Abstract
Few studies have explored racial/ethnic differences in healthcare outcomes among patients receiving home health care (HHC), despite known differences in other care settings. We conducted a retrospective cohort study examining racial/ethnic disparities in rehospitalization and emergency room (ER) use among post-acute patients served by a large northeastern HHC agency between 2013-2014 (N=22,722). We used multivariable binomial logistic regression to describe the relationship between race/ethnicity and healthcare utilization outcomes, adjusting for individual-level factors that are conceptually related to health service use. Overall rates of rehospitalization and ER visits were 10% and 13%, respectively. African-American and Hispanic patients experienced higher odds of ER visits or rehospitalization during their HHC episode. Racial/ethnic differences in utilization were mediated by enabling factors, such as caregiver availability, and illness level factors, such as illness severity, functional status, and symptoms. Intervention targets may include early risk assessment, proactive management of clinical conditions, rehabilitative therapy, and caregiver training.
Keywords: home health care, healthcare utilization, health disparities, older adults
INTRODUCTION
Older adults recently discharged from the hospital have unique clinical and therapeutic needs that put them at high risk for adverse outcomes during the post-acute period. Home healthcare (HHC) services address these vulnerable older adults’ post-acute needs to prevent adverse outcomes, such as rehospitalization and ER visits. Older adults who receive skilled HHC services often have multiple chronic conditions, require assistance with several activities of daily living (ADL), and have complex medication regimens (Murtaugh et al., 2009). Despite these clinical risk factors for rehospitalization and emergency room (ER) use (Fortinsky et al., 2006, 2014; Hass, DePalma, Craig, Xu, & Sands, 2015; Hass et al., 2015; McCusker et al., 2003; Mortensen & Song, 2008), the 30-day rehospitalization rate for Medicare HHC patients is 17%, which is lower than that for the broader population of Medicare beneficiaries (20%) (Alliance for Home Health, 2015; Jencks, Williams, & Coleman, 2009). ER visit rates for Medicare HHC patients is about 12% (Alliance for Home Health, 2015) compared to 20-30% for the population of adults age 65 and older (Garcia, Bernstein, & Bush, 2010). Nevertheless, rehospitalizations or ER visits that occur during a HHC episode are indicators of poor healthcare utilization outcomes suggesting lower care quality (Center for Medicare and Medicaid Services, 2010; Schlenker, Powell, & Goodrich, 2005; Towne, Probst, Mitchell, & Chen, 2015). Thus, racial/ethnic differences in these two subtypes of healthcare utilization in the HHC setting, rehospitalization and ER use, may indicate health disparities, in which racial/ethnic minority groups experience poorer outcomes compared to the majority groups (e.g., non-Hispanic White patients).
Almost 17% of HHC patients are from a racial/ethnic minority group (Alliance for Home Health Quality and Innovation, 2013). Racial/ethnic differences in healthcare utilization are well-documented among older adults in the community (Dunlop, Manheim, Song, & Chang, 2002; Remler et al., 2011) and in other healthcare settings (Fortinsky et al., 2014; Jenks et al., 2009; Li, Glance, Yin, & Mukamel, 2011; O’Connor, 2012). However, past research examining healthcare utilization in HHC has primarily focused on determining factors associated with utilization (Fortinsky, Madigan, Sheehan, Tullai-McGuinness, & Fenster, 2006; Fortinsky, Madigan, Sheehan, Tullai-McGuinness, & Kleppinger, 2014; Madigan et al., 2012; O’Connor, Hanlon, Naylor, & Bowles, 2015), versus identifying racial/ethnic differences in healthcare utilization that may indicate disparities in care and patient outcomes. Furthermore, methodological limitations in the existing literature contribute to the current knowledge gap on health disparities in the HHC setting. Previous studies either reported on a limited number of racial/ethnic groups or focused primarily on disparities between white and African-American patients (Fortinsky et al., 2006; Madigan et al., 2012). Other studies did not examine healthcare utilization outcomes by race/ethnicity (Fortinsky et al., 2006; Fortinsky et al., 2014). One study focused on patients with heart failure only (Madigan et al., 2012). None of these prior studies disaggregated samples by HHC admission source, even though risk for rehospitalization is highest among HHC patients admitted post-acute care (O’Connor, 2012). Finally, little research has identified factors associated with differences in healthcare utilization across race/ethnic groups. Additionally, none of the prior studies examined interactions between race/ethnicity and key variables such as age, gender, or functional status to explore relationships among these variables.
The Behavioral Model of Health Service Use proposed by Andersen (1968) and refined by Andersen and Newman (2005) proposes a unique lens to identifying and understanding racial/ethnic differences in healthcare utilization among older adults receiving HHC following hospitalization. The model suggests individual, health system, and social determinant factors influence healthcare utilization. For the purposes of this study, we examined the impact of individual determinants on two healthcare utilization indicators among HHC patients: rehospitalization and ER visits. The individual determinants in the Behavioral Model of Health Service Use are further defined as predisposing, enabling, and illness level factors (Table 1).
Table 1.
Operational Definitions
| Variable | Type | Definitions (OASIS item) |
|---|---|---|
| Predisposing Factors | ||
| Race | Categorical | Asian, African-American, Non-Hispanic White (M1040) |
| Ethnicity | Dichotomous | Hispanic/Latino (M1040) |
| Age | Continuous | From administrative data |
| Gender | Dichotomous | Female (M069) |
| Enabling Factors | ||
| Caregiver ADL assistance | Dichotomous | No ADL assistance needed; patient has a current caregiver to assist with ADL; or patient needs ADL assistance but does not have a caregiver to assist with ADL (M2100) |
| Frequency of assistance | Categorical | Describes ADL or instrumental ADL assistance;Daily/at least weekly (M2110) |
| Living arrangements | Dichotomous | Lives alone/Does not live alone (M1100) |
| Socioeconomic status proxy/Medicaid status | Dichotomous | Medicaid eligibility used as proxy for low SES (M1050) |
| Illness Level Factors | ||
| Total prescribed meds | Continuous | Total number of prescribed medications listed in administrative data |
| Total chronic conditions | Continuous | Sum of all flagged diagnoses from the Chronic Conditions Warehouse from administrative data (range 0-16) |
| Prognosis | Categorical | No risk, temporary risk, or high risk based on assessed clinical stability (M1034) |
| Illness severity | Ordinal | Total number of diagnoses rated as “symptoms controlled with difficulty” or “symptoms poorly controlled” (M1020, M1022). Higher scores indicate worse illness severity. |
| ADL severity score | Continuous | Start of care ADL items (e.g., bathing, dressing upper/lower body, grooming, toilet transferring, toilet hygiene, transferring, and ambulation) standardized to score of 0-1, then summed across all ADL items.Higher indicates worse ADL severity at start of care. |
| Recent decline in mental, emotional, behavioral status | Categorical | Yes/No (M1032, item 1) |
| Frailty | Categorical | Yes/No for frailty indicators such as weight loss, self-reported exhaustion (M1032, item 5) |
| Fall risk | Categorical | Yes/No for fall risk (e.g., falls history, multiple medications, cognitive impairment, toileting frequency, mobility impairment, environmental hazards) (M1910) |
| Vision impairment | Dichotomous | Yes/No for any vision impairment (M1200) |
| Hearing impairment | Dichotomous | Yes/No for any hearing impairment (M1210) |
| Pain | Dichotomous | Yes/No for pain interfering with activity or movement (M1242) |
| Has a surgical wound | Dichotomous | Yes/No for current surgical wound (M1340) |
| Shortness of breath | Categorical | No shortness of breath; mild shortness of breath, defined as shortness of breath with heavy exertion only; or moderate-severe shortness of breath, defined as shortness of breath with mild-moderate exertion (M1400) |
| Urinary incontinence | Dichotomous | Yes/No for urinary incontinence or catheter (M1610) |
| Bowel incontinence | Dichotomous | Yes/No for bowel incontinence (M1620) |
| Cognitive impairment | Dichotomous | Yes/No for any cognitive impairment based on assessment of alertness, orientation, comprehension, concentration, and immediate memory of simple commands (M1700) |
| Depression | Dichotomous | Yes/No for depression symptoms. Patients were assessed for prior screening for depression symptoms with standardized depression screening assessment tool. If not already screened, patient was then screened for depression symptoms by assessor using the PHQ-2 scale. |
| Confusion | Dichotomous | Yes/No for any reported or observed confusion symptoms within the last 14 days (M1710) |
| Anxiety | Dichotomous | Yes/No for any reported or observed anxiety symptoms within the last 14 days (M1720) |
| Cognitive, behavioral, or psychiatric symptoms | Categorical | Yes/No for reported or observed symptoms for at least one week (e.g., memory deficit impaired decisionmaking, physical aggression, verbal disruption, or delusional, hallucinatory, paranoid behavior) (M1740) |
Predisposing factors include demographic, sociocultural, and personal beliefs that may influence one’s decision to seek care. The healthcare utilization literature examining predisposing characteristics, such as race/ethnicity and gender, has been mixed. Some studies found greater in ER use and higher rates of rehospitalization among minorities (Feng et al., 2017; Fortinsky et al., 2014; Jenks et al., 2009; Johnson et al., 2012; Remler et al., 2011). In the context of multiple chronic conditions, older age and female gender were also associated with greater healthcare utilization (Hopman, Heins, Rijken, & Schellevis, 2015). Other studies have shown less healthcare utilization among minorities and women (Dunlop, Manheim, Song, & Chang, 2002; Song, Chang, Manheim, & Dunlop, 2006).
Enabling factors describe family (e.g., insurance, access, social support) and community (e.g., region of the country) characteristics. A literature review by McCusker and colleagues (2003) identified Medicaid status and low social support as determinants of greater ER use among older adults. In the HHC setting, Fortinsky and colleagues (2014) also found that Medicaid status, living alone, and receipt of informal care were risk factors for rehospitalization.
Illness level factors encompass perceived (e.g., disability, symptoms) or evaluated (e.g., chronic conditions) aspects of clinical morbidity (Andersen, 1968; Andersen & Newman, 2005). In recent literature, illness level factors have also been described as “need factors” (Fortinsky, Madigan, Sheehan, Tullai-McGuinness, & Fenster, 2006; Fortinsky et al., 2014; Madigan et al., 2012). Several studies suggest illness level factors are the largest contributor to differences in healthcare utilization between patient groups (Fortinsky et al., 2006, 2014; McCusker, Karp, Cardin, Durand, & Morin, 2003; Mortensen & Song, 2008). Examples of illness level factors specifically associated with greater ER use or rehospitalization include: mental health diagnoses (Andrea, Siegel, & Teo, 2016; Fortinsky et al., 2014), poor functional status (Fortinsky et al., 2006, 2014; Hass, DePalma, Craig, Xu, & Sands, 2015; McCusker et al., 2003; Mortensen & Song, 2008), clinical complexity (Fortinsky et al., 2006, 2014; Hass et al., 2015; McCusker et al., 2003; Mortensen & Song, 2008), and symptoms, such as shortness of breath (Madigan et al., 2012) and pain (Fortinsky et al., 2014). In the HHC setting, having urinary or bowel incontinence, cognitive impairment, or a history of falls are additional characteristics associated with greater healthcare utilization specifically in the HHC setting (Rönneikkö et al., 2017).
Race/ethnic group differences in healthcare utilization among post-acute HHC patients may be indicative of disparities in care quality (Center for Medicare and Medicaid Services, 2010; Schlenker et al., 2005; Towne et al., 2015). Identifying racial/ethnic differences in rehospitalizations and ER visits in this setting will advance the current body of research by uncovering potential targets for intervention or risk stratification to reduce disparities and improve healthcare utilization outcomes. Thus, the purpose of this study was to examine racial/ethnic differences in healthcare utilization among older adults receiving HHC after hospitalization and to explore how factors from the Behavioral Model of Health Service Use may explain any observed relationships between race/ethnicity and utilization outcomes. We hypothesized that 1) healthcare utilization would significantly differ across racial/ethnic groups; 2) with racial/ethnic minority groups having higher odds of healthcare utilization compared to non-Hispanic Whites; and that 3) predisposing, enabling, and illness level factors mediate the relationship between race/ethnicity and healthcare utilization.
METHODS
Study Setting and Data Sources
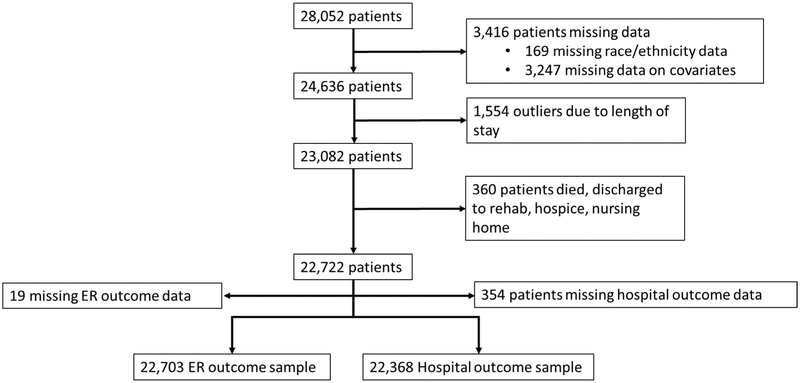
We conducted a retrospective cohort study using the electronic medical records of adult patients served by a large nonprofit certified home healthcare agency in New York City between 2013 and 2014. Separate analytic samples were constructed to examine the outcomes of rehospitalization and ER use among patients who met all study eligibility criteria (Figure 1). Eligible patients in both samples were Medicare beneficiaries, age 65 years or older, who received skilled HHC services immediately following hospitalization. These criteria yielded an overall study population of 28,052 patients. Patients were excluded from either analytic sample if they were missing information on study covariates (n=3,247) or race/ethnicity data (n=169) were enrolled in HHC for more than 91.5 days (n=1,554), or died while enrolled in HHC or were discharged to an institutional setting other than a hospital (i.e. hospice in-patient facility, nursing home, rehabilitation facility; n=360), resulting in a sample of 22,722. For patients with multiple HHC episodes, only the first record was used. We selected a cut point of 91.5 days of HHC enrollment because this number represented the third quartile of length of service for our analytic sample. Patients with longer lengths of HHC service tend to be clinically different from patients who fell within the cutpoints. Further, our primary interest was on healthcare utilization during the post-acute period in the weeks and months following hospitalization. We did not include patients discharged to institutional settings other than the hospital, as the aim of our study was to focus on patients who used acute care resources via rehospitalization or ER visits as these examples of healthcare utilization can be indicators of disparities in care quality (Fortinsky, et al., 2014; Schlenker et al., 2005). Patient data were obtained from merged across three data sources, including from administrative records, medication records, and the Outcome and Assessment Information Set (OASIS-C)—a comprehensive assessment instrument used by clinicians to gather information about patients’ demographic, clinical, functional, and service characteristics during the 60-day episodes of care provided under the Medicare Prospective Payment System. Prior research has established the validity and interrater reliability of OASIS items (Madigan & Fortinsky, 2004; Madigan, Tullai-McGuinness, & Fortinsky, 2003; Tullai-McGuinness, Madigan, & Fortinsky, 2009). The Institutional Review Boards at the BLINDED FOR REVIEW, BLINDED FOR REVIEW, and BLINDED FOR REVIEW approved all study procedures (IRB Approvals Project #812042-3; Approval: E15-007; Project #2004374-AA Review #220026).
Figure 1.
Flowchart for sample selection
Measures
Table 1 lists predictor variables selected from the OASIS based on The Behavioral Model of Health Service Use (Andersen & Newman, 2005) and other existing literature on factors contributing to healthcare utilization.
Predisposing factors.
The primary predictor of interest, race/ethnicity, was obtained from OASIS data. OASIS item M1040 uses the following racial/ethnic categories: American Indian or Alaska Native, Asian, Black or African-American, Hispanic or Latino, Native Hawaiian or Pacific Islander, and White. Patients may self-report multiple racial/ethnic categories; however, specific mixed racial/ethnic categories were not included in this analysis due to small sample sizes. Hispanic patients were categorized as Hispanic regardless of their specific self-identified race. Race/ethnicity was defined by the following categories: White (n=14034), African-American (n=3782), Hispanic (n = 3330), and Asian (n = 1576). Due to small sample sizes, American Indian and Native Hawaiian patients were omitted. Additionally, gender and age were obtained from administrative data.
Enabling factors.
Consistent with previous research examining health disparities among HHC patients (Brega, Goodrich, Powell, & Grigsby, 2005) and research on increased healthcare utilization (McCusker 2003, Fortinsky, 2014), Medicaid status was used as an indicator of low socioeconomic status (SES). Given the effects of social environment on healthcare utilization (McCusker 2003, Fortinsky, 2014), we included the following additional enabling factors: caregiver availability for ADL assistance, frequency of caregiver assistance, and living arrangements (e.g., lives alone or with others).
Illness level factors.
We included diverse indicators for patient clinical complexity: total number of prescribed medications listed in patients’ medication record, total number of chronic conditions (Murtaugh et al., 2009), prognosis (no risk, temporary risk, or high risk); illness severity, which was defined as the number of diagnoses recorded on the OASIS with difficult symptom control. Functional status was defined as ADL severity. To create a variable for ADL severity, we standardized responses to nine OASIS items that assessed patients’ ability to perform the following activities at the start of HHC (Brega et al., 2005; Scharpf & Madigan, 2010): ambulation/locomotion, bathing, dressing upper body, dressing lower body, eating, grooming, toileting/hygiene, toilet transferring, and transferring. Each ADL item is scored on an ordinal scale where higher scores indicate worse ADL disability. Scale ranges vary across individual ADL (e.g., ambulation 0-6, grooming 0-3); therefore, item responses were standardized by dividing the patient’s score by the highest possible response, so that every item was scored on a scale from 0 to 1. To create a total score representing functional status at the start of HHC (Scharpf & Madigan, 2010), individual ADL scores were summed across all ADL items. Higher scores indicated greater ADL severity.
Additional illness level factors included categorical variables for diverse symptoms, such as pain, shortness of breath, mental health symptoms (e.g., confusion, anxiety, depression symptoms, and presence of cognitive, behavioral, or psychiatric symptom, recent decline in mental, emotional, or behavioral status), and urinary or bowel incontinence. We also included frailty, fall risk, vision or hearing impairment, and the presence of a surgical wound, cognitive impairment. Length of HHC service was not included in the final multivariable models because we considered it endogenous. This variable could impact our dependent variable of healthcare utilization; however, length of HHC service could also be influenced by other independent variables in our model, such as illness severity, ADL severity, and chronic conditions.
Outcome variable.
Healthcare utilization was defined by two categorical variables: discharge from HHC to hospital, or ER visit at any time during the HHC episode. Data for all outcome variables were taken from patients’ discharge OASIS administered at the end of HHC services. Rehospitalization was captured using the OASIS discharge disposition items indicating if a patient was admitted to a hospital (M2410) or discharged to the community (M2420). ER visit was captured using the discharge OASIS item M2300 (“since the last time OASIS data were collected, has the patient utilized a hospital emergency department?”).
Statistical Analyses
Statistical analyses relied on 22,703 patients for the ER outcomes and 22,368 for the rehospitalization outcome. Means and standard deviations (overall and by race/ethnicity) were calculated for continuous variables. Frequencies and proportions (overall and by race/ethnicity) were calculated for categorical variables. Multivariable binomial logistic regression was used to model each healthcare utilization outcome, ER visit during HHC episode or discharge from HHC due to rehospitalization, on race/ethnic groups. Models were also estimated adjusting for predisposing factors, enabling factors, and illness level factors, respectively. Exploratory models for ER visit and rehospitalization were estimated including predisposing, enabling, and illness level factors with interaction terms of race/ethnicity by age, gender, Medicaid status, caregiver availability, and ADL severity score. Parameters were estimated using maximum likelihood methodology. Given the large sample size, the threshold for determining statistical significance was set at p≤.01. All analyses were performed using SAS 9.4.
RESULTS
Sample Characteristics
Table 2 lists sample characteristics. Patients were majority female (61%) with a mean age of 79 years (SD 8.64). Most patients had caregivers (72%) and 79% of caregivers provided at least daily assistance with ADL. Thirty-eight percent of the sample lived alone. Although only 8% of patients were dually eligible for Medicare and Medicaid, the majority of these patients were from racial/ethnic minority groups. Patients were clinically complex with most patients having four to six diagnoses with high illness severity. However, larger proportions of Hispanic (75%), African-American (75%), and Asian (72%) patients had four to six diagnoses with high illness severity compared to non-Hispanic Whites (63%) (p<.001). Eighty-six percent of patients had fall risks, and 33% of the sample were frail. Mean ADL severity score of the sample was 3.47 (SD 1.37); however, worse mean ADL severity scores were seen among Asian (3.7, SD 1.37) and Hispanic (3.53, SD 1.43) patients (p<.001). Most patients in both samples reported pain symptoms (73%), and about 40% of patients had surgical wounds. Greater proportions of patients from racial/ethnic minority groups had urinary or bowel incontinence, and shortness of breath symptoms (p<.001). About one-third of patients had cognitive impairment, depression symptoms, or anxiety. Thirteen percent of the sample visited the ER during their HHC episode, and about 10% were discharged from HHC due to rehospitalization. Except for recent decline in mental, emotional, behavioral status, statistically significant differences in all other patient characteristics were observed across race/ethnicities (p≤.01); however, this was likely due to the large sample size.
Table 2.
Patient Characteristics
| Variable | All Patients (n=22722) n (%) or M (SD) |
By Race/Ethnicity n (%) or M (SD) |
||||
|---|---|---|---|---|---|---|
| Asian (n=1576) | African- American (n=3782) |
Hispanic (n=3330) |
Non-Hispanic White (n=14034) |
|||
| Predisposing Factors | ||||||
| Age | 79.34 (8.64) | 80.18 (8.04) | 78.19 (8.60) | 78.85 (8.46) | 79.67 (8.72) | |
| Female Gender | 13808 (60.8) | 907 (57.55) | 2557 (67.61) | 2271 (68.20) | 8073 (57.52) | |
| Enabling Factors | ||||||
| Caregiver ADL Assistance | ||||||
| None needed | 1568 (6.9) | 58 (3.68) | 357 (9.44) | 236 (7.09) | 917 (6.53) | |
| Has a caregiver | 16423 (72.3) | 1135 (72.02) | 2588 (68.43) | 2282 (68.53) | 10418 (74.23) | |
| Needs caregiver | 4731 (20.8) | 383 (24.30) | 837 (22.13) | 812 (24.38) | 2699 (19.23) | |
| Frequency of Caregiver Assistance | ||||||
| Daily | 18028 (79.3) | 1342 (85.15) | 2921 (77.23) | 2637 (79.19) | 11128 (79.29) | |
| At least weekly | 4694 (20.7) | 234 (14.85) | 861 (22.77) | 693 (20.81) | 2906 (20.71) | |
| Living Arrangement | ||||||
| Lives alone | 8528 (37.5) | 400 (25.38) | 1533 (40.53) | 1302 (39.10) | 5293 (37.72) | |
| Does not live alone | 14194 (62.5) | 1176 (74.62) | 2249 (59.47) | 2028 (60.90) | 8741 (62.28) | |
| Medicaid status (SES proxy) | ||||||
| Yes | 1790 (7.9) | 415 (26.33) | 358 (9.47) | 656 (19.70) | 361 (2.57) | |
| No | 20932 (92.1) | 1161 (73.67) | 3424 (90.53) | 2674 (80.30) | 13673 (97.43) | |
| Illness Level Factors | ||||||
| Total Number of Prescribed Meds | 3.46 (4.02) | 4.32 (4.39) | 3.4 (4.00) | 3.68 (4.20) | 3.32 (3.92) | |
| Total Number of Chronic Conditions Prognosis | 2.40 (1.29) | 2.54 (1.21) | 2.74 (1.22) | 2.81 (1.28) | 2.19 (1.27) | |
| No risk | 2460 (10.8) | 119 (7.55) | 558 (14.75) | 356 (10.69) | 1427 (10.17) | |
| Temporary risk | 17087 (75.2) | 1165 (73.92) | 2722 (71.97) | 2587 (77.69) | 10613 (75.62) | |
| High risk | 3175 (14.0) | 292 (18.53) | 502 (13.27) | 387 (11.62) | 1994 (14.21) | |
| Length of Service Illness Severity - diagnoses rated>2 | 31.65 (17.56) | 31.21 (17.16) | 35.58 (17.92) | 34.99 (17.91) | 29.85 (17.14) | |
| 0-3 diagnoses | 7467 (32.86) | 445 (28.24) | 962 (25.44) | 841 (25.26) | 5219 (37.19) | |
| 4-6 diagnoses | 15255 (67.14) | 1131 (71.76) | 2820 (74.56) | 2489 (74.74) | 8815 (62.81) | |
| ADL severity score | 3.47 (1.37) | 3.7 (1.37) | 3.46 (1.50) | 3.53 (1.43) | 3.44 (1.32) | |
| Recent decline in mental, emotional, behavioral status* | 2803 (12.3) | 229 (14.53) | 457 (12.08) | 377 (11.32) | 1740 (12.40) | |
| Frailty | 7496 (33.0) | 583 (36.99) | 1087 (28.74) | 996 (29.91) | 4830 (34.42) | |
| Fall Risk | 19559 (86.1) | 1385 (87.88) | 3199 (84.58) | 2867 (86.10) | 12108 (86.28) | |
| Vision Impairment | 3811 (16.8) | 332 (21.07) | 751 (19.86) | 673 (20.21) | 2055 (14.64) | |
| Hearing Impairment | 4986 (21.9) | 405 (25.70) | 574 (15.18) | 617 (18.53) | 3390 (24.16) | |
| Has Pain | 16665 (73.3) | 1253 (79.51) | 2549 (67.40) | 2289 (68.74) | 10574 (75.35) | |
| Has Surgical Wound Shortness of Breath | 8998 (39.6) | 541 (34.33) | 977 (25.83) | 894 (26.85) | 6586 (46.93) | |
| No symptoms | 11594 (51.0) | 692 (43.91) | 1944 (51.40) | 1520 (45.65) | 7438 (53.00) | |
| Mild symptoms | 6041 (26.6) | 482 (30.58) | 1019 (26.94) | 1001 (30.06) | 3539 (25.22) | |
| Moderate-severe symptoms | 5087 (22.4) | 402 (25.51) | 819 (21.66) | 809 (24.29) | 3057 (21.78) | |
| Urinary Incontinence | 9173 (40.4) | 788 (50.00) | 1684 (44.53) | 1413 (42.43) | 5288 (37.68) | |
| Bowel Incontinence | 2943 (13.0) | 298 (18.91) | 528 (13.96) | 422 (12.67) | 1695 (12.08) | |
| Cognitive Impairment | 6928 (30.5) | 652 (41.37) | 1211 (32.02) | 1322 (39.70) | 3743 (26.67) | |
| Depression Symptoms | 6246 (27.5) | 419 (26.59) | 946 (25.01) | 1018 (30.57) | 3863 (27.53) | |
| Confusion | 9936 (43.7) | 868 (55.08) | 1848 (48.86) | 1798 (53.99) | 5422 (38.63) | |
| Anxiety | 6847 (30.1) | 430 (27.28) | 981 (25.94) | 1006 (30.21) | 4430 (31.57) | |
| Cognitive, behavioral, psychiatric symptoms | 20453 (90.0) | 1400 (88.83) | 3386 (89.53) | 2934 (88.11) | 12733 (90.73) | |
| Emergency room visit | 3054 (13.4) | 236 (14.97) | 667 (17.64) | 533 (16.01) | 1618 (11.53) | |
| Rehospitalized | 2226 (9.8) | 144 (9.14) | 491 (12.98) | 357 (10.72) | 1234 (8.79) | |
Note. Except for item marked by (*), statistically significant differences between race/ethnicities were found for all characteristics (p≤.01), likely due to large sample size. M=mean; SD=standard deviation; ADL=activities of daily living; SES=socioeconomic status
ER Visits
Table 3 shows the results of stepwise modeling for the ER visit outcome (n=22,703). In bivariate modeling, patients who were Asian (OR 1.35, 95% CI 1.17-1.57), African-American (OR 1.64, 95% CI 1.49-1.81), or Hispanic (OR 1.46, 95% CI 1.32-1.63) had statistically significantly greater odds of visiting the ER during their HHC episode compared to non-Hispanic Whites. When predisposing factors were added to the model, the odds of an ER visit were slightly worse for African-American (OR 1.70, 95% CI 1.54-1.88) and Hispanics (OR 1.50, 95% CI 1.35-1.67), but unchanged for Asians. In the model adjusted for enabling factors only, the relationship between race/ethnicity and odds of ER visit was attenuated; however, Asians (OR 1.28; 95% CI 1.10-1.49), African-Americans (OR 1.64, 95% CI 1.49-1.81), and Hispanics (OR 1.42, 95% CI 1.27-1.58) still had statistically significantly greater odds of rehospitalization compared to non-Hispanic Whites. Illness level factors had the greatest impact on the relationship between race/ethnicity and the odds of an ER visit. After controlling for illness level factors, Asian race was no longer a statistically significant category (OR 1.15, 95% CI .98-1.33). African-Americans (OR 1.45; 95% CI 1.31-1.61) and Hispanics (OR 1.26, 95% CI 1.13-1.41) still had greater odds of an ER visit compared to non-Hispanic Whites after controlling for illness level factors.
Table 3.
Stepwise modeling for ER outcome (n=22,703)
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 |
|---|---|---|---|---|---|
| Predisposing Factors | |||||
| Race (REF=Non-Hispanic White) | |||||
| Asian | 1.35** (1.17-1.57) |
1.35** (1.61-1.56) |
1.28* (1.10-1.49) |
1.15 (.98-1.33) |
1.13 (.97-1.33) |
| African-American | 1.64** (1.49-1.81) |
1.70** (1.54-1.88) |
1.64** (1.49-1.81) |
1.45** (1.31-1.61) |
1.45** (1.31-1.62) |
| Hispanic | 1.46** (1.32-1.63) |
1.50** (1.35-1.67) |
1.42** (1.27-1.58) |
1.26** (1.13-1.41) |
1.26** (1.12-1.41) |
| Age | 1.01** (1.00-1.01) |
.99** (.99-1.00) |
|||
| Female | .83** (.77-.90) |
.80** (.74-.87) |
|||
| Enabling Factors | |||||
| Caregiver ADL assistance (REF=none needed) | |||||
| Has caregiver | 1.63** (1.35-1.96) |
1.35* (1.11-1.65) |
|||
| Needs caregiver | 1.91** (1.57-2.32) |
1.40** (1.14-1.72) |
|||
| At least weekly of caregiver assistance (REF=daily) | .86* (.77-.96) |
.94 (.84-1.01) |
|||
| Lives alone | 1.08 (1.00-1.17) |
1.11 (1.02-1.22) |
|||
| Medicaid Status | 1.16 (1.01-1.32) |
1.02 (.89-1.17) |
|||
| Illness Level Factors | |||||
| Total Number of Prescribed Medications | 1.01** (1.01-1.02) |
1.01* (1.00-1.02) |
|||
| Total Number of Chronic Conditions | 1.07** (1.04-1.11) |
1.07** (1.04-1.11) |
|||
| Prognosis (REF=no risk) | |||||
| Temporary risk | 1.09 (.95-1.24) |
1.09 (.95-1.25) |
|||
| High risk | 1.47** (1.25-1.73) |
1.46** (1.24-1.71) |
|||
| Illness severity | 111** (1.07-1.14) |
1.10** (1.06-1.14) |
|||
| ADL severity | 1.11** (1.07-1.15) |
1.11** (1.07-1.15) |
|||
| Recent decline in mental, emotional, behavioral status | .97 (.86-1.09) |
.97 (.86-1.09) |
|||
| Frailty | 1.16** (1.07-1.27) |
1.15** (1.07-1.27) |
|||
| Fall Risk | 1.01 (.89-1.14) |
1.00 (.89-1.14) |
|||
| Vision Impairment | .97 (.88-1.08) |
.98 (.88-1.08) |
|||
| Hearing Impairment | .91 (.82-1.00) |
.94 (.85-1.04) |
|||
| Has Pain | .91 (.83-.99) |
.90 (.82-.99) |
|||
| Has Surgical Wound | 0.76** (.69-.83) |
.71** (.65-.79) |
|||
| Shortness of Breath (REF=nosymptoms) | |||||
| Mild symptoms | 1.10 (1.00-1.21) |
1.09 (.99-1.20) |
|||
| Moderate-Severe symptoms | 1.26** (1.14-1.39) |
1.24** (1.12-1.37) |
|||
| Urinary Incontinence | 1.02 (.93-1.11) |
1.06 (.96-1.16) |
|||
| Bowel Incontinence | 1.38** (1.22-1.55) |
1.38** (1.22-1.56) |
|||
| Cognitive Impairment | 1.01 (.90-1.14) |
1.02 (.91-1.15) |
|||
| Depression Symptoms | 1.25** (1.14-1.36) |
1.24** (1.14-1.36) |
|||
| Confusion | 1.01 (.91-1.13) |
1.01 (.91-1.13) |
|||
| Anxiety | 0.89* (.81-.98) |
.89* (.81-.98) |
|||
| Cognitive, behavioral, psychiatric symptoms | 0.82* (.72-.94) |
.83* (.72-.95) |
|||
Note. Data are presented as odds ratio (95% CI). Model 1=bivariate analysis of odds for emergency room visit by race/ethnicity; Model 2=Model 1 adjusting for predisposing factors; Model 3=Model 1 adjusting for enabling factors; Model 4=Model 1 adjusting for illness level factors; Model 5=multivariable model of odds of emergency room visit by race/ethnicity, adjusting for predisposing, enabling, and illness level factors. REF=reference category; Reference categories are the absence of the characteristics, unless otherwise indicated. ADL=activities of daily living
p≤.01
p≤.001
In the complete model, adjusting for all predisposing, enabling, and illness level factors (Table 3), African-Americans (OR 1.45; 95% CI 1.31-1.62) and Hispanics (OR 1.26, 95% CI 1.12-1.41) had greater odds of an ER visit while receiving HHC after hospitalization compared to non-Hispanic Whites. In contrast, there was no statistically significant difference between the odds of an ER visit between Asian and non-Hispanic White patients (OR 1.13; 95% CI .97-1.33). There were no statistically significant interactions between factors included in the model.
Table 3 depicts additional factors associated with greater odds of ER use in this sample. For example, women had 20% lower odds of visiting the ER compared to men. Younger age was associated with lower odds of an ER visit (p<.001). Compared to patients who did not need a caregiver, patients who had a caregiver were 1.35 times more likely to have an ER visit (p=.002). Additionally, patients who needed a caregiver but did not have one available were 1.40 times more likely to have an ER visit compared to patients with no caregiver needs (p=.001). Among illness level factors, having a surgical wound (p<.001), or having anxiety (p<.001) was associated with lower odds of an ER visit. Conversely, frailty (p=.001), greater number of prescribed medications (p=.004), more chronic conditions (p<.001), greater illness severity (p<.001), greater ADL severity at start of care (p<.001), high risk prognosis (p<.001), and severe shortness of breath (p<.001) were associated with greater odds of an ER visit.
Rehospitalization
Table 4 shows the results of stepwise modeling for the rehospitalization outcome (n=22,368). In bivariate modeling, African-American (OR 1.55, 95% CI 1.39-1.74), and Hispanic (OR 1.25, 95% CI 1.10-1.41) patients had significantly greater odds of being hospitalized compared to non-Hispanic Whites. No statistically significant difference in the odds of rehospitalization was observed between Asian and non-Hispanic White patients (OR 1.03; 95% CI .86-1.24). When predisposing factors only were added to the model, odds of rehospitalization for both African-American (OR 1.63, 95% CI 1.46-1.82) and Hispanic (OR 1.30, 95% CI 1.15-1.49) patients increased. In the model adjusted for enabling factors, the relationship between race/ethnicity and rehospitalization was attenuated with African-Americans having 1.54 times greater odds of rehospitalization (95% CI 1.38-1.73) and Hispanics having 1.19 times greater odds of rehospitalization (95% CI 1.04-1.35) compared to non-Hispanic Whites. Similar to the ER model, illness-level factors had the greatest impact on the relationship between race/ethnicity and the odds of rehospitalization. African-Americans still had greater odds of rehospitalization compared to non-Hispanic Whites after controlling for these factors (OR 1.35, 95% CI 1.20-1.52); whereas Asian race and Hispanic ethnicity were not statistically significant.
Table 4.
Stepwise modeling for rehospitalization outcome (n=22,368)
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|---|
| Predisposing Factors | ||||||
| Race (REF=non-Hispanic White) | ||||||
| Asian | 1.03 (.86-1.24) |
1.03 (.86-1.23) |
.94 (.78-1.13) |
.86 (.78-1.13) |
.82 (.68-.99) |
|
| African-American | 1.55** (1.39-1.74) |
1.63** (1.46-1.82) |
1.54** (1.38-1.73) |
1.35** (1.20-1.52) |
1.34** (1.19-1.51) |
|
| Hispanic | 1.25** (1.10-1.41) |
1.30** (1.15-1.49) |
1.19* (1.04-1.35) |
1.06 (.93-1.21) |
1.05 (.92-1.21) |
|
| Age | 1.01** (1.00-1.01) |
.98** (.98-.99) |
||||
| Female | .73** (.67-.80) |
.70** (.63-.76 |
||||
| Enabling Factors | ||||||
| Caregiver ADL assistance (REF=none needed) | ||||||
| Has caregiver | 1.67** (1.34-2.09) |
1.27 (1.00-1.59) |
||||
| Needs caregiver | 1.97** (1.57-2.48) |
1.29 (1.01-1.65) |
||||
| At least weekly of caregiver assistance (REF=daily) | 0.82* (.72-.93) |
.94 (.82-1.07) |
||||
| Lives alone | .99 (.90-1.09) |
1.04 (.94-1.15) |
||||
| Medicaid Status | 1.27** (1.09-1.48) |
1.10 (.93-1.28) |
||||
| Illness Level Factors | ||||||
| Total Number of Prescribed Medications | 1.00 (.99-1.01) |
1.00 (.99-1.01) |
||||
| Total Number of Chronic Conditions Prognosis (REF=no risk) | 1.04 (1.00-1.08) |
1.04 (1.00-1.08) |
||||
| Temporary risk | 1.14 (.97-1.34) |
1.13 (.96-1.33) |
||||
| High risk | 1.59** (1.32-1.92) |
1.54** (1.27-1.86) |
||||
| Illness severity | 1.13** (1.09-1.17) |
1.13** (1.09-1.17) |
||||
| ADL severity | 1.18** (1.18-1.14) |
1.19** (1.14-1.23) |
||||
| Recent decline in mental, emotional, behavioral status | 1.05 (.92-1.20) |
1.05 (.92-1.20) |
||||
| Frailty | 1.15** (1.04-1.27) |
1.14* (1.03-1.26) |
||||
| Fall Risk | .97 (.84-1.12) |
.98 (.85-1.13) |
||||
| Vision Impairment | .99 (.88-1.12) |
1.00 (.89-1.13) |
||||
| Hearing Impairment | .89 (.79-.99) |
.94 (.83-1.06) |
||||
| Has Pain | .94 (.85-1.05) |
.94 (.85-1.04) |
||||
| Has Surgical Wound | .63** (.56-.71) |
.57** (.51-.64) |
||||
| Shortness of Breath (REF=no symptoms) | ||||||
| Mild symptoms | 1.17* (1.04-1.31) |
1.16* (1.03-1.30) |
||||
| Moderate-Severe symptoms | 1.49** (1.33-1.66) |
1.46** (1.31-1.64) |
||||
| Urinary Incontinence | 1.07 (.97-1.19) |
1.15* (1.04-1.28) |
||||
| Bowel Incontinence | 1.32** (1.15-1.51) |
1.31** (1.15-1.51) |
||||
| Cognitive Impairment | .92 (.81-1.06) |
.94 (.82-1.08) |
||||
| Depression Symptoms | 1.25** (1.13-1.38) |
1.24** (1.12-1.37) |
||||
| Confusion | .99 (.87-1.12) |
1.00 (.88-1.13) |
||||
| Anxiety | 0.85* (.77-.94) |
0.85* (.76-.94) |
||||
| Cognitive, behavioral, psychiatric symptoms | .97 (.84-1.12) |
.88 (.76-1.02) |
||||
Note. Data are presented as odds ratio (95% CI). Model 1=bivariate analysis of odds for hospitalization by race/ethnicity; Model 2=Model 1 adjusting for predisposing factors; Model 3=Model 1 adjusting for enabling factors; Model 4=Model 1 adjusting for illness level factors; Model 5=multivariable model of odds of rehospitalization by race/ethnicity, adjusting for predisposing, enabling, and illness level factors. REF=reference category; Reference categories are the absence of the characteristics, unless otherwise indicated. ADL=activities of daily living
p≤.01
p≤.001
In the complete model, adjusting for all predisposing, enabling, and illness level factors (Table 4), African-Americans (OR 1.34; 95% CI 1.19-1.51) had significantly greater odds of rehospitalization compared to non-Hispanic Whites. There was no statistically significant difference in the odds of rehospitalization between Asians or Hispanics and non-Hispanic Whites. There were no statistically significant interactions between factors included in the model.
The complete model in Table 4 depicts additional factors associated with greater odds of rehospitalization in this sample. For example, women in our sample had almost 30% lower odds of being hospitalized compared to men (p<.001). Younger age was associated with lower odds of rehospitalization (p<.001). Among illness level factors, having a surgical wound (p<.001), or having anxiety (p=.002) was associated with lower odds of an ER visit. Conversely, frailty (p=.011), greater illness severity (p<.001), greater ADL severity at start of care (p<.001), high risk prognosis (p<.001), urinary (p=.008) or bowel incontinence (p<.001), mild (p=.012) or moderate to severe shortness of breath (p<.001), or depression symptoms (p<.001) were associated with greater odds of rehospitalization.
DISCUSSION
Health disparities research is sparse in the HHC setting. Our study adds to the existing body of research on health disparities by examining racial/ethnic differences in healthcare utilization among older adults receiving HHC after hospitalization. Differences in healthcare utilization outcomes by race/ethnicity may be indicators of disparities in care quality and other patient-centered outcomes, such as clinical and functional status (Center for Medicare and Medicaid Services, 2010). Although we observed overall low rates of ER visits and rehospitalization compared to previous studies (Fortinsky, Covinsky, Palmer, & Landefeld, 1999; Fortinsky et al., 2006; O’Connor, 2012), our findings demonstrated significant differences in healthcare utilization across racial/ethnic groups. Furthermore, by using a stepwise modeling approach, we observed that racial/ethnic differences in healthcare utilization patterns were partially explained by enabling and illness level factors. Thus, our study addresses important clinical issues for a population at high risk for healthcare utilization due to their post-acute status, morbidity, and age (Murtaugh et al., 2009).
We observed the highest healthcare utilization rates among African-American patients, who had a 45% higher likelihood of an ER visit during the HHC episode and a 34% higher likelihood of rehospitalization compared to non-Hispanic Whites. Hispanic patients in our sample also had greater odds of ER visits compared to non-Hispanic Whites. These findings align with past research on racial/ethnic disparities in ER use (Johnson et al., 2012; Saef et al., 2016) and rehospitalizations (Fortinsky et al., 2014). Despite also having more indicators of higher clinical morbidity, Asian HHC patients had no significant difference in odds of ER visit or rehospitalization compared to non-Hispanic Whites. These findings differ from previous work suggesting that Asian patients were less likely to be hospitalized during HHC service (Fortinsky et al., 2014).
Differences in healthcare utilization by race/ethnicity may be the result of diverse factors. Consistent with past literature, illness level factors had the greatest influence on the relationship between race/ethnicity and healthcare utilization of all factors included in our statistical models (Fortinsky et al., 2006, 2014; Mortensen & Song, 2008). African-American and Hispanic patients in our sample had more indicators of clinical morbidity (e.g., high illness severity, worse functional status at start of care, more prescribed medications, and more chronic conditions). Proactive management of clinical conditions and functional deficits in the post-acute setting could attenuate the effects of morbidity on healthcare utilization (Gruneir, Silver, & Rochon, 2011). Skilled HHC provides an excellent environment to implement proactive care to monitor patients and coordinate care with primary care providers in the post-acute period. For example, nurse-led care coordination models to facilitate healthcare transitions have been associated with reductions in rehospitalizations, rehospitalization, and ER use in the post-acute setting (Marek, Popejoy, Petroski, & Rantz, 2006; Naylor et al., 1994; Naylor et al., 2004; Popejoy et al., 2015). Additionally, educating patients and caregivers in chronic disease self-management (Lorig et al., 2001) and enhancing continuity of care between patients and their providers (Amjad, Carmichael, Austin, Chang, & Bynum, 2016) could also impact healthcare utilization outcomes. These interventions should be tested among racially/ethnically diverse samples to determine the effects on disparities in healthcare utilization.
Caregivers may also contribute to the differences in healthcare utilization observed in our study. Caregiver availability, an enabling factor, could be an important intervention target to improve disparities in healthcare utilization. After controlling for all covariates, having a caregiver was associated with a greater likelihood of ER visits. It is possible that patients in our sample who had caregivers also had greater functional deficits and were more clinically complex, which may have contributed to greater healthcare utilization. Additionally, needing, but not having a caregiver to assist with ADL, was associated with a greater likelihood of ER visits. Racial/ethnic minority groups are at high risk of unmet needs in the post-acute setting (Graham, Ivey, & Neuhauser, 2009). Indeed, greater proportions of all racial/ethnic minority groups in our sample reported unmet needs for caregiver assistance with ADL compared to non-Hispanic Whites. A growing body of literature suggests unmet needs related to ADL disability are associated with increased risk of rehospitalization (Depalma et al., 2013; Sands et al., 2006), ER use (Hass, DePalma, Craig, Xu, & Sands, 2015), and mortality (He et al., 2015). Therefore, minority older adults receiving HHC after hospitalization would be an excellent group in which to implement caregiver interventions. Such interventions should educate and empower patients and caregivers in the management of their care by involving them in care processes and planning (Foust, Vuckovic, & Henriquez, 2012; Naylor, 2006). Additional intervention strategies might include approaches to function-focused care (Resnick, Galik, Gruber-Baldini, & Zimmerman, 2011; Resnick & Galik, 2013) and training based on caregiver ability and needs (Wilkins, Bruce, & Sirey, 2009).
The observed differences in healthcare utilization by race/ethnicity may also be related to racial/ethnic disparities in the services patients may have received during the HHC service period. There is existing literature to suggest differences in skilled nursing and rehabilitative therapy services by racial/ethnic groups (BLINDED FOR REVIEW; Peng et al., 2003; Yeboah-Korang et al., 2011). Studies have documented fewer skilled nursing visits (Yeboah-Korang et al., 2011) or physical/occupational therapy visits (BLINDED FOR REVIEW; Peng et al., 2003; Yeboah-Korang et al., 2011) for African-American and Hispanic HHC patients compared to non-Hispanic Whites. These types of services are especially important given the explanatory effects of illness level factors on racial/ethnic difference in healthcare utilization outcomes among older post-acute HHC patients. However, there is little research examining the reasons behind disparities in services. Examining risk stratification strategies and exploring both patient preferences and provider decision-making in HHC could enhance understanding of observed disparities in the delivery and receipt of HHC services that can affect rates of rehospitalization and ER use.
Cultural differences may be an additional factor contributing to observed differences in healthcare utilization in our sample. Patient care preferences may vary based on cultural differences. For example, many African-American and Hispanic older adults do not have advanced care plans, and African-American patients tend to prefer more aggressive care at end-of-life (Johnson, Kuchibhatla, & Tulsky, 2008; Portanova, Ailshire, Perez, Rahman, & Enguidanos, 2017). Diverse patient care preferences may lead to declining post-acute services that are beneficial (Sefcik et al., 2017), such as HHC. Cultural differences can influence interactions and communication between patients and care providers. Several studies suggest that minority elders have difficulty communicating their preferences, and getting needed and timely care (Weech-Maldonado et al., 2003; Weech-Maldonado, Fongwa, Gutierrez, & Hays, 2008). Clinicians should consider the potential effects of cultural differences on patient preferences when working with racially/ethnically diverse older adults. Strategies may include building trust among clinicians, patients, and caregivers, and tailored education about the benefits of post-acute HHC services (Sefcik et al., 2016).
Limitations
There are some important limitations to this study. We used retrospective data from a single HHC agency in the northeast. Generalizability of these findings to other areas might be limited. Our outcome variables, rehospitalization and ER visits, were taken from the OASIS-C; therefore, we have limited information related to reasons for healthcare utilization and recurrent or multiple rehospitalizations or ER visits to accurately quantify the extent of healthcare utilization across groups. Additionally, because we examined a single time-point, from admission to discharge of one HHC episode, we are unable to determine the effects of prior healthcare utilization or health status on our outcomes. Social determinants of health are also important factors to consider in health disparities research; however, we did not have access to individual- or community-level determinants, such as education level, area income that may have effects on the relationship between race/ethnicity and healthcare utilization. Similarly, due to limited information on health services system and societal determinants, we could only examine individual determinants within the Behavioral Model of Health Service Use (Andersen & Newman, 2005). Expanding this research to include factors beyond individual determinants, such as agency-level and environmental characteristics, would provide greater insight into mechanisms of disparities in healthcare utilization. Finally, our study is observational, limiting the ability to draw conclusions regarding causal relationships. However, findings from our work may be used to guide future research, including interventions, to investigate and reduce health disparities in the HHC setting.
Conclusion
Our study adds to the growing body of research in the HHC setting. Importantly, our work addresses a critical knowledge gap in health disparities research among vulnerable patients. Racial/ethnic minority groups in our sample experienced higher odds of ER visits and rehospitalization during their HHC episode. Additional research is needed to address healthcare utilization outcomes in these groups and to identify promising intervention targets for reducing disparities in the HHC setting.
Acknowledgments
Funding acknowledgement: This work was supported by the University of Pennsylvania School of Nursing Center for Integrative Science in Aging Frank Morgan Jones Fund; and National Institutes of Health, National Institute of Nursing Research [T32NR009356]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interests: The authors have no conflicts of interest to disclose.
IRB Approval: for VNSNY – Project #812042-3; Approval: E15-007; for MU – Project #2004374-AA Review #220026
Contributor Information
Jo-Ana D. Chase, University of Pennsylvania, 338G School of Nursing, 418 Curie Blvd., Philadelphia, PA 19104, Assistant Professor, University of Missouri – Columbia, chasej@missouri.edu.
David Russell, Center for Home Care Policy & Research, Visiting Nurse Service of New York, 1250 Broadway, 7th Floor, New York, NY 10001, david.russell@vnsny.org.
Liming Huang, 418 Curie Blvd, Suite 479L, Claire M. Fagin Hall, School of Nursing, University of Pennsylvania, limingh@nursing.upenn.edu.
Alexandra Hanlon, 418 Curie Blvd, Suite 479L, Claire M. Fagin Hall, School of Nursing, University of Pennsylvania, alhanlon@nursing.upenn.edu.
Melissa O'Connor, National Hartford Center for Gerontological Nursing Excellence, Assistant Professor, College of Nursing, Villanova University, Driscoll Hall, Office #316, 800 Lancaster Avenue, Villanova, PA 19085, melissa.oconnor@villanova.edu.
Kathryn H. Bowles, University of Pennsylvania, 418 Curie Boulevard Room 340, Philadelphia, PA 19104; Director of the Center for Home Care Policy and Research, Visiting Nurse Service of New York, bowles@nursing.upenn.edu.
References
- Alliance for Home Health Quality and Innovation. (2013). Faces of home health: Cultural, racial, and ethnic diversity in home health patient populations. Retrieved October 14, 2016, from http://ahhqi.org/images/uploads/AHHQI_FacesHH_Cultural_FINAL.pdf
- Alliance for Home Health Quality and Innovation. (2015). Home Health Chartbook 2015. Retrieved November 2, 2017, from http://ahhqi.org/images/uploads/AHHQI_2015_Chartbook_FINAL_October_Aug2016Update.pdf
- Amjad H, Carmichael D, Austin AM, Chang C-H, & Bynum JPW (2016). Continuity of care and health care utilization in older adults with dementia in Fee-for-Service Medicare. JAMA Internal Medicine, 176(9), 1371–1378. 10.1001/jamainternmed.2016.3553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R (1968). A behavioral model of families’ use of health services. Center for Health Administration Studies, University of Chicago. [Google Scholar]
- Andersen R, & Newman JF (2005). Societal and individual determinants of medical care utilization in the United States. The Milbank Quarterly, 83(4). 10.1111/j.1468-0009.2005.00428.x [DOI] [PubMed] [Google Scholar]
- Andrea SB, Siegel SAR, & Teo AR (2016). Social support and health service use in depressed adults: Findings from the National Health and Nutrition Examination Survey. General Hospital Psychiatry, 39, 73–79. 10.1016/j.genhosppsych.2015.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brega AG, Goodrich GK, Powell MC, & Grigsby J (2005). Racial and ethnic disparities in the outcomes of elderly home care recipients. Home Health Care Services Quarterly, 24(3), 1–21. 10.1300/J027v24n03_01 [DOI] [PubMed] [Google Scholar]
- Center for Medicare and Medicaid Services. (2010). Outcome-Based Quality Improvement (OBQI) Manual. Centers for Medicare and Medicaid Services. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/downloads/HHQIOBQIManual.pdf
- Depalma G, Xu H, Covinsky KE, Craig BA, Stallard E, Thomas J, & Sands LP (2013). Hospital readmission among older adults who return home with unmet need for ADL disability. The Gerontologist, 53(3), 454–461. 10.1093/geront/gns103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop DD, Manheim LM, Song J, & Chang RW (2002). Gender and ethnic/racial disparities in health care utilization among older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 57(4), S221–233. [DOI] [PubMed] [Google Scholar]
- Feng C, Paasche-Orlow MK, Kressin NR, Rosen JE, López L, Kim EJ, … Hanchate AD (2017). Disparities in potentially preventable hospitalizations: near-national estimates for Hispanics. Health Services Research. 10.1111/1475-6773.12694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortinsky RH, Covinsky KE, Palmer RM, & Landefeld CS (1999). Effects of functional status changes before and during hospitalization on nursing home admission of older adults. Journals of Gerontology: Series A: Biological Sciences and Medical Sciences, 54A(10), M521–M526. doi: 10.1093/gerona/54.10.m521 [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Madigan EA, Sheehan TJ, Tullai-McGuinness S, & Fenster JR (2006). Risk factors for hospitalization among Medicare home care patients. Western Journal of Nursing Research, 28(8), 902–917. 10.1177/0193945906286810 [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Madigan EA, Sheehan TJ, Tullai-McGuinness S, & Kleppinger A (2014). Risk factors for hospitalization in a national sample of Medicare home health care patients. Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society, 33(4), 474–493. 10.1177/0733464812454007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foust JB, Vuckovic N, & Henriquez E (2012). Hospital to home health care transition: patient, caregiver, and clinician perspectives. Western Journal of Nursing Research, 34(2), 194–212. 10.1177/0193945911400448 [DOI] [PubMed] [Google Scholar]
- Garcia TC, Bernstein AB, & Bush MA (2010). Emergency department visitors and visits: Who used the emergency room in 2007? (NCHS Data Brief No. 38). U.S. Department of Health and Human Services; Retrieved from https://www.cdc.gov/nchs/data/databriefs/db38.pdf [PubMed] [Google Scholar]
- Graham CL, Ivey SL, & Neuhauser L (2009). From hospital to home: assessing the transitional care needs of vulnerable seniors. The Gerontologist, 49(1), 23–33. 10.1093/geront/gnp005 [DOI] [PubMed] [Google Scholar]
- Gruneir A, Silver MJ, & Rochon PA (2011). Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Medical Care Research and Review: MCRR, 68(2), 131–155. 10.1177/1077558710379422 [DOI] [PubMed] [Google Scholar]
- Hass Z, DePalma G, Craig BA, Xu H, & Sands LP (2015). Unmet need for help with activities of daily living disabilities and emergency department admissions among older Medicare recipients. The Gerontologist. 10.1093/geront/gnv142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S, Craig BA, Xu H, Covinsky KE, Stallard E, Thomas J, … Sands, L. P. (2015). Unmet need for ADL assistance is associated with mortality among older adults with mild disability. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 70(9), 1128–1132. 10.1093/gerona/glv028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopman P, Heins MJ, Rijken M, & Schellevis FG (2015). Health care utilization of patients with multiple chronic diseases in The Netherlands: Differences and underlying factors. European Journal of Internal Medicine, 26(3), 190–196. 10.1016/j.ejim.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, & Coleman EA (2009). Rehospitalizations among patients in the Medicare fee-for-service program. The New England Journal of Medicine, 360(14), 1418–1428. 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- Johnson KS, Kuchibhatla M, & Tulsky JA (2008). What explains racial differences in the use of advance directives and attitudes toward hospice care? Journal of the American Geriatrics Society, 56(10), 1953–1958. 10.1111/j.1532-5415.2008.01919.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PJ, Ghildayal N, Ward AC, Westgard BC, Boland LL, & Hokanson JS (2012). Disparities in potentially avoidable emergency department (ED) care: ED visits for ambulatory care sensitive conditions. Medical Care, 50(12), 1020–1028. 10.1097/MLR.0b013e318270bad4 [DOI] [PubMed] [Google Scholar]
- Li Y, Glance LG, Yin J, & Mukamel DB (2011). Racial disparities in rehospitalization among Medicare patients in skilled nursing facilities. American Journal of Public Health, 101(5), 875–882. 10.2105/AJPH.2010.300055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Bandura A, … Holman HR (2001). Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care, 39(11), 1217–1223. doi: 10.1097/00005650-200111000-00008 [DOI] [PubMed] [Google Scholar]
- Madigan EA, & Fortinsky RH (2004). Interrater reliability of the Outcomes and Assessment Information Set: Results from the field. The Gerontologist, 44(5), 689–692. doi: 10.1093/geront/44.5.689 [DOI] [PubMed] [Google Scholar]
- Madigan EA, Gordon NH, Fortinsky RH, Koroukian SM, Pina I, & Riggs JS (2012). Rehospitalization in a national population of home health care patients with heart failure. Health Services Research, 47(6), 2316–2338. 10.1111/j.1475-6773.2012.01416.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan EA, Tullai-McGuinness S, & Fortinsky RH (2003). Accuracy in the Outcomes and Assessment Information Set (OASIS): Results of a video simulation. Research in Nursing & Health, 26(4), 273–283. doi: 10.1002/nur.10094 [DOI] [PubMed] [Google Scholar]
- Marek KD, Popejoy L, Petroski G, & Rantz M (2006). Nurse care coordination in community-based long-term care. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau, 38(1), 80–86. doi: 10.1111/j.1547-5069.2006.00081.x [DOI] [PubMed] [Google Scholar]
- McCusker J, Karp I, Cardin S, Durand P, & Morin J (2003). Determinants of emergency department visits by older adults: a systematic review. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 10(12), 1362–1370. [DOI] [PubMed] [Google Scholar]
- Mortensen K, & Song PH (2008). Minding the gap: a decomposition of emergency department use by Medicaid enrollees and the uninsured. Medical Care, 46(10), 1099–1107. doi: 10.1097/MLR.0b013e318185c92d [DOI] [PubMed] [Google Scholar]
- Murtaugh C, Peng T, Totten A, Costello B, Moore S, & Aykan H (2009). Complexity in geriatric home healthcare. Journal for Healthcare Quality: Official Publication of the National Association for Healthcare Quality, 31(2), 34–43. doi: 10.1111/j.1945-1474.2009.00017.x [DOI] [PubMed] [Google Scholar]
- Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, & Pauly M (1994). Comprehensive discharge planning for the hospitalized elderly: A randomized clinical trial. Annals of Internal Medicine, 120(12), 999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005 [DOI] [PubMed] [Google Scholar]
- Naylor MD (2006). Transitional care: a critical dimension of the home healthcare quality agenda. Journal for Healthcare Quality: Official Publication of the National Association for Healthcare Quality, 28(1), 48–54. doi: 10.1111/j.1945-1474.2006.tb00594.x [DOI] [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, & Schwartz JS (2004). Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. Journal of the American Geriatrics Society, 52(5), 675–684. doi: 10.1111/j.1532-5415.2004.52202.x [DOI] [PubMed] [Google Scholar]
- O’Connor M (2012). Hospitalization among Medicare-Reimbursed Skilled Home Health Recipients. Home Health Care Management & Practice, 24(1), 27–37. doi: 10.1177/1084822311419498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor M, Hanlon A, Naylor MD & Bowles KH (2015). The impact of home health length of stay and number of skilled nursing visits on hospitalization among Medicare-reimbursed skilled home health beneficiaries. Research in Nursing and Health, 38(4), 257–267. doi: 10.1002/nur.21665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng TR, Navaie-Waliser M, & Feldman PH (2003). Social support, home health service use, and outcomes among four racial-ethnic groups. The Gerontologist, 43(4), 503–513. doi: 10.1093/geront/43.4.503 [DOI] [PubMed] [Google Scholar]
- Popejoy LL, Galambos C, Stetzer F, Popescu M, Hicks L, Khalilia MA, … Marek KD (2015). Comparing Aging in Place to home health care: Impact of nurse care coordination on utilization and costs. Nursing Economic$, 33(6), 306–313. [PMC free article] [PubMed] [Google Scholar]
- Portanova J, Ailshire J, Perez C, Rahman A, & Enguidanos S (2017). Ethnic differences in advance directive completion and care preferences: What has changed in a decade? Journal of the American Geriatrics Society, 65(6), 1352–1357. 10.1111/jgs.14800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remler DK, Teresi JA, Weinstock RS, Ramirez M, Eimicke JP, Silver S, & Shea S (2011). Health care utilization and self-care behaviors of Medicare beneficiaries with diabetes: comparison of national and ethnically diverse underserved populations. Population Health Management, 14(1), 11–20. 10.1089/pop.2010.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Galik E, Gruber-Baldini A, & Zimmerman S (2011). Testing the effect of function-focused care in assisted living. Journal of the American Geriatrics Society, 59(12), 2233–40. 10.1111/j.1532-5415.2011.03699.x [DOI] [PubMed] [Google Scholar]
- Resnick B & Galik E (2013). Using function-focused care to increase physical activity among older adults. Annual Review of Nursing Research, 31, 175–208. 10.1891/0739-6686.31.175 [DOI] [PubMed] [Google Scholar]
- Rönneikkö JK, Mäkelä M, Jämsen ER, Huhtala H, Finne-Soveri H, Noro A, & Valvanne JN (2017). Predictors for unplanned hospitalization of new home care clients. Journal of the American Geriatrics Society, 65(2), 407–414. 10.1111/jgs.14486 [DOI] [PubMed] [Google Scholar]
- Rosati RJ, Russell D, Peng T, Brickner C, Kurowski D, Christopher MA, & Sheehan KM (2014). Medicare home health payment reform may jeopardize access for clinically complex and socially vulnerable patients. Health Affairs, 33(6), 946–956. 10.1377/hlthaff.2013.1159 [DOI] [PubMed] [Google Scholar]
- Saef SH, Carr CM, Bush JS, Bartman MT, Sendor AB, Zhao W, … Obeid JS (2016). A comprehensive view of frequent emergency department users based on data from a regional HIE. Southern Medical Journal, 109(7), 434–439. 10.14423/SMJ.0000000000000488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sands LP, Wang Y, McCabe GP, Jennings K, Eng C, & Covinsky KE (2006). Rates of acute care admissions for frail older people living with met versus unmet activity of daily living needs. Journal of the American Geriatrics Society, 54(2), 339–344. 10.1111/j.1532-5415.2005.00590.x [DOI] [PubMed] [Google Scholar]
- Scharpf TP, & Madigan EA (2010). Functional status outcome measures in home health care patients with heart failure. Home Health Care Services Quarterly, 29(4), 155–170. 10.1080/01621424.2010.534044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker RE, Powell MC, & Goodrich GK (2005). Initial home health outcomes under prospective payment. Health Services Research, 40(1), 177–193. 10.1111/j.1475-6773.2005.00348.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sefcik JS, Ritter AZ, Flores EJ, Nock RH, Chase J-AD, Bradway C, … Bowles KH (2017). Why older adults may decline offers of post-acute care services: A qualitative descriptive study. Geriatric Nursing (New York, N.Y.), 38(3), 238–243. 10.1016/j.gerinurse.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sefcik JS, Nock RH, Flores EJ, Chase JD, Bradway C, Potashnik S, & Bowles KH (2016). Patient preferences for information on post-acute care services. Research in Gerontological Nursing, 9(4), 175–182. doi: 10.3928/19404921-20160120-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J, Chang RW, Manheim LM, & Dunlop DD (2006). Gender differences across race/ethnicity in use of health care among Medicare-aged Americans. Journal of Women’s Health (2002), 15(10), 1205–1213. 10.1089/jwh.2006.15.1205 [DOI] [PubMed] [Google Scholar]
- Towne SD, Probst JC, Mitchell J, & Chen Z (2015). Poorer quality outcomes of Medicare-Certified home health care in areas with high levels of Native American/Alaska Native residents. Journal of Aging and Health, 27(8), 1339–1357. 10.1177/0898264315583051 [DOI] [PubMed] [Google Scholar]
- Tullai-McGuinness S, Madigan EA, & Fortinsky RH (2009). Validity testing the Outcomes and Assessment Information Set (OASIS). Home Health Care Services Quarterly, 28(1), 45–57. 10.1080/01621420802716206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weech-Maldonado R, Fongwa MN, Gutierrez P, & Hays RD (2008). Language and regional differences in evaluations of Medicare managed care by Hispanics. Health Services Research, 43(2), 552–568. 10.1111/j.1475-6773.2007.00796.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weech-Maldonado R, Morales LS, Elliott M, Spritzer K, Marshall G, & Hays RD (2003). Race/ethnicity, language, and patients’ assessments of care in Medicaid managed care. Health Services Research, 38(3), 789–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins VM, Bruce ML, & Sirey JA (2009). Caregiving tasks and training interest of family caregivers of medically ill homebound older adults. Journal of Aging and Health, 21(3), 528–542. 10.1177/0898264309332838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeboah-Korang A, Kleppinger A, & Fortinsky RH (2011). Racial and ethnic group variations in service use in a national sample of Medicare home health care patients with type 2 diabetes mellitus. Journal of the American Geriatrics Society, 59(6), 1123–1129. 10.1111/j.1532-5415.2011.03424.x [DOI] [PMC free article] [PubMed] [Google Scholar]