Abstract
Network analysis may be a powerful tool for studying interprofessional practice. Using electronic health record data and social network analysis, the network of healthcare professionals involved in colorectal cancer care at a large, urban academic medical center were mapped and studied. A total of 100 surgical colorectal cancer patients receiving treatment in 2013 and 2014 were selected at random. We used detailed access logs for the EHR to map the network of all healthcare professionals for each patient, including inpatient and outpatient settings. Approximately 2.45 million records of access logs from more than 6,800 unique users, representing over 150 roles or occupations were analyzed. Across all networks, professionals were connected to an average of 5.8 other professionals, but some were rarely connected with others while over 20 were very highly connected (>100 other professionals). Housestaff, attending physicians, and nurses played central roles in the global network with a high number of inter- and intra-professional connections. Clusters of professionals with frequent interaction were demonstrated but, based on the size and complexity of the network, serendipitous interactions were unlikely. Settings for care seemed to influence these clusters. Patient-centric care networks were similar to the global network with some potentially important differences. Access-log information from electronic health records can be an important source of information about relationships between healthcare professionals. Findings from analyses such as this one may help define the state of current networks and potential targets for interventions to improve the quality of care.
Keywords: network analysis, electronic health records, healthcare teams, Quantitative method, Interprofessional care, Interprofessional collaboration, Teams, Teamwork
INTRODUCTION
Improving the performance of healthcare teams is essential for increasing the quality of care (Institute of Medicine, 2001). In cancer care in particular, better team-based care is seen as a key objective for achieving optimal outcomes (Institute of Medicine, 2014). Yet, team composition and structures in cancer care are poorly defined and understood. Broadly in healthcare, interprofessional practice can be seen as ranging from being delivered by teams where members of discrete teams work synchronously to help patients to being self-organized as networks where, although professionals work asynchronously, they are interconnected because of the shared responsibility for same patients (Reeves, Lewin, Espin, & Zwarenstein, 2011). Often, asynchronous interprofessional practice relies on electronic health records (EHRs) to organize and support individual work, creating virtual teams (Driskell, Radtke, & Salas, 2003). While discrete teams are present in some aspects of cancer care, such as multidisciplinary planning conferences and palliative care, much of cancer care is delivered asynchronously by virtual teams. These virtual teams are prime targets for improving teamwork and the resulting quality of care.
The increase of virtual teams has been spurred by the widespread adoption of EHRs. Healthcare professionals in hospital settings spend much of their workday working with the EHRs (Ammenwerth & Spötl, 2009; Hripcsak, Vawdrey, Fred, & Bostwick, 2011; O’Leary, Liebovitz, & Baker, 2006). Many physicians report spending over 4 hours a day on reading and writing notes (Hripcsak et al., 2011).EHR data may provide detailed information on interactions between healthcare professionals and EHRs, which might be used to study the composition and structures of healthcare teams and networks using social network analysis. Furthermore, by combining data from the EHR and patient outcomes, researchers might be able to correlate data about interprofessional practice with patient outcomes.
Social network analysis has been used in several capacities in healthcare research. For example, epidemiologists have used the technique to map transmission of communicable diseases and spread of health behaviors (Christakis & Fowler, 2007, 2008). Other researchers have used social network analysis to examine the dissemination of knowledge with survey and Medicare claims data (Keating, Ayanian, Cleary, & Marsden, 2007; Pollack, Weissman, Bekelman, Liao, & Armstrong, 2012). Previous studies in the clinical and health administration literature have used network principles to characterize the existing critical care network (Iwashyna, Christie, Moody, Kahn, & Asch, 2009) and identify opinion leaders (Kravitz et al., 2003; Soumerai et al., 1998). In non-healthcare settings (Borgatti, Mehra, Brass, & Labianca, 2009), social network analysis has been used to analyze how interactions occur in teams (Chambers, Wilson, Thompson, & Harden, 2012). However, few studies have used network analysis to describe healthcare teams, develop interventions to improve interprofessional practice, or examine the interactions of healthcare professionals mediated by EHRs (Rangachari et al., 2010), (Zheng, Mei, & Hanauer, 2011).
Describing networks of healthcare professionals with EHR data has advantages compared to other traditional data sources for network analysis. Collecting survey data to map a social network is laborious, time inefficient, costly, and possibly biased by the observation process (Keating et al., 2007). Data from administrative claims may be incomplete and may not reflect the valuable input from important team members (e g. nurses) that do not bill for services (Pollack et al., 2012). As such, analyzing EHR data provides a large amount of data efficiently and may provide a valuable addition to other approaches for describing networks of healthcare professionals and teamwork in healthcare.
In this exploratory descriptive study, our research aim is to use the access-log data from the EHR to construct the network of the healthcare professionals providing cancer care to one subset of patients at an academic medical center. Using social network analysis, we endeavored to visually and mathematically represent the electronic communication and functional state of care at a health system (O’Malley & Marsden, 2008). We sought to describe the network structure for each patient and of the entire network and make comparisons between individual patients’ networks. Our approach is grounded in the conceptual view that there is direct transmission of information from one healthcare professional to another as they access the same patient’s records (Borgatti et al., 2009). Variation in networks across patients may lead to different levels of information sharing among healthcare professionals and may be related to health outcomes such as inpatient costs, readmission rates, and hospital length of stay (Uddin, 2016; Uddin, Kelaher, & Piraveenan, 2015). Based on our findings, we discuss potential implications for this approach to measuring and improving interprofessional practice in cancer care.
METHODS
Setting, Patients, and Data Extraction
The study was conducted at an academic medical center and approved by its institutional review board. A total of 100 newly-diagnosed surgical colorectal cancer patients receiving treatment in 2013 and 2014 were selected at random. Data represented all care provided by the medical center, including both inpatient and outpatient care. We identified the EHR for each of these patients in the center’s EHR, Cerner. The Cerner EHR system supports an enterprise-wide view of clinical information to coordinate and document patient care. The comprehensive system has three integrated components: clinical documentation and management, patient portal, and revenue cycle solutions. We used access logs of the clinical documentation and management system in this study. We limited our study to data from one month before the official date of cancer diagnosis per the center’s cancer registry to nine months after the date of cancer diagnosis. We extracted detailed access-log information from the EHR to create a chronological data set of access to each patient’s EHR. The data include the patient’s identity, the healthcare professional’s identity, the role of the healthcare professional, the date and time of access, and the action performed on the record (e.g., view orders, write note). A sample of access-log data is provided in the Appendix file 1.
Dataset description
For the 100 randomly selected patients, there were approximately 2.45 million records of access logs by more than 6,800 unique users. Over 150 healthcare professional roles were defined in the EHR, and nurses, housestaff physicians. Three physicians on the research team reviewed and discussed the list of healthcare professional roles and categorized all these users into three groups: core patient care team (such as physicians and nurses), support team (such as radiology technicians, lab technicians), and administrative team (such as insurance professionals). The core group of professionals was used to perform the data analysis, excluding roles such as lab technicians, students, and database administrators to create a final list of 1933 healthcare professionalss of interest.
Data analysis
In order to create a network map for each patient, we ordered each patient’s access log according to its time sequence and used the sequence of accessing records as a surrogate for information transmission between healthcare professionals using the EHR. Each healthcare professional represented a node. We then created a link between healthcare professionals who accessed a patient’s EHR consecutively and used such links to construct a network of healthcare professionals. The assumption is that the two professionals who accessed one patient’s record sequentially are connected (Barnett, Landon, O’Malley, Keating, & Christakis, 2011; Pollack et al., 2012). This methodology attempts to extract the signal from the noise by using large amounts of data and is consistent with the theoretical and empirical knowledge about healthcare teams described in the literature (Borgatti et al., 2009; Pollack et al., 2012). While this is assumption requires validation, it provides a base for constructing provider networks from EHR access-log data (see Appendix). The access-log information could then provide combined to describe the overall network structure.
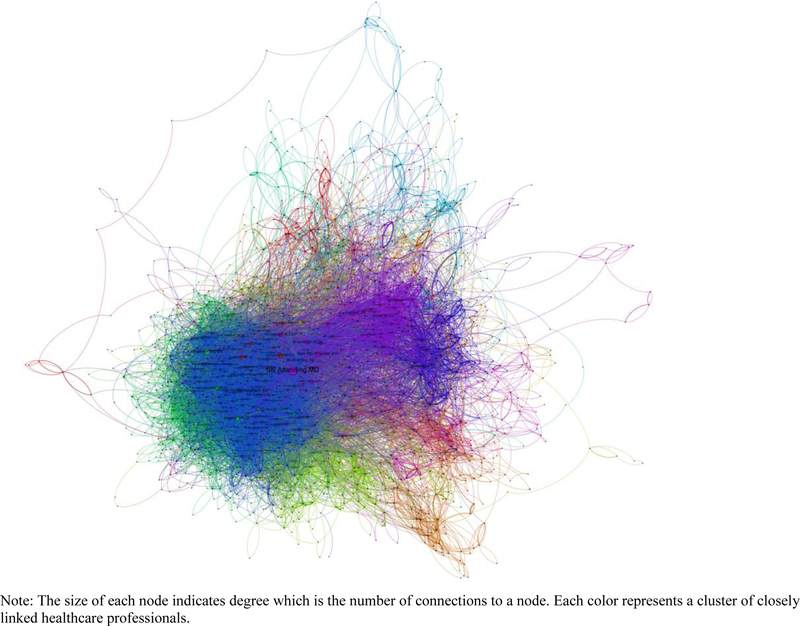
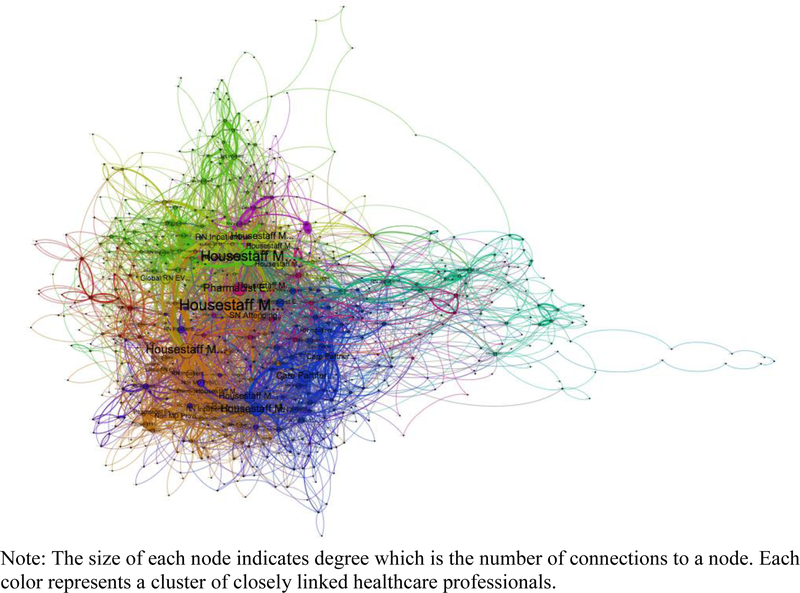
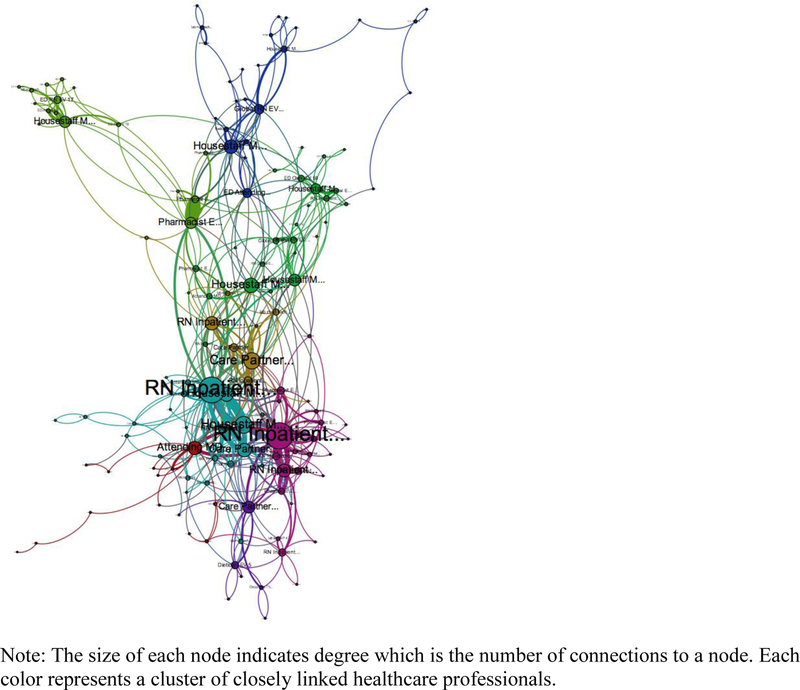
Network maps were analyzed to describe the relationships between healthcare professionals. We created a global network based on all 100 patients’ data (Figure 1) and also individual networks for each patient (Figures 2 and 3). Pairs of healthcare professionals with more frequent links are represented with a thicker line.
Figure 1.
Global network of core healthcare professionals for 100 cancer patients
Figure 2.
Network of healthcare professionals for Patient A
Figure 3.
Network of healthcare professionals for Patient B
For both global and individual networks, we analyzed node-level and network-level characteristics such as connectivity, centrality, and clustering. Network analysis is a multidisciplinary social science where the meanings of many measures may vary depending on the context. Table 1 defines key network terms and measures that are relevant for studying networks of healthcare professionals. Both node-level (i.e., individual level) and network-level (i.e., system or team level) measures are presented with examples pertinent to communication between healthcare professionals and possible hypotheses related to each concept. Briefly, the links between nodes can be analyzed mathematically to define parameters such as the shortest path between any two nodes (i.e. the distance), how often a node is most important for connecting other nodes (i.e. the node’s betweenness centrality), the number of links for an average node (i.e. the average degree), how interconnected a network is (i.e. the average clustering coefficient), and the number of subgroups in a network (i.e. the modularity). While network analysis has not been applied widely to healthcare, it may provide some new insights that can improve practice and outcomes (Uddin, 2016; Uddin, Kelaher, & Piraveenan, 2015). We used SAS and Gephi to manage, visualize, and analyze the networks and data (Gephi team, 2016; SAS Institute, Inc, 2015).Data presented primarily focus on the global network of all 100 patients.
Table 1.
Terms and definitions in network analysis
| Term | Definition | Example in This Study | Possible Considerations for Care Delivery and Outcomes |
|---|---|---|---|
| Fundamental Terms | |||
| Node (or circle) | A member of a network | A healthcare professional | What professionals are involved in patient care? Are all necessary professionals involved? |
| Link (or tie or edge) | A connection between two nodes or network members | The connection between a professional who accessed a patient’s EHR after another professional | Is patient information transmitted between professionals through writing and reviewing notes in EHR? Who communicates with whom through the EHR? |
| Path | A sequence of nodes and links that connects two nodes | Communication between two professionals mediated by other professionals | How are two professionals connected in the EHR? How do the lengths of paths affect care? |
| Cluster (or subgroup) | A subset of nodes more closely connected to each other than to nodes external to the subset | A group of professionals who communicate more frequently with each other than with other professionals | Are there distinct clusters in the network of healthcare professionals? Are the clusters associated with workflow, professional boundaries, patient circumstances, or patient outcomes? |
| Node-level measures | |||
| Degree | The number of links a node has | The number of other professionals with whom a professional directly communicates. |
Do certain professionals have more links than other professionals? Does the number of other professionals to whom a certain professional is linked affect information transmission or patient outcomes? |
| Distance | The number of connections on the shortest path between two nodes | The minimum number of intermediate steps needed to transmit information between two professionals | What is the distance between two specifc professionals? Are longer distances associated with communication and health outcomes? |
| Betweenness centrality | Across the entire network, how often a node appears on the shortest path between pairs of other nodes | The extent to which a certain professional mediates the shortest communication path between other professionals | Who plays a central role in mediating communication among other professionals? Which other professionals are connected by the most central professionals? |
| Closeness centrality | The distance (i.e. length of the shortest path) between a node and all other nodes in the network | The minimum numbers of intermediaries by which a professional can communicate with all other professionals in the network | Who plays more central roles in communicating with other professionals either directly or via the shortest paths? How central are different types of professionals to the network? |
| Clustering coefficient | The number of actual links for a node divided by the number of possible links for a node (i.e. a node linked to all other members of a network would have a value of 1) | The proportion of professionals in a network directly communicating with a professional divided by the number of all professionals in the network. | Which professional are more or less connected within the network? What factors contribute to professionals being a greater part of the network clusters? |
| Network-level measures | |||
| Network size | The number of nodes in the network | The number of professionals involved in providing care to a patient | How does the size of a healthcare network or team affect communication behaviors among professionals? How does the size of a healthcare network or team affect patient outcomes? |
| Diameter | Longest distance between any two nodes in the network | Longest distance information must traverse between healthcare professionals | How tightly are professionals connected in this network? Do networks with larger diameters have worse communication or patient outcomes? |
| Average degree | The average number of links that nodes in the network have | The average number of other professionals with whom members of a network are linked |
Is the average number of other professionals with whom members of a healthcare network are directly linked correlated with the accuracy and completeness of information transmitted or patient outcomes? |
| Average path length | Average distance of the shortest path between all pairs of nodes | The average minimum number of links between all pairs of professionals | Is the average path length between all pairs of professionals correlated with the accuracy and completeness of information transmitted or patient outcomes? |
| Average clustering coefficient | The average of the clustering coefficient for all nodes in the network | Averaged for all professionals, the proportion of professionals in a network directly linked to each professional divided by the total number of professionals in a network | How tightly clustered (i.e., having a higher clustering coefficient) are different networks? How do variations in clustering affect communication efficiency, accuracy, and outcomes? |
| Modularity | A measure of whether a network decomposes into subgroups | The number and size of various subgroups of health professionals | Do subgroups exist in healthcare networks? Are subgroups associated with profession, setting, or other factors? |
RESULTS
Diameter and Clustering
For the global network of all 100 patients, the diameter (i.e. the shortest path between the furthest two nodes in the network) was 14. The average path length (i.e. the average minimum distance between any two nodes) was 4.09. The relatively large diameter and long average path length imply that information cannot spread easily throughout the network.The average clustering coefficient, a measure of network density, was 0.178 (range: 0–1), meaning professionals were only directly linked to about 18 percent of the other professionals in the network on average. The combination of a low clustering coefficient and an average path length of 4.09 indicated that serendipitous or chance interactions among healthcare professionals were unlikely.
Degree
Healthcare professionals worked together in a complex, intra- and interprofessional manner (Figure 1). Professionals were connected to an average of 5.8 other professionalsbut showed wide variation in degree with a range between 1 and 277. A degree distribution plot, appendix file 2, is markedly skewed toward the left. Over 20 professionals were connected to over 100 other professionals.
Centrality
Betweenness centrality indicates the extent to which a provider is part of the shortest path between two other providers in the network. The Appendix file 3 shows the variation and distribution of betweenness centrality for the global network. The central purple node, an attending physician, in the middle of Figure 1 had the highest betweenness centrality score and eigenvector centrality score. This physician is mathematically the most central professional in the network. A total of 13 individuals had an eigenvector centrality greater than 0.5. They are among the providers with highest betweenness centrality scores. All were registered nurses, housestaff physicians, or attending physicians.
Modularity
The color and shape of a node in Figure 1 indicate in which subgroup each professional worked. There were 13 subgroups based on the data. The size of subgroup ranged from 3 professionals to 320 professionals (Appendix file 4). Attending physicians did not always have the highest betweenness centrality within these 13 subgroups. The largest subgroup was dominated by inpatient nurses and housestaff physicians. The second largest subgroup was led by outpatient nurses and attending physicians. The modularity score of this network was high at 0.48. A high modularity score, like this one, indicates a sophisticated internal structure with significant crosslinking while a low modularity score indicates a number of highly separated clusters.
Patient-centric care networks
Figures 2 and 3 show the networks of all professionals for two randomly selected patients. Table 2 compares the key measures of these two networks with the global network.
Table 2.
Network characteristics of the global network and the patient-specific networks of patients A and B
| Definition | Global | Patient A | Patient B | |
|---|---|---|---|---|
| Network size | Number of professionals | 1,933 | 577 | 143 |
| Average degree | Avg number of links per professional | 5.8 | 6.2 | 3.4 |
| Network diameter | Shortest path between most distant professionals | 14 | 17 | 12 |
| Average path length | Average path length between all professionals | 4.1 | 3.7 | 4.1 |
| Average clustering coefficient | Proportion of possible links | 0.18 | 0.25 | 0.26 |
| Modularity score | A measure of the tendency to form subgroups | 0.48 | 0.45 | 0.52 |
| Most “central” person | Most commonly found on shortest path between any two professionals | An attending physician | A housestaff physician | A registered nurse |
Patient A’s network was similar in many respects to the global network. It contained 577 professionals or nodes, and these professionals had 6,011 links. Intra- and interprofessional links were observed in patient A’s network. The network diameter was 17, slightly higher than the global network. The average path length was 3.7 and the average degree of all nodes is 6.2, describing a slightly denser network than the global network. The average clustering coefficient was 0.25 and modularity score was 0.45, similar to the global network. There were 11 clusters, ranging from 3 professionals to 113 professionals. A housestaff physician had the highest centrality.
In contrast, the network for Patient B was much smaller. It was comprised of 143 professionals and 727 links. Similar intra- and interprofessional links were observed. The network diameter was 12 with an average path length was 4.1. The average degree of all professionals was 3.4, a less dense network than with patient A. The average clustering coefficient was 0.26 and modularity score was 0.52 with 8 clusters ranging from 2 professionals to 26 professionals. A registered nurse had the highest centrality.
DISCUSSIONS
This exploratory, descriptive study demonstrated that the access-log data from EHR could be used to describe the network structure of care delivered to cancer patients. Using social network analysis, it is feasible to identify and examine structural characteristics of networks that emerged from interactions between healthcare professionals mediated by their access to patients’ EHRs. By describing some baseline data of the global network for cancer care, we were also able to compare network measures between the global network and two individual patients’ networks. Our findings have several implications for improving healthcare.
Understanding care to further research, training, and patient outcomes.
We described a complex network with interconnected clusters. While care has been described as ranging from teams to networks (Reeves, Lewin, Espin, & Zwarenstein, 2011), our data suggested the co-existence of many different structures for interprofessional care in the same patient. In addition, clustering, both across the entire network and in individual networks, seemed to correlate with location; for example, inpatient professionals were in a separate cluster from outpatient professionals. In terms of leadership, physicians and nurses were often the most central members of the networks, but, as measured by having the highest betweenness centrality, attending physicians were not necessarily always the most central members. Individual networks varied on whom was most central in each patient’s networks. Finally, the size and complexity of the network made serendipitous interactions unlikely. Each of these observations about this complex system has implications for inteprofessional cancer care.
The dynamic nature of healthcare teams.
Team-based approaches have been broadly promoted to improve health care (Bodenheimer, 1999; Institute of Medicine, 2014). The Institute of Medicine defined a team as a group of healthcare professionals working interdependently to achieve a shared goal (Institute of Medicine, 2001). Teams have been advocated as an imperative in the redesign of healthcare delivery systems, a cornerstone of safer healthcare organizations, the critical components of a “culture” of healthcare quality and safety, and a National Patient Safety Goal (Institute of Medicine, 2000, 2006, 2014). However, we are only at an early stage of understanding complex team behaviors in health care (Lemieux-Charles & McGuire, 2006; Taplin et al., 2015). We found that the networks of healthcare professionals are large and complex in terms of the number of professionals, the diameter of the network, and the connections between professionals. Subgroups, as measured by modularity, are common and may represent true teams, but these subgroups are also closely connected to the overall network. These healthcare teams may emerge from the needs of a patient and have fluid boundaries affected by organizational factors. If supported with further analyses, this data suggests: 1) team structures are not simple, 2) team structures vary greatly across patients, and 3) leaders cannot rely on serendipity to ensure team formation and optimal interprofessional care. Using network analysis techniques that assess how collaboration changes over time would build on these findings. In addition, subgroupss and the connections between subgroups might represent reasonable targets for further study and possible interventions to improve interprofessional care.
Implications for patient outcomes.
Global networks and individual networks differed, most notably by which role was most central. While attending physicians were most central overall, housestaff physicians and nurses were most central for specific patients. Contextual factors, such as inpatient versus outpatient care, may be a factor here and should be studied. Understanding this variation can help to target interventions. For example, nursing-directed interventions may have more value in certain contexts or for certain patients. These findings would have important implications for coordinating care by defining who best can integrate all the information involved in a patient’s care and how different healthcare professionals can provide leadership that bridges different subgroupss of care. Since failures in the integration of information underpin many medical errors and wasteful care (IOM. 2001), this aspect of interprofessional care is essential to improving patient outcomes and the patient experience.
Interprofessional education.
We found that intra- and interprofessional links were very prevalent. While attending physicians, housestaff physicians, and nurses played the most central roles in the care of surgical colorectal cancer patients, other professionals also played essential roles in the network. With the complexity of the network and the poorly defined boundaries of subgroups, the capacity of individuals to bridge subgroups and settings is essential to overcome the unlikelihood of serendipitous interactions between professionals. This is a prime target for education and training (Dow AW et al, 2017). Professionals should be given the knowledge, skills, and attitudes to think beyond their professional and organizational subgroups in order to better support patients as they move through this complex system. While nurses and physicians were defined by our analysis as the most central members of networks and, thus, prime targets for this intervention, other health professions may also be candidates for training and, with this training, have greater roles to help patients navigate cancer care in a safe and satisfying manner.
Future research.
The innovations of this project are twofold. First, we applied theoretical concepts and basic methods of network analysis to develop a systematic approach to quantitatively describe the team interaction within a healthcare system as a basis for possible improvements in care. Second, we systematically mined and analyzed access-log data as an efficient source of information about interactions among healthcare professionals. These approaches need further refinement and validation but may be powerful tools for future research. Moreover, our findings and future studies that systematically investigate the effects of EHR network structures on team commutation and patient outcomes will inform the design of new EHR functions or tools to facilitate team communication in care delivery, which will ultimately improve interprofessional practices in cancer care. Some other possible next steps in research include: defining how networks, subgroups, and central members change over time; identifying whether network measures correlate with other challenges in healthcare such as health disparities based on race or socioeconomic status; using network data to develop and target interventions; and determining whether and how this approach can measure the impact of interventions.
The limitations of this approach are several (Marsden, 1990). First, we assumed that sequential access of patient’s EHR signifies a connection between two individuals and sharing of information or knowledge based on the shared patient theory (Barnett, Landon, O’Malley, Keating, & Christakis, 2011; Pollack et al., 2012). Further study is important to strengthen the validity of this approach and explore other approaches of constructing communication networks from EHR data. Second, as an exploratory study, we aimed to illustrate the utility of using access logs to examine the composition and structures of healthcare teams that virtually emerged in the care delivery system. The real potential of this approach lies in finding the impacts of team composition and structures on patient outcomes and designing interventions to improve outcomes based on such findings. This requires future studies combining access logs data and outcomes. Third, our analysis drew on EHR chart accesses to describe the network structure in care delivery. The EHR system does not provide highly detailed information such as note accesses, which would have enhanced the precision of our analysis of connections between providers. Fourth, this is a single institution study on a limited subset of patients. In addition, the two individual patients described were randomly selected and may not be typical. As such, the generalizability of our findings cannot be assured, and further study is needed in a broader, multi-institutional manner.
CONCLUSIONS
Access-log information from EHRs described relationships between healthcare professionals caring for cancer patients. Using social network analysis, it was feasible to identify and examine structural characteristics of the healthcare professionals in these networks. The networks were large, heterogeneous, densely connected, and comprised of subgroups. Findings from this exploratory study and future research may be able to associate network measures with specific healthcare team behaviors or specific healthcare outcomes and inform interventions to improve the design of healthcare teams and the training of healthcare professionals in order to enhance the quality of patient care.
Supplementary Material
Acknowledgements
We would like to thank all colleagues at VCU Massey Cancer Center Informatics Core. This study was also supported by resources within the Population Sciences program of UVA Cancer Center.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Ethical approval to conduct the studies reported in this paper has been granted by the VCU Institutional Review Board.
Additional file
Additional file 1: A sample of access-log data
Additional file 2: node degree distribution (global network)
Additional file 3: distribution of betweenness centrality (global network)
Additional file 4: distribution of the size of subgroups (global network)
References
- Ammenwerth E, & Spötl H-P (2009). The time needed for clinical documentation versus direct patient care. A work-sampling analysis of physicians’ activities. Methods of Information in Medicine, 48(1), 84–91. [PubMed] [Google Scholar]
- Barnett ML, Landon BE, O’Malley AJ, Keating NL, & Christakis NA (2011). Mapping Physician Networks with Self-Reported and Administrative Data. Health Services Research, 46(5), 1592–1609. 10.1111/j.1475-6773.2011.01262.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer T (1999). The Movement for Improved Quality in Health Care. New England Journal of Medicine, 340(6), 488–492. 10.1056/NEJM199902113400621 [DOI] [PubMed] [Google Scholar]
- Borgatti SP, Mehra A, Brass DJ, & Labianca G (2009). Network Analysis in the Social Sciences. Science, 323(5916), 892–895. 10.1126/science.1165821 [DOI] [PubMed] [Google Scholar]
- Chambers D, Wilson P, Thompson C, & Harden M (2012). Social Network Analysis in Healthcare Settings: A Systematic Scoping Review. PLoS ONE, 7(8), e41911 10.1371/journal.pone.0041911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2007). The Spread of Obesity in a Large Social Network over 32 Years. New England Journal of Medicine, 357(4), 370–379. 10.1056/NEJMsa066082 [DOI] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2008). The Collective Dynamics of Smoking in a Large Social Network. New England Journal of Medicine, 358(21), 2249–2258. 10.1056/NEJMsa0706154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dow AW, Zhu X, Sewell D, Banas CA, Mishra V, Tu SP (2017).Teamwork on the rocks: Rethinking interprofessional practice as networking. Journal of Interprofessional Care, 31(6). 677–678. 10.1080/13561820.2017.1344048 [DOI] [PubMed] [Google Scholar]
- Driskell JE, Radtke PH, & Salas E (2003). Virtual Teams: Effects of Technological Mediation on Team Performance. Group Dynamics: Theory, Research, and Practice, 7(4), 297–323. 10.1037/1089-2699.7.4.297 [DOI] [Google Scholar]
- Gephi team. (2016). Gephi 091. [Google Scholar]
- Hripcsak G, Vawdrey DK, Fred MR, & Bostwick SB (2011). Use of electronic clinical documentation: time spent and team interactions. Journal of the American Medical Informatics Association : JAMIA, 18(2), 112–117. 10.1136/jamia.2010.008441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2000). To Err Is Human: Building a Safer Health System (Kohn LT, Corrigan JM, & Donaldson MS, Eds.) (1 edition). Washington, D.C: National Academies Press. [PubMed] [Google Scholar]
- Institute of Medicine. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century (1 edition). Washington, D.C: National Academies Press. [PubMed] [Google Scholar]
- Institute of Medicine. (2006). Preventing Medication Errors: Quality Chasm Series (Aspden P, Wolcott J, Bootman JL, & Cronenwett LR, Eds.) (1 edition). Washington, DC: National Academies Press. [Google Scholar]
- Institute of Medicine. (2014). Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis (Levit L, Balogh E, Nass S, & Ganz PA, Eds.) (1 edition). Washington, D.C: National Academies Press. [PubMed] [Google Scholar]
- Iwashyna TJ, Christie JD, Moody J, Kahn JM, & Asch DA (2009). THE STRUCTURE OF CRITICAL CARE TRANSFER NETWORKS. Medical Care, 47(7), 787–793. 10.1097/MLR.0b013e318197b1f5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating NL, Ayanian JZ, Cleary PD, & Marsden PV (2007). Factors Affecting Influential Discussions Among Physicians: A Social Network Analysis of a Primary Care Practice. Journal of General Internal Medicine, 22(6), 794–798. 10.1007/s11606-007-0190-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz RL, Krackhardt D, Melnikow J, Franz CE, Gilbert WM, Zach A, … Romano PS (2003). Networked for change? Identifying obstetric opinion leaders and assessing their opinions on caesarean delivery. Social Science & Medicine (1982), 57(12), 2423–2434. [DOI] [PubMed] [Google Scholar]
- Lemieux-Charles L, & McGuire WL (2006). What Do We Know about Health Care Team Effectiveness? A Review of the Literature. Medical Care Research and Review, 63(3), 263–300. 10.1177/1077558706287003 [DOI] [PubMed] [Google Scholar]
- Marsden PV (1990). Network Data and Measurement. Annual Review of Sociology, 16(1), 435–463. 10.1146/annurev.so.16.080190.002251 [DOI] [Google Scholar]
- O’Leary KJ, Liebovitz DM, & Baker DW (2006). How hospitalists spend their time: insights on efficiency and safety. Journal of Hospital Medicine: An Official Publication of the Society of Hospital Medicine, 1(2), 88–93. 10.1002/jhm.88 [DOI] [PubMed] [Google Scholar]
- O’Malley AJ, & Marsden PV (2008). The Analysis of Social Networks. Health Services & Outcomes Research Methodology, 8(4), 222–269. 10.1007/s10742-008-0041-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack CE, Weissman G, Bekelman J, Liao K, & Armstrong K (2012). Physician Social Networks and Variation in Prostate Cancer Treatment in Three Cities. Health Services Research, 47(1pt2), 380–403. 10.1111/j.1475-6773.2011.01331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangachari P, Rissing P, Wagner P, Rethemeyer K, Mani C, Bystrom C, … Gillespie W (2010). A baseline study of communication networks related to evidence-based infection prevention practices in an intensive care unit. Quality Management in Health Care, 19(4), 330–348. 10.1097/QMH.0b013e3181fa36a4 [DOI] [PubMed] [Google Scholar]
- Reeves S, Lewin S, Espin S, & Zwarenstein M (2011). Interprofessional Teamwork for Health and Social Care (1 edition). Wiley-Blackwell. [Google Scholar]
- Institute SAS, Inc. (2015). SAS 9.3 Cary, NC: SAS Institute, Inc. [Google Scholar]
- Soumerai SB, McLaughlin TJ, Gurwitz JH, Guadagnoli E, Hauptman PJ, Borbas C, … Gobel F (1998). Effect of local medical opinion leaders on quality of care for acute myocardial infarction: a randomized controlled trial. JAMA, 279(17), 1358–1363. [DOI] [PubMed] [Google Scholar]
- Taplin SH, Weaver S, Salas E, Chollette V, Edwards HM, Bruinooge SS, & Kosty MP (2015). Reviewing Cancer Care Team Effectiveness. Journal of Oncology Practice, JOP.2014003350 10.1200/JOP.2014.003350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin S (2016). Exploring the impact of different multi-level measures of physician communities in patient-centric care networks on healthcare outcomes: A multi-level regression approach. Scientific Reports, 6, 20222 10.1038/srep20222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin S, Kelaher M, & Piraveenan M (2015). Impact of Physician Community Structure on Healthcare Outcomes. Studies in Health Technology and Informatics, 214, 152–158. [PubMed] [Google Scholar]
- Zheng K, Mei Q, & Hanauer DA (2011). Collaborative search in electronic health records. Journal of the American Medical Informatics Association: JAMIA, 18(3), 282–291. 10.1136/amiajnl-2011-000009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.