Abstract
Purpose:
Depression and anxiety are growing global public health issues and affect millions of children and adolescents in the U.S. Although individuals with neurological disorders (NDs) are at increased risk of adverse mental health disorders, they represent a minority of the population. The purpose of this study was to characterize the prevalence of depression and anxiety disorders in children and adolescents by the presence of various NDs.
Methods:
Parent-reported data from the 2016 National Survey of Children’s Health were analyzed in children and adolescents with and without NDs aged 6–17 years.
Results:
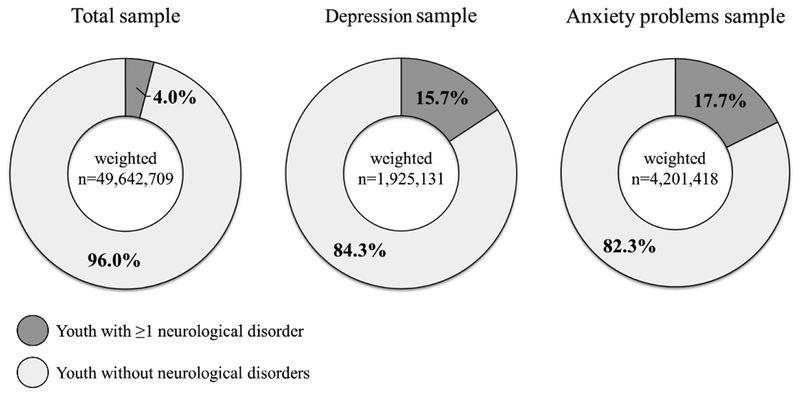
The prevalence of depression and anxiety problems varied by the type of ND (0–18.5% and 2.8–62.5%, respectively). In the combined group of children and adolescents with NDs (weighted estimate: 1,998,654), the prevalence of depression and anxiety problems was 15.3% and 37.9%, respectively, while in children and adolescents without NDs (weighted estimate: 47,644,055), the prevalence was 3.4% and 7.3%, respectively. Children and adolescents with NDs represented 4.0% of the total sample, but 15.7% and 17.7% of the overall sample with depression and anxiety problems, respectively.
Conclusions:
Children and adolescents with NDs contribute to a considerable portion of the overall prevalence of depression and anxiety problems, despite only representing 4% of the population.
Keywords: Neurological disorders, depression, anxiety
Introduction
Mental health disorders are growing global public health issues.1,2 Depression and anxiety disorders are leading contributors to the mental health-related disease2 and economic3 burden, and affect nearly 2 million and 4 million children and adolescents, respectively, in the U.S.1 Depression or anxiety disorders in adolescence are strong predictors of these mental health disorders in adulthood.4 Children and adolescents with neurological disorders (NDs) are at increased risk of depression and anxiety disorders due to a variety of physical and social factors,5–7 which can be inherent to the condition (e.g., communication impairments) or associated with the condition (e.g., participation restriction). The purpose of this study was to characterize the prevalence of depression and anxiety disorders in children and adolescents by the presence of various NDs. Knowing this information would greatly assist public health efforts towards early identification of mental health needs in high-risk subpopulations.
Material and methods
Data were from the 2016 National Survey of Children’s Health (NSCH). The NSCH was developed to produce state- and national-level data (i.e., nationally-representative) on demographic and health characteristics of American children 0–17 years of age, their families, and their communities. The survey utilized a self-administered data collection design using both internet and mailed paper data collection instruments between June 2016 and February 2017. There were >360,000 sampled household addresses that were allocated within states based on the relative household sizes containing at least one child less than 18 years of age, with an oversampling ratio of 5:1 compared to households that had no children. One child per household was selected for the survey. In households that had two or more children, children with special health care needs had a higher probability of being selected (oversampled) to allow for more robust data estimates. A parent or guardian (i.e., respondent) with knowledge of the health status of the surveyed child completed the survey. The completion rate for households that initiated the survey was 69.7%. The 2016 NSCH had an overall weighted response rate of 40.7%. The weighted sample by state ranged from 116,804 (Washington DC) to over 9 million (California). Although response was higher in geographical locations where income was higher, the U.S. Census Bureau conducted a Nonresponse Bias Analysis for the 2016 NSCH and concluded that there was no strong or consistent evidence of nonresponse bias.8 Additional information about the NSCH methodology and instrumentation is available from http://www.childhealthdata.org/.
The respondents were asked, “Has a doctor or other health care provider EVER told you that this child has [specified disorder]?” The child was considered to have a mental health disorder if the respondent reported a current diagnosis of “depression” or “anxiety problems”. The child was considered to have an ND if the respondent reported a current diagnosis of any of the following: (1) autism spectrum disorders; (2) intellectual disability; (3) epilepsy; (4) cerebral palsy; (5) Tourette’s syndrome; and (6) Down syndrome. Children and adolescents without NDs were considered individuals who did not have a current diagnosis of any of the aforementioned NDs. These NDs were chosen based on the availability in the 2016 NSCH, and because their etiology consists of neurodevelopmental causes (e.g., cerebral palsy), or the condition is associated with neurodevelopmental comorbidities (e.g., intellectual disabilities in those with Down syndrome). Since the data used in this investigation are publicly available and de-identified, approval from an Institutional Review Board was not necessary.
The 2016 NSCH uses a complex and multistage survey design to enhance the representativeness of the sample to the U.S. child and adolescent population. We therefore accounted for the primary sampling unit and sampling strata to obtain correct variance estimation, and weighted estimates to account for oversampling, survey nonresponse, and distribution of the target population. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC). Analyses were restricted to children and adolescents aged 6–17 years to address the need for early identification of adverse mental health disorders, and because of the infrequent prevalence of depression and anxiety disorders in children younger than 6 years.2 Less than 1% of the total sample had missing data for depression or anxiety problems. Weighted sample sizes are presented and weighted estimates are presented as median (interquartile range) or percentage (standard error [SE]). The prevalence of depression and anxiety problems among children and adolescents were examined with NDs as a combined subgroup and for each ND group. Prevalence among specific ND groups were calculated for each disorder compared to those without the disorder.
Results
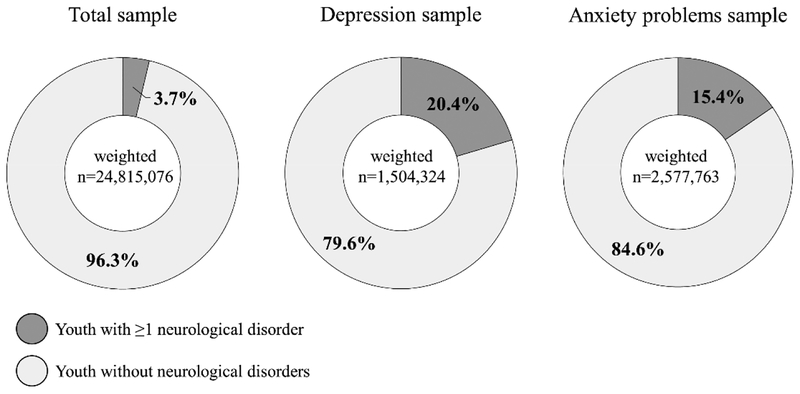
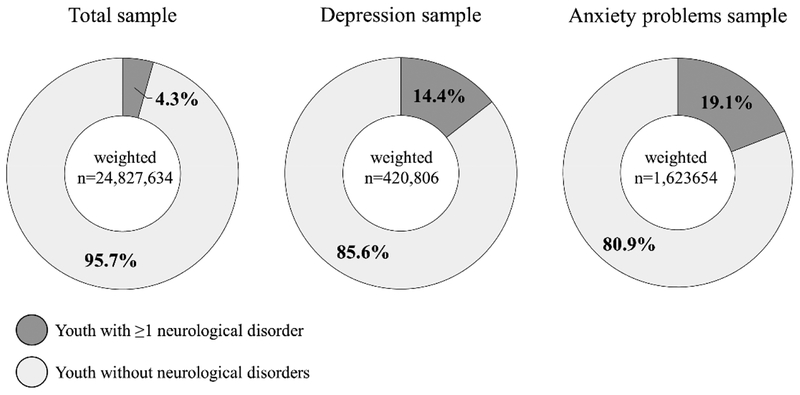
Of the 35,718 (weighted estimate: 49,642,709) individuals aged 6–17 years identified in the 2016 NSCH, 4.0% had at least one of the 6 NDs. The combined group of NDs had a prevalence of 15.3% and 37.9% for depression and anxiety problems, respectively, while individuals without NDs had a prevalence of 3.4% and 7.3%, respectively (Table 1). Of the children and adolescents with depression (weighted estimate: 1,925,131) or anxiety problems (weighted estimate: 4,201,418), children and adolescents with NDs represented 15.7% and 17.7%, respectively (Figure 1). Similar results were observed when stratified by age (figures in Appendix A, 6–11 years, and Appendix B, 12–17 years).
Table 1.
Parent-report descriptive characteristics of children aged 6–17 years by group of NDs
| Children without NDs | Children with NDs | Specific groups of NDs | ||||||
|---|---|---|---|---|---|---|---|---|
| Autism spectrum disorders | Intellectual disability | Epilepsy | Cerebral palsy | Tourette’s syndrome | Down syndrome | |||
| Sample size | ||||||||
| Unweighted | 34,161 | 1,557 | 1,008 | 423 | 261 | 111 | 104 | 68 |
| Weighted | 47,644,055 | 1,998,654 | 1,293,878 | 576,666 | 303,567 | 145,628 | 149,879 | 75,906 |
| Age | ||||||||
| Median | 11.0 | 11.5 | 11.1 | 12.6 | 11.6 | 12.2 | 13.5 | 10.2 |
| IQR | 8.0–14.0 | 8.0–14.0 | 7.7–13.7 | 9.0–14.4 | 8.0–14.2 | 8.2–14.6 | 11.0–15.4 | 8.7–12.8 |
| Male, % (SE) | 50.2 (0.6) | 72.0 (2.5) | 82.6 (2.2) | 63.3 (5.9) | 46.1 (5.8) | 62.8 (8.3) | 79.2 (6.5) | 72.4 (7.8) |
| Race, % (SE) | ||||||||
| Hispanic | 25.4 (0.7) | 22.1 (3.0) | 19.9 (3.3) | 26.2 (6.6) | 18.0 (5.5) | 10.8 (5.6) | 25.8 (10.3) | 18.0 (9.2) |
| Non-Hispanic White | 51.3 (0.6) | 54.7 (2.7) | 57.1 (3.2) | 48.1 (5.4) | 55.1 (6.0) | 60.7 (9.6) | 66.2 (9.6) | 61.6 (10.1) |
| Non-Hispanic Black | 13.1 (0.5) | 14.8 (1.9) | 14.6 (2.4) | 19.6 (4.2) | 12.3 (3.6) | 27.1 (9.6) | 5.3 (3.4) | 6.5 (4.6) |
| Other | 10.2 (0.3) | 8.4 (1.1) | 8.4 (1.2) | 6.1 (1.3) | 14.6 (4.3) | 1.4 (0.6) | 2.7 (1.3) | 13.9 (5.8) |
| *Poverty, % (SE) | ||||||||
| 0–199% | 44.3 (0.7) | 50.9 (2.6) | 50.2 (3.2) | 53.6 (5.5) | 50.4 (5.8) | 50.6 (9.2) | 40.7 (9.6) | 58.8 (10.5) |
| 200–399% | 26.0 (0.5) | 23.9 (2.2) | 23.7 (2.3) | 25.0 (5.4) | 18.6 (3.4) | 22.8 (6.1) | 25.7 (6.7) | 15.2 (5.3) |
| ≥400% | 29.7 (0.5) | 25.2 (2.0) | 26.1 (2.4) | 21.4 (3.9) | 31.0 (5.4) | 26.6 (8.5) | 33.6 (8.1) | 26.0 (10.8) |
| Depression, % (SE) | 3.4 (0.2) | 15.3 (1.9) | 18.5 (2.7) | 15.3 (3.2) | 10.2 (2.8) | 7.8 (3.5) | 11.3 (5.1) | 0 (0) |
| Anxiety problems, % (SE) | 7.3 (0.3) | 37.9 (2.5) | 44.7 (3.2) | 33.9 (4.7) | 33.2 (5.7) | 30.1 (9.1) | 62.5 (8.1) | 2.8 (1.9) |
NDs, neurological disorders; IQR, interquartile range; SE, standard error. Weighted values are presented.
Poverty as a ratio of the federal poverty line.
Figure 1.
Total, depression, and anxiety problems sample prevalence in children and adolescents with and without neurological disorders. Figure represents the distribution of children and adolescents with and without neurological disorders among the total sample (weighted estimate: 49,642,709) and among the sample of children and adolescents with depression (weighted estimate: 1,925,131) or anxiety problems (weighted estimate: 4,201,418).
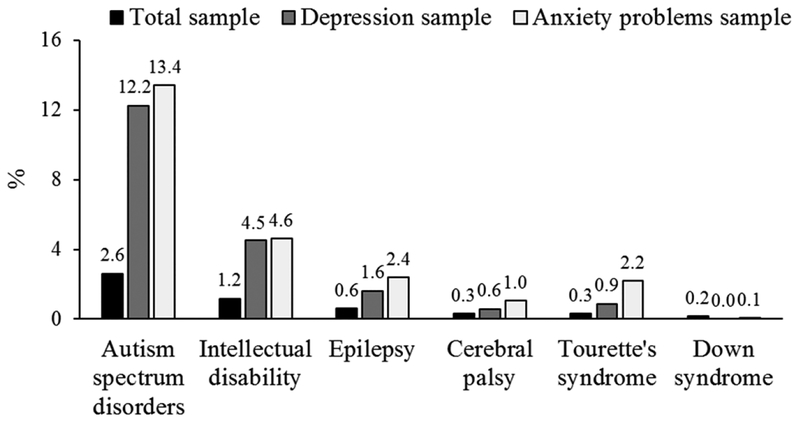
The prevalence of depression and anxiety problems varied by the type of ND (Table 1). Depression prevalence ranged from 0% to 18.5% among individuals with Down syndrome and autism spectrum disorders, respectively. Anxiety problems prevalence ranged from 2.8% to 62.5% among individuals with Down syndrome and Tourette’s syndrome, respectively. Figure 2 highlights the prevalence of specific NDs among the total sample and among the samples of children and adolescents with depression or anxiety problems.
Figure 2.
Total, depression, and anxiety problems sample prevalence in children and adolescents by specific neurological disorders. Bar graphs represent the prevalence of specific neurological disorders among the total sample (weighted estimate: 49,642,709) and among the sample of children and adolescents with depression (weighted estimate: 1,925,131) or anxiety problems (weighted estimate: 4,201,418). Prevalence among specific neurological disorders were calculated for each disorder compared to those without the disorder.
Discussion
The key finding of this investigation was that in a nationally-representative sample, children and adolescents with NDs contribute to a considerable portion of the overall prevalence of depression and anxiety problems, despite only representing 4% of the population. This pattern was consistent across all ND groups, except for Down syndrome. For example, youth with intellectual disabilities represented 1.2% of the total sample, but represented 4.5% of the overall prevalence of depression and 4.6% of the overall prevalence of anxiety problems.
Adverse mental health profiles differ based on ND-characteristics.9 Identifying these burdens in subpopulations at increased risk may facilitate targeted prevention and intervention efforts through partnerships among agencies that serve ND populations to address the growing burden of mental health disorders.1,2 In the current investigation, parent-reported prevalence of depression and anxiety problems varied considerably as a function of ND diagnosis. Moreover, the prevalence of anxiety problems was approximately 2 times higher than that of depression for individuals without NDs and was 2–6 times higher for ND groups, except for Down syndrome. The higher prevalence of anxiety problems relative to depression is consistent with previous reports in children and adolescents1,10 and may reflect developmental trends in prevalence of psychiatric diagnoses. While prevalence of anxiety disorders increases with age, rates of depression are greater than anxiety by late adolescence11 and early adulthood,2 which may explain the higher prevalence of anxiety overall in the current investigation. Importantly, depression or anxiety in adolescence is a strong predictor of these mental health disorders in adulthood.4,12
Children and adolescents with NDs frequently utilize a variety of healthcare services as a routine part of their condition-specific clinical care. Therefore, pediatric clinical settings treating those with NDs offer a promising venue to focus public health strategies including mental health screening. Increasing clinician awareness of mental health risks among children and adolescents with NDs, efficient screening strategies, and adequate referral resources for mental health care services could substantially reduce disease burden in this subpopulation.
In the current investigation, individuals with non-neurologically derived disabilities were included in the group of children without NDs. These groups of children and adolescents have increased risk of mental health disorders.13 Pediatric clinics treating those with NDs typically see children and adolescents with non-ND related complications. Therefore, public health initiatives targeting these clinics may reach a broader portion of the subpopulations contributing to the depression and anxiety burden among children and adolescents.
This study has several limitations. First, the presence of depression, anxiety problems, and NDs were based on parent report and may be subject to bias or misreporting. Second, the definitions of depression and anxiety problems were broad. There can be a conflation of the emotions depression and anxiety and the clinical diagnosis of these disorders. Third, discerning disorders by neurological or non-neurological roots using the 2016 NSCH survey was not possible for many groups that can have multiple causes, such as headaches/migraines, developmental delay, attention-deficit hyperactivity disorder, etc. These groups were included in the group of children and adolescents without NDs. Therefore, the results presented here are likely underreporting the extent that NDs contribute to the national mental health-related prevalence in children and adolescents. Finally, there is risk for over-interpretation of these results due to the small sample size for some of the specific ND groups. Further, the sex distribution of Down syndrome is more male dominant in the 2016 NSCH than what is expected from the population. However, the overall prevalence for the ND groups are similar to U.S. population-based estimates.
Conclusions
Study findings suggest that children and adolescents with NDs represent a considerable portion of the national prevalence of depression and anxiety problems. Within a pediatric clinical setting, routine screening, increased awareness and knowledge, and adequate resources to treat mental health disorders could be an avenue that leads to significant benefits in the national mental health-related burden among children and adolescents.
Acknowledgements and funding
Dr. Whitney is supported by the University of Michigan Advanced Rehabilitation Research Training Program in Community Living and Participation from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) [90AR5020–0200]. Dr. Peterson is funded by the National Institutes of Health (NIH) [1KO1 HD074706] and NIDILRR [90IF0102–01]. Dr. Warschausky is funded by the NIH [5 UL1 TR002240–05], the Cerebral Palsy Alliance, and the Mildred E. Swanson Foundation. The funding sources had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
List of abbreviations:
- ND
neurological disorder
- NSCH
National Survey of Children’s Health
- IQR
interquartile range
- SE
standard error
Appendix A
Fig. A.1.
Total, depression, and anxiety problems sample prevalence in children and adolescents with and without neurological disorders aged 6–11 years. Figure represents the distribution of children and adolescents with and without neurological disorders among the total sample and among the sample of children and adolescents with depression or anxiety problems.
Appendix B
Fig. B.1.
Total, depression, and anxiety problems sample prevalence in children and adolescents with and without neurological disorders aged 12–17 years. Figure represents the distribution of children and adolescents with and without neurological disorders among the total sample and among the sample of children and adolescents with depression or anxiety problems.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Global Burden of Disease Pediatrics C, Kyu HH, Pinho C, et al. Global and National Burden of Diseases and Injuries Among Children and Adolescents Between 1990 and 2013: Findings From the Global Burden of Disease 2013 Study. JAMA Pediatr. 2016;170(3):267-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197-2223. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden of generalized anxiety disorder. Depress Anxiety. 2008;25(1):72-90. [DOI] [PubMed] [Google Scholar]
- 4.Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55(1):56-64. [DOI] [PubMed] [Google Scholar]
- 5.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921-929. [DOI] [PubMed] [Google Scholar]
- 6.Downs J, Blackmore AM, Epstein A, et al. The prevalence of mental health disorders and symptoms in children and adolescents with cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2018;60(1):30-38. [DOI] [PubMed] [Google Scholar]
- 7.Green SA, Berkovits LD, Baker BL. Symptoms and development of anxiety in children with or without intellectual disability. J Clin Child Adolesc Psychol. 2015;44(1):137-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.2016 National Survey of Children’s Health Nonresponse Bias Analysis. 2017; https://census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/nonresponse-bias-analysis/NSCH%202016%20Nonresponse%20Bias%20Analysis.pdf. Accessed 03/30/2018, 2018.
- 9.Boland MC, Daly L, Staines A. Self-rated health and quality of life in adults attending regional disability services in Ireland. Disabil Health J. 2009;2(2):95-103. [DOI] [PubMed] [Google Scholar]
- 10.Petresco S, Anselmi L, Santos IS, et al. Prevalence and comorbidity of psychiatric disorders among 6-year-old children: 2004 Pelotas Birth Cohort. Soc Psychiatry Psychiatr Epidemiol. 2014;49(6):975-983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobson NC, Newman MG. Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychol Bull. 2017;143(11):1155-1200. [DOI] [PubMed] [Google Scholar]
- 13.Suryavanshi MS, Yang Y. Clinical and Economic Burden of Mental Disorders Among Children With Chronic Physical Conditions, United States, 2008–2013. Prev Chronic Dis. 2016;13:E71. [DOI] [PMC free article] [PubMed] [Google Scholar]