Abstract
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by the presence of autoantibodies against nucleic acids and nucleoproteins. Anti-dsDNA Abs are considered a hallmark of SLE and previous studies have indicated that nucleic acid-containing immune complexes (ICs) induce B cell and dendritic cell activation in a TLR-dependent process. How ICs containing nucleic acids affect neutrophil function has not been well investigated. Here we report that nucleic acid-containing ICs derived from the sera of SLE patients induce human and mouse neutrophil activation through TLR-independent mechanisms. Soluble ICs containing Sm/RNP, an RNA antigen, activate human neutrophils to produce reactive oxygen species (ROS) and IL-8. In contrast, ICs containing DNA have to be immobilized to efficiently activate neutrophils. We found that deleting TLR7 or TLR9, the receptors for RNA and DNA, had no effect on mouse neutrophil activation induced by RNA-containing and immobilized DNA-containing ICs. Binding of ICs are mediated through Fc γ receptor IIA (FcγRIIA) and FcγRIIIB. However, neutrophil activation induced by RNA- and DNA-containing ICs requires FcγRIIA, as blocking FcγRIIA inhibited ROS release from neutrophils. RNA-containing ICs induce calcium flux whereas TLR7/8 ligand R848 do not. Surprisingly chloroquine inhibits calcium flux induced by RNA-containing ICs, suggesting that this lesser known function of chloroquine is involved in the neutrophil activation induced by ICs. These data indicate the SLE-derived ICs activate neutrophils to release ROS and chemokines in an FcγRIIA-dependent, TLR7- and TLR9-independent manner that likely contributes to local tissue inflammation and damage.
Introduction
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease, which damages almost every organ system (1, 2). Lupus patients have autoantibodies against nucleic acids and proteins (3). Approximately half of SLE patients develop lupus nephritis, which correlates with the presence of anti-DNA Abs (4). Human Toll-like receptor-7 (TLR7) and TLR8 recognize RNA and TLR9 recognizes DNA (5). These TLRs activate B cells, dendritic cells and macrophages to induce antigen presentation, antibody production, and inflammatory cytokine production. Studies have shown that deletion of TLR7 or the downstream adaptor MyD88 markedly ameliorates SLE in lupus-prone mice, suggesting the importance of nucleic acids and nucleic acid-sensing receptors in this disease (6-10). We have previously shown that RNA-containing immune complexes stimulate mouse plasmacytoid dendritic cells to release type I interferon (IFN) and IL-6 by dual engagement of FcγR and TLR7 that subsequently leads to interferon regulatory factor-5 (IRF5) signaling (11).
Neutrophils are the most abundant immune cell type in peripheral blood (12). They appear to be inappropriately activated in SLE patients and a ‘Neutrophil signature” has been described that correlates with disease activity and the occurrence of lupus nephritis (13-15). Recent studies have shown that ICs containing ribonucleoproteins (RNP) activate neutrophils to release neutrophil extracellular traps (NETs) through TLR7-dependent signaling and reactive oxygen species (ROS) production, and that DNA in NETs forms ICs with anti-DNA Abs to produce a type I IFN response in plasmacytoid dendritic cells (16-18). Although human neutrophils have been reported to express TLR7, TLR8 and TLR9 (19, 20), whether DNA-containing ICs stimulate neutrophils and whether TLR receptors are required for the neutrophil activation has not been investigated.
In this study, we investigate how nucleic acid-containing ICs activate neutrophils to induce ROS and chemokines. Soluble RNA-containing ICs activate neutrophils to induce ROS and IL-8. Interestingly, DNA-containing ICs that are immobilized provide a strong activation signal in neutrophils while soluble DNA-containing ICs fail to activate the cells. In addition, the activation induced by RNA-containing ICs and immobilized DNA-containing ICs is TLR-independent because these ICs efficiently activate TLR9−/− neutrophils and TLR7−/− neutrophils. Both DNA- and RNA- containing ICs require FcγRIIA engagement. Taken together, these results define the mechanisms of neutrophil activation in the pathogenesis of SLE.
Materials and Methods
Human subjects
Blood from lupus patients was obtained under the protocols: Autoimmune Kidney Research Studies and Patient Registry and the Autoimmune Kidney Research Repository approved by the Boston University Medical Center Institutional Review Board. All samples used in these studies were from lupus patients that fulfilled at least 4 of the 11 American College of Rheumatology revised criteria for the classification of SLE (21). Patients with nephritis had biopsy-proven nephritis; lupus nephritis was classified according to the World Health Organization classification and the revisions suggested by the International Society of Nephrology and the Renal Pathology Society (22).
Animals
TLR7−/− mice and TLR9−/− mice were provided by Dr. Shizuo Akira (Osaka University, Osaka, Japan) and were backcrossed at least 12 generations to C57BL/6 background. All mice were maintained at the Boston University Laboratory Animal Sciences Center in accordance with the American Association for the Accreditation of Laboratory Animal Care regulations. All experiments were approved by the Institutional Animal Care and Use Committee at Boston University.
Autoantibody ELISA
Levels of anti-dsDNA Ab and anti-Sm/RNP Ab in sera of SLE patients and healthy subjects were measured using in-house ELISAs. For anti-Sm/RNP Ab, ELISA plates (MaxiSorp, NUNC) were coated with Sm/RNP (Arotec Diagnostic) in PBS overnight. The plates were washed and blocked with PBS containing 1% bovine serum albumin (Fraction V, Fisher Scientific) and 5% milk (Santa Cruz Biotechnologies), and serum were diluted with 1% BSA/5% milk/PBS at the concentration of 1/1000. SLE1 serum was used as a standard for the ELISA. Goat Anti-Human Ig-HRP (Southern Biotech) was diluted into 1% BSA/5% milk/PBS at the concentration of 1/20000. The detection limit of anti-Sm/RNP Ab were 0.1% of SLE1 serum. For double-stranded DNA Ab, ELISA plates were coated with calf thymus DNA (Sigma), which was treated with phenol/chloroform/isoamyl alcohol (25/24/1) extraction followed by a Triton X-114 purification to remove LPS contamination, as described previously (23). Serum was diluted with 1%BSA/5% milk/PBS at the concentration of 1/200. SLE9 serum, which contains anti-dsDNA Ab, was used as a standard of the ELISA (Table 1). Following steps were similar to that described for the anti-Sm/RNP Ab ELISA.
Table 1.
Sera reactivity and types of nephritis of lupus patients in this study.
| Patients | Anti- nuclear Ab Titer |
Autoantibody Reactivity | Nephritis | |||
|---|---|---|---|---|---|---|
| Sm | RNP | dsDNAa | ||||
| Crithidia Assay | ELISA (IU/ml) | |||||
| SLE1 | 1/2560 | +++ | ++++ | ND | 378 | Class IV |
| SLE9 | 1/2560 | − | − | ND | 10701 | Class III, V |
| SLE12 | 1/1280 | + | + | 1/10 | ND | Collapsing GN |
| SLE13 | 1/320 | ND | ND | − | − | Class IV |
| SLE14 | 1/1280 | + | + | 1/320 | ND | Class V |
| SLE15 | 1/640 | ND | ND | − | − | Class IV |
| SLE16 | 1/1280 | ND | ND | 1/80 | ND | − |
| SLE17 | ND | ND | ND | 1/40 | ND | − |
| SLE18 | − | − | − | − | − | Class V |
| SLE19 | − | − | − | − | − | Class V |
| Ctrl1 | ND | ND | ND | ND | ND | − |
for Abs against dsDNA, values > 5 IU/ml are considered positive. ND; not determined.
Human neutrophil purification.
Human neutrophils were purified from fresh blood of SLE patients using the method described previously (24). In brief, after PBMC isolation by Ficoll-Paque centrifugation, the neutrophils were isolated using dextran sedimentation following red blood cell lysis. Human granulocytes were stained with anti-CD66b FITC (clone G10F5, BioLegend), anti-FcγRIII PE or anti-FcγRIII PerCPCy5.5 (CD16, clone 3G8, BD Bioscience and BioLegend), anti-Siglec-8 PE-Cy7 (clone 7C9, BioLegend), anti-FcγRIIA FITC (CD32a, clone IV.3, Stem Cell Technology) and anti-FcγRI BV421 (CD64, clone 10.1, BioLegend). The cells were detected by a LSRII flow cytometer (BD Bioscience) and analyzed with FlowJo (Tree Star). The purity of neutrophils was determined as described in Fig. 1.
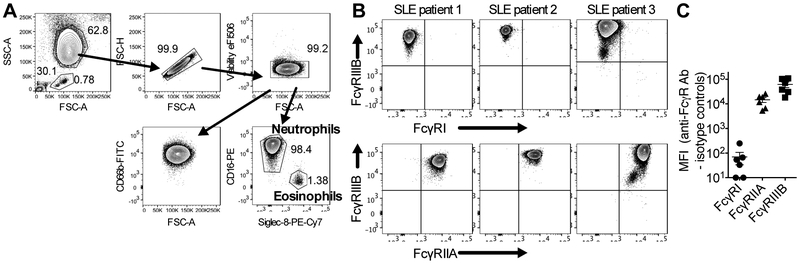
Figure 1. FcγR expression on human neutrophils.
A. Purity of neutrophils was determined by flow cytometry. Neutrophils were side scatter high, CD66+ CD16+ Siglec-8-. B. Fc γ receptor expression on neutrophils from 3 different SLE patients were determined by flow cytometry. C. FcγRI, FcγRIIA and FcγRIIIB expression on neutrophils from 6 lupus patients were shown. Data are shown as mean fluorescence intensity of anti-FcγR Ab minus mean fluorescence intensity of their isotype controls.
Mouse neutrophils isolation.
Bone marrow cells were isolated from wild type mice, TLR7−/− mice and TLR9−/− mice. PE-conjugated anti-Ly6G antibody (clone 1A8, BD Biosciences) was added to the bone marrow cells. Ly6G+ neutrophils were isolated using anti-PE magnetic particles (BD Bioscience). Ly6G+ neutrophils, which were already stained with anti-Ly6G-PE, were detected by the LSRII flow cytometer (BD Bioscience) or a FASCalibur (BD Bioscience) and analyzed with FlowJo (Tree Star). The purity of Ly6G+ neutrophils was more than 95 %.
Neutrophil activation.
NUNC Maxisorp plates (ThermoFisher Scientific) were coated with or without DNA for 2 hours in PBS. Sm/RNP was obtained from Arotec Diagnostic (New Zealand). TLR ligands were obtained from InVivoGen. PMA was obtained from Sigma. The generation of H2O2 was measured using the Amplex Red hydrogen peroxide/peroxidase assay kit (ThermoFisher Scientific), as previously described with slight modification (25). In brief, 1 × 105 cells were incubated with TLR ligands or immune complexes in presence of the solution which contains 50 μM Amplex Red reagent and 10 U/ml horseradish peroxidase in 1% FBS/HBSS. After a 1-hour incubation, the fluorescence intensity of Amplex Red was measured by an Infinite 200 Pro microplate reader (Tecan) excitation at 560 nm and emission at 590 nm. The H2O2 concentration was determined using an H2O2 standard curve. The detection limit of this assay was 0.625 μM of H2O2. In some experiments, anti-FcγRIIA Ab (CD32A, clone IV.3, Stem Cell Technology), anti-FcγRIII Ab (CD16, clone 3G8, BioLegend), inhibitory CpG sODN 2088 (Coley Pharmaceutical Group), inhibitory INH-18 sODN (26), and chloroquine (Sigma Aldrich) were added to the culture before the addition of the ICs.
For the measurement of chemokines, neutrophils were stimulated with TLR ligands or immune complexes for 24 hours in RPMI 1640 supplemented with fetal bovine serum (final 10%) and penicillin-streptomycin. IL-8 levels in the supernatant of human neutrophils were measured by the Human IL-8 ELISA Ready-Set-Go kit (eBioscience). MIP-1α levels in the supernatant of mouse neutrophils were measured by MIP-1α DuoSet ELISA (R&D Systems).
Calcium flux.
Neutrophils from lupus patients were stained with Fluo-4 AM (ThermoFisher Scientific) in PBS at the concentration of 1 μM. The neutrophils were washed with PBS and resuspended to RPMI1640 supplemented with 10% FBS and penicillin-streptomycin. The cells were incubated with chloroquine (20 μg/ml) for 30 min. The cells were stimulated with IC, TLR ligands, PMA or ionomycin. Increased levels of calcium flux were determined by flow cytometry.
Binding and uptake of immune complexes.
IgG from a lupus patient (SLE1) was purified with Protein G Sepharose 4 Fast flow (GE Healthcare). The purified IgG were labeled with Alexa Flour 647 Antibody Labeling Kit (ThermoFisher Scientific). The Alexa-647 labeled IgG were mixed with Sm/RNP to generate RNA-containing ICs. Neutrophils were treated with anti-FcγRIIA Ab, anti-FcγRIII Ab or chloroquine for 15 min and the ICs were added to the cells in RPMI1640 supplemented with 10% FBS and penicillin-streptomycin. After a 1-hour incubation at 4°C and 37°C, the cells were washed twice with ice-cold PBS supplemented with 3% FBS and 2mM EDTA. The cells were fixed with 2% formaldehyde in PBS. The binding and/uptake of Alexa647-labeled ICs were analyzed with flow cytometry.
Statistics.
Wilcoxon matched-pairs test was used for statistical analysis in Figure 5B&C and 6. Mann-Whitney U test or one-way ANOVA on ranks were used for other statistical analysis. All statistics were performed using GraphPad Prism with p<0.05 considered as statistically significant.
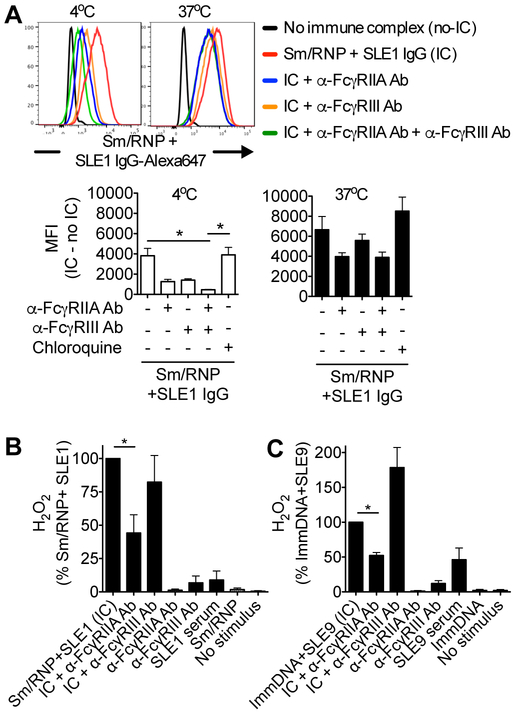
Figure 5. ICs bind to both FcγRIIA and FcγRIIIB, but the activation induced by the ICs is dependent on FcγRIIA on neutrophils.
A. Purified IgG from SLE1 patient was labeled with Alexa647 and combined with Sm/RNP to generate Sm/RNP-containing ICs. Neutrophils from lupus patients were pretreated with blocking Abs against FcγRIIA (clone IV.3) and FcγRIII (clone 3G8) and chloroquine, and incubated with Alexa647-labeled Sm/RNP-containing IC for 1 hr at 4°C and 37°C. The extent of Alexa647-labeled IC binding or internalization to neutrophils was determined by flow cytometry. The data were shown as mean fluorescence intensity (MFI) of Alexa647-labeled ICs minus MFI of no IC. The data represent the mean +/− SEM of 7 different experiments. One-way ANOVA on ranks was used. * P<0.05. B. Neutrophils from lupus patients were stimulated with Sm/RNP-containing ICs in the presence of blocking Abs against FcγRIIA (clone IV.3) and FcγRIII (clone 3G8). H2O2 production was measured after 1-hour incubation. The data were normalized by the levels of H2O2 induced by ICs without blocking Abs. The data represent the mean +/− SEM of 6 independent experiments. C. Neutrophils from lupus patients were stimulated with immobilized DNA-containing ICs in the presence of blocking Abs against FcγRIIA and FcγRIII. H2O2 production was measured after 1-hour incubation. The data were normalized by the levels of H2O2 induced by ICs without blocking Abs. The data represent the mean +/− SEM of 7 independent experiments. In B and C, Wilcoxon matched-pairs test was used for statistical analysis between ICs and ICs + anti-FcγRIIA antibody. * P<0.05.
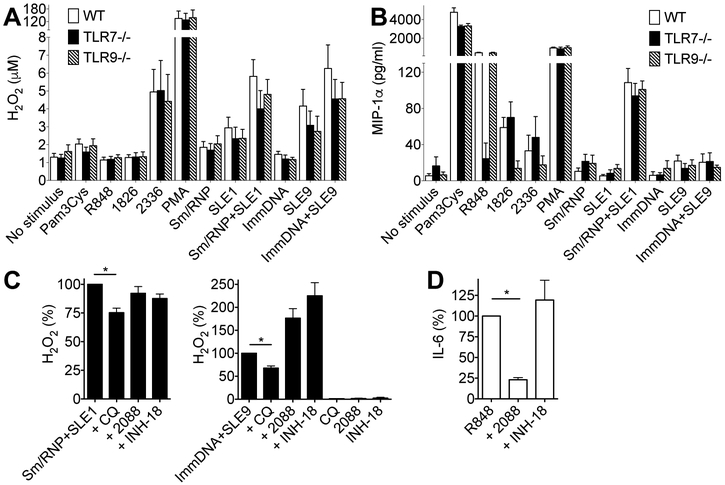
Figure 6. RNA-containing ICs and immobilized DNA-containing ICs induce TLR-independent neutrophil activation.
A. Ly6G+ neutrophils from wild type mice, TLR7−/− mice and TLR9−/− mice were stimulated with RNA-containing ICs (Sm/RNP + SLE1 serum), immobilized DNA-containing ICs (ImmDNA+SLE9 serum), TLR ligands and PMA for 1 hour. H2O2 production was measured by Amplex Red. The data represent the mean +/− SEM of 5-7 independent experiments. B. Ly6G+ neutrophils from wild type mice, TLR7−/− mice and TLR9−/− mice were stimulated with RNA-containing ICs (Sm/RNP + SLE1 serum), immobilized DNA-containing ICs (ImmDNA+SLE9 serum), TLR ligands and PMA for 24 hours. IL-8 production was measured by ELISA. The data represent the mean +/− SEM of 4-5 independent experiments. C. Neutrophils from lupus patients were stimulated with RNA-containing immune complexes and immobilized DNA-containing immune complexes in the presence of chloroquine (CQ, 20 μg/ml) and inhibitory oligonucleotides 2088 (1 μg/ml) and INH-18 (1 μg/ml) for 1 hour. H2O2 levels were determined by Amplex Red. The data represent the mean +/− SEM of 6 independent experiments. Wilcoxon matched-pairs test was used for statistical analysis between immune complexes and immune complexes + Chloroquine. * P<0.05. D. PBMC from lupus patients were stimulated with R848 (TLR7/8 ligand) in the presence or absence of inhibitory oligonucleotides 2088 (1 μg/ml) and INH-18 (1 μg/ml) for 24 hours. IL-6 levels in the supernatant were measured by ELISA. The data represent the mean +/− SEM of 4 independent experiments. Wilcoxon matched-pairs test was used for statistical analysis between R848 and R848 + 2088. * P<0.05.
Results
Neutrophils from lupus patients express Fc γ receptors.
We purified neutrophils from lupus patients. Isolated neutrophils were of high purity and contained > 95% neutrophils and 1-2 % of eosinophils (Fig. 1A). It was previously shown that low-affinity Fc γ receptors (FcγRIIA, FcγRIIB and FcγRIII) are responsible for the IC-mediated uptake, and the balance of activating FcγRs (FcγRIIA and FcγRIII) and inhibitory FcγRIIB controls the activation of immune cells (27, 28). Neutrophils from lupus patients expressed FcγRIIA (CD32a) and high levels of FcγRIIIB (CD16), but not FcγRI (CD64) (Fig. 1B). All neutrophils from SLE patients express substantial levels of FcγRIIA and FcγRIIIB, although there is a slight difference of FcγR expressions between SLE patients (Fig. 1C).
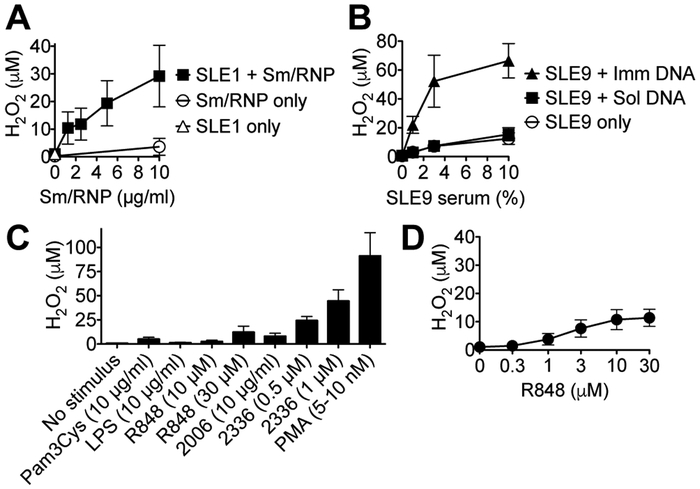
ICs activate neutrophils from lupus patients.
Previously, we have shown that an SLE patient’s serum (SLE1), which contain anti-Sm Ab and anti-ribonucleoprotein (RNP) Ab (Table 1), activates mouse plasmacytoid dendritic cells to induce type I IFN through Fc γ receptor and TLR7 signaling (11). RNA-containing ICs made by Sm/RNP antigen and SLE1 serum activated PBMC to induce type I IFN (29). We used a similar approach to stimulate neutrophils from lupus patients with Sm/RNP-containing ICs (Fig. 2A). Neutrophils from lupus patients released reactive oxygen species (ROS) in response to the Sm/RNP-containing ICs. In contrast, neither SLE1 serum nor Sm/RNP antigen alone induced H2O2. These results are consistent with the previous studies, showing that anti-RNP Abs from SLE patients activate neutrophils to produce ROS (16, 17).
Figure 2. Soluble RNA-containing ICs and immobilized DNA-containing ICs activate neutrophils from lupus patients.
A. Neutrophils from lupus patients were stimulated with SLE1 serum, Sm/RNP, SLE1+ Sm/RNP for 1 hour. The levels of H2O2 in the supernatant were determined. The data represent the mean +/− SEM of 3 independent experiments. B. Neutrophils from lupus patients were stimulated with SLE9 serum, SLR9 serum+ soluble DNA (SLE9+SolDNA), SLE9 serum + immobilized DNA (SLE9+ImmDNA) for 1 hour. The levels of H2O2 in the supernatant was measured by Amplex Red. The data represent the mean +/− SEM of 3 independent experiments. C. Neutrophils from lupus patients were stimulated with Pam3CyS (a TLR2 ligand), LPS (a TLR4 ligand), R848 (a TLR7/8 ligand), 2006 (CpG-B, a TLR9 ligand), 2336 (CpG-A, a TLR9 ligand) and PMA (a Protein kinase C ligand). One hour later, the levels of H2O2 in the supernatant was measured by Amplex Red. The data represent the mean +/− SEM of 5-16 experiments. D. Neutrophils from lupus patients were stimulated with R848 for 1 hour. The levels of H2O2 in the supernatant was measured by Amplex Red. The data represent the mean +/− SEM of 4 experiments.
Anti-DNA Abs are a hallmark of SLE, and the presence of serum anti-DNA Abs is associated with lupus nephritis (4, 30, 31). However, studies describing the activation induced by DNA-containing ICs are rather limited in plasmacytoid dendritic cells and B cells (32-37). There is no study describing whether DNA-containing ICs induce neutrophil activation, despite the fact that human neutrophils express TLR9, a DNA receptor (19, 20). To investigate this possibility, we generated DNA-containing ICs by mixing DNA and SLE9 serum which has high levels of anti-dsDNA Ab (Table 1). Soluble DNA-containing ICs and SLE9 serum only activated neutrophils to release very low levels of H2O2 (Fig. 2B), suggesting that soluble DNA-containing ICs are unable to stimulate neutrophils. Immobilized ICs have been shown to activate neutrophils effectively (38-40). To investigate the possibility, we coated plates with DNA, and added SLE9 serum to generate immobilized DNA-containing ICs. After an incubation with immobilized DNA-containing ICs, lupus neutrophils release large amount of H2O2 (Fig. 2B). These results indicate that DNA-containing ICs are able to trigger neutrophil response, but only if the DNA is immobilized.
It has been shown that TLR ligands induce reactive oxygen species (ROS) from neutrophils, and ROS triggers neutrophil extracellular traps (NETs) and FcγRIIA shedding (41, 42). We stimulated neutrophils from lupus patients with TLR ligands and measured ROS production (Fig. 2C&D). Interestingly, the ligands for TLR2 (Pam3CyS), TLR4 (LPS) and TLR9 (CpG-B, 2006) did not induce large amount of H2O2 from neutrophils from lupus patients. The TLR7/8 ligand (R848) required high concentrations to induce H2O2, whereas the TLR9 ligand (CpG-A, 2336) induced relatively high amount of H2O2. Phorbol 12-myristate 13-acetate (PMA), a protein kinase C (PKC) activator, induced high levels of H2O2 from neutrophils of lupus patients. These results suggest that soluble-RNA-containing immune complexes and immobilized DNA-containing immune complex are able to induce high levels of ROS from neutrophils of lupus patients, whereas synthetic TLR ligands, with the exception of CpG-A 2336, induce low levels of ROS.
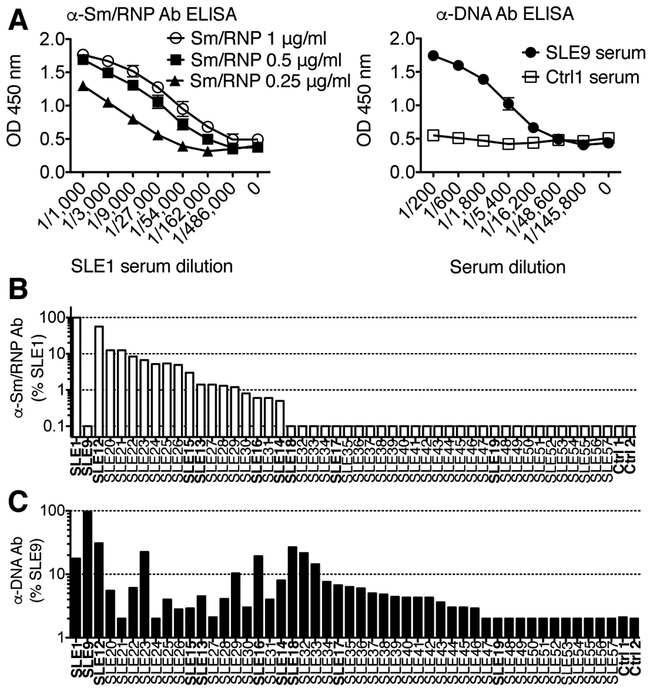
Determination of levels of anti-Sm/RNP Ab and anti-DNA Ab in sera from lupus patients.
To investigate whether sera from other SLE patients have similar capacities to induce neutrophil activation, we first determined the levels of autoantibodies in their sera by using an in-house ELISA for anti-Sm/RNP Abs and anti-DNA Abs. SLE1 serum contain high levels of anti-Sm/RNP Abs and SLE9 serum contains high levels of anti-double DNA Abs (Table 1)(11). Thus, we used SLE1 serum for a positive control of anti-Sm/RNP Ab ELISA and SLE9 serum for a positive control of anti-DNA Ab ELISA (Fig. 3A). Autoantibody levels of 38 out of 193 serum samples from lupus patients and two control sera are shown in Figure 3B&C. Approximately 32.3% of samples were anti-Sm/RNP Ab positive and 42.5% of samples were anti-DNA Ab positive (data not shown).
Figure 3. Levels of anti-Sm/RNP Ab and anti-DNA Ab in lupus patient sera.
A. ELISA plates were coated with different concentrations of Sm/RNP, and serial dilutions of SLE1 serum were added to the plate. Antibody levels were detected with anti-human IgG-HRP. Similarly, ELISA plates were coated with DNA (5 μg/ml), and serial dilutions of SLE9 serum or control serum (Ctrl serum) were added to the plate. Antibody levels were detected with anti-human IgG-HRP. B. Levels of anti-Sm/RNP Ab in 38 lupus sera and 2 control sera were detected by the ELISA, as described in A. SLE1 serum was used as a standard of the ELISA. Data were shown as comparison to SLE1. C. Levels of anti-DNA Ab in 38 lupus sera and 2 control sera were detected by the ELISA described in A. SLE9 serum was used as a standard of the ELISA. Data were shown as comparisons to SLE9.
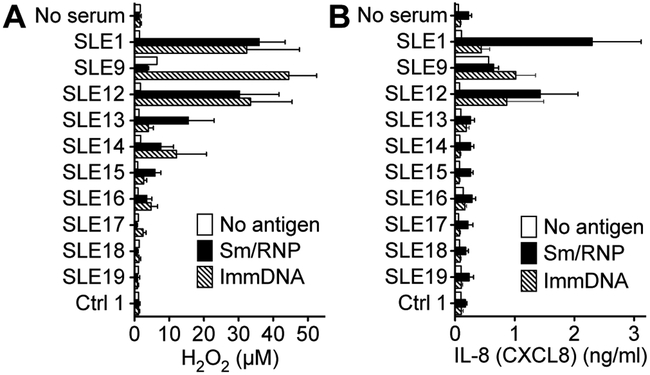
SLE sera with high levels of anti-DNA antibody and/or anti-Sm/RNP antibody induce neutrophil activation
To investigate the effect of SLE serum on neutrophil activation, we tested 10 SLE sera with different levels and specificities of autoantibodies and a control serum (Table 1)(Fig. 3B&C). Serum alone did not induce H2O2 from SLE neutrophils, except SLE9 which contains a high titer of anti-DNA Abs (Fig. 4A). All anti-Sm/RNP Ab-positive SLE sera induced H2O2 in the presence of Sm/RNP. Some SLE sera induced higher levels of H2O2 compared to others, and the levels were loosely associated with the levels of anti-Sm/RNP Abs in their sera. When combined with immobilized DNA, some SLE sera induced ROS. However, the ROS levels were not associated with the levels of anti-DNA Abs in their sera obtained from in-house ELISA (Fig. 3C) or clinical data (Table 1).
Figure 4. Soluble RNA-containing ICs and immobilized DNA-containing ICs activate neutrophils from lupus patients to release ROS and IL-8.
A. Neutrophils from lupus patients were stimulated with SLE and control sera with or without Sm/RNP or immobilized DNA (ImmDNA). One hour later, H2O2 levels in the supernatant were determined. The data represent the mean +/− SEM of 4 independent experiments. B. Neutrophils from lupus patients were stimulated with SLE and control sera with or without Sm/RNP or immobilized DNA (ImmDNA) for 24 hours. IL-8 levels in the supernatant were determined by ELISA. The data represent the mean +/− SEM of 5 independent experiments.
Human neutrophils release IL-8 (CXCL8), which attracts more neutrophils (43) and blocking IL-8 reduces disease severity of IC-based kidney disease (44). Thus, we examined neutrophil IL-8 production induced by nucleic acid-containing ICs. Without autoantigen, all sera except SLE9 serum induced no IL-8 (Fig. 4B). With the combination of Sm/RNP, SLE1 and SLE12 induced high levels of IL-8, whereas other sera did not induce IL-8. When combined with immobilized DNA, SLE1, SLE9 and SLE12 sera induced high levels of IL-8. These results suggest that nucleic acid-containing ICs activate neutrophils to induce ROS and IL-8.
FcγRIIA and FcγRIIIB are involved in the binding and phagocytosis of nucleic acid-containing ICs.
FcγRIIA and FcγRIIIB are the main activating Fc γ receptors on neutrophils (Fig. 1B). To understand the role of FcγRIIA and FcγRIIIB on binding and phagocytosis of nucleic acid-containing ICs, we generated fluorescence-labeled RNA-containing ICs. To investigate which receptors were involved in the binding and uptake we treated neutrophils from lupus patients with blocking anti-FcγRIIA Ab and/or anti-FcγRIII Ab. After a one-hour incubation of RNA-containing ICs at 4°C and 37°C, we measured the binding and/or uptake of ICs on neutrophils by flow cytometry (Fig. 5A). RNA-containing ICs binds to neutrophils at 4°C and the binding was inhibited by anti-FcγRIIA Ab and anti-FcγRIII Ab. The combination of anti-FcγRIIA and anti-FcγRIII Ab almost completely blocked the binding of RNA-containing ICs. At 37°C, blockage with anti-FcγRIIA Ab reduced binding and/or phagocytosis of RNA-containing ICs. Interestingly, the combination of anti-FcγRIIA Ab and anti-FcγRIII Ab did not completely block the binding and/or phagocytosis of RNA-containing ICs, suggesting that there may be other receptors involved in IC phagocytosis. Chloroquine did not inhibit the binding or phagocytosis of RNA-ICs.
Nucleic acid-containing ICs induce ROS from lupus neutrophils through FcγRIIA but not FcγRIIIB.
Fc γ receptors control immune cell activation induced by ICs. However, it is unclear which FcγRs play the main role in the neutrophil activation induced by soluble ICs and immobilized ICs (16, 38, 45, 46). To investigate this, we stimulated human neutrophils with nucleic acid-containing ICs in the presence of anti-FcγR blocking Abs. Anti-FcγRIIA Ab suppressed ROS release induced by RNA-containing ICs, whereas FcγRIIIB Ab did not (Fig. 5B). Anti-FcγRIIA Ab also inhibited ROS production induced by immobilized DNA-containing ICs (Fig. 5C). In contrast, Anti-FcγRIIIB Ab enhanced ROS production. These data indicate that both soluble RNA-containing ICs and immobilized DNA-containing ICs activate neutrophils through FcγRIIA engagement.
Nucleic acid-containing ICs induce TLR-independent activation of neutrophils.
TLR activation plays a role in SLE (8, 9). Previous studies have shown that human neutrophil activation induced by RNP-containing ICs is blocked by TLR7 inhibitor (IRS-661), suggesting that the importance of intracellular TLRs in the activation of neutrophils (16). Although neutrophils express TLR9, an intracellular receptor for DNA (5, 19, 20), whether TLR9 in neutrophils is responsible for the activation induced by DNA-containing ICs is not investigated. To investigate this, we stimulated neutrophils from wild type mice, TLR7−/− mice and TLR9−/− mice with nucleic acid-containing ICs and TLR ligands. TLR2 ligand (Pam3Cys), TLR4 ligand (LPS) and TLR9 ligand (CpG-B; 1826) did not induce ROS from mouse neutrophils (Fig. 6A). TLR9 ligand (CpG-A; 2336) stimulated neutrophils to release H2O2, in a TLR7 and TLR9-independent manner. Sm/RNP antigen only or SLE1 serum only did not induce H2O2. RNA-containing ICs induced H2O2 release from mouse neutrophils. Interestingly, the activation was TLR7-independent, as TLR7−/− neutrophils also release ROS in response to RNA-containing ICs. Immobilized DNA only did not induce H2O2, whereas SLE9 serum only slightly activated mouse neutrophils to induce H2O2. Immobilized DNA-containing ICs stimulated wild type mouse neutrophils to release H2O2. Interestingly the activation was TLR9-independent as neutrophils from TLR9−/− mice secreted similar levels of H2O2.
Next we examined whether nucleic acid-containing ICs induce chemokines through TLR signaling. Mice do not express IL-8 (47), and our previous study has shown that mouse neutrophils can induce MIP-1α upon stimulation with TLR ligands (48). TLR7 ligand (R848) did not induce MIP-1α from TLR7−/− neutrophils and TLR9 ligand (1826 and 2336) did not induce MIP-1α from TLR9−/− neutrophils (Fig. 6B). Thus, MIP-1α secretion is TLR-dependent. Surprisingly, RNA-containing ICs stimulated wild type neutrophils, TLR7−/− neutrophils and TLR9−/− neutrophils to release MIP-1α (Fig. 6B). Immobilized DNA-containing ICs did not activate mouse neutrophils to release MIP-1α. Taken together, these results suggest that nucleic acid-containing ICs activate mouse neutrophils to release ROS and MIP-1α through TLR-independent pathways.
To examine whether human neutrophils activation induced by nucleic acid-containing ICs is also TLR-independent, we used TLR7/9 inhibitors. Inhibitory oligonucleotides (ODNs) 2088 and INH-18 block the activation of both TLR7 and TLR9 in mice (26, 49-52). Chloroquine inhibits TLR7 and TLR9 activation by blocking acidification of endosomal compartment (53-55). Inhibitory ODNs 2088 and INH-18 did not inhibit ROS production from human neutrophils stimulated with RNA-containing ICs (Fig. 6C). Surprisingly, 2088 and INH-18 enhanced ROS production induced by immobilized DNA-ICs. 2088 and INH-18 alone did not activate neutrophils. Interestingly chloroquine suppressed ROS production induced by both Sm/RNP-containing ICs as well as immobilized DNA-containing ICs.
Because inhibitory ODNs did not suppress ROS production induced by Sm/RNP-containing ICs and immobilized DNA-containing ICs, we wondered whether these inhibitory ODNs can inhibit TLR7/8 activation in human immune cells. To investigate this possibility, we stimulated PBMC from lupus patients with R848 in the presence or absence of inhibitory ODNs and measured IL-6 (Fig. 6D). Inhibitory ODN 2088 blocked IL-6 released from PBMC stimulated R848, whereas inhibitory ODN INH-18 did not. These results suggest that inhibitory ODNs do not inhibit neutrophil activation induced by nucleic acid-containing ICs, but chloroquine is able to partially inhibit IC responses.
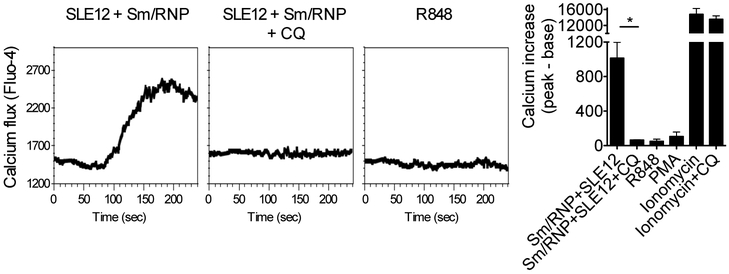
Chloroquine inhibits calcium flux induced by RNA-containing ICs.
Chloroquine is known to inhibit endosomal acidification, which is required for the activation of TLR7, TLR8 and TLR9. However, we observed TLR-independent but chloroquine-dependent activation of neutrophils induced by nucleic acid-containing ICs (Fig. 6C). Thus, we hypothesized that chloroquine blocks Fc γ receptor signaling. Immune complexes induce Fc γ receptor crosslinking and activate PLCγ activation following calcium flux (27, 56). Upregulation of intracellular calcium triggers the activation of NADPH oxidase which produces ROSs (57-59).
To understand the mechanisms of chloroquine inhibition in neutrophils, we stimulated neutrophils from lupus patients with TLR ligand R848, Sm/RNP-containing ICs, PMA and ionomycin and measured calcium influx. Sm/RNP-containing ICs induced calcium flux due to Fc γ receptor crosslinking (27)(Fig. 7). Interestingly chloroquine inhibited the calcium flux induced by Sm/RNP-containing ICs. R848 did not induce calcium flux, indicating that TLR7/8 signaling do not induce calcium signaling in neutrophils from lupus patients. PMA (a protein kinase C activator) did not induce calcium flux, because PKC is downstream of calcium signaling (60). Ionomycin, which is a calcium ionophore, induced calcium flux. Chloroquine did not inhibit calcium flux induced by ionomycin.
Figure 7. Chloroquine inhibits calcium flux induced by Sm/RNP-containing ICs.
Neutrophils from lupus patients were stimulated with R848 (TLR7/8 ligand, 10 μM), SLE12+Sm/RNP, SLE12+Sm/RNP with chloroquine (CQ, 20 μg/ml), PMA (100 nM), ionomycin (5 μg/ml), and ionomycin+ CQ. Calcium flux were determined the fluorescence intensity of Fluo-4. Mann-Whitney test was used for statistical analysis between IC and IC + CQ, and Ionomycin and Ionomycin + CQ. * P<0.05.
In, conclusion, nucleic acid-containing ICs induce neutrophil activation through FcγR-mediated activation. The activation triggers calcium flux which contributes to the production of H2O2. Chloroquine suppresses calcium flux and H2O2 production induced by nucleic acid-containing ICs.
Discussion
Neutrophils are the first immune cells to arrive at the site of inflammation, and a signature of neutrophil activation is correlated with lupus nephritis (14, 15, 61). In the present study, we have shown that nucleic acid-containing ICs trigger neutrophil activation to release ROS and IL-8. The activation is FcγRIIA-dependent and TLR-independent, despite the fact that neutrophils express TLR8 and TLR9 (19, 62). Interestingly, chloroquine, which has been used for the treatment of SLE (63), suppresses the neutrophil activation induced by nucleic acid-containing ICs. This depends on a less known mechanism that chloroquine is able to inhibit calcium flux triggered by nucleic acid-containing ICs.
In the present study, we have shown that immobilized DNA-containing ICs induce neutrophil activation leading to release of ROS and IL-8, whereas soluble DNA-containing ICs do not. In lupus nephritis, anti-DNA Ab are present in the glomerular basement membrane (GBM), and DNA and nucleosomes may be immobilized in the GBM, or anti-DNA Abs cross react with fixed components of the GBM in the kidney (64-66). Our findings may suggest that immobilized but not soluble DNA-containing ICs may trigger neutrophil activation in the kidney.
Neutrophils express FcγRIIA and FcγRIIIB, and IC binding is dependent on both FcγRIIA and FcγRIIIB on neutrophils from lupus patients. At 37°C, we observed that inhibition of FcγRIIA decreases the binding and/or phagocytosis of ICs. However, the mechanisms of ROS production may be different from the mechanisms of IC phagocytosis. We found that anti-FcγRIIA Ab inhibits the ROS production from neutrophils induced by both RNA-containing ICs and immobilized DNA-containing ICs, whereas anti-FcγRIIIB Ab does not. Distinct from other Fc γ receptors, FcγRIIA contains an ITAM motif and activates immune cells without using the Fc receptor common γ chain (67). Interestingly, nucleic acid-containing ICs activate plasmacytoid dendritic cells only through FcγRIIA, and not through other Fc γ receptors (68, 69). Similarly, platelet activation induced by ICs is FcγRIIA-dependent, and platelet activation enhances type I interferon production from plasmacytoid dendritic cells (70). Blocking this particular Fc γ receptor may ameliorate disease severity in SLE.
We observed that combination of anti-FcγRIIA Ab and anti-FcγRIII Ab do not fully inhibit the IC interaction to neutrophils at 37°C (Fig. 5A). In addition, we found that blocking FcγRIIA and FcγRIIIB do not abolish H2O2 production, as anti-FcγRIIA Ab inhibits half of the H2O2 production induced by nucleic acid-containing ICs while anti-FcγRIII Ab does not inhibit. This raises the possibility that other receptors may have a role in neutrophil activation and phagocytosis and several studies have reported that complement receptor-3 (CR3, Mac-1) may also be involved in ROS production induced by ICs (57, 71, 72). The cooperation of FcγRIIA, FcγRIIIB and Mac-1 (CR3) may be required for the phagocytosis of ICs and activation of neutrophils (73).
A previous study has shown that TLR7/8 activation is required for the neutrophil NET formation induced by RNP-containing ICs (16). However, in the present study using neutrophils from TLR7-deficient and TLR9-deficient mice, we have shown nucleic acid-containing ICs trigger ROS production through TLR9-independent and TLR7-independent pathways. Similarly, MIP-1α production is independent of TLR7 signaling. Several cytosolic DNA and RNA-sensing receptors are reported (74, 75), and neutrophils express RNA-sensing receptors RIG-I and MDA5 in the cytosol and possibly also on the cell surface (76-78). While it is beyond the scope of this present study, we postulate that these nucleic acid-sensing receptors may be involved in the neutrophil activation induced by nucleic acid-containing ICs. Another unexpected finding is that CpG-A induces ROS production from TLR9−/− neutrophils. Recent studies have demonstrated that DNA induce TLR9-dependent and TLR9-independent neutrophil activation, and neutrophils from IRAK4-deficient people still respond to CpG-DNA stimulation (79, 80). CpG-A might be the ligand of Sox2, as it has been reported that DNA induces Sox2-mediated activation in neutrophils (81, 82).
Several inhibitory oligonucleotides (ODNs) have been developed for the blocking of TLR7/8 and TLR9 signaling (26, 49, 52, 83-85). We used inhibitory ODNs 2088 and INH-18 and found that both do not inhibit the neutrophil activation induced by RNA-containing ICs, and upregulate the activation induced by immobilized DNA-containing ICs. These indicate that the activation of human neutrophils induced by nucleic acid-containing ICs does not require TLR7, TLR8 or TLR9 signaling. Although the precise mechanisms are not known, it is possible that inhibitory ODNs bind to anti-DNA Abs to form immune complexes. Anti-DNA Abs can bind to 20-mer phosphorothioate ODNs and to lesser extent 10-mer phosphorothioate ODNs, and inhibitory ODN 2088 consists of 15-mer phosphorothioate ODN and INH-18 is a 24-mer ODN (26, 86).
Chloroquine and hydroxychloroquine are used for the treatment of SLE, although the precise mechanisms of action are not fully investigated (63, 87). Chloroquine functions as an endosomal acidification inhibitor and an autophagy inhibitor (53, 88). As an endosomal acidification inhibitor, chloroquine inhibits the activation of TLR7/9 in endosomal/lysosomal compartments (50, 51, 89). Chloroquine and its derivative bind directly to nucleic acids and inhibit nucleic acid-TLR interaction (90). In the present study we have demonstrated that chloroquine suppresses ROS production in neutrophils induced by both soluble RNA-containing ICs and immobilized DNA-containing ICs. We found an additional role for chloroquine, which is the inhibition of calcium flux induced by nucleic acid-containing ICs. Goldman et al have reported that hydroxychloroquine blocks calcium flux induced TCR and BCR, but it does not inhibit PLCγ1 phosphorylation and inositol phosphate production which are upstream of calcium signaling (91). Misra et al have shown that chloroquine, quinine and quinidine inhibit calcium flux by blocking inositol trisphosphate receptor (92). The mechanisms of these anti-malarial drugs on immune cell activation induced by nucleic acid-containing ICs should be further investigated.
In conclusion, we have demonstrated that nucleic acid-containing ICs induce neutrophil activation through FcγRIIA-dependent and TLR-independent pathways. Antibodies that block FcγRIIA or chloroquine-derivatives that are less toxic than the form currently available are potential future treatments for SLE.
Acknowledgements
We thank the Autoimmune Kidney Research Repository at the Boston University Medical Center. We thank Carlos R. Sian for technical assistance. This work was supported by the Flow Cytometry Core Facility and Analytical Instrumentation Core Facility at the Boston University School of Medicine. The authors would like to thank Paul A. Monach and Makoto Okazaki for their insightful comments and suggestions.
This work was supported by the following National Institute of Health Grants 1K01AR0608507 (to K.Y) and R01 DK090558 (to R.G.B), Kidney foundation (to H. MJ), and the Boston University Undergraduate Research Opportunity Program (to J. D. L).
Nonstandard abbreviations:
- CR3
complement receptor-3
- CQ
chloroquine.
- GBM
glomerular basement membrane
- IC
Immune complexes
- IRF
interferon regulatory factor
- MFI
mean fluorescence intensity
- NET
neutrophil extracellular trap
- ODN
oligonucleotides.
- RNP
ribonucleoprotein
- ROS
reactive oxygen species
- SLE
systemic lupus erythematosus
Footnotes
Disclosures
The authors have no financial conflict of interest.
References
- 1.Rahman A, and Isenberg DA. 2008. Systemic lupus erythematosus. N Engl J Med 358: 929–939. [DOI] [PubMed] [Google Scholar]
- 2.Liu Z, and Davidson A. 2012. Taming lupus-a new understanding of pathogenesis is leading to clinical advances. Nat Med 18: 871–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaniv G, Twig G, Shor DB, Furer A, Sherer Y, Mozes O, Komisar O, Slonimsky E, Klang E, Lotan E, Welt M, Marai I, Shina A, Amital H, and Shoenfeld Y. 2015. A volcanic explosion of autoantibodies in systemic lupus erythematosus: a diversity of 180 different antibodies found in SLE patients. Autoimmun Rev 14: 75–79. [DOI] [PubMed] [Google Scholar]
- 4.Pisetsky DS 2017. Antinuclear antibody testing - misunderstood or misbegotten? Nat Rev Rheumatol 13: 495–502. [DOI] [PubMed] [Google Scholar]
- 5.Kawai T, and Akira S. 2010. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol 11: 373–384. [DOI] [PubMed] [Google Scholar]
- 6.Celhar T, Hopkins R, Thornhill SI, De Magalhaes R, Hwang SH, Lee HY, Yasuga H, Jones LA, Casco J, Lee B, Thamboo TP, Zhou XJ, Poidinger M, Connolly JE, Wakeland EK, and Fairhurst AM. 2015. RNA sensing by conventional dendritic cells is central to the development of lupus nephritis. Proc Natl Acad Sci U S A 112: E6195–6204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hwang SH, Lee H, Yamamoto M, Jones LA, Dayalan J, Hopkins R, Zhou XJ, Yarovinsky F, Connolly JE, Curotto de Lafaille MA, Wakeland EK, and Fairhurst AM. 2012. B cell TLR7 expression drives anti-RNA autoantibody production and exacerbates disease in systemic lupus erythematosus-prone mice. J Immunol 189: 5786–5796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marshak-Rothstein A 2006. Toll-like receptors in systemic autoimmune disease. Nat Rev Immunol 6: 823–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshak-Rothstein A, and Rifkin IR. 2007. Immunologically active autoantigens: the role of toll-like receptors in the development of chronic inflammatory disease. Annu Rev Immunol 25: 419–441. [DOI] [PubMed] [Google Scholar]
- 10.Rifkin IR, Leadbetter EA, Busconi L, Viglianti G, and Marshak-Rothstein A. 2005. Toll-like receptors, endogenous ligands, and systemic autoimmune disease. Immunol Rev 204: 27–42. [DOI] [PubMed] [Google Scholar]
- 11.Yasuda K, Richez C, Maciaszek JW, Agrawal N, Akira S, Marshak-Rothstein A, and Rifkin IR. 2007. Murine dendritic cell type I IFN production induced by human IgG-RNA immune complexes is IFN regulatory factor (IRF)5 and IRF7 dependent and is required for IL-6 production. J Immunol 178: 6876–6885. [DOI] [PubMed] [Google Scholar]
- 12.Amulic B, Cazalet C, Hayes GL, Metzler KD, and Zychlinsky A. 2012. Neutrophil function: from mechanisms to disease. Annu Rev Immunol 30: 459–489. [DOI] [PubMed] [Google Scholar]
- 13.Bennett L, Palucka AK, Arce E, Cantrell V, Borvak J, Banchereau J, and Pascual V. 2003. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J Exp Med 197: 711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banchereau R, Hong S, Cantarel B, Baldwin N, Baisch J, Edens M, Cepika AM, Acs P, Turner J, Anguiano E, Vinod P, Kahn S, Obermoser G, Blankenship D, Wakeland E, Nassi L, Gotte A, Punaro M, Liu YJ, Banchereau J, Rossello-Urgell J, Wright T, and Pascual V. 2016. Personalized Immunomonitoring Uncovers Molecular Networks that Stratify Lupus Patients. Cell 165: 551–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jourde-Chiche N, Whalen E, Gondouin B, Speake C, Gersuk V, Dussol B, Burtey S, Pascual V, Chaussabel D, and Chiche L. 2017. Modular transcriptional repertoire analyses identify a blood neutrophil signature as a candidate biomarker for lupus nephritis. Rheumatology (Oxford) 56: 477–487. [DOI] [PubMed] [Google Scholar]
- 16.Garcia-Romo GS, Caielli S, Vega B, Connolly J, Allantaz F, Xu Z, Punaro M, Baisch J, Guiducci C, Coffman RL, Barrat FJ, Banchereau J, and Pascual V. 2011. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci Transl Med 3: 73ra20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lood C, Blanco LP, Purmalek MM, Carmona-Rivera C, De Ravin SS, Smith CK, Malech HL, Ledbetter JA, Elkon KB, and Kaplan MJ. 2016. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med 22: 146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caielli S, Athale S, Domic B, Murat E, Chandra M, Banchereau R, Baisch J, Phelps K, Clayton S, Gong M, Wright T, Punaro M, Palucka K, Guiducci C, Banchereau J, and Pascual V. 2016. Oxidized mitochondrial nucleoids released by neutrophils drive type I interferon production in human lupus. J Exp Med 213: 697–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayashi F, Means TK, and Luster AD. 2003. Toll-like receptors stimulate human neutrophil function. Blood 102: 2660–2669. [DOI] [PubMed] [Google Scholar]
- 20.Trevani AS, Chorny A, Salamone G, Vermeulen M, Gamberale R, Schettini J, Raiden S, and Geffner J. 2003. Bacterial DNA activates human neutrophils by a CpG-independent pathway. Eur J Immunol 33: 3164–3174. [DOI] [PubMed] [Google Scholar]
- 21.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, and Winchester RJ. 1982. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25: 1271–1277. [DOI] [PubMed] [Google Scholar]
- 22.Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi LM, Makino H, Moura LA, and Nagata M. 2004. The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol 15: 241–250. [DOI] [PubMed] [Google Scholar]
- 23.Yasuda K, Ogawa Y, Kishimoto M, Takagi T, Hashida M, and Takakura Y. 2002. Plasmid DNA activates murine macrophages to induce inflammatory cytokines in a CpG motif-independent manner by complex formation with cationic liposomes. Biochem Biophys Res Commun 293: 344–348. [DOI] [PubMed] [Google Scholar]
- 24.Nauseef WM 2014. Isolation of human neutrophils from venous blood. Methods Mol Biol 1124: 13–18. [DOI] [PubMed] [Google Scholar]
- 25.Denny MF, Yalavarthi S, Zhao W, Thacker SG, Anderson M, Sandy AR, McCune WJ, and Kaplan MJ. 2010. A distinct subset of proinflammatory neutrophils isolated from patients with systemic lupus erythematosus induces vascular damage and synthesizes type I IFNs. J Immunol 184: 3284–3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lenert P, Yasuda K, Busconi L, Nelson P, Fleenor C, Ratnabalasuriar RS, Nagy PL, Ashman RF, Rifkin IR, and Marshak-Rothstein A. 2009. DNA-like class R inhibitory oligonucleotides (INH-ODNs) preferentially block autoantigen-induced B-cell and dendritic cell activation in vitro and autoantibody production in lupus-prone MRL-Fas(lpr/lpr) mice in vivo. Arthritis Res Ther 11: R79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nimmerjahn F, and Ravetch JV. 2008. Fcgamma receptors as regulators of immune responses. Nat Rev Immunol 8: 34–47. [DOI] [PubMed] [Google Scholar]
- 28.Nimmerjahn F, and Ravetch JV. 2006. Fcgamma receptors: old friends and new family members. Immunity 24: 19–28. [DOI] [PubMed] [Google Scholar]
- 29.Tan Y, Watkins AA, Freeman BB, Meyers JA, Rifkin IR, and Lerner A. 2015. Inhibition of type 4 cyclic nucleotide phosphodiesterase blocks intracellular TLR signaling in chronic lymphocytic leukemia and normal hematopoietic cells. J Immunol 194: 101–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pisetsky DS 2016. Anti-DNA antibodies--quintessential biomarkers of SLE. Nat Rev Rheumatol 12: 102–110. [DOI] [PubMed] [Google Scholar]
- 31.Linnik MD, Hu JZ, Heilbrunn KR, Strand V, Hurley FL, Joh T, and Consortium LJPI. 2005. Relationship between anti-double-stranded DNA antibodies and exacerbation of renal disease in patients with systemic lupus erythematosus. Arthritis Rheum 52: 1129–1137. [DOI] [PubMed] [Google Scholar]
- 32.Yasuda K, Richez C, Uccellini MB, Richards RJ, Bonegio RG, Akira S, Monestier M, Corley RB, Viglianti GA, Marshak-Rothstein A, and Rifkin IR. 2009. Requirement for DNA CpG content in TLR9-dependent dendritic cell activation induced by DNA-containing immune complexes. J Immunol 183: 3109–3117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leadbetter EA, Rifkin IR, Hohlbaum AM, Beaudette BC, Shlomchik MJ, and Marshak-Rothstein A. 2002. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature 416: 603–607. [DOI] [PubMed] [Google Scholar]
- 34.Viglianti GA, Lau CM, Hanley TM, Miko BA, Shlomchik MJ, and Marshak-Rothstein A. 2003. Activation of autoreactive B cells by CpG dsDNA. Immunity 19: 837–847. [DOI] [PubMed] [Google Scholar]
- 35.Vallin H, Perers A, Alm GV, and Ronnblom L. 1999. Anti-double-stranded DNA antibodies and immunostimulatory plasmid DNA in combination mimic the endogenous IFN-alpha inducer in systemic lupus erythematosus. J Immunol 163: 6306–6313. [PubMed] [Google Scholar]
- 36.Vallin H, Blomberg S, Alm GV, Cederblad B, and Ronnblom L. 1999. Patients with systemic lupus erythematosus (SLE) have a circulating inducer of interferon-alpha (IFN-alpha) production acting on leucocytes resembling immature dendritic cells. Clin Exp Immunol 115: 196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lovgren T, Eloranta ML, Bave U, Alm GV, and Ronnblom L. 2004. Induction of interferon-alpha production in plasmacytoid dendritic cells by immune complexes containing nucleic acid released by necrotic or late apoptotic cells and lupus IgG. Arthritis Rheum 50: 1861–1872. [DOI] [PubMed] [Google Scholar]
- 38.Behnen M, Leschczyk C, Moller S, Batel T, Klinger M, Solbach W, and Laskay T. 2014. Immobilized immune complexes induce neutrophil extracellular trap release by human neutrophil granulocytes via FcgammaRIIIB and Mac-1. J Immunol 193: 1954–1965. [DOI] [PubMed] [Google Scholar]
- 39.Coxon A, Cullere X, Knight S, Sethi S, Wakelin MW, Stavrakis G, Luscinskas FW, and Mayadas TN. 2001. Fc gamma RIII mediates neutrophil recruitment to immune complexes. a mechanism for neutrophil accumulation in immune-mediated inflammation. Immunity 14: 693–704. [DOI] [PubMed] [Google Scholar]
- 40.Chuang FY, Sassaroli M, and Unkeless JC. 2000. Convergence of Fc gamma receptor IIA and Fc gamma receptor IIIB signaling pathways in human neutrophils. J Immunol 164: 350–360. [DOI] [PubMed] [Google Scholar]
- 41.Lood C, Arve S, Ledbetter J, and Elkon KB. 2017. TLR7/8 activation in neutrophils impairs immune complex phagocytosis through shedding of FcgRIIA. J Exp Med 214: 2103–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wartha F, and Henriques-Normark B. 2008. ETosis: a novel cell death pathway. Sci Signal 1: pe25. [DOI] [PubMed] [Google Scholar]
- 43.Tecchio C, and Cassatella MA. 2016. Neutrophil-derived chemokines on the road to immunity. Semin Immunol 28: 119–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wada T, Tomosugi N, Naito T, Yokoyama H, Kobayashi K, Harada A, Mukaida N, and Matsushima K. 1994. Prevention of proteinuria by the administration of anti-interleukin 8 antibody in experimental acute immune complex-induced glomerulonephritis. J Exp Med 180: 1135–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen K, Nishi H, Travers R, Tsuboi N, Martinod K, Wagner DD, Stan R, Croce K, and Mayadas TN. 2012. Endocytosis of soluble immune complexes leads to their clearance by FcgammaRIIIB but induces neutrophil extracellular traps via FcgammaRIIA in vivo. Blood 120: 4421–4431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aleman OR, Mora N, Cortes-Vieyra R, Uribe-Querol E, and Rosales C. 2016. Differential Use of Human Neutrophil Fcgamma Receptors for Inducing Neutrophil Extracellular Trap Formation. J Immunol Res 2016: 2908034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singer M, and Sansonetti PJ. 2004. IL-8 is a key chemokine regulating neutrophil recruitment in a new mouse model of Shigella-induced colitis. J Immunol 173: 4197–4206. [DOI] [PubMed] [Google Scholar]
- 48.Ericson JA, Duffau P, Yasuda K, Ortiz-Lopez A, Rothamel K, Rifkin IR, Monach PA, and ImmGen C. 2014. Gene expression during the generation and activation of mouse neutrophils: implication of novel functional and regulatory pathways. PLoS One 9: e108553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stunz LL, Lenert P, Peckham D, Yi AK, Haxhinasto S, Chang M, Krieg AM, and Ashman RF. 2002. Inhibitory oligonucleotides specifically block effects of stimulatory CpG oligonucleotides in B cells. Eur J Immunol 32: 1212–1222. [DOI] [PubMed] [Google Scholar]
- 50.Lau CM, Broughton C, Tabor AS, Akira S, Flavell RA, Mamula MJ, Christensen SR, Shlomchik MJ, Viglianti GA, Rifkin IR, and Marshak-Rothstein A. 2005. RNA-associated autoantigens activate B cells by combined B cell antigen receptor/Toll-like receptor 7 engagement. J Exp Med 202: 1171–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boule MW, Broughton C, Mackay F, Akira S, Marshak-Rothstein A, and Rifkin IR. 2004. Toll-like receptor 9-dependent and -independent dendritic cell activation by chromatin-immunoglobulin G complexes. J Exp Med 199: 1631–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rommler F, Jurk M, Uhlmann E, Hammel M, Waldhuber A, Pfeiffer L, Wagner H, Vollmer J, and Miethke T. 2013. Guanine modification of inhibitory oligonucleotides potentiates their suppressive function. J Immunol 191: 3240–3253. [DOI] [PubMed] [Google Scholar]
- 53.Yi AK, Tuetken R, Redford T, Waldschmidt M, Kirsch J, and Krieg AM. 1998. CpG motifs in bacterial DNA activate leukocytes through the pH-dependent generation of reactive oxygen species. J Immunol 160: 4755–4761. [PubMed] [Google Scholar]
- 54.Lund JM, Alexopoulou L, Sato A, Karow M, Adams NC, Gale NW, Iwasaki A, and Flavell RA. 2004. Recognition of single-stranded RNA viruses by Toll-like receptor 7. Proc Natl Acad Sci U S A 101: 5598–5603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vollmer J, Tluk S, Schmitz C, Hamm S, Jurk M, Forsbach A, Akira S, Kelly KM, Reeves WH, Bauer S, and Krieg AM. 2005. Immune stimulation mediated by autoantigen binding sites within small nuclear RNAs involves Toll-like receptors 7 and 8. J Exp Med 202: 1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ravetch JV, and Bolland S. 2001. IgG Fc receptors. Annu Rev Immunol 19: 275–290. [DOI] [PubMed] [Google Scholar]
- 57.Lofgren R, Serrander L, Forsberg M, Wilsson A, Wasteson A, and Stendahl O. 1999. CR3, FcgammaRIIA and FcgammaRIIIB induce activation of the respiratory burst in human neutrophils: the role of intracellular Ca(2+), phospholipase D and tyrosine phosphorylation. Biochim Biophys Acta 1452: 46–59. [DOI] [PubMed] [Google Scholar]
- 58.Brechard S, Plancon S, and Tschirhart EJ. 2013. New insights into the regulation of neutrophil NADPH oxidase activity in the phagosome: a focus on the role of lipid and Ca(2+) signaling. Antioxid Redox Signal 18: 661–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nauseef WM, and Borregaard N. 2014. Neutrophils at work. Nat Immunol 15: 602–611. [DOI] [PubMed] [Google Scholar]
- 60.Mochly-Rosen D, Das K, and Grimes KV. 2012. Protein kinase C, an elusive therapeutic target? Nat Rev Drug Discov 11: 937–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soehnlein O, Steffens S, Hidalgo A, and Weber C. 2017. Neutrophils as protagonists and targets in chronic inflammation. Nat Rev Immunol 17: 248–261. [DOI] [PubMed] [Google Scholar]
- 62.Prince LR, Whyte MK, Sabroe I, and Parker LC. 2011. The role of TLRs in neutrophil activation. Curr Opin Pharmacol 11: 397–403. [DOI] [PubMed] [Google Scholar]
- 63.Lee SJ, Silverman E, and Bargman JM. 2011. The role of antimalarial agents in the treatment of SLE and lupus nephritis. Nat Rev Nephrol 7: 718–729. [DOI] [PubMed] [Google Scholar]
- 64.Kalaaji M, Fenton KA, Mortensen ES, Olsen R, Sturfelt G, Alm P, and Rekvig OP. 2007. Glomerular apoptotic nucleosomes are central target structures for nephritogenic antibodies in human SLE nephritis. Kidney Int 71: 664–672. [DOI] [PubMed] [Google Scholar]
- 65.Izui S, Lambert PH, and Miescher PA. 1976. In vitro demonstration of a particular affinity of glomerular basement membrane and collagen for DNA. A possible basis for a local formation of DNA-anti-DNA complexes in systemic lupus erythematosus. J Exp Med 144: 428–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.van Bavel CC, van der Vlag J, and Berden JH. 2007. Glomerular binding of anti-dsDNA autoantibodies: the dispute resolved? Kidney Int 71: 600–601. [DOI] [PubMed] [Google Scholar]
- 67.Guilliams M, Bruhns P, Saeys Y, Hammad H, and Lambrecht BN. 2014. The function of Fcgamma receptors in dendritic cells and macrophages. Nat Rev Immunol 14: 94–108. [DOI] [PubMed] [Google Scholar]
- 68.Means TK, Latz E, Hayashi F, Murali MR, Golenbock DT, and Luster AD. 2005. Human lupus autoantibody-DNA complexes activate DCs through cooperation of CD32 and TLR9. J Clin Invest 115: 407–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bave U, Magnusson M, Eloranta ML, Perers A, Alm GV, and Ronnblom L. 2003. Fc gamma RIIa is expressed on natural IFN-alpha-producing cells (plasmacytoid dendritic cells) and is required for the IFN-alpha production induced by apoptotic cells combined with lupus IgG. J Immunol 171: 3296–3302. [DOI] [PubMed] [Google Scholar]
- 70.Duffau P, Seneschal J, Nicco C, Richez C, Lazaro E, Douchet I, Bordes C, Viallard JF, Goulvestre C, Pellegrin JL, Weil B, Moreau JF, Batteux F, and Blanco P. 2010. Platelet CD154 potentiates interferon-alpha secretion by plasmacytoid dendritic cells in systemic lupus erythematosus. Sci Transl Med 2: 47ra63. [DOI] [PubMed] [Google Scholar]
- 71.Zhou MJ, and Brown EJ. 1994. CR3 (Mac-1, alpha M beta 2, CD11b/CD18) and Fc gamma RIII cooperate in generation of a neutrophil respiratory burst: requirement for Fc gamma RIII and tyrosine phosphorylation. J Cell Biol 125: 1407–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nielsen CH, Antonsen S, Matthiesen SH, and Leslie RG. 1997. The roles of complement receptors type 1 (CR1, CD35) and type 3 (CR3, CD11b/CD18) in the regulation of the immune complex-elicited respiratory burst of polymorphonuclear leukocytes in whole blood. Eur J Immunol 27: 2914–2919. [DOI] [PubMed] [Google Scholar]
- 73.Graham IL, Lefkowith JB, Anderson DC, and Brown EJ. 1993. Immune complex-stimulated neutrophil LTB4 production is dependent on beta 2 integrins. J Cell Biol 120: 1509–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hornung V, and Latz E. 2010. Intracellular DNA recognition. Nat Rev Immunol 10: 123–130. [DOI] [PubMed] [Google Scholar]
- 75.Chan YK, and Gack MU. 2016. Viral evasion of intracellular DNA and RNA sensing. Nat Rev Microbiol 14: 360–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tamassia N, and Cassatella MA. 2013. Cytoplasmic receptors recognizing nucleic acids and mediating immune functions in neutrophils. Curr Opin Pharmacol 13: 547–554. [DOI] [PubMed] [Google Scholar]
- 77.Berger M, Hsieh CY, Bakele M, Marcos V, Rieber N, Kormann M, Mays L, Hofer L, Neth O, Vitkov L, Krautgartner WD, von Schweinitz D, Kappler R, Hector A, Weber A, and Hartl D. 2012. Neutrophils express distinct RNA receptors in a non-canonical way. J Biol Chem 287: 19409–19417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tamassia N, Le Moigne V, Rossato M, Donini M, McCartney S, Calzetti F, Colonna M, Bazzoni F, and Cassatella MA. 2008. Activation of an immunoregulatory and antiviral gene expression program in poly(I:C)-transfected human neutrophils. J Immunol 181: 6563–6573. [DOI] [PubMed] [Google Scholar]
- 79.El Kebir D, Jozsef L, and Filep JG. 2008. Neutrophil recognition of bacterial DNA and Toll-like receptor 9-dependent and -independent regulation of neutrophil function. Arch Immunol Ther Exp (Warsz) 56: 41–53. [DOI] [PubMed] [Google Scholar]
- 80.Hoarau C, Gerard B, Lescanne E, Henry D, Francois S, Lacapere JJ, El Benna J, Dang PM, Grandchamp B, Lebranchu Y, Gougerot-Pocidalo MA, and Elbim C. 2007. TLR9 activation induces normal neutrophil responses in a child with IRAK-4 deficiency: involvement of the direct PI3K pathway. J Immunol 179: 4754–4765. [DOI] [PubMed] [Google Scholar]
- 81.Mankan AK, and Hornung V. 2015. Sox2 as a servant of two masters. Nat Immunol 16: 335–336. [DOI] [PubMed] [Google Scholar]
- 82.Xia P, Wang S, Ye B, Du Y, Huang G, Zhu P, and Fan Z. 2015. Sox2 functions as a sequence-specific DNA sensor in neutrophils to initiate innate immunity against microbial infection. Nat Immunol 16: 366–375. [DOI] [PubMed] [Google Scholar]
- 83.Duramad O, Fearon KL, Chang B, Chan JH, Gregorio J, Coffman RL, and Barrat FJ. 2005. Inhibitors of TLR-9 act on multiple cell subsets in mouse and man in vitro and prevent death in vivo from systemic inflammation. J Immunol 174: 5193–5200. [DOI] [PubMed] [Google Scholar]
- 84.Barrat FJ, Meeker T, Gregorio J, Chan JH, Uematsu S, Akira S, Chang B, Duramad O, and Coffman RL. 2005. Nucleic acids of mammalian origin can act as endogenous ligands for Toll-like receptors and may promote systemic lupus erythematosus. J Exp Med 202: 1131–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rommler F, Hammel M, Waldhuber A, Muller T, Jurk M, Uhlmann E, Wagner H, Vollmer J, and Miethke T. 2015. Guanine-modified inhibitory oligonucleotides efficiently impair TLR7- and TLR9-mediated immune responses of human immune cells. PLoS One 10: e0116703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pisetsky DS, and Reich CF 3rd. 1998. The binding of anti-DNA antibodies to phosphorothioate oligonucleotides in a solid phase immunoassay. Mol Immunol 35: 1161–1170. [DOI] [PubMed] [Google Scholar]
- 87.An J, Minie M, Sasaki T, Woodward JJ, and Elkon KB. 2017. Antimalarial Drugs as Immune Modulators: New Mechanisms for Old Drugs. Annu Rev Med 68: 317–330. [DOI] [PubMed] [Google Scholar]
- 88.Levy JMM, Towers CG, and Thorburn A. 2017. Targeting autophagy in cancer. Nat Rev Cancer 17: 528–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hacker H, Mischak H, Miethke T, Liptay S, Schmid R, Sparwasser T, Heeg K, Lipford GB, and Wagner H. 1998. CpG-DNA-specific activation of antigen-presenting cells requires stress kinase activity and is preceded by non-specific endocytosis and endosomal maturation. EMBO J 17: 6230–6240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kuznik A, Bencina M, Svajger U, Jeras M, Rozman B, and Jerala R. 2011. Mechanism of endosomal TLR inhibition by antimalarial drugs and imidazoquinolines. J Immunol 186: 4794–4804. [DOI] [PubMed] [Google Scholar]
- 91.Goldman FD, Gilman AL, Hollenback C, Kato RM, Premack BA, and Rawlings DJ. 2000. Hydroxychloroquine inhibits calcium signals in T cells: a new mechanism to explain its immunomodulatory properties. Blood 95: 3460–3466. [PubMed] [Google Scholar]
- 92.Misra UK, Gawdi G, and Pizzo SV. 1997. Chloroquine, quinine and quinidine inhibit calcium release from macrophage intracellular stores by blocking inositol 1,4,5-trisphosphate binding to its receptor. J Cell Biochem 64: 225–232. [DOI] [PubMed] [Google Scholar]