INTRODUCTION
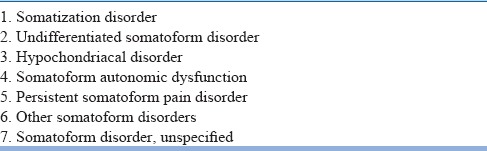
Somatoform disorders are characterized by the repeated subjective experience of physical symptoms (hereafter somatoform symptoms) which are not explained by any physical disease. The types of somatoform disorders in International Classification of Diseases-10 (ICD-10) are listed in Table 1. All the disorder subtypes share one common feature, that is, predominance and persistence of somatic symptoms associated with significant distress and impairment. There are repeated requests by the child or adolescent (hereafter child unless specified) or family for medical investigations inspite of consistent negative findings and reassurances from medical professionals. Even if a physical disorder is present, it does not explain the nature and extent of the somatoform symptoms. These affected children often have a degree of attention-seeking behavior. They are usually diagnosed by excluding organic causes for the somatoform symptoms. Despite the absence of any physiological abnormality, these children show considerable distress and impairment.
Table 1.
International Classification of Diseases-10 categories of somatoform disorders
These guidelines are an update of the previous IPS guidelines on the management of pediatric somatoform disorders (2008). These guidelines are broad and are expected to help in the systematic assessment and management of a child with somatoform disorders.
ASSESSMENT
Difficulties in assessment [Table 2]
Table 2.
Difficulties in assessment
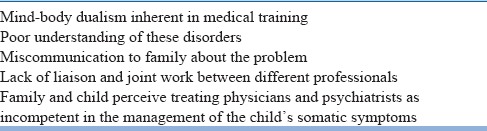
The assessment of these disorders is not straightforward, partly because of the nature of these disorders and partly because of the nature of medical training of physicians [Table 2]. Mind–body dualism has traditionally existed in the way doctors understand medical problems. Therefore, when presented with disorders that are not properly understood because they do not conform to this dualism, physicians feel that it must be something to do with the mind (functional/psychogenic) and hence refer the patient to a psychiatrist. The message often perceived by the family is that their child is making up the symptoms. Poor liaison between the treating physician and the psychiatrist results in the family seeking multiple medical opinions. Even when the family sees a psychiatrist, they do not feel confident enough as the treating physician is not seen as competent in assessing the physical symptoms.
Initial assessment [Table 3]
Table 3.
Assessment
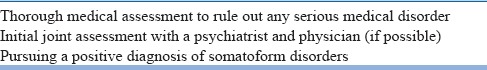
Once somatoform disorders are suspected, the assessment requires a comprehensive, multidisciplinary approach with close monitoring of symptom evolution [Table 3]. The assessment should include thorough history taking, physical examination, and diagnostic tests to rule out both serious and benign medical factors that may be contributing to the child's symptoms. Relevant investigations should be done wherever indicated. The possibility of a somatoform disorder superimposed on neurological or medical disorders, or other psychiatric disorders should always be considered.
Somatoform disorders should not be primarily diagnosed by the exclusion of an organic cause. It is much more effective to pursue a positive diagnosis of somatoform disorder when the child presents with typical features of somatoform disorders. Multiple symptoms, often occurring in different organ systems, symptoms that are vague or that exceed in number or intensity or do not conform to the objective findings are suggestive of somatoform disorders. A chronic course, prior history of unexplained physical symptoms, the presence of a psychiatric disorder, history of extensive diagnostic testing, rejection of previous physicians, and responsiveness of the symptoms to placebo or suggestion are some important pointers to the diagnosis of somatoform disorders. The treating psychiatrist should always consider seeking appropriate consultations if there are new symptoms or there is a possibility of a somatoform disorder superimposed on neurological or medical disorders. There must be an ongoing liaison between the treating psychiatrist and the pediatrician and any new symptom should be assessed by the pediatrician.
Psychosocial assessment [Table 4]
Table 4.
Psychosocial assessment
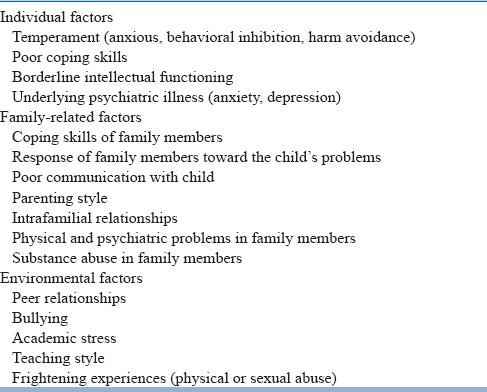
Psychiatric assessment should take a systemic perspective looking into all relevant biopsychosocial factors [Table 4]. These can be divided into individual factors, family-related factors, and other environmental factors.
Individual factors
Assessment of the child's temperament (anxious, behavioral inhibition, and harm avoidance) helps to understand how he/she copes with stress. The child's coping skills are often modeled on the family's coping skills, which also need to be understood. Assessment of intelligence to rule out borderline or low intellectual functioning can help to understand the child's coping skills in the face of stress. Low intelligence is also a risk factor for a number of psychiatric disorders. A detailed psychiatric assessment is needed to assess psychiatric conditions, such as depression and anxiety disorders, which may present with nonspecific physical symptoms to pediatricians or physicians. Separation fears in the child can be associated with the somatic symptoms and therefore should be properly assessed. The presence of a psychiatric condition gives a valuable clue that the child may be suffering from a somatoform disorder.
Family-related factors
Obtaining examples of how the family members deal with stressful situations can be very helpful. Sometimes, maladaptive ways of dealing with stressors are evident in family members, which serves as a model for the child. Exploring the family's understanding of and response to the child's symptoms is crucial to understanding the perpetuating and maintaining factors. Both lack of communication and overinvolvement with the child can maintain the symptoms of a somatoform disorder. Any secondary gain because of somatic symptoms should be carefully elicited. The style of parenting, intrafamily relationships, and family functioning need to be assessed comprehensively, focusing not only on the difficulties but also on the strengths. These strengths can be used later in therapy. It is particularly relevant to comprehensively assess for the recent or ongoing stressors which interact with the individual factors (as discussed above) to shape the course of child's problems. Studies in children have shown that stressors are generally present in their day-to-day life and are known to the child and their family members. It is important for the clinician to evaluate for stressors from a developmental perspective and to try and assess for any temporal relationship between the stressor and onset of symptoms. It may not be possible to find out stressor in the initial interviews; however, by repeated, careful, and sensitive interviewing, stressors can be elicited. Mental illness, substance abuse, physical illness, conflictual relationships in parents, and other key family members can present as both acute and ongoing stressors and therefore need to be properly assessed. History of chronic physical illness, somatoform symptoms, and disability in close family members, together with their coping mechanisms, serve as a model for the child to emulate. They can contribute to the child's problems in multiple ways.
Environmental factors
Environmental factors can also present as both acute and ongoing stressors in the life of the child and need to be assessed comprehensively. Stressors in school can arise from poor peer relationships, bullying, academic stress, and teaching style (harsh or critical). Acute and ongoing frightening experiences that include physical and sexual abuse also need to be assessed. Information should be obtained both from the family and school to understand the nature and extent of stressors. At times, stressors may not be obvious or severe enough to be noticed by the family members. In such cases, stressors should be assessed systematically, and their severity and temporal correlation with the onset of somatoform symptoms should be clearly delineated. One may use the WHO interview schedule for the assessment of psychosocial situations (ICD-10 Axis V) for the systematic assessment of stressors in children.
TREATMENT
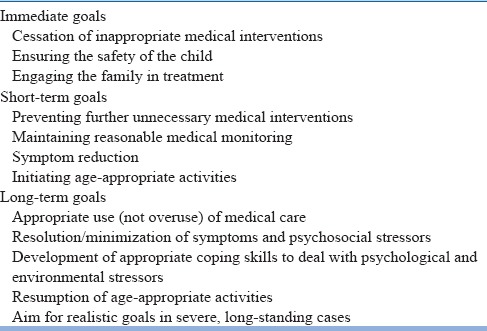
It is imperative to treat these disorders promptly to prevent habituation and future disability. The longer the symptoms remain, the more aggressive the treatment should be. It may be helpful to consider treatment in stages with having immediate, short- and long-term goals [Table 5]. Immediate goals can be cessation of inappropriate medical interventions, ensuring the safety of the child, engaging the family in treatment, and arranging ongoing care. Short-term goals can be preventing further unnecessary medical interventions, maintaining reasonable medical monitoring, symptom reduction, and steps to initiate age-appropriate activities. Long-term goals can be appropriate use (not overuse) of medical care, resolution/minimization of symptoms and psychosocial stressors, development of appropriate coping skills to deal with psychological and environmental stressors, and resumption of age-appropriate activities. In severe cases, symptoms are unlikely to resolve completely and even if they do, they are likely to keep relapsing. Therefore, the goals may have to be revised regularly and kept realistic. Unrealistic goals often lead to symptom substitution by the child to stay in the sick role. A better goal is to help the child and family in coping with the symptoms, keeping the child engaged in school, extracurricular activities, and away from hospital admission.
Table 5.
Treatment goals
Rapport and therapeutic alliance
Once a diagnosis of one of the somatoform disorders is made, the most difficult process is engaging the child and family in the treatment plan. The cornerstones of successful therapy include establishment of rapport and therapeutic alliance with them. Resistance to seeing a psychiatrist because of various misconceptions and stigma is prevalent. The initial sessions, even while the assessment is ongoing, should aim to come to a shared formulation of symptoms that the child and family agree with. We recommend using a cognitive behavioral therapy (CBT) framework [Figure 1]. Family influences are particularly relevant, especially in young children, and these need to be built into the formulation.
Figure 1.
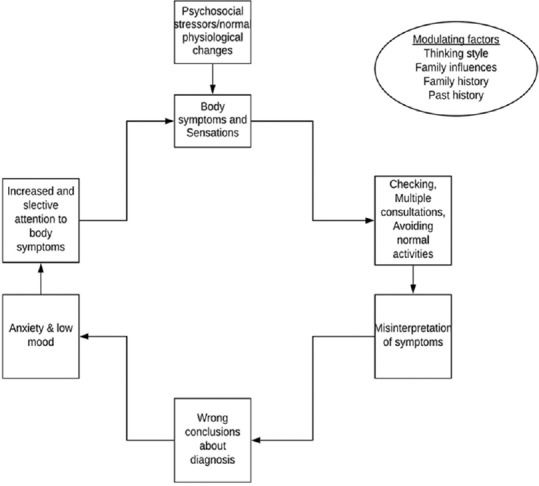
Cognitive behavioral therapy framework for formulating somatic problems
Psychoeducation [Table 6]
Table 6.
Psychoeducation - key points
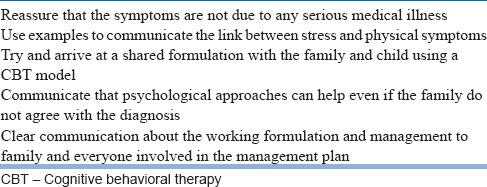
The family and the child should be educated that physical symptoms in the absence of known physical disorder are common and representative of how the body responds to stress [Table 6]. Communicating that there is nothing seriously wrong with the child from a medical point of view is not always straightforward. The family and the child may disagree with the view that there could be anything psychologically wrong with their child, their parenting styles, or the family functioning. Any suggestion of this possibility can be met with resentment, anger, and sometimes, open hostility. It is, therefore, important to not get into an argument with the family over this. Common examples of physical symptoms in stressful situations, for example, becoming sweaty, experiencing palpitations, and feeling “butterflies in the stomach” can be quite helpful in driving home the point that physical symptoms can be present in the absence of physical disease. The best approach is to get these examples from the history narrated by the family. However, when the diagnosis is presumptive, it is best to acknowledge that rather than pretending to be certain. A better stand would be that although there is no evidence of a serious life-threatening medical illness, the child does have an impairing illness that is not properly understood. If a confident diagnosis of somatoform disorder has been made, then unnecessary medical workup should be avoided unless there are new symptoms that are not consistent with the diagnosis. However, if the diagnosis is presumptive, then the family should be reassured that the pediatrician will continue to monitor symptoms from a medical point of view. At the same time, it should be communicated that practical psychological approach can alleviate the symptoms even if the family thinks that these are due to a medical cause (that a physician has not found). An alternative formulation of symptoms is presented using the CBT framework. The child and family is educated about that while the child's symptoms may be physiological, it is their interpretation and the subsequent behaviour of the child that exacerbates them. The CBT formulation should be collaborative and prepared involving the child and family. A shared formulation helps to shift the beliefs away from a purely medical model of the child's problems. Subsequent treatment approach using the CBT model should be explained early on, and its collaborative nature needs to be stressed upon properly. It is important to arrive at shared treatment goals that are explicitly communicated between the treating clinician, the child, and family so that the members of the treating team should adopt the same approach toward the disorder and the child and family.
Solving the psychosocial problems
It is important to understand the psychosocial problems that may be contributing to the child's condition. Once these are known, then attempts should be made to resolve or minimize them. The problem should be discussed with the child and the family. In case of adolescents, if the problem has been revealed to doctor or the ward staff in confidence, then consent of the adolescent should be taken to discuss it with the family. The physician should not force his/her opinion on the child or the family. Problems of family relationships should be discussed and family should be told that the child is being adversely affected by the family problems and their resolution will improve the child. It is important to open up the channels of communication between the child and his/her family. Throughout the treatment, attention should be focused on the child rather than on the symptoms to ensure a speedy recovery.
Psychological treatment [Table 7]
Table 7.
Nonpharmacological management - key points
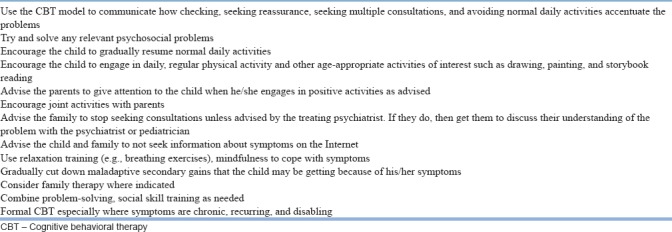
CBT-based approaches have been shown to be helpful in reducing the intensity of symptoms and help the child in coping with them and improve his/her general functioning [Table 7]. CBT formulation is useful in understanding the symptoms regardless of whether formal CBT is used in the treatment or not. In mild cases, the formulation itself may be therapeutic. However, where symptoms are chronic, recurring, and disabling, formal CBT is recommended. The following are the key points:
8–16 weekly sessions following the general CBT framework
A shared formulation to understand the child's problems
Using active CBT techniques, the dysfunctional beliefs are gently challenged and replaced by the adaptive ones
Gradually replace illness behavior with more healthy behaviors
Negotiate a phased return to school and other extracurricular activities that the child was pursuing before. Incorporating some physical activity can be especially useful. It helps the child to improve fitness, build self-esteem, and replace the time spent on illness behaviors. It can also serve as a behavior experiment that proves that the child is not too physically unwell
Combine relaxation training, yoga, problem-solving, social skill training, and mindfulness to the child.
Family therapy can be useful if there is evidence that dysfunctional family dynamics are contributing to the child's difficulties. It can also be helpful if there are strengths in the family setup that can be used therapeutically.
Secondary gains
Reduction in secondary gains is not advisable very early in the treatment and without adequate explanations to the family because of three reasons.First, the physician himself/herself may not be certain about the origin of the symptoms. Second, the family may perceive reduction in secondary gain as neglect of the child. Third, initially, the family may not have full confidence in the hospital's ability to take total care of their child.
Later on, the family should be offered adequate explanations regarding the secondary gains. Reduction in secondary gains in a child should be accompanied by providing the child with an alternative, healthy, socially acceptable, and age-appropriate role in which he or she can be rewarded for doing something positive.
Pharmacological treatment
There is no good-quality evidence to recommend any particular medication for somatoform disorders in the pediatric population. A recent Cochrane review (Kleinstäuber et al.) concluded that there is low or very low-quality evidence for the efficacy of pharmacological interventions for somatoform disorders in adults which makes it difficult to extrapolate those findings to the pediatric population. Medications including SSRIs and SNRIs have been used and reported to be helpful in somatoform disorders, especially when symptoms are particularly severe, resistant to psychological approaches, and when other psychiatric comorbidity is present. Anxiety and depressive disorders may be associated with somatoform disorders, and these respond well to antidepressants. However, it is advised that only those antidepressants which are approved in pediatric age group for other indications should be used if required. The clinician should pay particular importance to the side effects while choosing medication, as this patient group is more sensitive to them. One should start with low doses and increase them progressively to avoid side effects that may mimic the symptoms present before the treatment.
Dealing with negative emotions
These patients and the families often arouse negative responses in medical professionals and hospital staff. The staff can feel frustrated and angry. There can be beliefs that these patients and families are abusing healthcare resources, wasting the professionals’ time, and that no intervention will help. The psychiatrist needs to both deal with these negative emotions himself/herself and help other treating team members including the pediatrician, in coping with them. Flow Diagram 1 summarizes the management of somatoform disorder in children.
Flow Diagram 1.
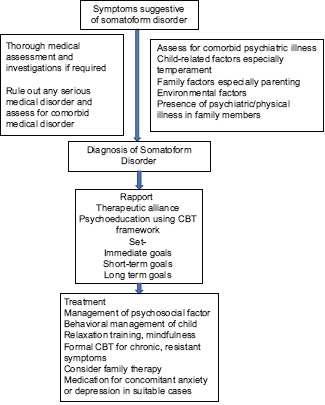
Management scheme for pediatric somatoform disorders
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
FURTHER READING
- 1.Campo JV. Annual research review: Functional somatic symptoms and associated anxiety and depression – Developmental psychopathology in pediatric practice. J Child Psychol Psychiatry. 2012;53:575–92. doi: 10.1111/j.1469-7610.2012.02535.x. [DOI] [PubMed] [Google Scholar]
- 2.Karkhanis DG, Winsler A. Somatization in children and adolescents: Practical implications. J Indian Assoc Child Adolesc Ment Health. 2016;12:79–115. [Google Scholar]
- 3.Escobar JI, Dimsdale JE. Somatic symptom and related disorders. In: Saddock BJ, Saddock VA, Ruiz P, editors. The Comprehensive Textbook of Psychiatry. 10th ed. Philadelphia: Wolters Kluwer; 2017. [Google Scholar]
- 4.Garralda ME, Rask CU. Somatoform and related disorders. In: Thapar A, Pine DS, Leckman JF, Scott S, Snowling MJ, Taylor E, editors. Rutter's Child and Adolescent Psychiatry. 6th ed. West Sussex: Wiley-Blackwell; 2015. [Google Scholar]
- 5.Kleinstäuber M, Witthöft M, Steffanowski A, van Marwijk H, Hiller W, Lambert MJ, et al. Pharmacological interventions for somatoform disorders in adults. Cochrane Database Syst Rev. 2014;11:CD010628. doi: 10.1002/14651858.CD010628.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes: A critical review of controlled clinical trials. Psychother Psychosom. 2000;69:205–15. doi: 10.1159/000012395. [DOI] [PubMed] [Google Scholar]
- 7.Malas N, Ortiz-Aguayo R, Giles L, Ibeziako P. Pediatric somatic symptom disorders. Curr Psychiatry Rep. 2017;19:11. doi: 10.1007/s11920-017-0760-3. [DOI] [PubMed] [Google Scholar]
- 8.Schaefert R, Hausteiner-Wiehle C, Häuser W, Ronel J, Herrmann M, Henningsen P, et al. Non-specific, functional, and somatoform bodily complaints. Dtsch Arztebl Int. 2012;109:803–13. doi: 10.3238/arztebl.2012.0803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sitholey P, Agarwal V. 2008. Child and Adolescent Psychiatry: Clinical Practice Guidelines for Psychiatrists in India; pp. 154–8. [Google Scholar]


