Abstract
An anorectal abscess, specifically a perianal abscess, is a relatively uncommon infection in children. It is a purulent fluid collection under the soft tissue outside the anus. Some of these abscesses may spontaneously drain and heal by themselves, while others may result in sepsis and require surgical intervention. The transition to a systemic illness requiring hospital admission is considered rare. We present the case of a 2-year-old male presenting with a febrile seizure and found to be systemically ill secondary to a perianal abscess. To our knowledge, this is the first case reported in the literature of a febrile seizure secondary to a perianal abscess.
INTRODUCTION
A perianal abscess occurs most often in male children <1 year of age; however, they can occur at any age and in either sex [1]. In one study, an incidence was reported of up to 4.3% [1]. In another study, only 16 pediatric perianal abscesses were identified over a 5-year period at one hospital, making it a rather rare presentation [2].
CASE REPORT
A 2-year-old male presented to the Emergency Department (ED) with his mother with the chief complaint of testicular swelling. The mother noted decreased appetite for the past 2 days, crying at night time and febrile up to 104°F at home. Prior to this, he had been acting normal, eating/drinking, urinating regularly and having bowel movements without difficulty. She noted increasing swelling from the right side of his scrotum to his anus that prompted the ED visit. His past medical history included being born at 38 weeks and 6 days via c-section. The patient was on no medications and had routine pediatric care.
Vitals on arrival to the ED were as follows: 103.1°F, blood pressure of 96/78 mmHg, respiratory rate 27 breaths/min, heart rate 126 beats/min, weight 12.8 kg and 100% oxygen saturation on room air. As soon as he was brought back to the treatment area, the patient was noted to have had a 20 s generalized tonic–clonic seizure. On physical examination, the patient appeared ill, lethargic, with mottling to the extremities. His head/neck examination was unremarkable. Cardiopulmonary examination revealed a tachycardic rate without murmur and clear lungs bilaterally. His abdominal/genitourinary examination revealed a soft abdomen, non-tender and non-distended. There was erythema and induration along the right perineal region consistent with cellulitis. This area was tracking anteriorly towards the scrotum with an associated perineal fluctuant mass (Fig. 1). The patient would cry to the palpation of this region. No other acute abnormalities were noted.
Figure 1:

Clinical image demonstrating erythema and induration along the right perineal region consistent with cellulitis. This area was tracking anteriorly towards the scrotum with an associated perineal fluctuant mass
Code sepsis was activated on arrival. Fluid resuscitation and intravenous vancomycin were initiated. Laboratory evaluation was notable for a neutrophil predominant leukocytosis of 18.9 (3.3–10.7 bil/l), a thrombocytosis of 522 (150–450 bil/l) and a hyponatremia of 132 (138–145 mmol/l). Ultrasound of the scrotum with Doppler and ultrasound of the perineal region were emergently performed. The left and right testicles were unremarkable with vascular flow demonstrated on color Doppler images with both arterial and venous waveforms identified. There was extensive soft tissue swelling/edema noted along the anterior and inferior aspect of the medial thigh (Fig. 2). Within the gluteal region, there was a small hypoechoic focus measuring up to 5 mm with an echogenic wall concerning for a small fluid collection (Fig. 3). No other acute pathology was noted on ultrasound.
Figure 2:
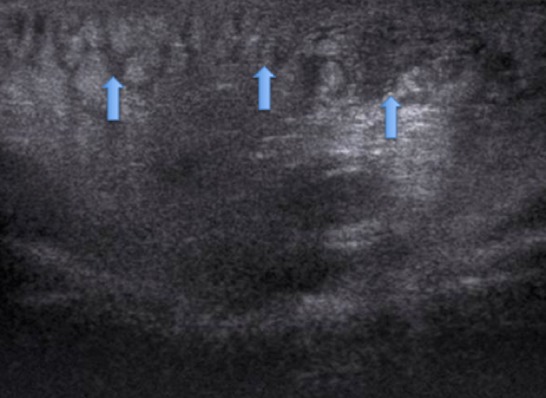
Bedside ultrasound of the medial thigh revealed a cobblestone appearance, as noted by the arrows, indicating extensive soft tissue swelling/edema.
Figure 3:

Bedside ultrasound within the gluteal region revealed a small hypoechoic focus measuring up to 5 mm with an echogenic wall concerning for a small fluid collection
The patient was taken to the operating room by pediatric general surgery for both an anorectal examination under anesthesia and an incision and drainage of the right perianal abscess. An incision was made on the posterior aspect of the fluid collection with a large amount of purulent drainage obtained. The wound was bluntly probed, and a counter incision was made on the anterior aspect of the collection for which a draining vessel loop was passed. The wound cavity was thoroughly irrigated with saline, with a large amount of infected material being drained. Wound cultures came back positive for MRSA. Blood cultures remained negative. His remaining hospital course was unremarkable. By Day 2, the patient was rapidly improving and his vital signs remained stable. By Day 3, he was back to baseline, tolerating a regular diet, and was discharged home. At his 1-week postoperative follow-up appointment, the patient continues to do well and has returned to his baseline activity and energy.
DISCUSSION
The development of a perianal abscess can often be divided into two categories. The first category includes those children who are healthy, without risk factors, and present with no history or symptoms to suggest an inflammatory bowel disease. Many children who present to the ED have constipation, but this is not considered a risk factor for the development of an abscess; however, it is risk factor for an anal fissure [1]. The second category presents in patients who do have a history of Crohn’s disease. These patients often present to the ED with abdominal pain, diarrhea, weight loss, anorexia and failure to thrive. The complication rate for the development of a fistula after a perianal abscess has been reported in up to 24%, with the majority being in patients with underlying inflammatory bowel disease [3].
A perianal abscess generally appears as a swollen red area near the anus and often noticed at diaper change. It has been shown that infants often do not have any underlying medical illness that predisposes them to this development. A retrospective study was performed by the Department of Pediatric Surgery in the United Kingdom involving 38 children (34 boys and 4 girls, 1 month to 12 years old) that presented with an anorectal abscess and 24 children who presented with a fistula (21 boys and 3 girls). Only four of the patients had an identifiable cause for the development of either an abscess or a fistula, with three of them having a history of Crohn’s disease [4]. Multiple risk factors have been proposed, including hematogenous spread, neoplasms, immunocompromised states, inflammatory bowel disease, granulomatous disease, penetrating trauma to the area, infection of the anal glands and Hirschsprung’s disease [2, 3].
The most common bacterial isolate is Staphylococcus aureus, with one study reporting 35% of perianal abscesses in pediatric patients [3]. Other organisms include Escherichia coli, Proteus,Enterobacter species, Streptococcus and Pseudomonas [3]. The progression of a simple perianal abscess in a healthy patient to a systemic illness requiring IV antibiotics, hospital admission and operative intervention is considered exceptionally rare, as most cases involve treatment with oral antibiotics, drainage in the office, warm compresses, with resulting resolution without operative intervention. Overall, the prognosis is considered excellent in the majority of cases, with the exception of perineal pathology in patients with Crohn’s disease, which is complex [1].
Our patient presented with a febrile seizure and perineal swelling and was found to be septic secondary to a perianal abscess. Febrile seizures are a common condition observed in the pediatric population, with an incidence of 1 in every 25 children presenting with at least one febrile seizure [5]. A large retrospective study and meta-analysis involving 4599 children with at least one febrile seizure was performed. Causes of a febrile seizure included: upper respiratory infection (42%), gastroenteritis (21%), otitis media (15%), pneumonia (9%), urinary tract infection (3%), and other infections (12%), with overlap with multiple infections in a few cases. Febrile seizures are seen in children ages 6 months to 5 years of age, peaking by age 2 years. Seizures are simple if there is only one seizure within 24 h, <15 min in length, generalized, with no prior history of seizures without a fever. Seizures are complex if >15 min in length and unilateral/focal and occur >1 time within 24 h [6]. To our knowledge, this is the first case reported in the literature of a febrile seizure secondary to a perianal abscess.
Conflict of Interest Statement
None declared.
FUNDING
No financial support was received for this study.
ETHICAL APPROVAL
No approval is required.
CONSENT
Informed consent was obtained.
GUARANTOR
G.T. is the guarantor of this study.
REFERENCES
- 1. Rosen N. Anorectal Abscess in Children Medscape. https://emedicine.medscape.com/article/935226-overview?pa=8hIkNVbMw%2BHe4k9s5dcd5AxuDUj7MOn2Zp26CdqEO81s9rpc4LyLXAVAgj%2FmQ1Y9LCEJNCrbkqLWYvqLrhntWA%3D%3D(18 August 2017, date last accessed).
- 2. Abercrombie J, George B. Perianal abscess in children. Ann R Coll Surg Engl 1992;74:385–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2497699/?page=2. [PMC free article] [PubMed] [Google Scholar]
- 3. Enberg R, Cox R, Burry V. Perirectal abscess in children. JAMA Pediatrics 1974;128:360–1. https://jamanetwork.com/journals/jamapediatrics/fullarticle/505698. [DOI] [PubMed] [Google Scholar]
- 4. Nix P, Stringer M. Perianal sepsis in children. Br J Surg 1997;84:819–21. https://onlinelibrary.wiley.com/doi/pdf/10.1046/j.1365-2168.1997.02699.x. [PubMed] [Google Scholar]
- 5. Delpisheh A, Veisani Y, Sayehmiri K, Fayyazi A. Febrile seizures: etiology, prevalence, and geographical variation. Iran J Child Neurol 2014;8:30–7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4135278/. [PMC free article] [PubMed] [Google Scholar]
- 6. National Institute of Neurological Disorders and Stroke What Are Febrile Seizures NINDS. September 2015. NIH Publication No. 15-3930. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Febrile-Seizures-Fact-Sheet


