Abstract
Market-based reforms in health care, such as public reporting of quality, may inadvertently exacerbate disparities. We examined how the Centers for Medicare and Medicare Services’ five-star rating system for nursing homes has affected residents who are dually enrolled in Medicare and Medicaid (“dual eligibles”), a particularly vulnerable and disadvantaged population. Specifically, we assessed the extent to which dual eligibles and non–dual eligibles avoided the lowest-rated nursing homes and chose the highest-rated homes once the five-star rating system began, in late 2008. We found that both populations resided in betterquality homes over time but that by 2010 the increased likelihood of choosing the highest-rated homes was substantially smaller for dual eligibles than for non–dual eligibles. Thus, the gap in quality, as measured by a nursing home’s star rating, grew over time. Furthermore, we found that the benefit of the five-star system to dual eligibles was largely due to providers’ improving their ratings, not to consumers’ choosing different providers. We present evidence suggesting that supply constraints play a role in limiting dual eligibles’ responses to quality ratings, since high-quality providers tend to be located close to relatively affluent areas. Increases in Medicaid payment rates for nursing home services may be the only long-term solution.
It is well known that market failures in health care contribute to lower quality for consumers.1 These failures are related to both demand- and supply-side factors. On the demand side, people often cannot make informed choices as a result of asymmetric information about product quality, which means in this case that patients have less information about quality than providers do. On the supply side, providers often do not compete on the basis of quality because of factors such as administratively set prices and regulations that impede competition.
These market failures are frequently amplified in long-term care, where demand is driven by people who are often among the most vulnerable—the frail elderly with cognitive impairment—and who are potentially less able to search out and use information about quality. Many of these consumers lack family and financial resources to help them choose a care setting.
Supply-side competition in long-term care markets is blunted by a high degree of government involvement. In particular, Medicaid is the dominant payer of nursing home care, typically paying a rate far below the private-pay price. Moreover, long-term care markets are heavily regulated, which further impedes provider competition. For example, “certificate of need” laws in many states restrict the supply of nursing home beds so that it is difficult for new nursing homes to enter the market.
Government intervention in health care markets is often designed to make them more like well-functioning markets for other products. Such market-based approaches to improving health care quality are popular across the political spectrum, in part because they are intuitively appealing.
Perhaps the most prominent of market-based reforms in recent decades is the public reporting of health care quality. This is a direct attempt to solve the problem of asymmetric information by putting information about quality in the public domain. However, the evidence that consumers respond to such public reporting by choosing higher-quality providers is mixed.2,3 Research on health plans,4–7 hospitals,8,9 and cardiac surgeons4 has shown that providers that receive high rankings in publicly reported quality assessments do not consistently gain market share.
Two prior studies have examined the consumer response to public reporting in the nursing home sector. In research on long-stay nursing home residents, David Grabowski and Robert Town10 found that the release of nursing home quality information in the form of residents’ clinical outcome measures had no discernible effect on nursing homes’ market share. In a study of nursing home residents who were receiving postacute care, Rachel Werner and colleagues11 found that quality ratings for pain control had a significant effect on nursing home choice, but the size of the effect was small.
We examined whether the most disadvantaged among nursing home residents—those dually enrolled in Medicare and Medicaid—benefit from the public reporting of quality, and we posit potential reasons why dual eligibles benefit less than non–dual eligibles do. Nursing home residents might experience improved care from public reporting in two ways. First, in choosing a nursing home, they might use publicly reported information to select a higher-ranked facility than they would have otherwise. Second, public reporting might motivate nursing homes to improve the quality of care they deliver. Residents already in nursing homes might benefit in this second way, if the nursing home they reside in improves its quality. These benefits might accrue unevenly across nursing home residents.
The intervention we studied was the five-star rating system introduced by the Centers for Medicare and Medicaid Services (CMS) in late 2008. There is little empirical evidence about the effectiveness of this system. Importantly, our goal was to examine responses to the intervention of the rating system, not to evaluate whether the rating system is an accurate reflection of nursing home quality.
Dually Enrolled Beneficiaries
People who are enrolled in both Medicare and Medicaid (often called dual eligibles) have been the focus of increased policy attention in recent years as a result of their disproportionate use of health care services and share of costs. Dual eligibles account for only 15 percent of Medicaid enrollment and 21 percent of Medicare enrollment. However, they account for 39 percent of Medicaid expenditures and 36 percent of Medicare expenditures.12
Dual eligibles are a vulnerable population: They are much more likely than other Medicare beneficiaries to have incomes of less than $10,000, be cognitively impaired, have less than a high school education, be in only fair or poor health, be disabled, be members of a racial or ethnic minority group, and reside in a nursing home.13 Dual eligibles are also more likely than other nursing home residents to receive care in poor neighborhoods.14 And they are subject to misaligned and conflicting policy incentives from Medicare and Medicaid.15 Dual eligibles are thus more likely than other nursing home residents to receive low-quality health care.14
Nursing home residents who are dual eligibles are a heterogeneous group, and dual status does not necessarily imply previous poverty or a low level of education. Sometimes the high cost of nursing home care leads Medicare beneficiaries to spend down their private resources until reliance on Medicaid becomes necessary. An estimated 10 percent of nursing home residents transition to Medicaid during a nursing home stay—some of whom may have transferred assets in anticipation of needing nursing home care.16,17 Nonetheless, the consequences of being dependent on Medicaid are likely to apply regardless of the pathway to Medicaid enrollment.
A substantial body of research has linked low-quality nursing home care to residents’ source of payment. Nursing homes are funded largely by public payers, with approximately two-thirds of the residents in a typical facility on Medicaid (the majority of them are dual eligibles). Another 12 percent are funded by Medicare for postacute care, and most of the rest pay for their care privately.18 Medicaid generally provides the lowest reimbursement rates of any payer, and, as a result, nursing homes generally prefer private-paying residents or those with Medicare.
Despite this payer-based disparity in reimbursement rates, researchers have not found that Medicaid residents receive lower-quality care than Medicare residents within a given facility.19,20 Instead, there are differences in quality across nursing homes associated with the proportion of residents on Medicaid at each facility. A high proportion of Medicaid residents is presumed to be responsible for a low level of resources.14
Dual eligibles are more likely than others to reside in low-quality nursing homes and thus to receive low-quality care.
Therefore, dual eligibles are more likely than others to reside in low-quality nursing homes and thus to receive low-quality care. And because dual eligibles are generally sicker than other residents, the low quality of care they receive may affect them more.
The Five-Star Rating System
In 2002 CMS publicly released a Web-based report card called Nursing Home Compare, which detailed the quality of care at all Medicare- or Medicaid-certified nursing homes. The rating system included numerous individual measures of staffing, regulatory compliance, and clinical outcomes. In December 2008 CMS launched a new rating system of nursing homes that aggregated the information into a rating system of one to five stars, with more stars indicating better quality.
In contrast to the 2002 system, the star rating system was intended to provide highly simplified information in a form that consumers would find familiar. The stars are based on three domains of quality: ratios of staff members to residents, residents’ clinical outcomes, and the results of regulatory inspections. The overall rating combines the three domains. In this article we focus on the overall star ratings on the assumption that these garner the most attention from both providers and consumers.21
Public reporting systems such as the five-star rating system are designed to improve quality of care. However, it is unknown how public reporting affects vulnerable populations specifically.
On the one hand, public reporting might improve care for such populations. Because low-quality providers have the most to lose from the revealing of quality scores and have the greatest potential for improvement under public reporting,22 and because underserved patients are concentrated in low-quality providers,14,23,24 disparities in quality could decrease through improvements in quality among such providers. In addition, well-educated consumers with more resources may be better positioned to judge the quality of facilities in the absence of public reporting, so the benefit of new and easier-to-access information may go disproportionately to less-well-educated consumers with fewer resources.25,26
On the other hand, vulnerable populations might not benefit from public reporting as much as other groups do. One study of Medicare-funded postacute care patients in nursing homes found that the response to the 2002 version of Nursing Home Compare was greater among highly educated consumers, compared to those with less education.11
Nursing homes that serve large populations of dual eligibles are less likely than other nursing homes to have the resources necessary to improve quality in response to public reporting. In addition, dual eligibles may be less able to benefit from quality information, either because they live in an area with few high-quality providers or few Medicaid beds at high-quality facilities, or because dual eligibles are less able to access and understand the information than non–dual eligibles are. Despite concern about the effects of public reporting on vulnerable populations, there is little empirical evidence about those effects.25,27–29
We hypothesized that dual eligibles benefited less than non–dual eligibles from the introduction of the five-star nursing home rating system. We tested this hypothesis by examining changes in the probability that members of the two groups would reside in a one-star or a five-star nursing home before and after the rating system was introduced. We also assessed the extent to which changes in the probability of residing in a one-star or five-star nursing home were due to providers’ improving their ratings over time or to consumers’ choosing different nursing homes.
Study Data And Methods
In addition to basic descriptive analyses, we assessed these issues using difference-in-differences models, comparing residence in one-star and five-star nursing homes over time for dual eligibles and non–dual eligibles.
DATA
Our analysis used data from 2008–10, a period that spanned the introduction of the five-star system in December 2008. We used three main data sets: Nursing Home Compare data; the Nursing Home Minimum Data Set, version 2.0; and the Medicare Beneficiary Summary File.
The Nursing Home Compare data included star ratings for each nursing home for each month during the study period, including unpublished ratings for 2008. The Nursing Home Minimum Data Set contained clinical assessment data collected at regular intervals for every resident in a Medicare- or Medicaid-certified nursing home, regardless of payer source. We used this data set to obtain numbers and demographic and health characteristics of people in the sample. The Medicare Beneficiary Summary File was the source of our indicator for dual-eligible status.
Because our study focused on the long-stay population of nursing homes, we limited the sample to long-stay residents (those who spent at least ninety days in the nursing home). Each long-stay resident is assessed at least quarterly in the Nursing Home Minimum Data Set, including on admission, annually, quarterly, and at any significant change in status. We limited our sample to people who had at least one quarterly or annual assessment or an assessment because of a significant change in health status and who also had had one prior assessment of those types or an assessment on admission.
For people who had more than one assessment in a given quarter, we used only the last assessment. This avoided overweighting sicker residents who might have had more frequent assessments.
We excluded assessments for short-term stays for postacute care, but we included subsequent quarterly and annual assessments and those at any significant change for people who entered the nursing home through a postacute care stay and transitioned to long-term care. We merged these assessments with the facility star ratings for the middle month of each quarter.
Our goal in defining the sample was to generate a comprehensive view of the long-stay population during any given quarter in our study period. However, we allowed this population to change over time as a result of both admissions and discharges. Our sample included new admissions during the study period, even if residents entered the nursing home through a stay for postacute care—as long as they remained in the nursing home long enough to have a qualifying long-stay Nursing Home Minimum Data Set assessment.
Our sample consisted of 16,065,677 resident-quarter assessments from 5,591,356 residents of 15,894 nursing homes. On average, each resident in the sample was present for 3.3 quarters out of the 11 quarters in the study period. Thus, while providing a snapshot of the long-stay population each quarter, this definition of the sample gave us ample opportunity to detect both consumer-driven and provider-driven changes over time in the ratings of nursing homes.
There was very little facility entry (new homes beginning to operate) and exit (existing homes ceasing to operate) during the study period. Excluding those facilities that did not operate throughout the study period made no meaningful difference to the results.
Following standard practice, we defined dual eligibles as people who had full Medicaid coverage in addition to Medicare at any point during a quarter.30 All others were considered non–dual eligibles. Most of the non–dual eligibles were Medicare beneficiaries. However, because Medicare does not cover chronic care stays in nursing homes, those residents had to pay for their longterm stay through private funds or other government sources—for example, Veterans Affairs or TRICARE funds.
ANALYSIS
To assess the issue of differential effects between dual eligibles and non–dual eligibles, we began with a descriptive analysis of where each group received care over time, specifically in the two quarters in 2008 before the release of the star ratings and in the seven quarters in 2009–10 after the release.
For a more precise estimate of magnitudes and the ability to include control variables, we assessed the differential trends for dual eligibles and non–dual eligibles. We used difference-indifferences regression models, with resident-quarter observations as our unit of analysis. We modeled the probability of a resident’s being in a one-star (or, separately, in a five-star) nursing home as a function of year dummies (with 2008 as the reference), dual-eligible status, and interactions between that status and each year dummy.
We ran these regressions with and without case-mix controls. For ease of interpretation, we present linear probability models. As a robustness check, we ran nonlinear models (including ordered probit regressions of the complete range of stars). They produced similar results, so we do not present the nonlinear models.
To examine whether dual eligibles’ residence in better-rated nursing homes over time was due more to provider behavior or to differences in nursing home choice by consumers, we ran stratified regressions among dual eligibles and non–dual eligibles. We exploited the fact that inclusion of a nursing home fixed effect (essentially, a site dummy) gave within-facility estimates of changes in star ratings over time—that is, provider-driven changes in star ratings, holding consumer choice constant. Without the fixed effects, differences in star ratings for dual eligibles over time would reflect a combination of provider-driven changes and changes in the distribution of dual eligibles across different types of facilities.
Specifically, we modeled whether a person resided in a one-star or a five-star facility as a function of year dummy variables for 2009 and 2010 (using 2008 as a reference), with and without facility fixed effects. If dissimilar estimates resulted from these two regressions, consumer response was likely to be a significant factor in explaining changes in star ratings. Similar estimates would indicate that the changes were largely provider driven.
Study Results
Characteristics of dual eligibles and non-dual eligibles in US nursing homes are displayed in online Appendix Exhibit A1.31 Approximately 64 percent of long-stay nursing home residents were dual eligibles. Consistent with expectations, dual eligibles were more likely to be female and less likely to have a high school or college degree, compared to non–dual eligibles. Dual eligibles were disproportionately more likely than non–dual eligibles to be members of a minority group. However, more than three-quarters of dual eligibles were non-Hispanic whites. Dual eligibles also had higher rates of mental illness and dementia, compared to non–dual eligibles.
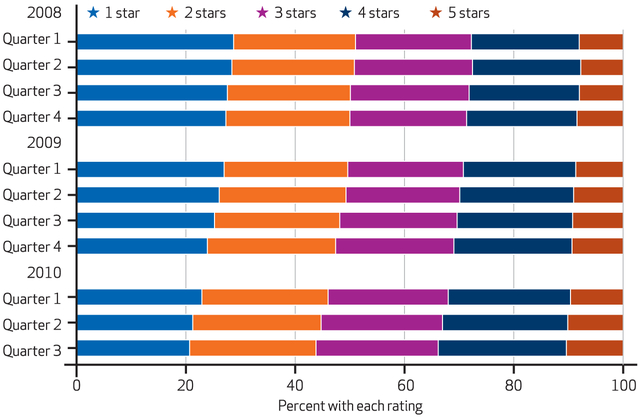
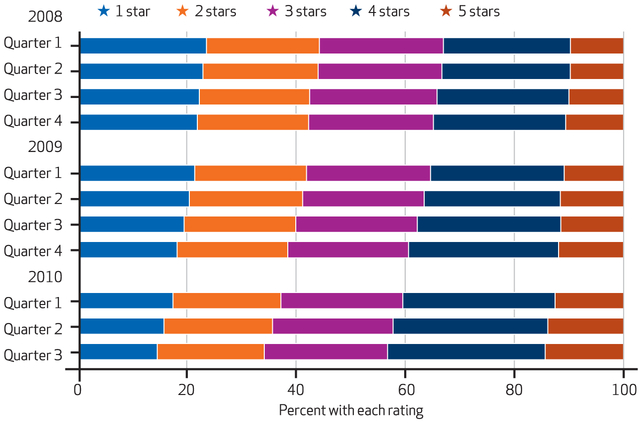
Exhibits 1 and 2 depict the distribution of dual eligible and non–dual eligible residents of nursing homes by the homes’ star ratings. The leftward shift of the distributions over time indicates that both groups were less likely to reside in the lowest-rated homes over time and more likely to reside in the highest-rated homes. For example, at baseline (in the first quarter of 2008), more than a quarter of dual eligibles in nursing homes resided in one-star homes, a proportion that decreased to approximately a fifth by the third quarter of 2010. Although both groups appeared to reside in better-rated nursing homes over time, the distribution for non–dual eligibles was more favorable than that for dual eligibles in any given year.
EXHIBIT 1. Star Ratings Of Nursing Homes In Which Dual Eligibles Resided, 2008-10.
SOURCE Authors’ analysis of data from the Centers for Medicare and Medicaid Services: Nursing Home Compare; the Nursing Home Minimum Data Set, version 2.0; and the Medicare Beneficiary Summary File.
EXHIBIT 2. Star Ratings Of Nursing Homes In Which Non-Dual Eligibles Resided, 2008-10.
SOURCE Authors’ analysis of data from the Centers for Medicare and Medicaid Services: Nursing Home Compare; the Nursing Home Minimum Data Set, version 2.0; and the Medicare Beneficiary Summary File data.
Regression results captured the magnitude and significance of these shifts (Exhibit 3). At baseline (in 2008), dual eligibles were 4 percentage points more likely to be in a one-star home and 1.5 percentage points less likely to be in a five-star home, compared to non–dual eligibles. Non–dual eligibles’ likelihood of being in a one-star home declined, and their likelihood of being in a five-star home increased. The same was true of dual eligibles, and the decline in likelihood of residing in one-star facilities was not significantly different for the two groups.
EXHIBIT 3.
Effects Of Dual Eligible Status On Residence In One-Star Or Five-Star Nursing Homes, 2008-10
| Rating of nursing home |
||
|---|---|---|
| One star | Five stars | |
| Dual eligibles, 2008 (relative to non–dual eligibles)a | 0.040*** | −0.015*** |
| Dual-eligible status interacted with yearb | ||
| 2009 | 0.003 | −0.004 |
| 2010 | 0.002 | −0.014*** |
| Time trend for non–dual eligibles | ||
| 2009 | −0.027*** | 0.015*** |
| 2010 | −0.065*** | 0.036*** |
| Constant | 0.358*** | 0.053*** |
SOURCE Authors’ analysis of data from the Centers for Medicare and Medicaid Services: Nursing Home Compare; the Nursing Home Minimum Data Set, version 2.0; and the Medicare Beneficiary Summary File. NOTES There were 16,065,677 resident-quarter assessments in both categories of nursing homes. Both regressions controlled for residents’ demographic characteristics and health status. Full regression results are available in Appendix Exhibit A2 (see Note 31 in text). Estimation used linear probability regression models.
Baseline adjusted difference in the probability of being in a one-star or a five-star nursing home for dual eligibles, relative to non–dual eligibles.
Extent to which time trends were different for dual eligibles and non–dual eligibles.
p<0.01
However, by 2010 dual eligibles had experienced a smaller increase than non–dual eligibles in the shift toward five-star facilities. Whereas non–dual eligibles were 3.6 percentage points more likely to reside in a five-star nursing home in 2010 versus 2008 (Exhibit 3), the increase for dual eligibles was only 2.2 percentage points—that is, the 3.6-percentage-point-increase for non–dual eligibles minus the 1.4-percentage-point differential for dual eligibles (Exhibit 3).
Results of the stratified regressions comparing time trends with and without nursing home fixed effects are shown in Exhibit 4. For dual eligibles, the coefficients on the time trends produced extremely similar results whether or not we included those fixed effects in the model. Thus, the demonstrated shifts among dual eligibles away from one-star facilities and toward five-star facilities cannot be attributed to dual eligibles’ using the information on Nursing Home Compare to choose more highly rated nursing homes over time. Instead, dual eligibles have generally remained in (exhor have chosen) the same nursing homes that they were (or would have been) admitted to in 2008, but some of these nursing homes have achieved higher star ratings over time.
EXHIBIT 4.
Time Trends In Residence Of Dual Eligibles And Non–Dual Eligibles In One-Star Or Five-Star Nursing Homes
| Rating of nursing home |
||||
|---|---|---|---|---|
| One star |
Five stars |
|||
| Total change |
Provider-driven change |
Total change |
Provider-driven change |
|
| DUAL ELIGIBLES ONLY | ||||
| 2009 | −0.023 | −0.022 | 0.010 | 0.010 |
| 2010 | −0.062 | −0.059 | 0.020 | 0.020 |
| Constant | 0.277 | 0.275 | 0.080 | 0.080 |
| NON–DUAL ELIGIBLES ONLY | ||||
| 2009 | −0.027 | −0.020 | 0.014 | 0.012 |
| 2010 | −0.066 | −0.054 | 0.035 | 0.032 |
| Constant | 0.222 | 0.216 | 0.099 | 0.101 |
SOURCE Authors’ analysis of data from the Centers for Medicare and Medicaid Services: Nursing Home Compare; the Nursing Home Minimum Data Set, version 2.0; and the Medicare Beneficiary Summary File.NOTES “Total change” is without nursing home fixed effects. “Provider-driven change” is with nursing home fixed effects. Regression results, including t-statistics, are available in Appendix Exhibit A3 (see Note 31 in text). Estimates are based on linear probability regression models. All results are significant (p<0.01).
For non–dual eligibles, in contrast, the effects varied more, which indicates the presence of some consumer-driven response. For example, by 2010 non–dual eligibles were 6.6 percentage points less likely to be in a one-star nursing home, compared to 2008. Of that total, 1.2 percentage points were due to consumers’ having gone to different nursing homes, while 5.4 percentage points could be attributed to provider-driven improvement in ratings. However, dual eligibles were 6.2 percentage points less likely to be in a one-star nursing home in 2010 than in 2008, with only 0.3 percentage point of the change being the result of consumers’ going to different nursing homes.
As a robustness check, we estimated our main regressions with and without controlling for residents’ characteristics. Education and race were significant in the expected direction: More highly educated people and non-Hispanic whites were more likely to receive care in highly rated nursing homes, compared to less educated people and nonwhites.
However, the improvements over time were very similar with and without the controls. This suggests that dual-eligible status itself (not simply as a proxy for race or ethnicity, health status, or education) likely plays an important role in the choice of nursing homes. That finding is consistent with the literature on Medicaid payment and quality of care.14,29
Discussion
Our finding that dual eligibles tend to reside in lower-quality nursing homes was unsurprising and consistent with prior literature.14,29 However, we provide new evidence of the following three points: Dual eligibles have increasingly been served by more highly rated nursing homes since the beginning of the five-star system; the shift toward higher-quality homes was smaller for dual eligibles than for non–dual eligibles; and the shift toward more highly rated homes among dual eligibles appears to be a result of providers’ improving their ratings over time, not of dual eligibles’ increasingly choosing different providers over time. Consumer response to the five-star rating system among non–dual eligibles has been somewhat larger than among dual eligibles.
There are multiple ways for nursing homes to improve their scores beyond actually improving quality.
INFORMATION ON QUALITY
Why dual eligibles benefit less than non–dual eligibles from the public reporting of nursing home quality is less clear. However, investigating this question is crucial to the formulating of appropriate policy to address this disparity. Interest often centers on access to and usability of quality information. Researchers have found that consumers have difficulty processing a large number of quality metrics32,33 and using quality metrics to judge a provider’s overall quality.34,35 Misunderstanding is more common among patients of lower socioeconomic status.36
In the case of nursing home residents, many of whom suffer from cognitive impairment, their placement in a particular home is likely to be heavily influenced by families and referring physicians. However, the extent to which these groups use quality reports is unknown and largely unstudied.
In contrast to prior evidence that education enhanced the response of Medicare-funded postacute care patients to public reporting of nursing home quality,11 our results indicate that education did not mediate the effect of dual-eligible status on benefit from public reporting. To the extent that education is a proxy for the ability to access and use Web-based quality information, this suggests that increasing access to the information may not be very effective in the presence of Medicaid payment.
SUPPLY CONSTRAINTS
How supply constraints affect vulnerable populations under public reporting has received less attention. Supply constraints may take the form of living a long way from a highly rated nursing home or of the inability to access a Medicaid bed in a highly rated nursing home. Fewer nursing homes are located in neighborhoods whose residents are predominantly members of racial minority groups, and the nursing homes there tend to be of lower quality than those in neighborhoods whose residents are predominantly white.14,37,38 One study that examined nursing home placement by race found that the local supply of skilled nursing beds was a barrier to entering a nursing home for blacks, but not for whites.39
In addition, because Medicaid provides the lowest payment rates in the nursing home sector, a long history of access problems for Medicaid residents has been documented, especially when occupancy rates are high.40 The access challenges associated with Medicaid payment may be the main drivers of the disparate effects we found between dual eligibles and non–dual eligibles.
Indeed, when we examined the geographic location of five-star nursing homes, we found evidence that suggested supply constraints for dual eligibles. Using the greater Chicago area as an example, online Appendix Exhibit A431 depicts the geographic distribution of nursing homes by star ratings and by median household income of each census tract. The distribution of green squares suggests that consumers throughout the greater Chicago area live within a relatively short distance of at least one low-quality (one-star) nursing home. The dark blue squares, however, demonstrate that five-star nursing homes have a very limited geographic distribution: Most of them are near the higher-income areas in the northern part of the city.
Thus, a consumer on the South Side of Chicago (in one of the poorer neighborhoods) would likely have to travel a great distance to reach a five-star nursing home. This suggests that supply constraints may help explain the lack of response to public reporting of quality among dual eligibles.
Solving the issue of supply constraints is an inherently difficult policy problem. The location decisions of nursing home providers are complex and likely involve proximity to referral sources as well as the socioeconomic status of the surrounding neighborhood. However, the reality is that few highly rated nursing homes exist in or near poorer neighborhoods.
The nursing home sector is largely for profit, and financial incentives may favor location in more affluent neighborhoods. Location in less affluent areas generally means operating on Medicaid reimbursement rates, as nursing home residents tend to be local. In turn, dependence on Medicaid reimbursement rates may limit a nursing home’s ability to improve its quality over time.
A substantial increase in the Medicaid rate or a systematic replacement of Medicaid with a national insurance system for long-term care might be the only solutions that would lead to dramatic change. However, both seem politically unlikely for the time being.
An alternative to changing the incentives for location would be to pursue policies that incentivize low-rated nursing homes to improve their quality, which is one of the goals of public reporting. Our results indicate that this provider-driven improvement was responsible for the bulk of the change in distribution of star ratings for dual eligibles between 2008 and 2010, consistent with evidence on provider-driven improvement overall during this period.41
Conclusion
Our goal was to analyze changes in the ratings of nursing homes in which dual eligibles reside, since the ratings are a major policy intervention in which CMS continues to invest substantial resources. However, for these changes to indicate an increase in the well-being of dual eligibles, an improvement in the star ratings must reflect an actual improvement in quality. Recent press coverage casts doubt on this assumption.42 There are multiple ways for nursing homes to improve their scores beyond actually improving quality, such as changing their coding practices and avoiding sicker residents.
The fact that dual eligibles as a group have found themselves to some extent in better-rated nursing homes over time may be taken as a good sign, with the caveat that the ratings might not indicate the homes’ true quality. However, the gap between dual eligibles and non–dual eligibles still grew slightly over time. The latter group experienced a larger shift toward highly rated nursing homes, in part driven by consumer response to the five-star rating system among non–dual eligibles.
Well-intentioned policies often have heterogeneous effects, and it remains open to debate whether average improvement is beneficial if disparities increase. Our analysis revealed a growing disparity within just a few years of the release of the five-star Nursing Home Compare rating system. As time goes on, public reporting could perpetuate and exacerbate this disparity. Any evaluation of the success of an intervention such as public reporting needs to consider the heterogeneity of effects as well as average effects.
In the case of nursing homes, a small overall effect that is subject to significant heterogeneity might not be surprising, and there may be additional heterogeneity within the broad categories of dual eligibles and non–dual eligibles. Decisions about nursing home choice depend upon many factors in addition to quality. In addition, consumers’ responses to quality measures may depend in part on the extent to which they find the measures valid and useful.
The list of potential market failures (such as asymmetric information, constrained supply, and constrained price) in long-term care is long, and policies to mitigate any one of them in isolation are unlikely to lead to dramatic improvement. Even if the problem of asymmetric information is addressed through public reporting of health care quality, other market failures, such as constrained supply, may prove more intractable barriers to the existence of well-functioning markets. ■
Supplementary Material
Acknowledgments
Results from this analysis were presented at the International Conference for Evidence-Based Policy in Long-Term Care, London, England, September 2, 2014, and at the annual meeting of the Gerontological Society of America, Washington, D.C., November 8, 2014. The authors gratefully acknowledge funding from the Agency for Healthcare Research and Quality (Grant No. R21HS021877).
Contributor Information
R. Tamara Konetzka, Department of Public Health Sciences at the University of Chicago, in Illinois..
David C. Grabowski, Harvard Medical School, in Boston, Massachusetts..
Marcelo Coca Perraillon, Department of Public Health Sciences at the University of Chicago..
Rachel M. Werner, University of Pennsylvania, in Philadelphia..
NOTES
- 1.Akerlof GA. The market for “lemons”: quality uncertainty and market mechanism. Q J Econ. 1970;84(3):488–500. [Google Scholar]
- 2.Fung CH, Lim YW, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148(2):111–23. [DOI] [PubMed] [Google Scholar]
- 3.Marshall MN, Shekelle PG, Leatherman S, Brook RH. The public release of performance data: what do we expect to gain? A review of the evidence. JAMA. 2000;283(14):1866–74. [DOI] [PubMed] [Google Scholar]
- 4.Dranove D, Sfekas A. Start spreading the news: a structural estimate of the effects of New York hospital report cards. J Health Econ. 2008;27(5):1201–7. [DOI] [PubMed] [Google Scholar]
- 5.Chernew M, Gowrisankaran G, Scanlon DP. Learning and the value of information: evidence from health plan report cards. J Econom. 2008;144(1):156–74. [Google Scholar]
- 6.Wedig GJ, Tai-Seale M. The effect of report cards on consumer choice in the health insurance market. J Health Econ. 2002;21(6):1031–48. [DOI] [PubMed] [Google Scholar]
- 7.Jin GZ, Sorensen AT. Information and consumer choice: the value of publicized health plan ratings. J Health Econ. 2006;25(2):248–75. [DOI] [PubMed] [Google Scholar]
- 8.Baker DW, Einstadter D, Thomas C, Husak S, Gordon NH, Cebul RD. The effect of publicly reporting hospital performance on market share and risk-adjusted mortality at high-mortality hospitals. Med Care. 2003;41(6):729–40. [DOI] [PubMed] [Google Scholar]
- 9.Cutler DM, Huckman RS, Landrum MB. The role of information in medical markets: an analysis of publicly reported outcomes in cardiac surgery. Am Econ Rev. 2004;94(2):342–6. [DOI] [PubMed] [Google Scholar]
- 10.Grabowski DC, Town RJ. Does information matter? Competition, quality, and the impact of nursing home report cards. Health Serv Res. 2011;46(6 pt1):1698–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Werner RM, Norton EC, Konetzka RT, Polsky D. Do consumers respond to publicly reported quality information? Evidence from nursing homes. J Health Econ. 2012;31(1):50–61. [DOI] [PubMed] [Google Scholar]
- 12.Henry J Kaiser Family Foundation. Affordable Care Act provisions relating to the care of dually eligible Medicare and Medicaid beneficiaries [Internet]. Menlo Park (CA): KFF; 2011. May [cited 2015 Mar 6]. Available from: http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8192.pdf [Google Scholar]
- 13.Kaiser Commission on Medicaid and the Uninsured. Dual eligibles: Medicaid’s role for low-income Medicare beneficiaries [Internet]. Washington (DC): The Commission; 2011. May [cited 2015 Mar 6]. Available from: http://kaiserfamilyfoundation.files.wordpress.com/2013/01/4091-08.pdf [Google Scholar]
- 14.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank Q. 2007;85(4):579–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spence DA, Wiener JM. Estimating the extent of Medicaid spend-down in nursing homes. J Health Polit Policy Law. 1990;15(3):607–26. [DOI] [PubMed] [Google Scholar]
- 17.Taylor DH Jr, Sloan FA, Norton EC. Formation of trusts and spend down to Medicaid. J Gerontol B Psychol Sci Soc Sci. 1999;54(4):S194–201. [DOI] [PubMed] [Google Scholar]
- 18.Norton EC. Long-term care In: Cuyler AJ, Newhouse JP, editors. Handbook of health economics. Amsterdam: Elsevier; 2000. Vol. 1B p. 955–94. [Google Scholar]
- 19.Grabowski DC, Gruber J, Angelelli JJ. Nursing home quality as a common good. Rev Econ Stat. 2008;90(4):754–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Troyer JL. Examining differences in death rates for Medicaid and non-Medicaid nursing home residents. Med Care. 2004;42(10):985–91. [DOI] [PubMed] [Google Scholar]
- 21.Rainwater J, Enders SR, Romano PS, Dhamar M, Tancredi D. Evaluation of California’s Quality of Care Report Card: final report to the California Office of the Patient Advocate [Internet]. Davis (CA): UCD Center for Health Services Research in Primary Care; 2005. February [cited 2015 Mar 9]. Available from: http://www.opa.ca.gov/Documents/Reports/Evaluation-of-Californias-Quality-of-Care-Report-Card%28UCD2005%29.pdf [Google Scholar]
- 22.Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: from concept to practice. JAMA. 2005;294(14):1788–93. [DOI] [PubMed] [Google Scholar]
- 23.Goldman LE, Vittinghoff E, Dudley RA. Quality of care in hospitals with a high percent of Medicaid patients. Med Care. 2007;45(6):579–83. [DOI] [PubMed] [Google Scholar]
- 24.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–82. [DOI] [PubMed] [Google Scholar]
- 25.Chien AT, Chin MH, Davis AM, Casalino LP. Pay for performance, public reporting, and racial disparities in health care: how are programs being designed? Med Care Res Rev. 2007;64(5 Suppl):283S–304S. [DOI] [PubMed] [Google Scholar]
- 26.Mukamel DB, Weimer DL, Zwanziger J, Gorthy SF, Mushlin AI. Quality report cards, selection of cardiac surgeons, and racial disparities: a study of the publication of the New York State Cardiac Surgery Reports. Inquiry. 2004–05;41(4):435–46. [DOI] [PubMed] [Google Scholar]
- 27.Casalino LP, Elster A, Eisenberg A, Lewis E, Montgomery J, Ramos D. Will pay-for-performance and quality reporting affect health care disparities? Health Aff (Millwood). 2007;26(3):w405–14. DOI: 10.1377/hlthaff.26.3.w405. [DOI] [PubMed] [Google Scholar]
- 28.Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007;64(5 Suppl):7S–28S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konetzka RT, Werner RM. Disparities in long-term care: building equity into market-based reforms. Med Care Res Rev. 2009;66(5):491–521. [DOI] [PubMed] [Google Scholar]
- 30.Chronic Conditions Data Warehouse. Options for determining which CMS Medicare beneficiaries are dually eligible for Medicare and Medicaid benefits—a technical guidance paper [Internet]. [Place unknown]: Chronic Conditions Data Warehouse; 2014. February [cited 2015 Mar 16]. Available from: http://www.ccwdata.org/cs/groups/public/documents/training/ccw_dualeligibles_techguide.pdf [Google Scholar]
- 31.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 32.Peters E, Dieckmann N, Dixon A, Hibbard JH, Mertz CK. Less is more in presenting quality information to consumers. Med Care Res Rev. 2007;64(2):169–90. [DOI] [PubMed] [Google Scholar]
- 33.Schultz J, Call KT, Feldman R, Christianson J. Do employees use report cards to assess health care provider systems? Health Serv Res. 2001;36(3):509–30. [PMC free article] [PubMed] [Google Scholar]
- 34.Sibbald B, Addington-Hall J, Brenneman D, Obe PF. The role of counsellors in general practice. A qualitative study. Occas Pap R Coll Gen Pract. 1996(74):1–19. [PMC free article] [PubMed] [Google Scholar]
- 35.Hibbard JH, Jewett JJ. Will quality report cards help consumers? Health Aff (Millwood). 1997;16(3):218–28. [DOI] [PubMed] [Google Scholar]
- 36.Jewett JJ, Hibbard JH. Comprehension of quality care indicators: differences among privately insured, publicly insured, and uninsured. Health Care Financ Rev. 1996;18(1):75–94. [PMC free article] [PubMed] [Google Scholar]
- 37.Reed SC, Andes S. Supply and segregation of nursing home beds in Chicago communities. Ethn Health. 2001;6(1):35–40. [DOI] [PubMed] [Google Scholar]
- 38.Reed SC, Andes S, Tobias RA. Concentrated poverty and nursing home bed supply in Chicago. J Health Care Poor Underserved. 2001;12(1):88–102. [DOI] [PubMed] [Google Scholar]
- 39.Akamigbo AB, Wolinsky FD. New evidence of racial differences in access and their effects on the use of nursing homes among older adults. Med Care. 2007;45(7):672–9. [DOI] [PubMed] [Google Scholar]
- 40.Nyman JA. Prospective and “costplus” Medicaid reimbursement, excess Medicaid demand, and the quality of nursing home care. J Health Econ. 1985;4(3):237–59. [DOI] [PubMed] [Google Scholar]
- 41.Abt Associates, Colorado Foundation for Medical Care. Nursing Home Compare five-star quality rating system: year three report [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services; 2013. June 7 [cited 2015 Mar 9]. Available from: http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/FSQRSReport.pdf [Google Scholar]
- 42.Thomas K Medicare star ratings allow nursing homes to game the system. New York Times. 2014. August 24. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.