24.9% had never received it before.
Upon assessing the general knowledge of influenza infection and vaccine; as shown in Figure 3; data showed that (70.5%) were aware of CDC recommendations to use injectable influenza vaccines for HCP’s immunization.
Figure 3.

HCPs knowledge regarding the influenza vaccine: this figure demonstrates the results regarding some of the knowledge components that were asked in the survey about influenza vaccine. The first one shows the response of the recommended type of vaccine for healthcare workders. The middle part shows the response of the efficacy of the vaccine. While the last part shows the response regarding the annual recommendation of influenza vaccine for HCPS.
51.3% of the HCPs were aware that the vaccine protects against specific influenza strains 70–90% of the time only.
Upon scoring the knowledge questions in our questionnaires, the knowledge level was categorized into 3 groups based on the number of correctly answered questions. Those answering less than 8 questions were identified as having poor knowledge, while those answering between 8–10 questions as average knowledge, and those answering more than 11 questions were identified as having good knowledge.
65.3% of those with good knowledge accepted the vaccine, which was the highest percentage of uptake in comparison with knowledge level. As those with poorer levels of knowledge were less likely to accept the vaccine. This was a statistically significant result (0.017).
Moreover, 85.7% of those with good knowledge recommended the influenza vaccine to their patients (< 0.000).
Although 70.3%of the participants were aware of the recommendations for HCPs to be immunized annually against influenza; 65.1% stated that they believe that one of the reasons for this recommendation is that HCPs have an increased risk of acquiring influenza, and only 56.1% believed a patient can acquire influenza from infected HCPs, while 50% believed HCPs themselves can serve as a vector to spread influenza among hospitalized patients.
The percentage of correct responses in regards to the most common side effects of influenza vaccination were; Fever 71.2%, Soreness at the injection site 42.2%, Headache 25.1% and Muscle aches 42.2%. The Advisory Committee on immunization Practices (ACIP) strongly recommends annual influenza immunization for specific high-risk groups, however our data reflected varying level of knowledge with regards to the specific categories as shown in Figure 4 with healthcare group category being the most known category for recommended immunization(65.4%), followed by resident of nursing home (63.1%) and household contacts of individual at high risk (63.6%).
Figure 4.
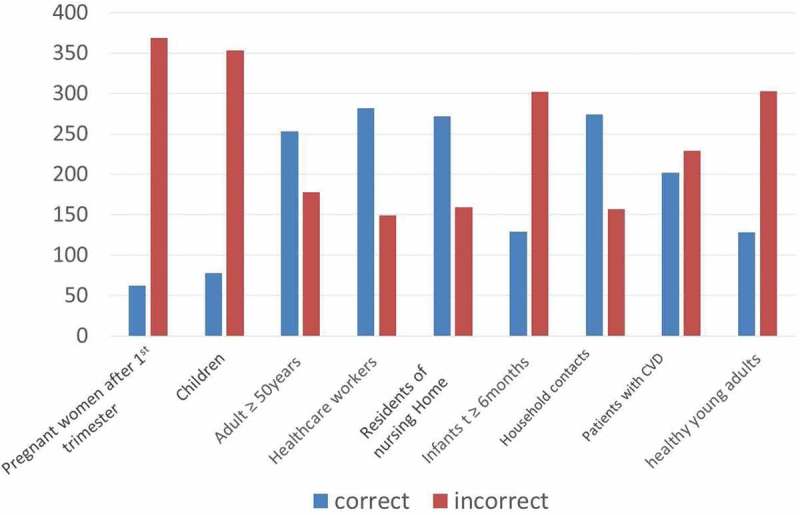
ACIP recommendations for immunization categories: This figure demonstrates the responses of the HCWs regarding the ACIP recommendation for immunization categories.
Overall, 73.9% of the healthcare providers who received the vaccine were also recommending it to their patients, while 64.7% of them were recommending to their families and 50% to their friends as well.
Discussion
This is the first cross-sectional study among healthcare providers in Dubai, United Arab Emirates addressing their knowledge, attitude and practice towards seasonal influenza vaccine.
Although the ideal vaccination rate among healthcare providers is 100%, different studies have suggested that vaccination rate of 80% or more of healthcare providers are considered sufficient to reduce transmission and provide herd immunity in a safe level within healthcare facilities.9
In our study, the vaccine coverage among healthcare providers (53.4%) was similar to previously reported rates in other studies such as in Spain 50.7% coverage,10 and in Austria 52% coverage.11
43.9% of participants who have received the vaccine were having co-morbidities. Those with diabetes, bronchial asthma and obesity had increased acceptance of influenza vaccine (< 0.001), which falls in lines with their respective disease management strategies. However this finding was to the contrary to a study done among primary health care workers where immunization rates were not higher among staff with chronic disease.12
Moreover, out of the total number who received the vaccine, 46% of them were physicians, 42% were nurses, and 12% were from the dental department.
The difference in the vaccine uptake between the different professional categories was significant [P value < .000]. Upon dividing the physions into subcategories; consultants seemed to have the highest vaccine uptake, however, the difference among the subcategories was not significant. The large number of nurses maybe be attributed to the fact they compromise a large sector in the healthcare system. However, as for the dental department, which seemed to have the lowest percentage of vaccine uptake, also demonstrated the least awareness with regards the vaccine knowledge. This seems to be a universal issue as dental vaccine coverage appears to be low in several studies.13,14 The results of other studies addressing the knowledge and attitude of the healthcare providers toward influenza vaccine conducted in two Middle Eastern countries found that the vaccination rates were 67.2% and 46.4% in Kuwait and Oman respectively.6
Furthermore, a study conducted in Saudi Arabia showed only 38% of HCPs reported getting vaccinated, and the main reasons for the low rate of immunization seemed to be related to fear of contracting illness and lack of adequate knowledge. 5
Our study found that the primary reason given by the respondents for being vaccinated was to protect themselves (94.8%) which was in concordance with another study performed in New Jersey.7 However, other studies have found that patient protection was the primary reason for their staff for being vaccinated.15
In our study data showed that 46.6% have never received influenza vaccine and attributed their reasons to the misconception that they were not at high risk of contracting the influenza and also the lack of time to get vaccinated.
A similar study done in US identified their most common reasons for not receiving the vaccine were due to the lack of time (34%) and concerns about adverse reactions (26%).15
Likewise, majority of the literatures reviewed revealed similar reasons for not receiving the vaccine.12,13,16
Our data showed variable levels of awareness of and knowledge about influenza vaccination.
The results of our study showed that 57.4% of those who received the vaccine were aware of the effectiveness of influenza vaccine.
Most of the participants had basic knowledge of the influenza vaccine ACIP recommendations (70.3%), this was in concordance with other studies done in Saudi Arabia.5
Since we have not found any studies addressing similar issues in United Arab Emirates, conducted in the primary health sector, we were unable to find any comparison to our study locally. However, studies globally and in other Middle Easern countries have found that it is universal to have a low rate of vaccinated healthcare providers as well as inadequate knowledge of aspects related to influenza vaccine and influenza infection which may influence the decision of professionals to be vaccinated.
However, one interesting study done in US showed high family physicians’ vaccination rate ranging up to 87%.15 They attributed these high acceptance levels due to strong worksite polices and free access onsite for all staff.
Our study confronted some limitations, most important of which is that the data was self-reported, making it vulnerable to recall bias and misinterpretation of some questions. Also since it was manually distributed some questionnaires may have been lost or not returned back and possibly affecting our outcome and analysis. Another key point was that we admittedly missed to verify the source of our participants’ knowledge, whether it was from medical school, on-campus campaigns, or their periodic CME lectures. This information would have been helpful to indentify the source of knowledge of our staff and provide tools enforce it.
Lastly, our two of our 3 key predictors for identifying knowledge; the gender, specialty and designation, were not statistically significant and hence we were not able to perform further regression analysis to our satisfaction.
Moreover, in our results, we observed that the dental department had the lowest coverage rate of influenza vaccination, this could be attributed to the fact the they are small in number to begin with, however we need to focus on this important category to increase their awareness of the importance of immunization against the seasonal influenza and its positive repercussions including reducing productivity loss and improving health status in general. Healthcare provider’s attitude and knowledge about influenza vaccination are important determinants of vaccine uptake.
Therefore, it is important to continue the efforts of maximizing influenza vaccine coverage and awareness among HCPs through campaigns, educational sessions and online tutorials to be held on regular basis.
Hence, ways of facilitating healthcare providers’ vaccination rate should be identified and implemented to improve outcomes. Although our HCPs intention to vaccine uptake, knowledge and practice were positive; the misconception about the vaccine remains the main reason for not being vaccinated as per our study findings. If not addressed, this may adversely impact their own health, productivity, and patient care
Furthermore, vaccine should be free of charge, readily available on site and accessible in all health centers for all the healthcare providers.
Conclusion
According to the result of our study, the vaccination rates against influenza seems similar among healthcare providers in DHA (Dubai Health Authority) compared to rates previously reported by other studies internationally and regionally. We believe that this study may serve as a basis for future interventions to increase influenza immunization among healthcare providers in our country. One of the suggested intervention methods would be the continuation of education about the vaccine for the health providers by holding mandatory annual awareness seminars and have an online assessment following the seminar. One more method would be to apply mandatory vaccination policies since voluntary vaccinations have shown lesser results than required and to be integrated in the online staff file system to be able to verify the uptake, In addition to provide easily accessible vaccine centers, during the season in order to facilitate tracking and verification of the vaccination status & to encourage staff compliance rather than it being only at the staff clinic at the main hospitals. Another one is to have a reminder service for people who have not taken their vaccination.
Funding Statement
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
References
- 1.Influenza Vaccination of Health-Care Personnel Recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) Cdc.gov; 2018. accessed May 19 https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5502a1.htm [PubMed]
- 2.Saxén H, Virtanen M.. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J. 1999;18:779–783. [DOI] [PubMed] [Google Scholar]
- 3.Suchitra Bajpai Chaudhary S. 2018. Influenza virus highly active in the UAE. GulfNews. accessed May 19 http://gulfnews.com/news/uae/health/influenza-virus-highly-active-in-the-uae-1.1917646
- 4.Alhammadi A, Khalifa M, Abdulrahman H, Almuslemani E, Alhothi A, Janahi M. Attitudes and perceptions among the pediatric health care providers toward influenza vaccination in Qatar: A cross-sectional study. Vaccine. 2015;33:3821–3828. doi: 10.1016/j.vaccine.2015.06.082. [DOI] [PubMed] [Google Scholar]
- 5.Alshammari T, AlFehaid L, AlFraih J, Aljadhey H. Health care professionals’ awareness of, knowledge about and attitude to influenza vaccination. Vaccine. 2014;32:5957–5961. doi: 10.1016/j.vaccine.2014.08.061. [DOI] [PubMed] [Google Scholar]
- 6.Garcell H, Ramirez E. Influenza immunization coverage for healthcare workers in a community hospital in Qatar (2011–2012 and 2012–2013 seasons). J Infect Public Health. 2014;7:70–72. doi: 10.1016/j.jiph.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Wodi A, Samy S, Ezeanolue E, Lamour R, Patel R, Budnick L, Dashefsky B. Influenza vaccine: immunization rates, knowledge, and attitudes of resident physicians in an Urban Teaching Hospital. Infect Control Hosp Epidemiol. 2005;26:867–873. doi: 10.1086/502510. [DOI] [PubMed] [Google Scholar]
- 8.OpenEpi Menu 2018. Openepi.com. accessed May 19 http://www.openepi.com/Menu/OE_Menu.htm.
- 9.Salgado C, Giannetta E, Hayden F, Farr B. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–928. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 10.Domínguez A, Godoy P, Castilla J, Soldevila N, Toledo D, Astray J, Mayoral J, Tamames S, García-Gutiérrez S, González-Candelas F, et al. Knowledge of and attitudes to influenza vaccination in healthy primary healthcare workers in Spain, 2011-2012. PLoS ONE. 2013;8:e81200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrison N, Brand A, Forstner C, Tobudic S, Burgmann K, Burgmann H. Knowledge, risk perception and attitudes toward vaccination among Austrian health care workers: A cross-sectional study. Hum Vaccin Immunother. 2016;12:2459–2463. doi: 10.1080/21645515.2016.1168959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abramson Z, Levi O. Influenza vaccination among primary healthcare workers. Vaccine. 2008;26:2482–2489. doi: 10.1016/j.vaccine.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Socan M, Erculj V, Lajovic J. Knowledge and attitudes on pandemic and seasonal influenza vaccination among Slovenian physicians and dentists. Eur J Public Health. 2012;23:92–97. doi: 10.1093/eurpub/cks006. [DOI] [PubMed] [Google Scholar]
- 14.Di Giuseppe G, Nobile C, Marinelli P, Angelillo I. A survey of knowledge, attitudes, and behavior of Italian dentists toward immunization. Vaccine. 2007;25:1669–1675. doi: 10.1016/j.vaccine.2006.10.056. [DOI] [PubMed] [Google Scholar]
- 15.Cowan A, Winston C, Davis M, Wortley P, Clark S. Influenza vaccination status and influenza-related perspectives and practices among US physicians. Am J Infect Control. 2006;34:164–169. doi: 10.1016/j.ajic.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 16.Clark S, Cowan A, Wortley P. Influenza vaccination attitudes and practices among US registered nurses. Am J Infect Control. 2009;37:551–556. doi: 10.1016/j.ajic.2009.02.012. [DOI] [PubMed] [Google Scholar]


