Abstract
We evaluated associations between levels of alcohol use and HIV care continuum components using national Veterans Aging Cohort Study data for all patients with HIV and AUDIT-C screening (2/1/2008–9/30/14). Poisson regression models evaluated associations between alcohol use levels (non-drinking, low-, medium-, high-, and very high-level drinking) and: 1) engagement with care (documented CD4 cells/μl or viral load copies/mL labs), 2) ART treatment (≥1 prescription), and 3) viral suppression (HIV RNA<500 copies/ml) within one year. Among 33,224 patients, alcohol use level was inversely associated with all care continuum outcomes (all p<0.001). Adjusted prevalence of care engagement ranged from 77.8% (95% CI 77.1%–78.4%) for non-drinking to 69.1% (66.6%–71.6%) for high-level drinking. The corresponding range for ART treatment was 74.0% (73.3%–74.7%) to 60.1% (57.3%–62.9%) and for viral suppression was 57.3% (56.5%–58.1%) to 38.3% (35.6%−41.1%). Greater alcohol use is associated with suboptimal HIV treatment across the HIV care continuum.
Keywords: HIV, care continuum, treatment cascade, antiretroviral therapy, viral suppression, alcohol
INTRODUCTION
In the U.S., approximately 1.1 million people are living with human immunodeficiency virus (HIV).1–4 Though infectious and previously fatal, HIV has increasingly become a preventable chronic disease. This epidemiologic transition was made possible through medical advances— and antiretroviral therapy (ART) specifically—that help preserve health and decrease risk of transmission.5,6 These advances have highlighted the importance of ensuring all persons living with HIV know their status and obtain recommended care to reduce HIV-related morbidity and mortality and new infections. Thus, national and international agencies now monitor care targets considered essential for effective treatment and prevention of future infections to gauge progress and care gaps.6–12 These targets, collectively referred to as the HIV care continuum,6,7 include: 1) diagnosis, 2) linkage to medical care, 3) engagement with HIV medical care, 4) treatment with ART, and 5) achievement of viral suppression.
Alcohol use is common among people living with HIV (PLWH). In the U.S., 54% of PLWH report any alcohol use and 25% report any heavy episodic drinking, an unhealthy pattern of use known to adversely influence multiple health outcomes.13 Alcohol use is associated with HIV care including: testing14–16 and diagnosis;17 care engagement,18 quality,19 and retention;20–23 receipt and use of ART;24,25 and potentially viral suppression.26–28 Thus, alcohol use may represent a modifiable influence on HIV care continuum targets.29,28
However, previous studies offer limited information on the influence of alcohol use on HIV care continuum targets in the U.S. for several reasons. First, most studies have been conducted within samples of PLWH living outside of the U.S.17,24,25,27 or in recruited samples with limited generalizability.18,30,31 Second, existing studies do not assess multiple components of the HIV care continuum in a single sample of PLWH, limiting understanding of the effect of alcohol use across care targets. Third, studies have used limited measures of alcohol use, and most have assessed dichotomous measures of consumption and/or severity as predictors,21,23 limiting understanding of levels of consumption at which risk of undertreatment is increased.
The U.S. Veterans Health Administration (VA) offers a unique opportunity to investigate associations between alcohol use and clinical components of the HIV care continuum in a large national sample of PLWH receiving healthcare, a population who should theoretically have equal access to all components of the HIV care continuum. The VA is the nation’s largest integrated healthcare system and largest provider of HIV care.32,33 The VA also routinely screens nearly all outpatients annually for unhealthy alcohol use34 using a validated screening instrument35 shown to be a strong scaled measure of alcohol consumption.36 Therefore, in a national sample of VA PLWH, we evaluated the association between level of alcohol use and three clinical components of the HIV care continuum: engagement with HIV care, treatment with ART, and viral suppression. We hypothesized that level of alcohol use would have a dose-dependent association with HIV care continuum measures such that greater levels of alcohol use would be associated with decreased receipt and worse outcomes of care.
METHODS
Data Source and Sample.
This retrospective cohort study used national electronic health records (EHR) data from the Veterans Aging Cohort Study (VACS)32,37 to identify all VA patients with documented HIV between 2/1/2008 and 9/30/2014 who also had documented alcohol screening. International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to identify HIV infection, defined as documentation of 2 outpatient or 1 inpatient diagnosis code(s) for AIDS (042) and/or HIV infection (V08).32,38
Measures.
Predictor.
Level of alcohol use was measured using the 3-item Alcohol Use Disorders Identification Test Consumption (AUDIT-C) questionnaire, which is administered annually to over 90% of established outpatients in the VA and documented in the EHR.34 Scores on the AUDIT-C range from 0 to 12, with scores of ≥3 (women)39 and ≥4 (men)40 optimizing sensitivity and specificity for unhealthy alcohol use.35 Each patient’s first documented AUDIT-C score after enrollment in VACS was used to categorize patients into five levels of alcohol use, reflecting non-drinking (AUDIT-C score 0 points), low- (AUDIT-C 1–3 men/1–2 women), medium- (AUDIT-C 4–5 men/3–5 women), high- (AUDIT-C 6–7), and very high- (AUDIT-C 8–12) level drinking. These categories were selected based on previous research demonstrating increased consumption, severity, and probability of alcohol dependence associated with increasing AUDIT-C scores36,41 and previous studies that have identified clinically meaningful differences in risk of medical and surgical outcomes across similar AUDIT-C categories.42–55
Outcome Measures.
Three outcomes were derived to reflect clinical elements of the HIV care continuum. Engagement with HIV care was measured based on the presence of documented CD4 (cells/μl) or viral load (copies/mL) laboratory values. Treatment with ART was defined as having at least one filled prescription for any antiretroviral medication (see Appendix 1 for list of medications). Viral Suppression was measured based on having HIV RNA <500 copies/ml based on the first available lab measure following alcohol screening. All outcomes were assessed in the 0–365 days following the first documented AUDIT-C. Assessment of the first two components of the HIV care continuum—HIV diagnosis and linkage to care—was not possible due to studying a national sample of patients who used VA healthcare and had HIV diagnoses at the time of the study.
Other measures.
Age in years was measured at the time of alcohol screening and categorized (<50, 50–65, >65) for descriptive purposes. Gender (male/female) and race/ethnicity (non-Hispanic black, Hispanic, non-Hispanic white and other/unknown) were measured based on documentation in the EHR. Because HIV care has changed over time, year of AUDIT-C screening was measured. Consistent with previous research,56 ICD-9-CM codes documented in the year prior to alcohol screening were used to generate dichotomous measures of any alcohol use disorder (diagnosis for alcohol abuse, dependence, or alcohol-attributable conditions, e.g., alcoholic cirrhosis), any non-alcohol substance use disorder (diagnosis for opioid, stimulant, cannabis, or other drug use disorders) and any mental health disorder (diagnosis for depressive disorder, anxiety, or serious mental illness including schizophrenia, bipolar disorder, and schizoaffective disorder).
Analyses.
First, descriptive analyses were conducted to describe patient characteristics and the number and proportion of patients with each level of alcohol use. Second, modified Poisson regression models with robust error variances57 were fit to estimate the relative risk and 95% confidence interval (CI) of each binary HIV care continuum outcome for each level of alcohol use relative to non-drinking. Modified Poisson regression models were used to estimate relative rates because outcomes were expected to be common.57 Non-drinking was used as the referent category because we hypothesized based on previous research (summarized in Williams 201628) that the likelihood of HIV care outcomes would be lower (worse) at any level of alcohol use relative to none. Models were first unadjusted and then adjusted for demographics, year of AUDIT-C screening, and any mental health or non-alcohol substance use disorder, to assess the potential influence of alcohol use on HIV care components independent of other factors that may be associated with HIV treatment receipt and outcomes. For each regression model, we tested whether the relationship between level of alcohol use and each binary outcome was linear using orthogonal polynomial contrast tests.
Third, to understand the magnitude of differences, we estimated the predicted prevalence and 95% CI of each outcome for each level of alcohol use using the Poisson regression models. For adjusted models, the predicted prevalence of each outcome was obtained using recycled prediction methods, which hold covariates constant while allowing AUDIT-C category to vary. This approach enables assessment of the magnitude of differences in each HIV care continuum outcome attributable to the level of alcohol use. Because all patients with HIV should be targeted for all components of the care continuum, primary analyses were conducted in the full sample of all patients with HIV and alcohol screening.
Fourth, we undertook three sets of secondary analyses. Consistent with approaches used to monitor progress and identify key HIV prevention and care needs nationally, secondary analyses were conducted to assess two outcomes (treatment with ART and viral suppression) among only those in the subpopulation targeted at that stage. Specifically, we examined treatment with ART only among those who met criteria for HIV treatment engagement and viral suppression only among those being treated with ART. Next, because alcohol use disorder (AUD) is another indicator of alcohol use, and AUD diagnosis may influence HIV care received and/or the extent to which level of alcohol use influences HIV care, we assessed the main effect of AUD on HIV care continuum outcomes, and examined whether AUD modified the effect of levels of alcohol use on care continuum outcomes. Specifically, we repeated primary analyses with AUD as the predictor variable (excluding level of alcohol use) and then, in each model, added level of alcohol use and tested the interaction with AUD. Finally, because the AUDIT-C assessment of non-drinking does not differentiate between persons with lifetime abstinence and those who abstain in response to illness (“sick-quitters”58) we repeated primary analyses only among PLWH reporting past-year alcohol use (AUDIT-C >0) using low-level alcohol use as the referent category.
All analyses were conducted using Stata 14 software.59 The study, including waivers of written consent and HIPAA authorization, was approved by Internal Review Boards at VA Connecticut Healthcare System and VA Puget Sound. The VACS study is approved by Yale University, and this study was overseen and approved by the VACS Alcohol and Behavior Intervention Core.
RESULTS
Between 2/1/2008 and 9/30/2014, there were 33,224 patients with documented HIV and alcohol screening who were thus eligible. Characteristics of the sample are described in Table I. Most were male and age 50 and above; nearly half were of black race/ethnicity. Comorbid mental health and substance use disorders were common—14.2%, 12.8% and 36.4% had a diagnosed alcohol, substance use, and mental health disorder, respectively.
TABLE I.
Characteristics of Veterans Aging Cohort Study VA Patients Living with HIV who had Documented Alcohol Screening Between February 2008 and May 2014 (n=33,224)
| Characteristic | N | (%) |
|---|---|---|
| Demographics | ||
| Age | ||
| <50 | 11,928 | (35.9) |
| 50–64 | 17,813 | (53.6) |
| ≥65 | 3,483 | (10.5) |
| Race/Ethnicity | ||
| Non-Hispanic Black | 16,028 | (48.2) |
| Hispanic | 2,691 | (8.1) |
| Non-Hispanic White | 13,346 | (40.2) |
| Other/Unknown | 1,159 | (3.5) |
| Alcohol and Other Substance Use and Mental Health Disorders | ||
| Any mental health disorder | 12,082 | (36.4) |
| Any non-alcohol substance use disorder | 4,248 | (12.8) |
| Alcohol use disorder | 4,724 | (14.2) |
| Level of Alcohol Use (AUDIT C Score) | ||
| Non-drinking (0) | 15,446 | (46.5) |
| Low-Level (1–3; 1–2 women) | 12,985 | (39.1) |
| Medium-Level (4–5; 3–5 women) | 2,685 | (8.1) |
| High-Level (6–7) | 885 | (2.7) |
| Very High-Level (8–12) | 1,223 | (3.7) |
Among eligible patients, 46.5% had AUDIT-C scores consistent with non-drinking, while 39.1% had AUDIT-C scores consistent with low-, 8.1% with medium-, 2.7% with high-, and 3.7% with very high-level drinking. Further, 25,833 (77.8%) were engaged in HIV treatment in the year following alcohol screening, 21,764 (65.5%) were treated with ART, and 18,449 (55.5%) had achieved viral suppression. Among the 25,833 PLWH who were engaged in HIV treatment, 21764 (84.3%) were treated with ART, and among the 21,764 meeting criteria for ART treatment, 16,826 (77.3%) were virally suppressed.
Patients with medium-, high-, and very high-level alcohol use were significantly less likely than patients with non-drinking to meet criteria for all HIV care continuum outcomes in all models with one exception: in unadjusted analyses, the likelihood of engagement with HIV treatment did not differ for those with high-level alcohol use compared to those with non-drinking at the p<0.05 level (Table II). Findings regarding low-level drinking were mixed (Table II). Specifically, relative to patients with non-drinking, patients with low-level drinking had greater likelihood of engagement in HIV care and treatment with ART in both unadjusted and adjusted analyses. However, likelihood of viral suppression was lower among those with low-level drinking than those with non-drinking in unadjusted analyses, but the two groups did not differ after adjustment for other factors (Table II). There was a significant (inverse) linear trend between level of alcohol use and all three domains of the HIV care continuum in both unadjusted and adjusted analyses.
TABLE II.
Associations between Level of Alcohol Use and Three HIV Care Continuum Targets in a Large National Sample of VA Patients Living with HIV from the Veterans Aging Cohort Study (n=33,224)
| Unadjusted | AdjustedϮ | |||||||
|---|---|---|---|---|---|---|---|---|
| Level of Alcohol Useϒ | RR | [95% CI] | p-value | Test for Linear Trend* | aRR | [95% CI] | p-value | Test for Linear Trend* |
| Engaged in HIV Medical Care | ||||||||
| Non-drinking (0) | 1.00 | [1.00,1.00] | REF | <0.001 | 1.00 | [1.00,1.00] | REF | <0.001 |
| Low-Level (1–3; 1–2 women) | 1.02 | [1.01,1.03] | 0.00 | 1.02 | [1.01,1.03] | 0.00 | ||
| Medium-Level (4–5; 3–5 women) | 0.97 | [0.94,0.99] | 0.01 | 0.96 | [0.94,0.99] | 0.00 | ||
| High-Level (6–7) | 0.96 | [0.93,1.00] | 0.07 | 0.95 | [0.91,0.98] | 0.01 | ||
| Very High-Level (8–12) | 0.91 | [0.88,0.94] | 0.00 | 0.89 | [0.86,0.92] | 0.00 | ||
| Treated with ART | ||||||||
| Non-drinking (0) | 1.00 | [1.00,1.00] | REF | <0.001 | 1.00 | [1.00,1.00] | REF | <0.001 |
| Low-Level (1–3; 1–2 women) | 1.03 | [1.02,1.04] | 0.00 | 1.02 | [1.00,1.03] | 0.03 | ||
| Medium-Level (4–5; 3–5 women) | 0.96 | [0.94,0.99] | 0.00 | 0.95 | [0.93,0.98] | 0.00 | ||
| High-Level (6–7) | 0.92 | [0.87,0.96] | 0.00 | 0.91 | [0.87,0.95] | 0.00 | ||
| Very High-Level (8–12) | 0.81 | [0.77,0.85] | 0.00 | 0.81 | [0.77,0.85] | 0.00 | ||
| Virally Suppressed | ||||||||
| Non-drinking (0) | 1.00 | [1.00,1.00] | REF | <0.001 | 1.00 | [1.00,1.00] | REF | <0.001 |
| Low-Level (1–3; 1–2 women) | 0.97 | [0.95,0.99] | 0.00 | 0.99 | [0.97,1.01] | 0.25 | ||
| Medium-Level (4–5; 3–5 women) | 0.86 | [0.83,0.90] | 0.00 | 0.88 | [0.85,0.92] | 0.00 | ||
| High-Level (6–7) | 0.80 | [0.75,0.86] | 0.00 | 0.82 | [0.77,0.88] | 0.00 | ||
| Very High-Level (8–12) | 0.64 | [0.60,0.69] | 0.00 | 0.67 | [0.62,0.72] | 0.00 | ||
Ns = 15,446, 13,025, 1832, 2,019, and 902 for non-drinking, low-level drinking, and medium-, high-, and very high-level drinking, respectively.
Adjusted for race, ethnicity, gender, fiscal year of AUDIT-C screening, age, and any mental health and non-alcohol substance use disorders
linear trend tested using orthogonal polynomial contrasts
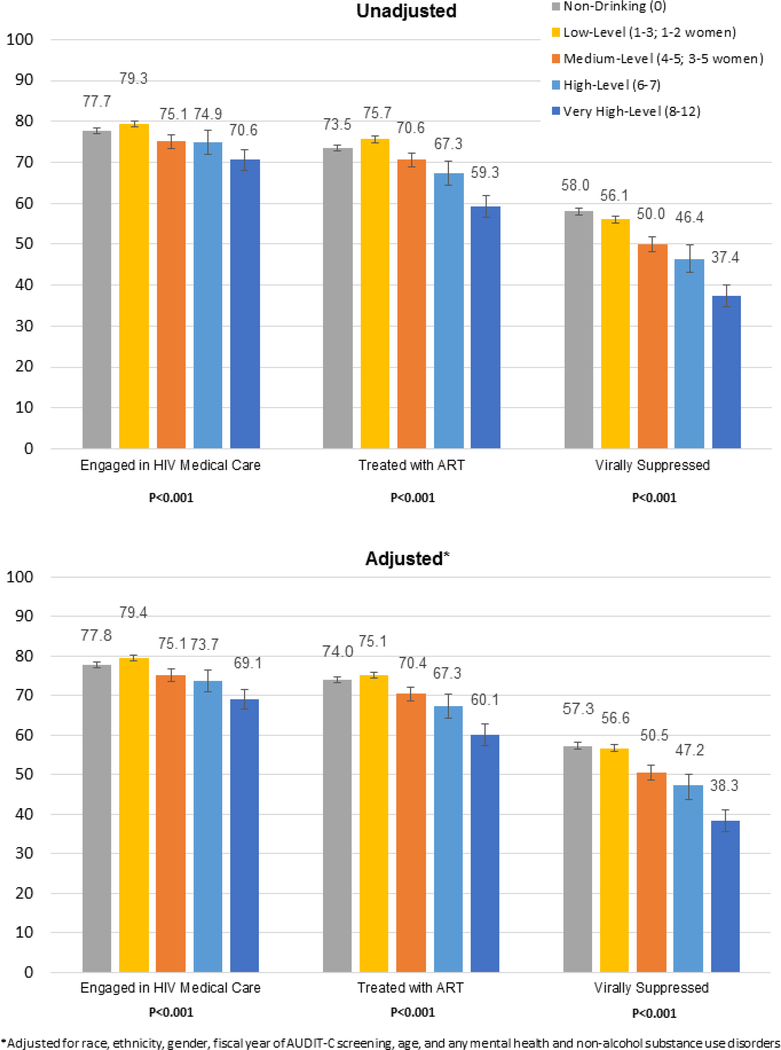
The unadjusted predicted prevalence of patients engaged with HIV medical care ranged from 77.7% (95% CI 77.0% – 78.3%) among patients with non-drinking to 70.6% (95% CI 68.1% – 73.2%) among patients with very-high level alcohol use (Figure 1). The corresponding range for treatment with ART was 73.5% (95% CI 72.8% – 74.2%) to 59.3% (95% CI 56.5% – 62.0%) and for viral suppression was 58.0% (95% CI 57.2% – 58.8%) to 37.4% (95% CI 34.7% – 40.1%). Adjusted prevalence estimates were very similar (Figure 1).
Figure 1.
Percent of VA Patients Living with HIV (n=33,224)) Meeting Three HIV Care Continuum Targets Across Level of Alcohol Use
In secondary analyses assessing treatment with ART only among those who met criteria for HIV treatment engagement, and assessing viral suppression only among those treated with ART, findings were similar (Table III, Appendix 2). Specifically, among patients engaged in care, those with medium-, high-, and very high-level drinking were less likely than those with non-drinking to be treated with ART in both unadjusted and adjusted analyses, though no differences between patients with low-level and non-drinking were observed (Table III, Appendix 2). Among patients treated with ART, patients with all levels of alcohol use were less likely to be virally suppressed than those with non-drinking. Significant linear trends between level of alcohol use and each outcome were observed in all models (Table III, Appendix 2).
TABLE III.
Associations between Level of Alcohol Use and Treatment with Antiretroviral (ART) Medications and Viral Suppression Among VA Patients Living with HIV who Would Be Specifically Targeted for Each Outcome
| Unadjusted | AdjustedϮ | |||||||
|---|---|---|---|---|---|---|---|---|
| Level of Alcohol Useϒ | RR | [95% CI] | p-value | Test for Linear Trend* | aRR | [95% CI] | p-value | Test for Linear Trend* |
| Treatment with ART Among VA PLWH Who Were Engaged in Care (n=25,833) | ||||||||
| Non-drinking (0) | 1.00 | [1.00,1.00] | REF | <0.001 | 1.00 | [1.00,1.00] | REF | <0.001 |
| Low-Level (1–3; 1–2 women) | 1.00 | [0.98,1.01] | 0.46 | 1.00 | [0.98,1.01] | 0.45 | ||
| Medium-Level (4–5; 3–5 women) | 0.95 | [0.93,0.97] | 0.00 | 0.95 | [0.93,0.98] | 0.00 | ||
| High-Level (6–7) | 0.92 | [0.88,0.96] | 0.00 | 0.93 | [0.89,0.97] | 0.00 | ||
| Very High-Level (8–12) | 0.84 | [0.81,0.88] | 0.00 | 0.86 | [0.83,0.90] | 0.00 | ||
| Virally Suppressed Among VA PLWH Who Were Treated With ART (n=21,764) | ||||||||
| Non-drinking (0) | 1.00 | [1.00,1.00] | REF | <0.001 | 1.00 | [1.00,1.00] | REF | <0.001 |
| Low-Level (1–3; 1–2 women) | 0.96 | [0.95,0.97] | 0.00 | 0.98 | [0.96,0.99] | 0.00 | ||
| Medium-Level (4–5; 3–5 women) | 0.93 | [0.90,0.96] | 0.00 | 0.94 | [0.92,0.97] | 0.00 | ||
| High-Level (6–7) | 0.85 | [0.81,0.91] | 0.00 | 0.89 | [0.84,0.94] | 0.00 | ||
| Very High-Level (8–12) | 0.76 | [0.71,0.81] | 0.00 | 0.80 | [0.75,0.85] | 0.00 | ||
Among VA PLWH who were engaged in care, Ns = 11,996, 10,293, 2,017, 663, 864, respectively. Among VA PLWH who were treated with ART, Ns = 10,237, 8,747, 1,637, 520, 623, respectively.
Adjusted for race, ethnicity, gender, fiscal year of AUDIT-C screening, age, and any mental health and non-alcohol substance use disorders
linear trend tested using orthogonal polynomial contrasts
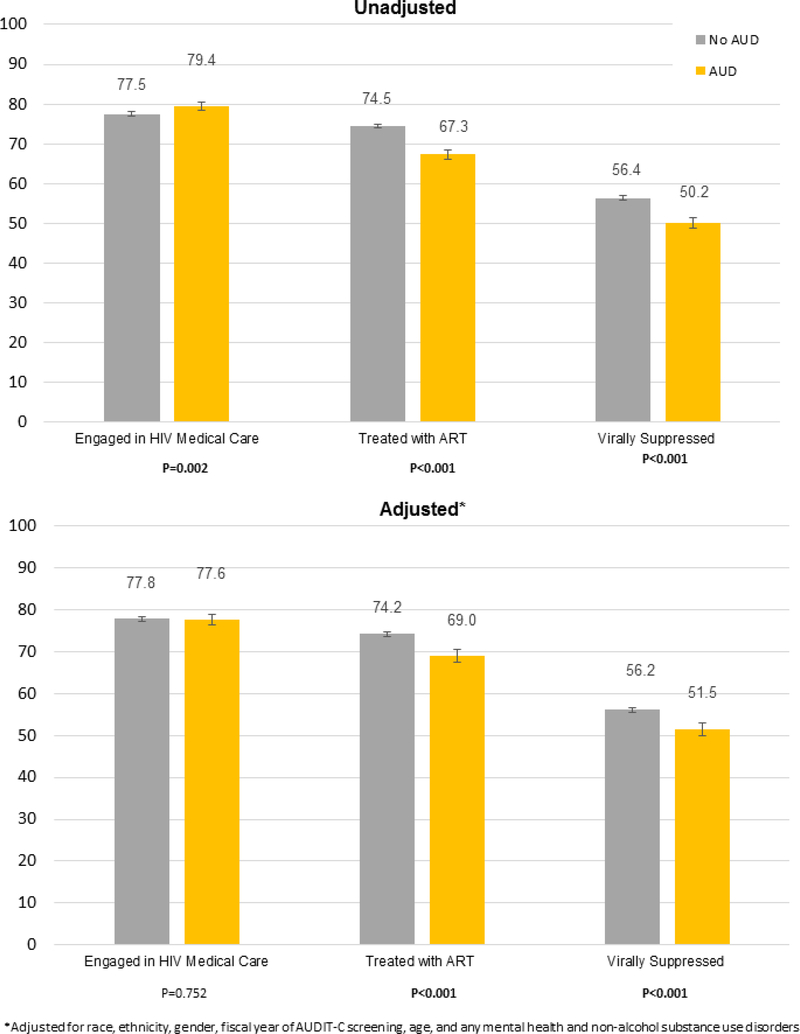
Findings of secondary analyses assessing associations between AUD on HIV care continuum outcomes are presented in Table IV and Figure 2. AUD diagnosis was associated with increased likelihood of engagement in HIV medical care in unadjusted analyses, but no differences were observed after adjustment. AUD diagnosis was associated with decreased likelihood of treatment with ART and viral suppression in both unadjusted and adjusted analyses. Interactions between AUD and level of alcohol use were non-significant in all models (p-values for interaction terms in unadjusted and adjusted models, respectively, were 0.55 and 0.48 for care engagement, 0.27 and 0.26 for ART treatment, and 0.19 and 0.24 for viral suppression). In analyses only among PLWH reporting any past-year alcohol use, with low-level alcohol use as the referent category, relative risks followed a similar pattern as in primary analyses, and significant linear trends between level of alcohol use and each outcome were observed in all models (data not shown).
TABLE IV.
Associations between Alcohol Use Disorder (AUD) diagnosis and Three HIV Care Continuum Targets in a Large National Sample of VA Patients Living with HIV from the Veterans Aging Cohort Study (n=33,224)
| Unadjusted | AdjustedϮ | |||||
|---|---|---|---|---|---|---|
| Alcohol Use Disorder Diagnosis | RR | [95% CI] | p-value | aRR | [95% CI] | p-value |
| Engaged in HIV Medical Care | 1.03 | [1.01,1.04] | 0.00 | 1.00 | [0.98,1.01] | 0.75 |
| Treated with ART | 0.90 | [0.88,0.92] | 0.00 | 0.93 | [0.91,0.95] | 0.00 |
| Virally Suppressed | 0.89 | [0.86,0.92] | 0.00 | 0.92 | [0.89,0.95] | 0.00 |
Adjusted for race, ethnicity, gender, fiscal year of AUDIT-C screening, age, and any mental health and non-alcohol substance use disorders
Figure 2.
Percent of VA Patients Living with HIV (33,224) Meeting Three HIV Care Continuum Targets Across Alcohol Use Disorder (AUD) Diagnosis Status
DISCUSSION
In this national sample of PLWH receiving VA healthcare, progressively higher levels of alcohol use were associated with progressively increased risk of suboptimal HIV treatment across three measures of the HIV care continuum. Relative to PLWH reporting no alcohol use, those with the highest-level alcohol use were nearly 10% less likely to engage in care, nearly 20% less likely to be treated with ART, and more than 30% less likely to be virally suppressed. Only slightly more than one-third of patients with the highest levels of drinking were virally suppressed—the ultimate goal of HIV treatment.
This is the first study to our knowledge to assess the association between levels of alcohol use and multiple stages of the HIV care continuum in a single large U.S. sample. This is also the first study to present estimates of the prevalence of care continuum outcomes both for the entire sample of PLWH and for subsamples of patients specifically targeted at each stage of the HIV care continuum, consistent with U.S. Centers for Disease Control recommendations for monitoring progress and identifying key HIV prevention and care needs.6 Results are consistent with those of previous studies and strengthen the evidence regarding the potential influence of alcohol use on meeting HIV care continuum targets.
Findings specifically support those of earlier studies that identified alcohol use as a risk factor for lower engagement in HIV care,21–23,27,60 treatment with ART 24,25,27 and viral suppression.26,27 Moreover, this study newly demonstrated a dose-dependent association between alcohol use and three HIV care continuum outcomes such that PLWH reporting alcohol use at medium, high, and very high levels had progressively lower likelihood of all care continuum outcomes relative to patients who reported non-drinking. Further, in secondary analyses, diagnosis for AUD was associated with lower likelihood of treatment with ART and viral suppression. However, AUD diagnosis was not associated with engagement in care after adjustment, a finding that could be due to greater illness severity among PLWH with AUD, which may increase motivation to engage in HIV care.
Previous research investigating associations between alcohol use and HIV severity and/or control (i.e., viral suppression), has had mixed findings.27,28,61 Specifically, several studies11,28,61 have suggested that alcohol use may influence viral suppression only through its well-documented association with ART adherence.62 Although other studies have observed a dose-response association between alcohol use and viral suppression, questions remain regarding this association. Given that ART potency has increased over time such that even patients with lower adherence appear to be benefiting,63–65 it is unclear whether alcohol use has a direct biological influence on viral suppression (e.g., via inflammation) or whether other behavioral mechanisms (e.g., non-adherence to ART resulting from alcohol use) are accounting for the dose-response relationship observed.28 In the present study, the association between alcohol use and viral suppression was not attenuated in secondary analyses in the sample of persons treated with ART, and in fact appeared stronger.
Future research is needed to further explore mechanisms underlying associations between alcohol use and viral suppression, especially among persons treated with ART, as well as mechanisms underlying associations observed between alcohol use and other care continuum outcomes. It is possible that associations observed in the present study are influenced by complex community-, healthcare system-, provider-, and patient-level factors. Adjusted models in the present study included factors that may influence HIV treatment and outcomes, yet adjustment did not substantially influence results. Thus, factors measured in this study do not appear to account for associations between alcohol use and HIV outcomes.
This study has several limitations. First, we conducted this study in a national sample of patients who used VA healthcare and had an HIV diagnosis. Therefore, we were unable to assess associations between alcohol use and the first two components of the HIV care continuum (diagnosis and linkage to care), and generalizability may have been limited. Second, it is possible this study did not capture a very small proportion of HIV care that may have been received outside of VA given that a small proportion of patients had viral suppression with no indication of being on ART. However, over 96% of PLWH receiving VA care report receiving ART through VA’s pharmacy,66 and a post-hoc sensitivity analysis removing those who were virally suppressed but not on ART confirmed findings. Third, we assessed level of alcohol use using clinically-documented responses to a 3-item alcohol screen and clinically documented AUD, both of which may underestimate alcohol use. Though clinically-documented AUDIT-C scores have acceptable agreement with patient-reported scores among PLWH,67 clinical screening in the VA may not be conducted in a validated, standardized, or reproducible way68 and may be subject to social desirability bias.69 Fourth, use of EHR data limited measurement of some potential biological/behavioral mechanisms underlying associations between alcohol use and HIV care continuum measures. Further, our ascertainment of past-year diagnoses to measure comorbid conditions in the EHR enabled adjustment for factors that may influence care in real-time, but may be limited given that health conditions experienced prior to the past year or not documented may also be influential. However, our data source was also a strength because it enabled objective measurement of clinical HIV care continuum outcomes, whereas many previous studies have relied on patient-reported clinical outcomes, which may have been biased by social desirability. Additionally, both our predictor and outcome variables may be time-varying, and our study design did not account for changes over time in alcohol use or receipt of HIV care. Further research should be conducted to understand these dynamic associations over time. Finally, while we accounted for potential correlation by conducting secondary analyses only among those PLWH who met criteria for the care continuum target preceding the outcome assessed, it is possible that in the main analyses one of the outcomes may drive results for the other correlated outcomes, which may have resulted in a Type I error.
CONCLUSIONS
This large national study of PLWH is the first to our knowledge to demonstrate a dose-dependent association between alcohol use and multiple components of the HIV care continuum in the U.S. Findings suggest that even in a national integrated care system where HIV care is routinely provided, we are falling short of meeting HIV care continuum targets, particularly among persons with high-level alcohol use. These findings have important clinical implications for optimal treatment and prevention of HIV. The World Health Organization aims for the achievement of 90–90-90 with regard to percent identification, engagement with ART initiation, and viral suppression by 2020.7 To optimize HIV treatment and prevent future infections, targeting interventions across the care continuum towards PLWH with higher levels of alcohol use may be warranted.
Supplementary Material
ACKNOWLEDGMENTS
Funding
This study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (R21AA022866–01; Williams/Bradley PIs) and by COMpAAAS/Veterans Aging Cohort Study (U24-AA020794, U01-AA020790, U01-AA020795,U01-AA020799; U10 AA013566). Dr. Williams is supported by a Career Development Award from VA Health Services Research & Development (CDA 12–276); Dr. Bradley is supported by a mid-career mentoring award from the National Institute on Alcohol Abuse and Alcoholism (K24-AA022128). The funders of this study had no role in study design, data collection, analysis, interpretation and presentation, or in the decision to submit the manuscript for publication. Views presented in the manuscript are those of the authors and do not reflect those of the University of Washington, the Department of Veterans Affairs, or the United States Government.
Footnotes
Conflict of Interest
Dr. Bradley owns stock in Pfizer Pharmaceuticals. All other authors declare no potential conflicts of interest. Preliminary findings of this research study were presented at the Addictions Health Services Research (AHSR) Conference in Madison, WI in September 2017
Ethical Approval: For this type of study, formal consent is not required. The study, including waivers of written consent and HIPAA authorization, was approved by Internal Review Boards at VA Connecticut Healthcare System and VA Puget Sound.
REFERENCES
- 1.Hall HI, Geduld J, Boulos D, et al. Epidemiology of HIV in the United States and Canada: current status and ongoing challenges. J. Acquir. Immune Defic. Syndr May 1 2009;51 Suppl 1:S13–20. [DOI] [PubMed] [Google Scholar]
- 2.Lansky A, Brooks JT, DiNenno E, Heffelfinger J, Hall HI, Mermin J. Epidemiology of HIV in the United States. J. Acquir. Immune Defic. Syndr December 2010;55 Suppl 2:S64–68. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV Surveillance Report: Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas. 2011;23. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data - United States and 6 U.S. dependent areas - 2010 Vol 17: HIV Surveillance Supplemental Report; 2012.
- 5.Taddei TH, Lo Re V 3rd, Justice AC. HIV, aging, and viral coinfections: taking the long view. Curr. HIV/AIDS Rep October 2016;13(5):269–278. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Understanding the HIV Care Continuum. https://www.cdc.gov/hiv/pdf/library/factsheets/cdc-hiv-care-continuum.pdf Atlanta, GA: CDC;2017. [Google Scholar]
- 7.Joint United Nations Programme on HIV/AIDS. 90–90-90—an ambitious treatment target to help end the AIDS epidemic. http://www.unaids.org/en/resources/documents/2014/90-90-90:;2014.
- 8.Skarbinski J, Rosenberg E, Paz-Bailey G, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. Apr 2015;175(4):588–596. [DOI] [PubMed] [Google Scholar]
- 9.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin. Infect. Dis. October 2013;57(8):1164–1171. [DOI] [PubMed] [Google Scholar]
- 10.Bor J, Geldsetzer P, Venkataramani A, Barnighausen T. Quasi-experiments to establish causal effects of HIV care and treatment and to improve the cascade of care. Curr Opin HIV AIDS. Nov 2015;10(6):495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. J. Acquir. Immune Defic. Syndr December 15 2014;67(5):519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park WB, Choe PG, Kim SH, et al. One-year adherence to clinic visits after highly active antiretroviral therapy: a predictor of clinical progress in HIV patients. J. Intern. Med March 2007;261(3):268–275. [DOI] [PubMed] [Google Scholar]
- 13.Williams EC, Joo YS, Lipira L, Glass JE. Psychosocial stressors and alcohol use, severity, and treatment receipt across human immunodeficiency virus (HIV) status in a nationally representative sample of US residents. Subst Abus. December 07 2016:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fatch R, Bellows B, Bagenda F, Mulogo E, Weiser S, Hahn JA. Alcohol consumption as a barrier to prior HIV testing in a population-based study in rural Uganda. AIDS Behav June 2013;17(5):1713–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vagenas P, Ludford KT, Gonzales P, et al. Being unaware of being HIV-infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav. January 2014;18(1):120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bengtson AM, L’Engle K, Mwarogo P, King’ola N. Levels of alcohol use and history of HIV testing among female sex workers in Mombasa, Kenya. AIDS Care. 2014;26(12):1619–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heimer R, Usacheva N, Barbour R, Niccolai LM, Uuskula A, Levina OS. Engagement in HIV care and its correlates among people who inject drugs in St Petersburg, Russian Federation and Kohtla-Jarve, Estonia. Addiction. August 2017;112(8):1421–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samet JH, Freedberg KA, Stein MD, et al. Trillion virion delay: time from testing positive for HIV to presentation for primary care. Arch. Intern. Med April 13 1998;158(7):734–740. [DOI] [PubMed] [Google Scholar]
- 19.Korthuis PT, Fiellin DA, McGinnis KA, et al. Unhealthy alcohol and illicit drug use are associated with decreased quality of HIV care. J. Acquir. Immune Defic. Syndr July 19 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Samet JH, Freedberg KA, Savetsky JB, Sullivan LM, Stein MD. Understanding delay to medical care for HIV infection: the long-term non-presenter. AIDS. January 5 2001;15(1):77–85. [DOI] [PubMed] [Google Scholar]
- 21.Giordano TP, Visnegarwala F, White AC Jr., et al. Patients referred to an urban HIV clinic frequently fail to establish care: factors predicting failure. AIDS Care August 2005;17(6):773–783. [DOI] [PubMed] [Google Scholar]
- 22.Samet JH, Freedberg KA, Savetsky JB, Sullivan LM, Padmanabhan L, Stein MD. Discontinuation from HIV medical care: squandering treatment opportunities. J. Health Care Poor Underserved May 2003;14(2):244–255. [DOI] [PubMed] [Google Scholar]
- 23.Monroe AK, Lau B, Mugavero MJ, et al. Heavy alcohol use is associated with worse retention in HIV care. J. Acquir. Immune Defic. Syndr May 26 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wechsberg WM, van der Horst C, Ndirangu J, et al. Seek, test, treat: substance-using women in the HIV treatment cascade in South Africa. Addict Sci Clin Pract. April 26 2017;12(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jean K, Puren A, Cutler E, et al. Level of viral suppression and the cascade of HIV care in a South African semi-urban setting in 2012. AIDS. August 24 2016;30(13):2107–2116. [DOI] [PubMed] [Google Scholar]
- 26.Deiss RG, Mesner O, Agan BK, et al. Characterizing the Association Between Alcohol and HIV Virologic Failure in a Military Cohort on Antiretroviral Therapy. Alcohol. Clin. Exp. Res March 2016;40(3):529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amirkhanian YA, Kelly JA, DiFranceisco WJ, et al. Predictors of HIV Care Engagement, Antiretroviral Medication Adherence, and Viral Suppression Among People Living with HIV Infection in St. Petersburg, Russia. AIDS Behav. December 19 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH. Alcohol use and Human Immunodeficiency Virus (HIV) Infection: current knowledge, implications, and future directions. Alcohol Clin. Exp. Res 2016;4 (10):2056–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Metsch LR, Pugh T, Colfax G. An hiv behavioral intervention gets it right—and shows we must do even better. JAMA Intern Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Samet JH, Cheng DM, Libman H, Nunes DP, Alperen JK, Saitz R. Alcohol consumption and HIV disease progression. J. Acquir. Immune Defic. Syndr October 1 2007;46(2):194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samet JH, Horton NJ, Meli S, Freedberg KA, Palepu A. Alcohol consumption and antiretroviral adherence among HIV-infected persons with alcohol problems. Alcohol. Clin. Exp. Res April 2004;28(4):572–577. [DOI] [PubMed] [Google Scholar]
- 32.Fultz SL, Skanderson M, Mole LA, et al. Development and verification of a “virtual” cohort using the National VA Health Information System. Med. Care August 2006;44(8 Suppl 2):S25–30. [DOI] [PubMed] [Google Scholar]
- 33.Department of Veterans Affairs. HIV/Hepatitis C QUERI Strategic Plan. http://www.queri.research.va.gov/about/strategic_plans/hiv.pdf Washington, D.C.: U.S. Department of Veterans Affairs;2010. [Google Scholar]
- 34.Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am. J. Manag. Care October 2006;12(10):597–606. [PubMed] [Google Scholar]
- 35.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol. Clin. Exp. Res July 2007;31(7):1208–1217. [DOI] [PubMed] [Google Scholar]
- 36.Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol. Clin. Exp. Res August 2013;37(8):1380–1390. [DOI] [PubMed] [Google Scholar]
- 37.Justice AC, Dombrowski E, Conigliaro J, et al. Veterans Aging Cohort Study (VACS): Overview and description. Med. Care August 2006;44(8 Suppl 2):S13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams EC, Lapham GT, Shortreed SM, et al. Among patients with unhealthy alcohol use, those with HIV are less likely than those without to receive evidence-based alcohol-related care: A national VA study. Drug Alcohol Depend. 2017;174:113–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch. Intern. Med April 14 2003;163(7):821–829. [DOI] [PubMed] [Google Scholar]
- 40.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch. Intern. Med September 14 1998;158(16):1789–1795. [DOI] [PubMed] [Google Scholar]
- 41.Rubinsky AD, Kivlahan DR, Volk RJ, Maynard C, Bradley KA. Estimating risk of alcohol dependence using alcohol screening scores. Drug Alcohol Depend. April 1 2010;108(1–2):29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams EC, Bryson CL, Sun H, et al. Association between alcohol screening results and hospitalizations for trauma in Veterans Affairs outpatients. Am. J. Drug Alcohol Abuse January 2012;38(1):73–80. [DOI] [PubMed] [Google Scholar]
- 43.Williams EC, Bradley KA, Gupta S, Harris AH. Association between alcohol screening scores and mortality in black, Hispanic, and white male veterans. Alcohol. Clin. Exp. Res December 2012;36(12):2132–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams EC, Bradley KA, Balderson BH, et al. Alcohol and Associated Characteristics among Older Persons Living with HIV on Antiretroviral Therapy. Subst Abus. March 13 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Au DH, Kivlahan DR, Bryson CL, Blough D, Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcohol. Clin. Exp. Res March 2007;31(3):443–451. [DOI] [PubMed] [Google Scholar]
- 46.Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann. Intern. Med December 2 2008;149(11):795–804. [DOI] [PubMed] [Google Scholar]
- 47.Williams EC, Bryson CL, Sun H, Au DH, Bradley KA. Association Between Alcohol Use and Angina Symptoms Among Outpatients From the Veterans Health Administration. J Addict Med. Mar/Apr 2018;12(2):143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Justice AC, McGinnis KA, Tate JP, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. April 1 2016;161:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris AH, Bradley KA, Bowe T, Henderson P, Moos R. Associations between AUDIT-C and mortality vary by age and sex. Popul Health Manag. October 2010;13(5):263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harris AH, Bryson CL, Sun H, Blough D, Bradley KA. Alcohol screening scores predict risk of subsequent fractures. Subst. Use Misuse June 17 2009;44(8):1055–1069. [DOI] [PubMed] [Google Scholar]
- 51.Rittmueller SE, Frey MS, Williams EC, Sun H, Bryson CL, Bradley KA. Association between alcohol use and cardiovascular self-care behaviors among male hypertensive Veterans Affairs outpatients: a cross-sectional study. Subst Abus. 2015;36(1):6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thomas RM, Francis GPA, Williams EC, et al. Association between alcohol screening scores and diabetic self-care behaviors. Fam. Med 2012;44(8):555–563. [PubMed] [Google Scholar]
- 53.Chavez LJ, Williams EC, Lapham G, Bradley KA. Association between alcohol screening scores and alcohol-related risks among female veterans affairs patients. J Stud Alcohol Drugs May 2012;73(3):391–400. [DOI] [PubMed] [Google Scholar]
- 54.Chavez LJ, Liu CF, Tefft N, et al. Unhealthy alcohol use in older adults: Association with readmissions and emergency department use in the 30 days after hospital discharge. Drug Alcohol Depend. January 01 2016;158:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rubinsky AD, Sun H, Blough DK, et al. AUDIT-C alcohol screening results and postoperative inpatient health care use. J. Am. Coll. Surg March 2012;214(3):296–305 e291. [DOI] [PubMed] [Google Scholar]
- 56.Williams EC, Lapham GT, Shortreed SM, et al. Among patients with unhealthy alcohol use, those with HIV are less likely than those without to receive evidence-based alcohol-related care: A national VA study. Drug Alcohol Depend. May 01 2017;174:113–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zou G A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol April 1 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 58.Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. December 3 1988;2(8623):1267–1273. [DOI] [PubMed] [Google Scholar]
- 59.StataCorp. Stata Statistical Software: Release 14, College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 60.Cunningham WE, Sohler NL, Tobias C, et al. Health services utilization for people with HIV infection: comparison of a population targeted for outreach with the U.S. population in care. Med. Care November 2006;44(11):1038–1047. [DOI] [PubMed] [Google Scholar]
- 61.Hahn JA, Samet JH. Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep. November 2010;7(4):226–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J. Acquir. Immune Defic. Syndr October 1 2009;52(2):180–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moore RD, Bartlett JG. Dramatic decline in the HIV-1 RNA level over calendar time in a large urban HIV practice. Clin. Infect. Dis September 2011;53(6):600–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gordon LL, Gharibian D, Chong K, Chun H. Comparison of HIV Virologic Failure Rates Between Patients with Variable Adherence to Three Antiretroviral Regimen Types. Aids Patient Care STDS July 2015;29(7):384–388. [DOI] [PubMed] [Google Scholar]
- 65.Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin. Infect. Dis October 01 2006;43(7):939–941. [DOI] [PubMed] [Google Scholar]
- 66.Justice AC, Lasky E, McGinnis KA, et al. Medical disease and alcohol use among veterans with human immunodeficiency infection: a comparison of disease measurement strategies. Med. Care August 2006;44(8 Suppl 2):S52–60. [DOI] [PubMed] [Google Scholar]
- 67.McGinnis KA, Tate JP, Williams EC, et al. Comparison of AUDIT-C collected via electronic medical record and self-administered research survey in HIV infected and uninfected patients. Drug Alcohol Depend. November 01 2016;168:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams EC, Achtmeyer CE, Thomas RM, et al. Factors Underlying Quality Problems with Alcohol Screening Prompted by a Clinical Reminder in Primary Care: A Multi-site Qualitative Study. J. Gen. Intern. Med March 3 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bradley KA, Lapham GT, Hawkins EJ, et al. Quality concerns with routine alcohol screening in VA clinical settings. J. Gen. Intern. Med March 2011;26(3):299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.