Abstract
This study aims to evaluate the effectiveness and safety of the application of a 3-dimensional (3D)-printed composite guide plate for atlantoaxial pedicle screw.
This was a retrospective study. A total of 43 atlantoaxial dislocation patients admitted in our hospital between January 2014 and October 2016 were retrospectively analyzed. According to the different methods of operation, patients were divided into 2 groups: 3D-printed plate group (n = 19) and traditional fixation group (n = 24). Placement time, operation duration, fluoroscopy number, intraoperative bleeding volume, and the neck and shoulder pain visual analog scale and Japanese Orthopaedic Association cervical nerve function scores were compared between pre- and postoperation.
Differences in general data between these 2 groups were not statistically significant (P > .05). For patients in the 3D-printed plate group, a total of 68 assisting screws were placed at the pedicle, the accuracy rate of screw placement was 94.1%, placement time was 2.2 ± 0.4 minutes, fluoroscopy number was 4.6 ± 1.1 times, operation duration was 197 ± 41 minutes, and intraoperative bleeding volume was 395 ± 64 mL. In the traditional fixation group, a total of 76 screws were placed at the pedicle of patients, the accuracy rate of screw placement was 76.3%, placement time was 3.4 ± 0.7 minutes, fluoroscopy number was 9.4 ± 2.7 times, operation duration was 245 ± 67 minutes, and intraoperative bleeding volume was 552 ± 79 mL. Differences in accuracy rate, placement time, fluoroscopy number, operation duration, and intraoperative bleeding volume between these 2 groups were statistically significant (P < .05).
The effectiveness and safety of 3D-printed composite guide plate for atlantoaxial pedicle screw were better than traditional method.
Keywords: cervical vertebrae, computer assisted, 3-dimensional printing model, pedicle screw, rapid prototyping technology
1. Introduction
Cervical vertebrae, especially atlantoaxial dislocation, is usually caused by traffic accidents, falls, and crushing, which likely leads to high cervical spinal cord injury and other serious consequences.[1] Effective pedicle screw is considered to be a reliable method for the treatment of these injuries.[2] However, the anatomical structures of the atlantoaxial joint are complex, while the pedicle is tiny and close to many important tissues such as the vertebral artery, cervical spinal cord, and nerve root. Therefore, the unarmed placement of atlantoaxial pedicle screws is difficult and of high risk.[3] Three-dimensional (3D) printing model technology has been successfully applied in fracture, joint replacements, and spine pedicle screw fixations.[4–6] Its application in orthopedic surgery has become more and more mature. Through medical digital technology, computer-aided design, and rapid prototyping technology, an individualized guide plate could be designed to make the operation safer and more effective.
In this study, data obtained from 19 atlantoaxial fracture dislocation patients, who were admitted in our hospital and underwent atlantoaxial pedicle screw fixation assisted by a 3D-printed guide plate between January 2013 and October 2015, were retrospectively analyzed and compared with 24 patients who underwent traditional screw placement, to verify the safety, feasibility, and effectiveness of this approach. Details are reported in the following sections.
2. Materials and methods
This study was conducted in accordance with the Declaration of Helsinki. This study was conducted with approval from the Ethics Committee of our hospital. Written informed consent was obtained from all participants.
This was a retrospective study. A total of 43 atlantoaxial dislocation patients admitted in our hospital between January 2013 and October 2015 were retrospectively analyzed. The statistical software was used to calculate the sample size. According to the different methods of operation, patients were divided into 2 groups: 3D-printed plate group (n = 19) and traditional fixation group (n = 24). Placement time, operation duration, fluoroscopy number, intraoperative bleeding volume, and the neck and shoulder pain visual analog scale (VAS) and Japanese Orthopaedic Association (JOA) cervical nerve function scores were compared between pre- and postoperation.
2.1. Inclusion and exclusion criteria
Inclusion criteria: patients who were diagnosed as atlantoaxial fracture/dislocation (subluxation) and suitable for pedicle screw; patients with neck pain and limited movement; and patients without surgical contraindications.
Exclusion criteria: patients who had small vertebral arch pedicles or unsuitable for pedicle screw placement due to deformities and variations; patients who could not tolerate surgery due to multisystem diseases, such as heart failure, cancer, severe liver dysfunction, or kidney dysfunction and so on.
2.2. Application of the 3D-printed plate in the operation
Before the operation, the atlantoaxial model and 3D-printed plate were subjected to low temperature plasma sterilization. A posterior incision was routinely made, and the soft tissues of the spinous process, lamina, and facet of the cervical spine were fully stripped to expose the dorsal bony structure. The 3D-printed plate was attached to the corresponding cervical spinous process, lamina, and facet, and the tight attachment of the plate was determined. When the fit was good, the plate was fixed and maintained by the assistant in the corresponding position on the lamina. A hole was 1st drilled on the atlas along the guide channel using a Kirschner wire to establish an access channel. The Kirschner wire was maintained to stabilize the guide plate. After a hole was drilled on the atlas, the Kirschner wire used to establish the guide channel and the guide plate were removed. After opening the pedicle channel, the channel walls were inspected using a probe to confirm that the bony walls were continuously smooth. According to the preoperative measurement of the pedicle screw length and pedicle width, suitable screws were chosen, tapped, and fixed. Lateral X-ray imaging was performed using a C-arm X-ray machine, and the position of the screws was verified. Next, nail rod fixation and bone graft were performed. Patients in the traditional fixation group were treated according to the traditional screw placement technology reported in literatures.[7,8]
2.3. Assessment methods
The main ourtcomes included the placement time of each pedicle screw, operation duration, intraoperative blood loss, the number of intraoperative fluoroscopy, VAS, and JOA scores in these 2 groups. Furthermore, the VAS and JOA scores of patients in these 2 groups were recorded 1 day before and 3 days after the operation.
A computed tomography (CT) scan of the cervical spine was performed after the operation, and the accuracy of the screw placement was evaluated based on the Kawaguchi method[9]: grade 0, the screw was completely in the pedicle; grade 1: the screw pierced out of the pedicle wall for <2 mm, but no complication was found; grade 2: the screw pierced out of the pedicle wall for >2 mm, but no complication was found; grade 3: clinical complications occurred, such as vertebral artery and nerve root injuries.
At the same time, the expected values and actual measured values of the medial angle and head angle of the screw canal were measured and compared in the Mimics software.[10,11] Medial angle: the included angle between the screw canal and the median sagittal plane of the vertebral body in the CT reconstructed image on an overlooking section; head angle: the included angle between the screw canal and the vertebral endplate in the CT reconstructed image on a left view section.
At 3, 6, 12, and 24 months after discharge, patients underwent a regular review. The main observation indexes included VAS and JOA scores, bone fusion and the presence of loosening, fractures, and other complications. The VAS score was used to evaluate neck–shoulder pain. The maximum score of this index was 10 points, where 0 point suggests no pain and 10 points suggest unbearable pain. The judgment criterion of JOA fusion: cervical spinal nerve function was evaluated by cervical lateral flexion and extension scores. The maximum score of this index was 17 points. The higher the score was, the better the neurologic function become.[4] Bone graft was scanned by X-ray, a nonenhanced CT scan was performed, and the image was subjected to sagittal reconstruction. The X-ray films revealed no signs of loosening, breakage, or invagination. The CT sagittal reconstruction images revealed that there were continuous trabecular bones in the vertebral body. When both methods drew a fusion judgment, the final conclusion was bone fusion; otherwise, it was judged as nonfusion.[12]
2.4. Statistics analysis
Data were statistically analyzed using SPSS 19.0 statistical software. Continuous data were expressed as mean ± standard deviation (M ± SD). Discontinuous variable were expressed as percentage (%). Data on age, follow-up time, perioperative parameters, and preoperative and postoperative indexes were compared between the 2 groups using the Mann–Whitney U test. Count data were compared between the 2 groups using Chi-squared test. The nonnormally distributed continuous data were compared using nonparametric tests. P < .05 was considered statistically significant.
3. Results
3.1. General clinical data
Among these patients, 26 patients were males and 17 patients were females. The mean follow-up duration was 32.4 ± 10.7 months. A total of 68 screws were placed at the pedicle in the 19 patients who underwent atlantoaxial pedicle screw assisted by a 3D-printed guide plate, while a total of 76 screws were placed at the pedicle in 24 patients using the traditional method. The gender, age, diagnosis, complications, and other conditions of patients in these 2 groups are shown in Table 1. All patients in these 2 groups had trauma. The follow-up time of these 2 groups of patients was 24 ± 11 and 23 ± 9 months, respectively, and the difference was not statistically significant. In our study, no patients were lost to follow-up (Fig. 1).
Table 1.
Comparison of general information in 3-dimensional (3D) printed navigational guiding template group and traditional pedicle screw placement group.
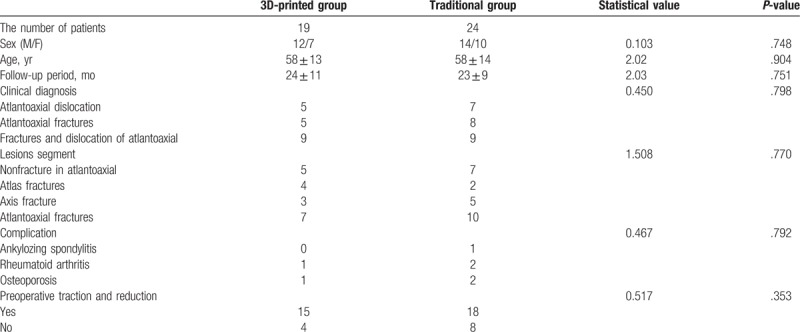
Figure 1.
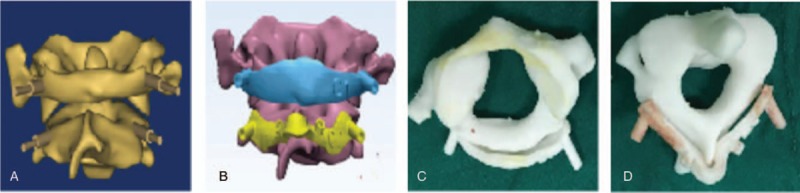
Preoperative atlantoaxial 3-dimensional (3D) model and navigational templates. (A) Atlantoaxial 3D model. (B) Atlantoaxial 3D model and templates. (C) 3D printing atlas model and temple. (D) 3D printing axis model and temple.
3.2. Evaluation of screw placement accuracy
In the 3D-printed group, 64 screws were grade 0 (94.1%, 64/68), 2 screws were grade 1 (2.94%, 2/68), 2 screws were grade 2 (2.94%, 2/68), and no screw was grade 3. In the traditional fixation group, a total of 76 screws were placed at the pedicle of patients. Among these screws, 58 screws were grade 0 (76.3%, 58/76), 12 screws were grade 1 (15.8%, 12/76), 6 screws were grade 2 (7.89%, 6/76), and no screw was grade 3. Screw placement accuracy was higher in the 3D-printed plate group than in the traditional fixation group, and the difference was statistically significant (Table 2). In addition, screw placement accuracy was further verified by deviation analysis. Results revealed that for both the atlas and axis, differences in medial angle and head angle between these 2 groups were statistically significant, and differences in medial angle and head angle between actual and expected values in the 3D-printed plate group were not statistically significant (Tables 3 and 4).
Table 2.
Evaluating the precision of 2 kinds of placing screw with Kawaguchi method.
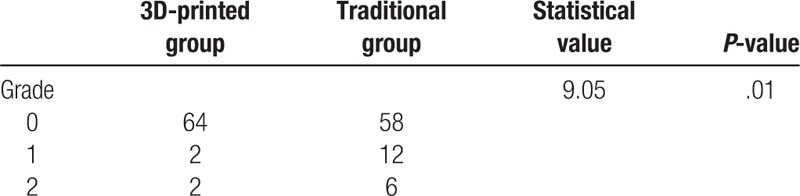
Table 3.
Comparing the sagittal angle and transverse angle of atlas in preset screw track and actual screw track.
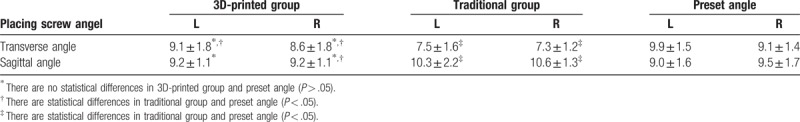
Table 4.
Comparing the sagittal angle and transverse angle of axis in preset screw track and actual screw track.
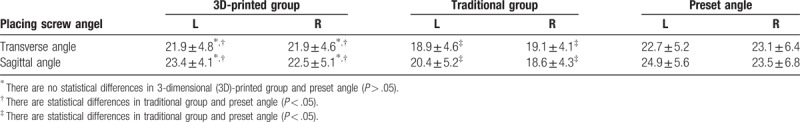
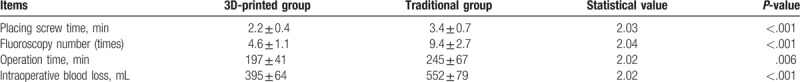
3.3. Placement time, operation duration, fluoroscopy examinations, and intraoperative bleeding volume
Placement time in the 3D-printed plate group (2.2 ± 0.4 minutes) was less than that in the traditional fixation group (3.4 ± 0.7 minutes), and the difference between these 2 groups were statistically significant (P < .001, Table 3). The number of fluoroscopy examinations was 4.6 ± 1.1 times in the 3D-printed plate group, while this number increased to 9.4 ± 2.7 times in the traditional fixation group; and the difference between these 2 groups was statistically significant (P < .001, Table 3). Operation duration and the volume of intraoperative bleeding was 197 ± 41 minutes and 395 ± 64 mL, respectively, in the 3D-printed plate group; and this was significantly lower than those in the traditional fixation group (245 ± 67 minutes and 552 ± 79 mL, respectively; P = .006 and P < .001, respectively; Table 5).
Table 5.
Comparison of perioperative related parameters in 3-dimensional (3D)-printed group and traditional group.
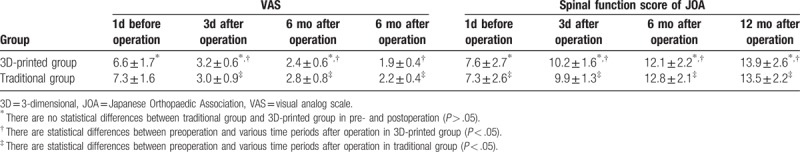
3.4. VAS and JOA scores
Differences in VAS and JOA scores 1 day before the operation between these 2 groups were not statistically significant. VAS scores of the neck and shoulder in these 2 groups were significantly lower at 3 days and at 6 and 12 months after the operation than before the operation (P < .05, Table 4). However, differences in VAS scores of the neck and shoulder at 3 days and at 6 and 12 months after the operation between the 3D-printed plate group and traditional fixation group were not statistically significant (all, P > .05, Table 4). JOA cervical nerve function scores in the 3D-printed plate group at 3 days and at 6 and 12 months after the operation significantly improved, compared with those before the operation (P < .05). However, differences in JOA cervical nerve function scores at 3 days and at 6 and 12 months after the operation between these 2 groups were not statistically significant (P > .05, Table 6).
Table 6.
Comparing VAS and JOA score in 3D-printed group and traditional group.
3.5. Complications and bone graft fusions
One patient in the traditional fixation group developed cerebrospinal leakage caused by intraoperative improper stripping, which healed after 2 weeks of active symptomatic treatment. No screw placement-related symptoms in the vertebral artery, nerve root, and cervical cord were found in these 2 groups. Up to the last follow-up, the fractures of patients in these 2 groups all healed; and patients with bone graft achieved bony fusion. No failure-related complications, such as internal fixation loosening and fracture, were found in these 2 groups. These typical cases are shown in Figure 2.
Figure 2.
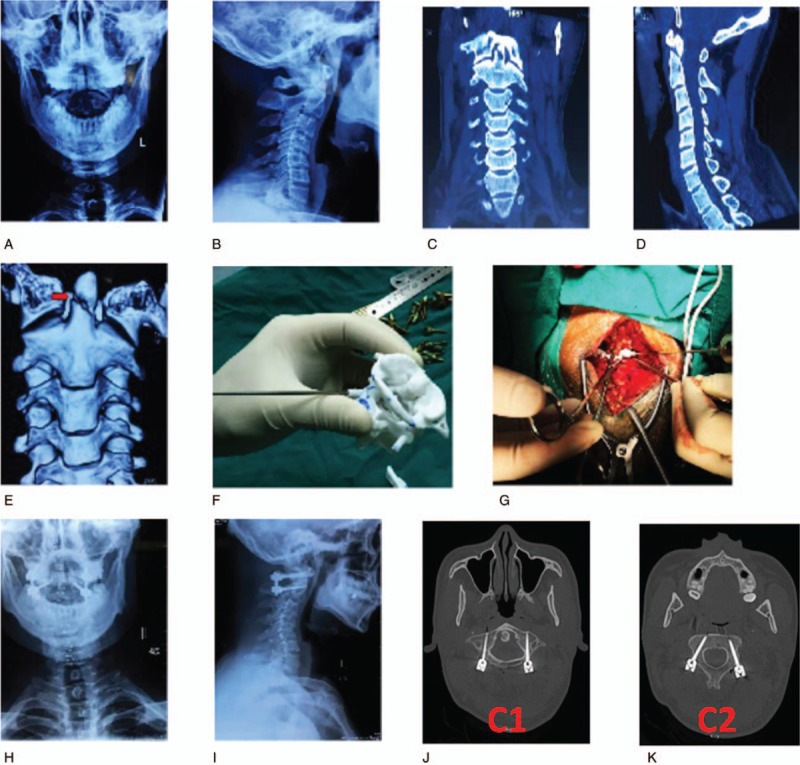
A 45-year-old man suffered traffic accident injury. (A, B) Preoperative anteroposterior and lateral X-ray view of cervical spine showed C2 odontoid fracture. (C–E) Preoperative coronal position, sagittal position, and 3-dimensional (3D) reconstruction image of computed tomography (CT) scans also showed C2 odontoid fracture. (F) Simulation operation in the printing navigation model preoperatively. (G) Placing the 3D printing model intraoperatively. (H, I) Postoperative cervical anteroposterior and lateral X-ray showed the internal fixation is well positioned. (J, K) Postoperative CT scans confirmed the pedicel screws were safely inserted into the C1 and C2 pedicles.
4. Discussion
In our study, the results showed that atlantoaxial pedicle screw fixation assisted by a 3D-printed plate significantly improved the accuracy rate of screw placement, shorted placement time, and operation duration, reduced the number of fluoroscopy examinations and intraoperative bleeding volume when compared with the traditional method.
These outcomes are consistent with those reported in some recent literatures.[13–15] Finally, after an average of 32 months of follow-ups, the clinical function (neck and shoulder VAS and JOA cervical nerve function scores) of patients in these 2 groups significantly improved after the operation, compared to those before the operation. However, differences in the above indexes at 3 days, and at 6, 12, and 24 months after the operation were not statistically significant between the 2 groups. This suggests that 3D-printed screw placement has a clinical curative effect equivalent to that of traditional screw placement. In summary, the application of 3D-printed guide plates has a relatively satisfactory safety, feasibility, and effectiveness in assisting atlantoaxial pedicle screw placement; which is worth extensive popularization and application.
In this study, the results reveal that the atlantoaxial pedicle screw placement for atlantoaxial fractures and dislocations is safe and feasible. Furthermore, the accuracy of screw placement in the 3D-printed plate group (94.1%) was far higher than that in the traditional fixation group (76.3%). Meanwhile, deviation analysis revealed that differences in medial angle and head angle between actual and expected values were not statistically significant. However, these 2 angles were significantly better than those in the traditional fixation group. This suggests that this approach can locate accurately and rapidly, and improve the accuracy of the screw placement with high safety during the operation. In addition, during the perioperative period, related parameters such as the placement time, the number of fluoroscopy examinations, operation duration, and volume of intraoperative bleeding were better in the 3D-printed plate group than in the traditional fixation group. The reasons may be that 3D-printed screw placement reduced excessive intraoperative striping, and simplified the operation. This shortened the operation duration, reduce the volume of intraoperative bleeding, reduce the number of intraoperative fluoroscopy examinations, and reduce the dose of radiation exposure.
Lu et al first designed a pedicle guide plate to conduct an experiment on screw placement in cervical vertebrae specimens, and results revealed that all screws placed at the atlantoaxial pedicle did not pierce the bone cortex; satisfactorily verifying the safety of the application of 3D-printed guide plates in atlantoaxial pedicle screw internal fixations.[16] Huang et al also confirmed through an experimental study that 3D-printed guide plates provide a new method of treatment.[17] Subsequently, Hu et al first performed screw placement assisted by a digitized 3D-printed guide plate to treat patients with atlantoaxial instability, and results revealed that after controlling human factors, it could significantly improve the accuracy of the screw placement and increase surgical safety.[18,19] Kaneyama et al and Fan et al respectively applied this technique in clinical practice, and all achieved satisfactory clinical efficacy. In addition, studies also revealed that this method had advantages of high accuracy in pedicle screw placement, lower risk during the operation, and significant improvement in surgical safety.[20,21] At present, there are a few studies on 3D-printed guide plates applied in atlantoaxial fractures and dislocations; and these studies are mostly in the explorative stage. Hence, there is an urgent need for more clinical cases to verify its safety, feasibility, and effectiveness, especial in our country. Therefore, the study of the clinical application of 3D-printed guide plates for atlantoaxial pedicle screw placement has important clinical significance.
However, there were several limitations about our study: Firstly, patients with irregular vertebral rear bony structures, such as severe bone hyperplasia, the fabrication and installation of the guide plate are difficult. Hence, the use of a 3D-printed guide plate is not suitable for these patients. Secondly, this 3D-printing technology will increase the medical costs of patients to a certain extent. Finally, the sample size in this study is still small, and the study is retrospective in nature. Hence, the credibility of the conclusion may be affected to a certain extent. Thirdly, this was only a retrospective study, not a randomized controlled trial. Fourthly, although we adopted strict inclusions and exclusions, potential sources of bias was unavoidable due to the limitation of the small size.
5. Conclusion
The effectiveness and safety of 3D printed composite guide plate for atlantoaxial pedicle screw were better than traditional method.
Author contributions
Fei Wang substantial contributions to the conception and design of the work; the acquisition, analysis, and interpretation of data for the work; Fei Wang drafting the work and Zhi-Bin Liu, Zhang-Jian Hua, Chang-Hong Li revising it critically for important intellectual content; Xiao-Qian Dang final approval of the version to be published; Yong-Jin He, Jun Liu, Yan-Xiong Liu agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy and integrity of any part of the work are appropriately investigated and resolved.
Conceptualization: Fei Wang.
Data curation: Fei Wang, Zhang-Jian Hua, Chang-Hong Li, Yong-Jin He, Jun Liu, Xiao-Qian Dang.
Formal analysis: Zhang-Jian Hua.
Methodology: Fei Wang, Zhi-Bin Liu, Zhang-Jian Hua, Chang-Hong Li, Yong-Jin He, Jun Liu, Yan-Xiong Liu.
Validation: Zhi-Bin Liu, Chang-Hong Li, Jun Liu, Yan-Xiong Liu.
Writing – original draft: Fei Wang.
Writing – review & editing: Yan-Xiong Liu, Xiao-Qian Dang.
Footnotes
Abbreviations: 3D = 3-dimensional, JOA = Japanese Orthopaedic Association, VAS = visual analog scale.
This study was conducted in accordance with the Declaration of Helsinki. This study was conducted with approval from the Ethics Committee of The Second Affiliated Hospital of Xi’an Jiaotong University. Written informed consent was obtained from all participants.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Angermann CE, Gelbrich G, Störk S, et al. Efficacy and safety of bone marrow-derived cell transplantation for spinal cord injury: a systematic review and meta-analysis of clinical trials. Clin Transplant 2015;29:786–95. [DOI] [PubMed] [Google Scholar]
- [2].Tan MS. Current situation and thinking of surgical treatment to atlantoaxial dislocation. Chin J Orthopaed 2015;35:463–4. [Google Scholar]
- [3].Jiang LH, Tan MS, Dong L, et al. Accuracy assessment of a 3D printed navigational guiding template for atlantoaxial pedicle screw placement. J Spine Surg 2016;14:205–10. [Google Scholar]
- [4].Jiang LH, Tan MS, Yang F, et al. Design and application of 3D printed navigational guiding template in cervical pedicle screw placement. Chin J Orthopaed 2016;36:257–64. [Google Scholar]
- [5].Zhang YZ, Pei GX, Lu S, et al. Establishing lower-extremity mechanical axis by computer-aided design and its application in total knee arthroplasty. Chin J Orthopaed 2013;33:1196–203. [Google Scholar]
- [6].Chen HF, Zhao H, Wang FM, et al. Feasibility study of navigational template for antegrade lag screw fixation of the fractures in the posterior column of acetabulum. Chin J Orthopaed 2013;33:514–9. [Google Scholar]
- [7].Tan MS, Yi P, Wang WJ, et al. Clinical application of pedicle screw instrument in atlas. Chin J Spine Spinal Cord 2015;16:336–40. [Google Scholar]
- [8].Ma XY, Yin QS, Wu ZH, et al. Anatomic evaluation the entry point of C2 pedical screw [in Chinese]. Chin J Surg 2006;44:562–4. [PubMed] [Google Scholar]
- [9].Kawaguchi Y, Nakano M, Yasuda T, et al. Development of a new technique for pedicle screw and Magerl screw insertion using a 3-dimensional image guide. Spine (Phila Pa 1976) 2012;37:1983–8. [DOI] [PubMed] [Google Scholar]
- [10].Jiang L, Dong L, Tan M, et al. Accuracy assessment of atlantoaxial pedicle screws assisted by a novel drill guide template. Arch Orthopaed Trauma Surg 2016;136:1483–90. [DOI] [PubMed] [Google Scholar]
- [11].Hu Y, Yuan ZS, Spiker WR, et al. Deviation analysis of C2 translaminar screw placement assisted by a novel rapid prototyping drill template: a cadaveric study. Eur Spine J 2013;22:2770–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zhou FF, Sun Y, Zhang FS, et al. Prospective study of axial symptoms after anterior cervical discectomy and fusion with plating for cervical spondylotic myelopathy. Chin J Spine Spinal Cord 2014;24:505–9. [Google Scholar]
- [13].YM LI, LI m, Zhang GY, et al. Application of 3D printing in orthopedics of scoliosis. Acad J Second Military Med Univ 2016;37:231–5. [Google Scholar]
- [14].Tan HT, Xie ZL, Jiang JZ, et al. Application of digital navigation template for cervical pedicle screw placement. Chin J Spine Cord 2015;25:497–502. [Google Scholar]
- [15].Pang JY, Zhao Y, Xiao YL, et al. Application of 3D printing technique in spinal surgery. Chin J Tissue Eng Res 2016;20:577–82. [Google Scholar]
- [16].Lu S, Xu YQ, Lu WW, et al. A novel patient-specific navigational template for cervical pedicle screw placement. Spine (Phila Pa 1976) 2009;34:E959–66. [DOI] [PubMed] [Google Scholar]
- [17].Huang X, lI FN, Zhang F, et al. A cadaveric study on establishing individualized navigation templates for axis laminar screw insertion by using a three-dimensional printing forming technique. Chin J Spine Spinal Cord 2014;24:366–71. [Google Scholar]
- [18].Hu Y, Yuan ZS, Kepler CK, et al. Deviation analysis of atlantoaxial pedicle screws assisted by a drill template. Orthopedics 2014;37:e420–7. [DOI] [PubMed] [Google Scholar]
- [19].Hu Y, Yuan ZS, Dong WX, Wang, et al. Safety and accuracy of C1-C2 pedicle screw placement assisted by 3D-printed patient-specific “pointing-drilling” guide template. Chin J Trauma 2016;32:27–34. [Google Scholar]
- [20].Fan Y, Yang C, Yang HJ, et al. Application of 3D printing and intraoperative navigation in surgical treatment for atlantoaxial dislocation. Chin J Orthopaed Trauma 2016;18:29–34. [Google Scholar]
- [21].Kaneyama S, Sugawara T, Sumi M, et al. A novel screw guiding method with a screw guide template system for posterior C-2 fixation: clinical article. J Neurosurg Spine 2014;21:231–8. [DOI] [PubMed] [Google Scholar]


