Abstract
Cubitus varus deformity is common in children. The purpose of this study was to assess the usefulness of computer simulation based on three-dimensional computed tomography (3D-CT) reconstruction with regard to preoperative planning and surgical treatment in children with traumatic cubitus varus deformity.
The study included 13 patients with traumatic cubitus varus deformity between January 2012 and January 2015. The original 3D-CT data were transferred to Mimics 10.01 software. Special tools were used for simulation of supracondylar lateral wedge osteotomy of the humerus. Intraoperative elbow arthrography was used to identify the articular surface of the elbow joint for assisting the judgment of the osteotomy site. Kirschner wires were used to determine the osteotomy plane and angle. The osteotomy site was fixed by crossing Kirschner wires and steel wire tension band.
Of the 13 patients, 11 were male and 2 were female. The left side was affected in 8 patients, and the right side was affected in 5 patients. The patient age ranged from 2 years to 14 years (mean age, 6 years and 7 months). The varus angle ranged from 12° to 35° (mean angle, 20°). The carrying angle on the contralateral side ranged from 5° to 18° (mean angle, 10°). The varus deformities showed good correction. The 13 patients were followed up for 24 to 60 months (mean follow-up, 38 months). According to the Flynn score of elbow joint function after surgery: 10 patients had excellent function, 2 had good function, and 1 had fair function. The excellent rate was 92.3%. At the final follow-up, the ipsilateral carrying angle ranged from 4° to 15° (mean angle, 11°).
Computer simulation based on 3D-CT reconstruction can provide good information on the right humeral osteotomy position and osteotomy angle. It can guide the actual operation and provide better results after surgery. Intraoperative elbow arthrography is useful to determine the level of elbow joint osteotomy, and it can assist in the operation.
Level of evidence: Level IV-retrospective case, treatment study.
Keywords: 3D reconstruction, children, computer simulation, cubitus varusreconstruction
1. Introduction
Cubitus varus deformity is common in children, and it is caused by the malunion of supracondylar fractures of the humerus in most clinical cases.[1] Cubitus varus deformity not only causes poor aesthetic appearance of the elbow but also affects the biomechanics of the elbow joint. Additionally, it might increase the risk of lateral condyle fractures and other secondary fractures.[2,3] Supracondylar osteotomy is one of the common surgical procedures for the treatment of cubitus varus deformity in children. There are various techniques for performing supracondylar osteotomy, including lateral closing-wedge osteotomy,[4,5] medial opening-wedge osteotomy,[6] dome osteotomy,[7] and reverse V osteotomy.[8,9] However, performing osteotomy with an accurate angle is a challenge. 3D-CT reconstruction could be used to simulate the direction of osteotomy and the angle of osteotomy.[10] Simulation can make osteotomy more accurate, and it might help achieve a better postoperative outcome.[11] The purpose of this study was to assess the usefulness of computer simulation based on 3D-CT reconstruction with regard to preoperative planning and surgical treatment in children with traumatic cubitus varus deformity.
2. Methods
From January 2012 to January 2015, we experienced 13 cases of traumatic cubitus varus. The inclusion criteria were as follows:
-
(1)
varus angle above 10°;
-
(2)
post-traumatic time over 6 months; and
-
(3)
no progression of the deformity over 3 months.
The time from injury to operation ranged from 6 months to 5 years and 2 months (mean time, 1 year and 8 months). The study was approved by the ethics committee of Hong Hui Hospital, Xi’an Jiao Tong University College of Medicine. All patients were operated at Hong Hui Hospital.
Data were collected using the Brilliance 16-slice spiral CT system (Philips Healthcare, Best, the Netherlands). Mimics 10.01 software (Materialise, Leuven, Belgium) was used to simulate the operation on a computer. The computer had the following specifications: AMD AthlonTM II Dual-Core M320 2.09 GHz processor and ATI Mobility Radeon HD 4200 graphics card.
The varus angle on the affected side (Fig. 1a) and the carrying angle on the normal side (Fig. 1b) were measured before the operation. The original CT data were imported into Mimics 10.01 software to reconstruct 3D images of the distal humerus and proximal ulna and radius. The osteotomy plane was selected on the supracondylar side of the humerus. The first osteotomy line was 0.5 cm above the proximal end of the olecranon fossa. There was a certain angle between the line and the horizontal articular surface of the elbow. The line was from the lateral supracondylar region to the medial epicondyle of the humerus (Fig. 1c). The second osteotomy line was above the first line. The length of these 2 lines was the same. The angle between the second and first osteotomy lines was the angle to be corrected (the carrying angle on the normal side plus the varus angle on the affected side) (Fig. 1d). The bone block was removed, and the osteotomy surface was involuted to observe the effect of the correction. The angle of the osteotomy bone block and the length of the bottom edge could be measured by using the measuring tools in the software to guide the operation. The angle of a typical case was 36°, and the length of the bottom edge was 1.6 cm.
Figure 1.
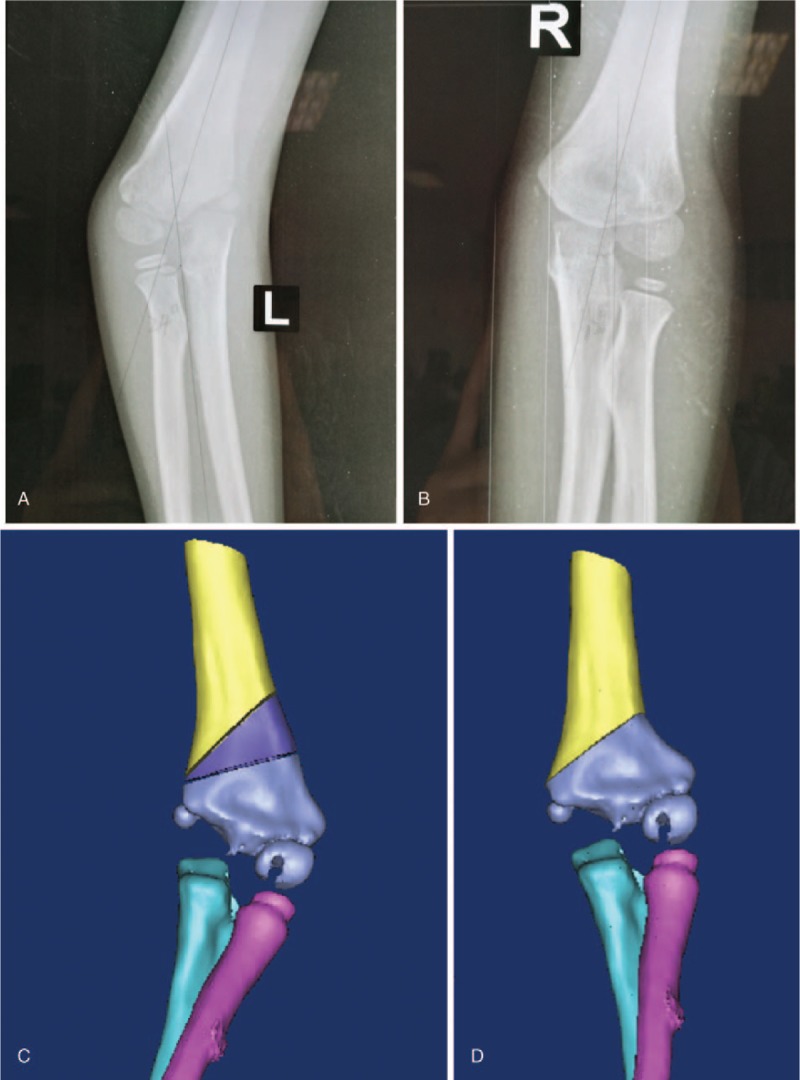
A: Frontal radiograph of the affected elbow joint shows a 24° varus angle preoperatively. B: Normal lateral carrying angle is 12° preoperatively. C: Simulation of closed-wedge osteotomy of the supracondylar region of the humerus preoperatively. D: Outcome after removing the osteotomy bone block.
Elbow arthrography was performed to assess the articular surface of the elbow in the horizontal plane (Fig. 2a). Closed-wedge osteotomy was performed on the lateral supracondylar region of the humerus using Kirschner-wires (K-wires). The bottom edge of the osteotomy was measured with a ruler, which was consistent with the simulation before the operation (Fig. 2b). In order to achieve an osteotomy angle of 36°, the bottom edge of the osteotomy should be 1.6 cm. A second K-wire was placed proximal to the first wire. The distance from the first K-wire was 1.6 cm. Wedge-shaped osteotomy was performed with a saw along the direction of the K-wires. Then, the osteotomy bone block was removed. Two or three 1.5 mm K-wires were used at the distal end, and one or two 1.5 mm K-wires were used at the proximal end of the osteotomy site. Fixation was observed through intraoperative fluoroscopy (Fig. 2c and d). In some cases, in which the stability of the fixation was not sufficient, a 0.6 mm or 0.8 mm wire was used for tension-band wiring to strengthen the internal fixation.
Figure 2.

A: Measurement of the bottom edge of the osteotomy with a ruler intraoperatively. B: Kirschner-wires are used to locate the osteotomy site with the assistance of intraoperative arthrography of the elbow joint. C: Intraoperative fluoroscopy shows satisfactory correction of the varus angle. D: Lateral view of the elbow shows good correction of distal humeral anteversion.
An external brace was used 4 weeks after the operation. After removal of the external fixation, function exercises of the elbow joint could be started early, and these were beneficial for the recovery of elbow joint function. The follow-up period ranged from 1 year to 2 years and 4 months (mean follow-up, 1 year and 6 months).
3. Results
Of the 13 patients, 11 were male and 2 were female. The left side was affected in 8 patients, and the right side was affected in 5 patients. The patient age ranged from 2 years to 14 years (mean age, 6 years and 7 months). The varus angle ranged from 12° to 35° (mean angle, 20°). The carrying angle on the contralateral side ranged from 5° to 18° (mean angle, 10°). All 13 patients were followed up for 24 to 60 months (mean follow-up, 38 months). According to the Flynn score of elbow joint function, 10 patients had excellent function, 2 had good function, and 1 had fair function. The excellent and good rate was 92.3%. There were no complications, such as wound infection, ulnar nerve injury, nonunion at osteotomy, and delayed healing. At the final follow-up, the carrying angle on the affected side ranged from 4° to 15° (mean angle, 11°).
4. Discussion
Cubitus varus deformity not only causes a poor aesthetic appearance of the elbow joint, but also causes pain and progressive humeral condyle and ulnar olecranon pathological changes. Ulnar nerve paralysis has been reported in severe cases.[12] Cubitus varus caused by supracondylar fracture of the humerus in children is usually non-progressive. The timing of surgical correction is at least 6 months after injury, and the cubitus varus deformity can be corrected after 3 months without progress.
Supracondylar wedge osteotomy of the humerus is the most common procedure in the treatment of cubitus varus deformity in children.[13–15] Other procedures include step osteotomy, fornix osteotomy, and multiplanar osteotomy.[9,16,17] The important aspect of the procedure is the determination of the angle and length of the wedge-shaped osteotomy, as well as the plane and direction of the osteotomy. The postoperative appearances of different osteotomy planes and directions differ. The traditional osteotomy plane and direction were 0.5 to 1 cm at the proximal end of the olecranon fossa, and the direction was parallel to the elbow joint. Thus, the distal side of the humerus was especially prominent after the osteotomy. The lateral side of the elbow presented an "S” shape. Isosceles triangle osteotomy could make the distal and proximal ends of the osteotomy continuous, without obvious lateral protrusion.[18,19] The direction of osteotomy was from the outer upper oblique to the inner region, and it had a certain angle with the horizontal plane of the elbow joint. Isosceles triangle osteotomy was used in all 13 patients. In previous studies, K-wires, steel plates, or external fixators were used to fix the osteotomy site.[20,21] We used K-wires for fixation. The approach is simple to perform, and the cost is low.
Preoperative simulation based on 3D-CT has been widely used in orthopedic fields,[22,23] and there are few reports on the correction of cubitus varus deformity in children.[24] With preoperative simulation, the appropriate osteotomy plane and direction can be selected, the length of the bottom edge of the osteotomy can be accurately measured, and the actual operation can be guided. Additionally, the possible appearance improvement after osteotomy can be directly shown. If the appearance improvement after osteotomy does not appear ideal, the plane and direction of osteotomy can be changed on the computer, and the angle of osteotomy can be adjusted to achieve the best effect. Preoperative simulation provides information on the plane and direction of osteotomy, which might reduce operation time, reduce surgical trauma, and support postoperative rehabilitation. During osteotomy, attention should be paid to the correction of sagittal deformity as well as the coronal plane. In some cases, the anteversion angle of the distal humerus decreased; thus, anterior and narrow osteotomy was needed to restore the normal anteversion angle of the distal humerus.
Preoperative simulation has some limitations. Preoperatively, the cartilage of the distal humerus is not developed, and the horizontal articular surface of the elbow can only be judged according to the proximal end of the ulna and radius. However, during the actual operation, we can clearly identify the cartilage of the distal humerus and the horizontal articular surface of the elbow through elbow arthrography. Therefore, there are certain deviations in the plane and direction between actual osteotomy and the preoperative simulation. Isosceles triangle osteotomy can be simulated before the operation; however, in the actual operation, it is very difficult to make the lengths of the two osteotomy lines equal.
5. Conclusion
Computer simulation based on 3D-CT reconstruction can be used to observe the pathological changes of cubitus varus deformity after trauma in children more clearly and can be used to design the preoperative operation plan conveniently and guide the selection of the osteotomy plane and direction accurately. With computer simulation, better clinical results can be obtained after the operation.
Author contributions
Formal analysis: Yongtao Wu.
Investigation: Min Li.
Methodology: Yongtao Wu.
Supervision: Yongtao Wu.
Writing – original draft: Hai Jiang.
Writing – review & editing: Yongtao Wu.
Footnotes
Abbreviations: 3D = three-dimensional, CT = computed tomography, K-wire = Kirschner wire.
The authors have no conflicts of interest to disclose.
References
- [1].Solfelt DA, Hill BW, Anderson CP, et al. Supracondylar osteotomy for the treatment of cubitus varus in children: a systematic review. Bone Joint J 2014;96-B:691–700. [DOI] [PubMed] [Google Scholar]
- [2].Davids JR, Maguire MF, Mubarak SJ, et al. Lateral condylar fracture of the humerus following posttraumatic cubitus varus. J Pediatr Orthop 1994;14:466–70. [DOI] [PubMed] [Google Scholar]
- [3].Takahara M, Sasaki I, Kimura T, et al. Second fracture of the distal humerus after varus malunion of a supracondylar fracture in children. J Bone Joint Surg Br 1998;80:791–7. [DOI] [PubMed] [Google Scholar]
- [4].Siris IE. Supracondylar fractures of the humerus: an analysis of 330 cases. Surg Gynecol Obstet 1939;68:201–22. [Google Scholar]
- [5].French PR. Varus deformity of the elbow following supracondylar fractures of the humerus in children. Lancet 1959;2:439–41. [DOI] [PubMed] [Google Scholar]
- [6].King D, Secor C. Bow elbow (cubitus varus). J Bone Joint Surg Am 1951;33-A:572–6. [PubMed] [Google Scholar]
- [7].Ali AM, Abouelnas BA, Elgohary HS. Dome osteotomy using the paratricipital (triceps-sparing) approach for cubitus varus deformity in children: a surgical technique to avoid lateral condylar prominence. J Pediatr Orthop B 2016;25:62–8. [DOI] [PubMed] [Google Scholar]
- [8].Mishra PK, Verma AK, Dwivedi R, et al. Reverse V osteotomy and treatment of cubitus varus deformity - results and experience. J Clin Orthop Trauma 2016;7Suppl 2:154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yun YH, Shin SJ, Moon JG. Reverse V osteotomy of the distal humerus for the correction of cubitus varus. J Bone Joint Surg Br 2007;89:527–31. [DOI] [PubMed] [Google Scholar]
- [10].Jiang H, Miao WS, Wu YT, et al. Application of computer simulation based on three-dimensional computed tomographic reconstruction in the treatment of pediatric congenital elevated scapula with Woodward method. Chin J Pediatr Surg 2015;36:509–12. [Google Scholar]
- [11].Jiang H, Miao WS, Wu G, et al. Application of preoperative computer simulation based on three dimensional computed tomography reconstruction during Salter pelvic osteotomy of children with developmental dislocation of the hip. J Clin Pediatr Surg 2016;15:246–9. [Google Scholar]
- [12].Davids JR, Lamoreaux DC, Brooker RC, et al. Translation step-cut osteotomy for the treatment of posttraumatic cubitus varus. J Pediatr Orthop 2011;31:353–65. [DOI] [PubMed] [Google Scholar]
- [13].Devnani AS. Lateral closing wedge supracondylar osteotomy of humerus for post-traumatic cubitus varus in children. Injury 1997;28:643–7. [DOI] [PubMed] [Google Scholar]
- [14].Lee SC, Shim JS, Sul EJ, et al. Remodeling after lateral closing-wedge osteotomy in children with cubitus varus. Orthopedics 2012;35:e823–8. [DOI] [PubMed] [Google Scholar]
- [15].Hui JH, Torode IP, Chatterjee A. Medial approach for corrective osteotomy of cubitus varus: a cosmetic incision. J Pediatr Orthop 2004;24:477–81. [DOI] [PubMed] [Google Scholar]
- [16].Takagi T, Seki A, Takayama S, et al. Modified step-cut osteotomy for correction of post-traumatic cubitus varus deformity: a report of 19 cases. J Pediatr Orthop B 2016;25:424–8. [DOI] [PubMed] [Google Scholar]
- [17].Takeyasu Y, Oka K, Miyake J, et al. Preoperative, computer simulation-based, three-dimensional corrective osteotomy for cubitus varus deformity with use of a custom-designed surgical device. J Bone Joint Surg Am 2013;95:e173. [DOI] [PubMed] [Google Scholar]
- [18].Zhou HY, Zuo YM, Wang YG, et al. Supracondylar isosceles triangle osteotomy combined with locking plate fixation for cubitus varus in older children. Chin J Bone Joint Injury 2016;31:58–60. [Google Scholar]
- [19].Su Y, Nan G. Lateral closing isosceles triangular osteotomy for the treatment of a post-traumatic cubitus varus deformity in children. Bone Joint J 2016;98-B:1521–5. [DOI] [PubMed] [Google Scholar]
- [20].Belthur MV, Iobst CA, Bor N, et al. Correction of cubitus varus after pediatric supracondylar elbow fracture: alternative method using the Taylor spatial frame. J Pediatr Orthop 2016;36:608–17. [DOI] [PubMed] [Google Scholar]
- [21].Slongo T. Treatment of posttraumatic cubitus varus in children and adolescents. Supracondylar humeral osteotomy using radial external fixation. Oper Orthop Traumatol 2015;27:194–209. [Article in German]. [DOI] [PubMed] [Google Scholar]
- [22].Xu HJ, Zhou YX, Chen LB, et al. Simulated surgeries of acetabular reconstruction for high-dislocated hips. Chin J Exp Surg 2016;33:820–2. [Google Scholar]
- [23].Bao HD, Yan P, Zhu F, et al. Technology of pre-operative digitalized simulation of osteotomy in degenerative spinal deformity with sagittal malalignment. Chin J Orthop 2016;36:321–8. [Google Scholar]
- [24].Zhang YZ, Lu S, Chen B, et al. Application of computer-aided design osteotomy template for treatment of cubitus varus deformity in teenagers: a pilot study. J Shoulder Elbow Surg 2011;20:51–6. [DOI] [PubMed] [Google Scholar]


