Supplemental Digital Content is available in the text
Keywords: economic well-being, financial difficulties, financial toxicity
Abstract
The aim of the study was to examine how multimorbidity influences the prevalence of financial burden among older adults with heart disease, diabetes, or cancer.
The study was a cross-sectional analysis of prospective observational cohort survey study.
Older adults (age 65 or older) who did not report 1/6 major chronic illnesses (n = 2773; reference group), reported 1/3 major chronic illnesses without comorbidity (heart disease n = 206; diabetes n = 460; cancer n = 417), and reported 1/3 major chronic illnesses with comorbidity (heart disease n = 232; diabetes n = 202; cancer n = 109).
The measures were presence of chronic diseases (heart disease, diabetes, cancer), comorbid chronic diseases (stroke, lung disease, dementia), medical-related financial burden (credit card debt due to medical costs, paying medical bills over time), and overall financial burden (financial help from family, credit card debt, help with food, utilities, and other necessities).
The proportion reporting financial burden ranged from 15% to 27% across samples. Heart disease was unrelated to medical or overall financial burden, regardless of comorbidity. Diabetes was unrelated to financial burden except diabetes without comorbidity was associated with lower odds of overall financial burden compared to healthy older adults (odds ratio [OR] = 0.655, 95% confidence interval [CI]: 0.468–0.917). Cancer with comorbidity, but not cancer without comorbidity, was associated with greater odds of medical related (OR = 1.678, 95% CI: 1.057–2.664) and overall financial burden (OR = 1.748, 95% CI: 1.064–2.872).
The association of multimorbidity with financial burden likely varies based on specific diseases. Future research on financial burden should focus on specific disease combinations such as cancer with comorbidity.
1. Introduction
Increased life expectancy partly reflects the success of advanced health interventions, but the steady growth of the aging population also poses a challenge in the increased number of older adults with chronic conditions.[1] Total health care expenses in 2014 estimated that cancer, heart disease, and diabetes were among the top 5 most expensive chronic conditions.[2] Persons diagnosed with cancer, heart disease, or diabetes often face potential financial burden due to ongoing out of pocket expenses for both medical and nonmedical care. Severe financial burden can cause nonadherence with treatment.[3,4]
Financial burden can be defined a variety of ways. Bankruptcy, out-of-pocket costs, and out-of-pocket costs in relation to family income have frequently been studied as a measure of objective financial burden.[5–7] Subjective financial burden, also called financial stress or perceived financial burden, has also frequently been studied.[8–10] These measures can be conceptualized at the individual level (i.e., such as using individual income) or the family level (such as using family or household income). For this particular study, we were interested in assessing financial burden not specifically related to the chronic conditions to see if chronic illness can increase the risk of financial problems in other areas of a person's life as has been suggested by prior research.[11]
Patient-level factors may increase the risk of financial burden, including multimorbidity (the presence of 2 or more chronic conditions)[12] and comorbidity (the presence of another chronic condition in addition to the index condition).[13] Previous research on comorbidity and patient-level financial burden has been mixed[14–16] but previous studies did not always focus on a specific index condition. We have to know who is at highest risk for financial burden by index condition to intervene, particularly given the organization of most health care systems by specialty.
Using cross-sectional analysis of data from The National Health and Aging Trends Study (NHATS),[17] this study examined whether comorbidity in the context of heart disease, diabetes, or cancer predicted worse individual (patient) level financial burden. Research has documented the cost to society overall (i.e., payers, total costs) of these diseases, but the actual individual impact to older adults is less studied.[18] We hypothesized that comorbidity will be associated with greater likelihood of financial problems compared to healthy controls.
2. Methods
2.1. Participants and procedures
We used public use data files from the National Health and Aging Trends Study (NHATS).[17] NHATS consists of a nationally representative sample of Medicare enrollees age 65 or older with oversampling of African American enrollees. The NHATS sample is community dwelling. NHATS started in 2011 and surveys participants every year. Surveys cover the environment, technology use, and other factors that affect the independence of older adults. Trained interviewers administered each survey. In 2015, NHATS recruited additional participants for the 5th survey. The 1st cohort, recruited in 2011, had 8245 participants. The 2nd cohort, recruited in 2015, had 4182 participants. The NHATS study was reviewed by the John Hopkins Bloomberg School of Public Health Institutional Review Board and all NHATS participants provided written informed consent. For this analysis, we used both cohorts and focused on the baseline surveys (2011 for the 1st cohort, 2015 for the 2nd cohort).
2.2. Measures
2.2.1. Medical-related financial burden
Each of the NHATS surveys included 2 questions about financial difficulties due to medical costs: paying medical bills over time and any amount of credit card debt from medical costs. We counted participants as experiencing medical-related financial burden if they reported at least one of the 2 items on the 1st survey.
2.2.2. Overall financial burden
Each of the NHATS surveys included 5 questions about financial difficulties the participant might have experienced in the previous year: only paying the minimum each month on credit cards; financial help from family members; used food stamps (Supplemental Nutrition Assistance Program or SNAP); received other food assistance such as meals-on-wheels; and received assistance with utilities. We counted a participant as experiencing financial burden if they reported any of the 5 items on the 1st survey. This dichotomous measure is similar to analyses from the Medical Expenditure Panel Survey, Cancer Survivorship Supplement.[15,19]
2.2.3. Health conditions
The NHATS also asks participants to self-report whether a doctor diagnosed them with any of the following medical conditions: heart attack, heart disease, high blood pressure (hypertension), arthritis, osteoporosis, diabetes, lung disease, stroke, dementia, and cancer. Previous research has shown good concordance between self-report and medical-record extracted health conditions except for arthritis.[20,21]
2.2.4. Demographics and insurance characteristics
The NHATS surveys ask participants to self-report age, gender, household income, and race/ethnicity. Participants also report whether they have prescription drug insurance, such as through Medicare Part D, a Medicare Advantage Plan or other means. The surveys also ask whether participants have additional health insurance from Medicaid or Tricare. Age is reported in 5-year increment categories: 65 to 69 years, 70 to 74 years, 75 to 79 years, 80 to 84 years, 85 to 89 years, and 90 years or more. Income was also categorized: less than $27,600 per year, $27,600 to $41,999, $42,000 to $63,999, $64,000 to $107,999, and $108,000 or more. NHATS provides multiple imputations for income when missing. We used the average of the 5 imputations for any participants with missing income data. As the income data came from 2 different years, we converted income amount to 2015 dollars.
2.3. Data analysis
We limited the NHATS sample (n = 12,427) to 6 groups of participants with chronic illness and compared the association of chronic illness to a control (comparison) group with no reported chronic disease. People were classified into the disease groups if they reported one of the 3 diseases of interest and whether they reported another comorbid disease: cardiovascular disease (either heart attack or heart disease; No comorbidity, n = 206; Comorbidity, n = 232), diabetes (No comorbidity, n = 460; Comorbidity, n = 202), or cancer (No comorbidity, n = 417; Comorbidity, n = 109). Participants were classified as having a comorbidity if they reported one or more of the other 3 index diseases (heart disease, diabetes, cancer), stroke, lung disease, or dementia. The comparison group (n = 2773) were NHATS participants that did not report any of the following 6 diseases: cardiovascular disease, diabetes, cancer, lung disease, stroke, or dementia. Participants missing information on diseases were excluded from analyses.
A logistic regression tested the relationship of group (disease only, disease with comorbidity, and control) to reporting financial burden (Y/N). Predictors included group and covariates (age, gender, income, race/ethnicity, drug coverage, and additional insurance). Our dependent variable was whether participants reported financial burden at the 1st survey. If they did not have financial burden data at the 1st survey, we checked subsequent surveys and used that financial burden data instead. For participants who entered NHATS on the 5th survey, we treated the 5th survey as their 1st survey. A separate logistic regression was run for each disease group (cancer, cardiovascular disease, diabetes) and for 2 measures of financial burden (overall, medical-related) for a total of 6 regressions. We constructed 95% confidence intervals (CIs) around each odds ratio (OR). Analyses were performed using SAS, version 9.4 (SAS Institute, Inc, Cary, NC).
3. Results
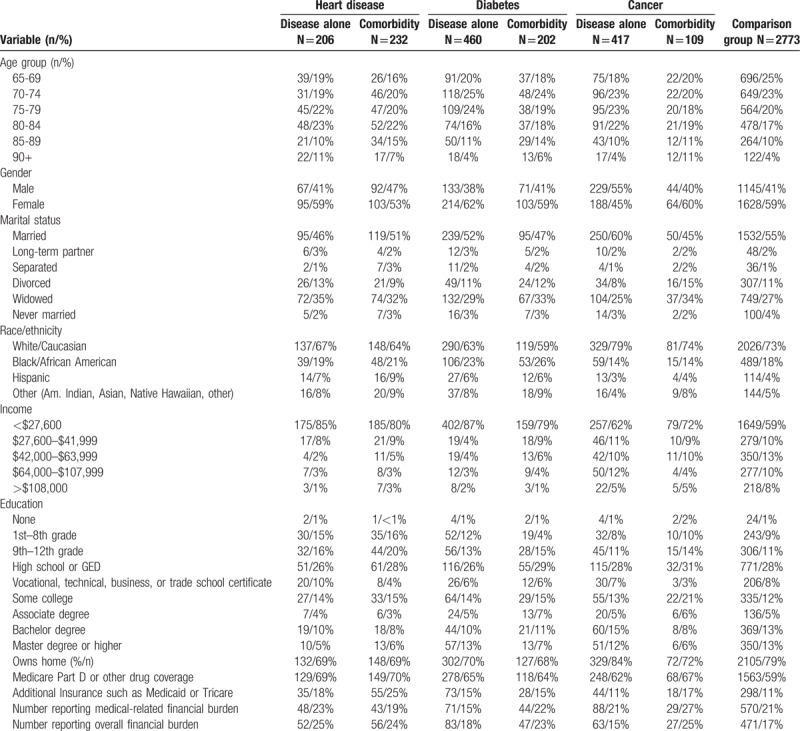
More than half the sample was female and half was married or in a long-term relationship (Table 1). The majority of the sample was white and reported incomes below $27,600. Most had completed high school or some form of college degree. Between two-thirds and four-fifths reported owning their home. Between 59% and 71% reported some form of health insurance for medications. Across the 7 groups, the proportion reporting financial burden ranged from 15% to 27%. Of the 232 people with heart disease and a comorbidity, 35% (n = 81) also had diabetes and 25% (n = 59) also had cancer. Of the 202 people with diabetes and a comorbidity, 40% (n = 81) also had heart disease and 31% (n = 62) also had cancer. Of the 109 people with cancer and a comorbidity, 57% (n = 62) also had diabetes and 54% (n = 59) also had heart disease.
Table 1.
Descriptive statistics for disease samples and controls.
In unadjusted logistic regressions, heart disease was associated with overall financial burden (without comorbidity OR: 1.609, 95% CI: 1.159–2.234; with comorbidity OR: 1.516, 95% CI: 1.106–2.078) but not medical-related financial burden (without comorbidity OR: 1.168, 95% CI: 0.836–1.633; with comorbidity OR: 0.875, 95% CI: 0.621–1.232). Diabetes with comorbidity (OR: 1.439, 95% CI: 1.025–2.022) was associated with overall financial burden but diabetes without comorbidity was not (OR: 1.045, 95% CI: 0.809–1.349). Diabetes with comorbidity was not associated with medical-related financial burden (OR: 1.077, 95% CI: 0.762–1.522) but diabetes without comorbidity was (OR: 0.706, 95% CI: 0.540–0.924). Cancer without comorbidity was not associated with financial burden (medical-related OR: 1.031, 95% CI: 0.802–1.327; overall OR: 0.847, 95% CI: 0.637–1.126). Cancer with comorbidity was associated with overall financial burden (OR: 1.568, 95% CI: 1.004–2.447) and nearly associated with medical-related financial burden (OR: 1.398, 95% CI: 0.906–2.158).
In the multivariate models, increasing age predicted lower odds of medical-related financial burden (Figs. 1 and 2; Supplementary Tables S1–S3; P < .01) compared to the youngest age group (65–69 years old) but not for overall financial burden. Women, Hispanic and African American participants had higher odds of reporting both medical-related and overall financial burden than men and white participants (P < .05) in nearly all analyses. People with higher incomes tended to report less financial burden (P < .02) but this association was less consistent with medical-related financial burden. Not having drug coverage and not having additional insurance was unassociated with medical-related financial burden but was associated with overall financial burden (P < .05) such that not having additional insurance or drug coverage predicted lower odds of overall financial burden. This was likely because some of the financial burden measures (qualifying for food stamps or other assistance programs) had similar eligibility requirements as Medicaid, one of the other forms of insurance and a possible source of drug coverage.
Figure 1.
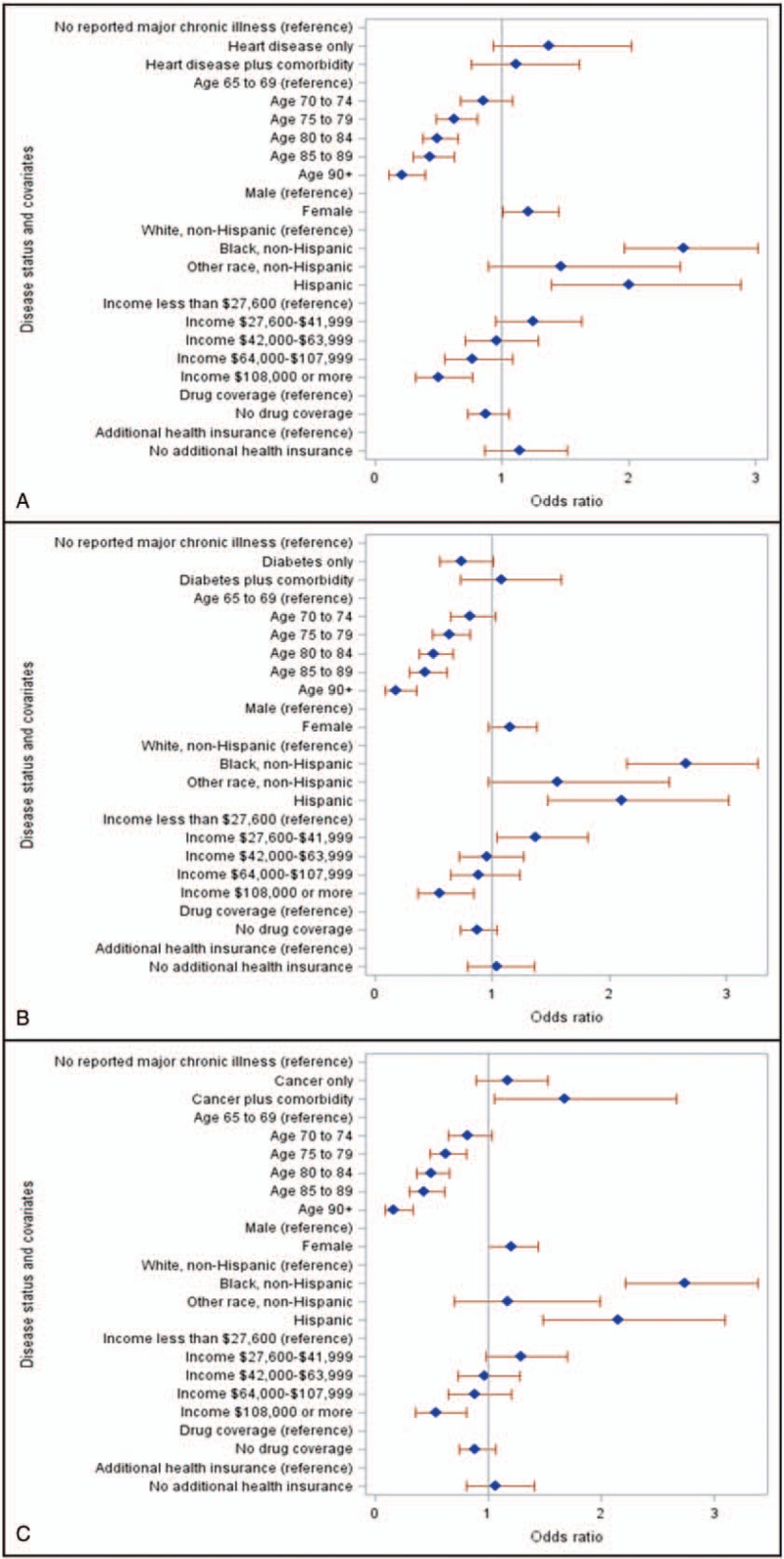
Forest plots for medical-related financial burden for heart disease (A), diabetes (B), and cancer (C). Odds ratios over 1 indicate greater odds of reporting financial burden. Reference groups are listed before corresponding effects groups.
Figure 2.
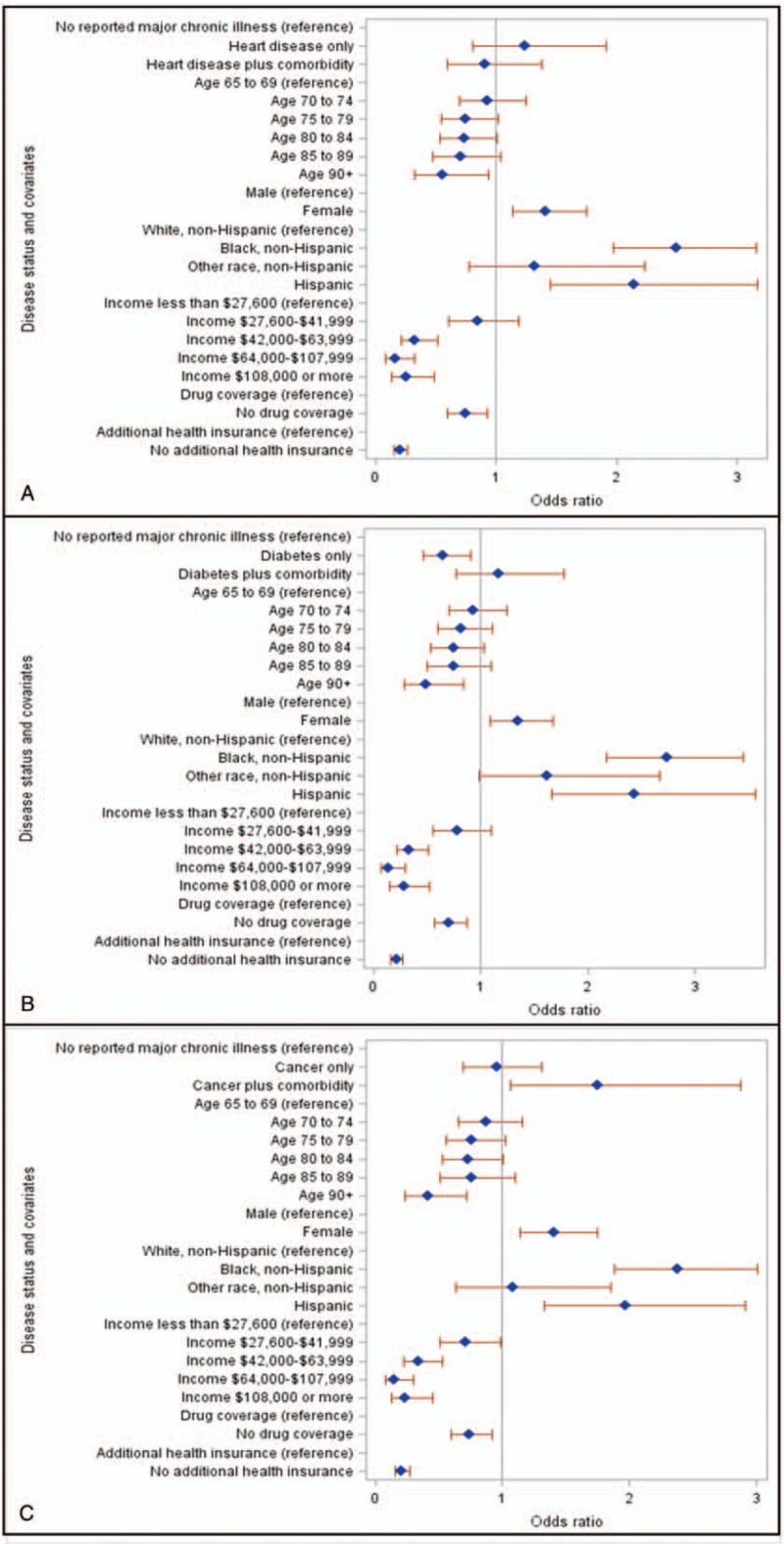
Forest plots for overall financial burden for heart disease (A), diabetes (B), and cancer (C). Odds ratios over 1 indicate greater odds of reporting financial burden. Reference groups are listed before corresponding effects groups.
In the multivariate analyses, the majority of the relationships from the unadjusted models did not remain. Diagnosis of heart disease was not associated with increased or decreased odds of medical-related and overall financial burden compared to healthy controls (P > .260). A diagnosis of diabetes without one of the other 5 major illnesses was associated with lower odds of overall financial burden (OR = 0.66, 95% CI: 0.47–0.92) but was unrelated to medical-related financial burden (P = .139). Having a diagnosis of cancer without comorbidity was unrelated to financial burden compared to healthy controls but having a cancer diagnosis plus comorbidity was associated with greater odds of medical-related financial burden (OR = 1.68, 95% CI: 1.06–2.66) and overall financial burden (OR = 1.75, 95% CI: 1.06–2.87).
4. Discussion
The present study examined the cross-sectional association of comorbidity in common medical conditions to self-reported financial burden compared to healthy older adults. Heart disease and diabetes were largely unrelated to reported financial burden regardless of comorbidity status. Cancer with comorbidity was associated with greater odds of financial burden, both medical related and general. Cancer without comorbidity was not associated with increased odds of financial burden compared to controls without major chronic illness. Results suggest the relationship of comorbidity to financial burden may depend on the index disease.
Previous studies examining the relationship between comorbidity and financial burden at the patient level have been mixed. Some studies have shown no relationship between comorbidity and financial burden[15,16] while another study showed comorbidity in cancer and heart disease was associated with a decrease in income.[14] Previous studies have not focused exclusively on older adults and this could explain the difference from our results in older adults as younger adults may face different financial problems (loss of or decrease in employment, less savings) than most older adults (fixed income). Also, the studies finding no relationship of comorbidity and financial burden used disease count instead of examining specific diseases. Both our study and the study finding a relationship[14] examined specific diseases.
Heart disease was unrelated to financial burden as was diabetes despite increasing insulin costs.[22] A possible explanation is that Medicare coverage, which the entire sample had, buffered against some of the financial consequences of chronic illness. Research in cancer has shown that younger patients (<65 years of age) experience higher costs than older patients (>65 years of age) in the United States.[23] Adverse selection may also explain these findings. Adverse selection refers to people with more medical needs selecting more comprehensive health insurance coverage[24] and this can occur in Medicare plans.[25] The variability in heart disease could account for the lack of a relationship of heart disease to financial burden. The survey did not ask about specific forms of heart disease so this hypothesis was not tested. People with diabetes in this sample may have been less likely to need expensive medications like insulin and may have used less expensive medication such as metformin. The cost of diabetes may have largely been due to medication costs rather than outpatient or inpatient services[26] and the insurance coverage of participants buffered against the cost of medications more so than the cost of outpatient treatments such as chemotherapy infusions.[27] This would explain why having diabetes was unassociated with financial burden but cancer with comorbidity was. It is also important to note that the majority of the people with cancer and a comorbidity had diabetes or heart disease and this group had higher financial burden. So it might be the combination of cancer with either heart disease or diabetes that confers the greatest risk of financial burden.
The limitations of the study warrant discussion. The sample sizes for some subgroups were relatively small preventing additional investigation of specific disease combinations and our design was cross-sectional. Due to the sample size, we had to combine 2 cohorts of data. Comorbidity and cancer may have led to financial problems or financial problems may have preceded cancer with comorbidity. The financial difficulties and chronic conditions measured were not comprehensive. We also could not include all possible confounds such as Medicare advantage vs Medicare supplement. We were unable to determine who had a Medicare advantage plan based on the survey. Although we had information on other insurance plans, one of these plans (Medicaid) has similar eligibility criteria to some of the measures of financial burden (food assistance). We also were not able to assess medical or out-of-pocket costs directly as these were not collected in the survey. Despite these limitations, the results suggest important directions for future research.
Our results support the continued focus on comorbidity in older adults.[12,28] While research has shown the overall societal cost of comorbidity,[13] our results suggest that, for cancer at least, comorbidity may also increase financial burden for patients despite any buffering from Medicare coverage. As this sample all had health insurance (Medicare), future research is needed on what insurance characteristics buffer against financial burden. Research has shown that increases in price[29] and service intensity[26] account for growth in health care spending in the United States and these may also be factors in patient-level financial burden for people with cancer and comorbidity. Although continued research on societal costs of comorbidity is warranted, future research should include a focus on how increasing health care costs affect patients financially.
Author contributions
Conceptualization: Salene M.W. Jones, Trung Nguyen, Catherine Fedorenko, Scott D. Ramsey.
Formal analysis: Salene M.W. Jones, Shasank Chennupati, Catherine Fedorenko.
Methodology: Salene M.W. Jones.
Supervision: Salene M.W. Jones.
Writing – original draft: Salene M.W. Jones.
Writing – review & editing: Salene M.W. Jones, Shasank Chennupati, Trung Nguyen, Catherine Fedorenko, Scott D. Ramsey.
Salene M. W. Jones orcid: 0000-0003-2140-5798.
Supplementary Material
Footnotes
Abbreviations: GED = general education degree, NHATS = National Health and Aging Trends Study, OR = Odds ratio.
The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
References
- [1].An Aging World: 2001. Washington, DC: US Census Bureau; 2001. [Google Scholar]
- [2].AHRQ. Total expenses and percent distribution for selected conditions by source of payment: United States, 2010. Medical Expenditure Panel Survey. AHRQ; 2014. [Google Scholar]
- [3].Dusetzina SB, Winn AN, Abel GA, et al. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol 2014;32:306–11. [DOI] [PubMed] [Google Scholar]
- [4].Kaisaeng N, Harpe SE, Carroll NV. Out-of-pocket costs and oral cancer medication discontinuation in the elderly. J Manag Care Spec Pharm 2014;20:669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Park J, Look KA. Relationship between objective financial burden and the health-related quality of life and mental health of patients with cancer. J Oncol Pract 2018;14:e113–21. [DOI] [PubMed] [Google Scholar]
- [6].Ramsey S, Blough D, Kirchhoff A, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 2013;32:1143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 2016;34:980–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Francoeur RB. Cumulative financial stress and strain in palliative radiation outpatients: the role of age and disability. Acta Oncol (Stockholm, Sweden) 2005;44:369–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ell K, Xie B, Wells A, et al. Economic stress among low-income women with cancer: effects on quality of life. Cancer 2008;112:616–25. [DOI] [PubMed] [Google Scholar]
- [10].Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract 2014;10:332–8. [DOI] [PubMed] [Google Scholar]
- [11].Hamilton JG, Wu LM, Austin JE, et al. Economic survivorship stress is associated with poor health-related quality of life among distressed survivors of hematopoietic stem cell transplantation. Psychooncology 2013;22:911–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Salive ME. Multimorbidity in older adults. Epidemiol Rev 2013;35:75–83. [DOI] [PubMed] [Google Scholar]
- [13].Glynn LG, Valderas JM, Healy P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract 2011;28:516–23. [DOI] [PubMed] [Google Scholar]
- [14].Dowling EC, Chawla N, Forsythe LP, et al. Lost productivity and burden of illness in cancer survivors with and without other chronic conditions. Cancer 2013;119:3393–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yabroff KR, Dowling EC, Guy GP, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol 2016;34:259–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Rogowski J, Lillard LA, Kington R. The financial burden of prescription drug use among elderly persons. Gerontologist 1997;37:475–82. [DOI] [PubMed] [Google Scholar]
- [17]. National Health and Aging Trends Study. Produced and distributed by www.nhats.org with funding from the National Institute on Aging (grant number NIA U01AG32947) [Google Scholar]
- [18].Valtorta NK, Hanratty B. Socioeconomic variation in the financial consequences of ill health for older people with chronic diseases: a systematic review. Maturitas 2013;74:313–33. [DOI] [PubMed] [Google Scholar]
- [19].Jones SMW, Walker R, Fujii M, et al. Financial difficulty, worry about affording care, and benefit finding in long-term survivors of cancer. Psychooncology 2018;27:1320–6. [DOI] [PubMed] [Google Scholar]
- [20].Haapanen N, Miilunpalo S, Pasanen M, et al. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol 1997;145:762–9. [DOI] [PubMed] [Google Scholar]
- [21].Zhu K, McKnight B, Stergachis A, et al. Comparison of self-report data and medical records data: results from a case-control study on prostate cancer. Int J Epidemiol 1999;28:409–17. [DOI] [PubMed] [Google Scholar]
- [22].Holden SE, Poole CD, Morgan CL, et al. Evaluation of the incremental cost to the National Health Service of prescribing analogue insulin. BMJ Open 2011;1:e000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Banegas MP, Yabroff KR, O’Keeffe-Rosetti MC, et al. Medical care costs associated with cancer in integrated delivery systems. J Natl Compr Canc Netw 2018;16:402–10. [DOI] [PubMed] [Google Scholar]
- [24].Adverse Selection Issues and Health Insurance Exchanges Under the Affordable Care Act. Washington, DC: National Association of Insurance Commissioners; 2011. [Google Scholar]
- [25].Lustig J. Measuring welfare losses from adverse selection and imperfect competition in privatized Medicare. Manuscript, Boston University; 2010 [Google Scholar]
- [26].Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US Health Care Spending, 1996-2013. JAMA 2017;318:1668–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Adrion ER, Ryan AM, Seltzer AC, et al. Out-of-pocket spending for hospitalizations among nonelderly adults. JAMA Intern Med 2016;176:1325–32. [DOI] [PubMed] [Google Scholar]
- [28].Loza E, Jover JA, Rodriguez L, et al. Multimorbidity: prevalence, effect on quality of life and daily functioning, and variation of this effect when one condition is a rheumatic disease. Semin Arthritis Rheum 2009;38:312–9. [DOI] [PubMed] [Google Scholar]
- [29].Anderson GF, Reinhardt UE, Hussey PS, et al. It's the prices, stupid: why the United States is so different from other countries. Health Aff (Millwood) 2003;22:89–105. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


