Abstract
Background:
Dual mobility designs were introduced to increase stability and reduce the risk of dislocation, both being common reasons for surgical revision after total hip arthroplasty. The in vivo behavior of dual mobility constructs remains unclear, and to our knowledge, no data have been published describing in vivo surface damage to the polyethylene bearing surfaces.
Methods:
We used surface damage assessed on the inner and outer polyethylene bearing surfaces in 33 short-term retrieved dual mobility liners as evidence of relative motion at the 2 bearings. A lever out test was performed to determine the force required for dislocation of the cobalt-chromium femoral head from the polyethylene liner.
Results:
Both bearings showed damage; however, the inner polyethylene bearings had higher damage scores, lower prevalence of remaining machining marks, and higher incidence of concentric wear, all consistent with more motion at the inner polyethylene bearing. The inner polyethylene bearings also had a higher occurrence of embedded titanium debris. The damage sustained in vivo was insufficient to lead to intraprosthetic dislocation in any of the retrieved components. Lever out tests of 12 retrievals had a mean dislocation load of 261 ± 52 N, which was unrelated to the length of implantation.
Conclusion:
Our short-term retrieval data of 33 highly cross-linked polyethylene dual mobility components suggest that although motion occurs at both bearing articulations, the motion of the femoral head against the inner polyethylene bearing dominates. Although damage was not severe enough to lead to intraprosthetic dislocation, failure may occur long term and should be assessed in future studies.
Keywords: total hip arthroplasty, retrieval analysis, bearing surfaces, polyethylene wear, dual mobility
Hip instability remains the most common reason for surgical revision (22.5%) after total hip arthroplasty (THA) in the United States [1]. Dislocation rates after subsequent revision THA range from 2% to 15% [2–4]. Factors including surgical technique, patient history of hip fracture, osteonecrosis, dysplasia, revision surgery, or neuromuscular disease predispose patients to dislocation [1–4]. Constrained liners and large diameter femoral heads have been used in an attempt to stabilize THAs [3]. More recently, dual mobility THA designs were introduced to increase stability and reduce the risk of dislocation by combining the reduced wear of a small femoral head and the benefit of stability from a large diameter femoral head. The dual mobility concept was first developed by Bousquet in the 1970s as an alternative to constrained liners [1–3,5]. The contemporary generation of dual mobility designs is intended to provide increased range of motion, increased stability, and reduced risk of dislocation [6,7].
Dual mobility systems consist of 3 components that form 2 unconstrained articulations [8]: an acetabular component with a highly polished metal inner bearing that articulates with a large polyethylene bipolar head that snap fits around a standard 28-mm head [6,9]. The reduced risk of dislocation is based on 2 hypotheses. The first is that the introduction of the mobile polyethylene insert diminishes the occurrence of prosthetic neck impingement. The second is that the large diameter articulation between the polyethylene component and the metallic acetabular component increases the range of motion before dislocation [10]. Theoretically, these designs provide a greater jump distance (ie, the amount of lateral translation of the femoral head required for dislocation) than is possible with a standard femoral head design [9].
Survival rates of primary THA dual mobility systems range from 95% at 5-year follow-up to 80% at 15-year follow-up [1,2]. In revision procedures for instability, dual mobility constructs have survival rates as high as 95% at 10 years, with low incidence of recurrent dislocation [1–3]. Data collected from the Swedish Hip Arthroplasty Registry show promising short-term results for preventing dislocation with dual mobility systems. In a study of 228 dual mobility THA patients from the Registry, 99% were revision free for failure because of dislocation at 2-year follow-up [7]. Despite this success, 2 dislocation modes are associated with dual mobility systems: large head dislocation and intraprosthetic dislocation (IPD), at the smaller articulation [11,12]. Rates of large head dislocation and IPD range from 0.6% to 1.5% and 0.2% to 0.28%, respectively [10,13].
Additional concerns include subsequent osteolysis, acetabular component loosening, fibrosis, and IPD due to excessive polyethylene wear and loss of retaining power [1,8,10]. The current dual mobility literature shows rates of osteolysis ranging from 7% to 38% and rates of cup loosening from 0% to 12% [10]. Recent hip simulator studies demonstrated that dual mobility THA designs have similar wear rates to designs with traditional single articulation bearings; however, the in vivo behavior of dual mobility constructs remains unclear, and to our knowledge, no data have been published describing in vivo surface damage to the polyethylene bearing surfaces [8]. Such information could help describe the mechanical performance of the dual mobility construct.
At our institution, dual mobility bearings were often coupled with a modular stem that went on to cause adverse local tissue reactions that required revision surgery [14]. Therefore, we retrieved short-term dual mobility bearings and evaluated the polyethylene bearing surfaces to gain a better understanding of the construct’s behavior in vivo. In this study, we sought to answer the following questions: (1) Is there motion at both articulations in vivo, and if so, does one experience more motion than the other? (2) Is there a difference in the modes or severity of damage between the inner and outer articulation? (3) Are the deformation and damage experienced in vivo sufficient to lead to IPD?
Materials and Methods
All 33 dual mobility highly cross-linked polyethylene liners revised at our institution between 2011 and 2013 were collected through our ongoing institutional review boardeapproved implant retrieval program. Patient demographic data were collected from medical records. Twenty-eight of the dual mobility liners were implanted by 5 different surgeons at our institution, and the remaining 5 liners were implanted at outside hospitals. From the limited data we collected regarding the components’ implantation, it appears that 24 liners were implanted for degenerative joint disease, 3 during conversions from hemiarthroplasties, 1 to address recurrent dislocation, and the remaining 5 unknown. Other data collected from the records included age at index procedure, body mass index (BMI), length of implantation (LOI), and revision diagnosis (Tables 1 and 2). Average patient age at index procedure was 67.8 ± 9 years, average patient BMI was 26.9 ± 7 kg/m2, and average LOI was 15.7 ± 19 months. Reason for revision was adverse local tissue reaction in 48% of cases, dislocation in 12% of cases, periprosthetic fracture in 9%, allergy in 6%, instability in 3%, with the remainder of cases unknown. Twenty-nine components were the Mobile Bearing Hip System ADM design (Anatomic Dual Mobility; Stryker, Mahwah, NJ), and four were the Mobile Bearing Hip System MDM design (Modular Dual Mobility; Stryker). The ADM construct has a cobalt-chrome alloy acetabular shell that is coated with titanium and hydroxyapatite sprays. The rim of the shell includes curved cutouts to comply with the anatomic orientation of the anterior psoas tendon and inferior obturator foramen. A 28-mm cobalt-chrome or ceramic femoral head is snap fit into the highly cross-linked polyethylene liner (X3; Stryker) that articulates with the highly polished bearing surface of the metallic shell. The MDM construct is compatible with several conventional cementless acetabular components including an acetabular shell with titanium and hydroxyapatite spray coating and multiple holes for screw fixation. Shells range in size from 42 to 64 mm. A modular polished cobalt-chrome articular surface component fits into the acetabular shell via a direct taper connection and articulates with the large highly cross-linked polyethylene liner (X3). Similarly to the ADM system, a 28-mm cobalt-chrome or ceramic head (or a 22.225-mm cobalt-chrome head in the smaller sizes) snap fits within the polyethylene liner. In both the ADM and MDM systems, the mouth of the polyethylene inner bearing is slightly smaller in diameter than the femoral head itself. This serves to retain the head. We refer to this as the locking mechanism (Fig. 1).
Table 1.
Patient Demographics.
| Demographics | Mean (Range) |
|---|---|
| Age (y) | 67.8 (52–86) |
| Gender (% females) | 64% |
| BMI (kg/m2) | 26.9 (18–54) |
| Length of implantation (mo) | 15.7 (0–96) |
BMI, body mass index.
Table 2.
Indications for Revision Surgery of the 33 Total Hip Arthroplasties.
| Indications | Cases | Frequency (%) |
|---|---|---|
| Adverse local tissue reaction | 16 | 49 |
| Dislocation | 4 | 12 |
| Unknown/miscellaneous | 7 | 21 |
| Periprosthetic fracture | 3 | 9 |
| Allergy | 2 | 6 |
| Instability | 1 | 3 |
| Total | 33 | 100 |
Fig. 1.
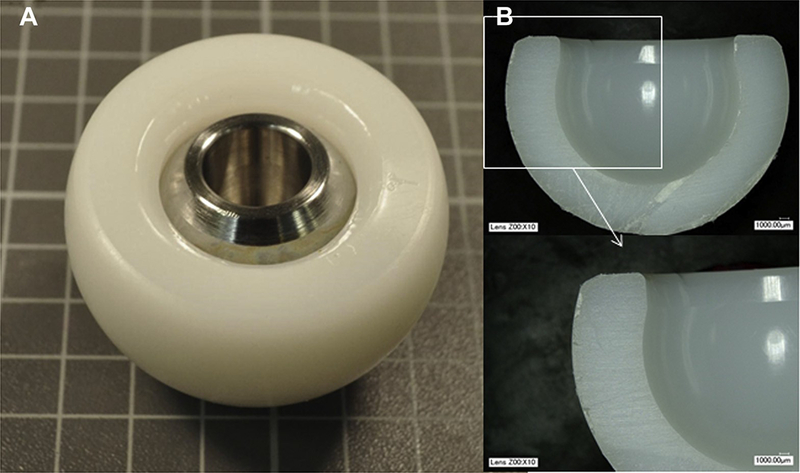
(A) A cobalt-chrome alloy or ceramic femoral head is snap fit into a highly cross-linked polyethylene liner, which is retained by (B) the mouth of the liner that is slightly smaller in diameter than the femoral head.
In our series of 33 retrievals, 23 (70%) had been paired with a modern modular neck stem design that was recently withdrawn from the market, the Rejuvenate Modular (Stryker). Of the remaining retrievals, 3 (9%) were paired with Secur-Fit stems (Stryker), 2 (6%) with Accolade stems (Stryker), 2 (6%) with Restoration Modular stems (Stryker), 1 (3%) with an MP Reconstruction Prosthesis stem (LinkBio Corp, Rockaway, NJ), 1 (3%) with an OmniFit stem (Stryker), and 1 (3%) with a Novation stem (Exactech, Gainesville, FL). Implant characteristics were determined by manufacturing markings on the components and confirmed with the manufacturers.
Lever Outer Assessment
A lever out test was performed to determine the force required for dislocation of the cobalt-chromium femoral head from the polyethylene liner. Twelve retrieved liners of outer diameters 40 (4 liners), 42 (1 liner), 44 (4 liners), 46 (1 liner), and 48 mm (2 liners) with intact femoral heads were evaluated. The assembled specimens were uniaxially loaded 100 mm from the femoral head at a rate of 20 N/s until failure (Fig. 2).
Fig. 2.
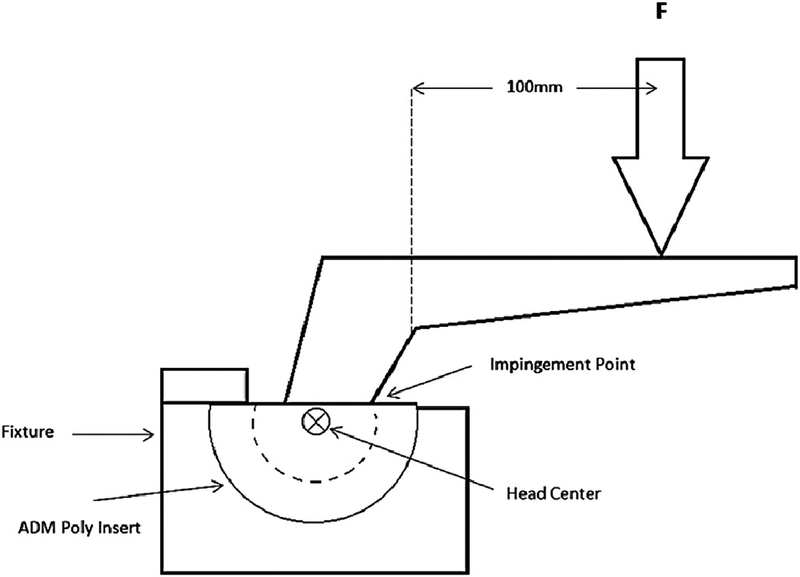
The setup for the lever out testing used a cantilevered force (F) applied near the end of the femoral stem causing impingement between the neck of the femoral component and the rim of the acetabular component, leading to a levering out of the head from the acetabulum. ADM, anatomic dual mobility.
Visual Assessment of Damage
Surface damage on the inner and outer polyethylene bearings was visually assessed independently by 2 observers using a light stereomicroscope (×10 to ×32 magnification). Surface damage on the inner polyethylene bearing of the 33 cross-linked polyethylene acetabular liners was visually assessed under optical microscopy after removal of the femoral head by sectioning of the liner above the locking mechanism using an IsoMet Saw (Buehler, Ontario, Canada) or after lever out testing. The inner polyethylene bearing of the liner was divided into 4 quadrants (Fig. 3A). Owing to mobility of the polyethylene, orientation of each liner was standardized using the manufacturing markings on the rim. Each zone was scored based on the extent and severity of damage, on a scale of 0–3 (none to severe), for 7 modes of damage (scratching, pitting, burnishing, abrasion, embedded debris, delamination, deformation) according to a previously established method [15]. The maximum score for each inner polyethylene bearing was 84 (4 quadrants ×7 modes ×maximum score of 3).
Fig. 3.
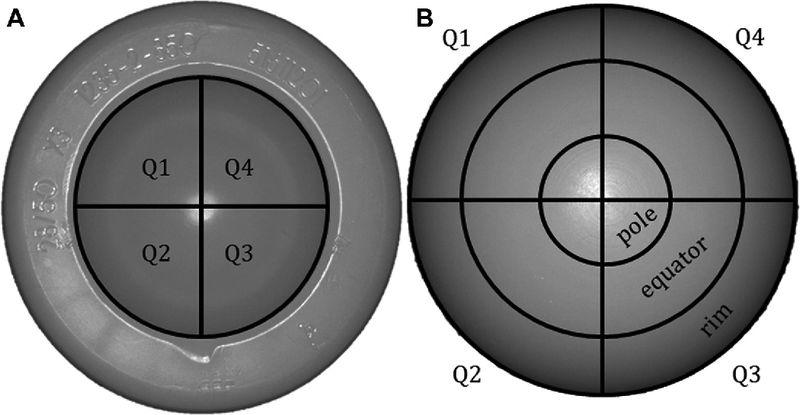
Outer bearing (A) and inner bearing (B) zones were visually assessed for damage.
Surface damage on the outer bearing of the 33 cross-linked polyethylene acetabular liners was visually assessed. The outer polyethylene bearing of the liner was divided into 12 zones: 4 quadrants each for the pole, equator, and rim (Fig. 3B). Each zone was scored according to the same method described previously. The maximum damage score each for the pole, equator, and rim was 84 (4 quadrants ×7 modes× maximum score of 3), and the maximum score for the entire outer polyethylene bearing was therefore 252 (12 zones×7 modes× maximum score of 3). Discrepant scores that varied by >3 (out of a possible score of 12 for each mode of the inner polyethylene bearing and out of a possible score of 36 for each mode of the outer polyethylene bearing) were resolved by the observers. This occurred in 7 out of 33 inner polyethylene bearings and 5 out of 33 outer polyethylene bearings. Secondary electron imaging, back-scattered electron imaging, and embedded debris composition identification using energy- dispersive x-ray were performed for a randomly selected group of 7 liners (the outer polyethylene bearing for 3 liners and the inner polyethylene bearings for 4 liners) using a Zeiss Supra 55VP scanning electron microscopy (Carl Zeiss Microscopy GmbH, Jena, Germany).
Deviation Assessments of the Polyethylene Bearing Surfaces
Coordinate measuring machine (CMM) measurements were taken to assess the deviation of 16 inner and 25 outer polyethylene bearing surfaces of sectioned liners. Inclusion was based on the availability of size-matched pristine CMM scans provided by the manufacturer (WENZEL LH87 Standard; WENZEL, Wixom, MI; resolution: 0.1 mm). CMM measurements were also taken to assess the deviation of the locking mechanism within the inner polyethylene bearing for the 12 lever out specimens. These measurements did not include the remainder of the inner bearing surface. The term “deviation” describes the geometric differences between the surface of a retrieved liner and that of a pristine liner of the same size that had never been implanted. The amount of the differences due to wear (loss of material from the bearing surface) and to deformation (due to yielding or creep of the polyethylene) cannot be determined from the deviation measurements [16]. Eight helical CMM scans spaced 45o apart were taken with each helix centered 30o off of the pole for each surface analyzed. Point spacing was set to 0.5 mm (Fig. 4).
Fig. 4.
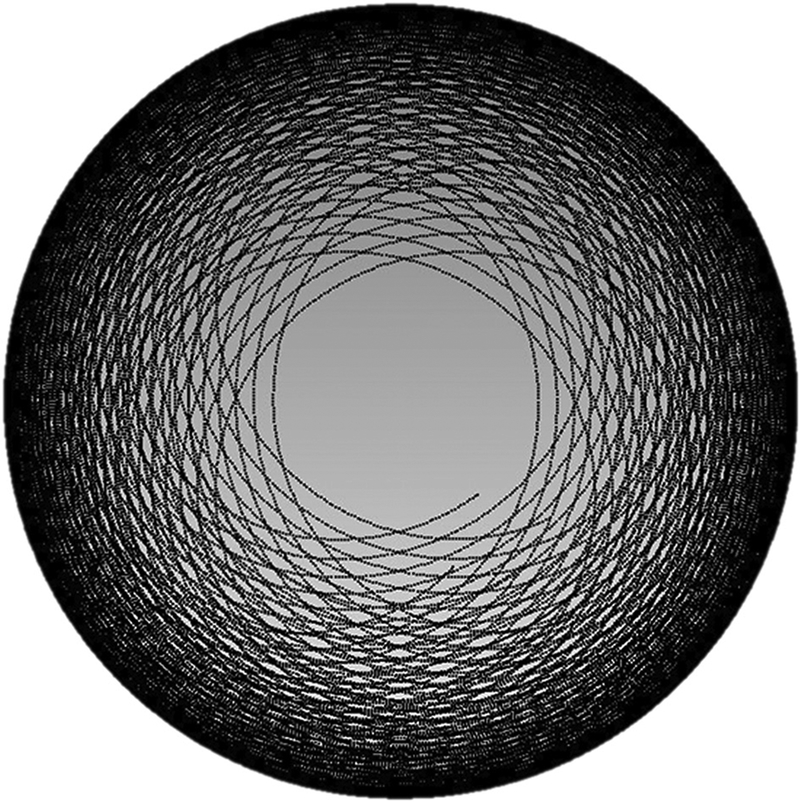
Eight helical CMM scans were taken of 16 inner and 25 outer polyethylene bearing surfaces. The raw scans ranged in size from 60,000 to 105,000 points per surface. CMM, coordinate measuring machine.
The 3D models from the scans of the retrieved liners were compared to pristine models, made from CMM scans of pristine, never-implanted liners provided by the manufacturer using Geomagic Qualify software (version 12; Durham, NC). The 8 helical scans of each surface are merged into a spherical computer-aided design model (with holes at the deepest region of the inner polyethylene bearing and the pole of the outer polyethylene bearing where the probe stylus could not reach). The bearing surfaces of the retrieved implants were aligned to the pristine bearing surfaces using a best fit method with corrective minimization of the differences of the sums of squares [16]. The deviation maps were generated in Geomagic, and damage patterns were then categorized into 1 of 4 groups: no wear, concentric wear, edge loading, or concentric wear and edge loading. Deviations within ±20 mm were considered within manufacturing tolerances and disregarded based on a deviation analysis between CMM scans of 2 pristine, never-implanted components of the same size. Average deviation (mm) was determined by averaging the measured differences in position of matched points between the retrieved and pristine models.
Statistical Analysis
Polyethylene damage scores between the damage modes were evaluated using a Kruskal-Wallis 1-way analysis for variance on ranks for both the inner and outer polyethylene bearings. Damage scores of inner and outer polyethylene bearings from the same component were compared using a paired t test for parametric data (scratching and total damage scores) and a Mann-Whitney rank sum test for nonparametric data (pitting, burnishing, abrasion, delamination, deformation, and debris). Differences in the lever out loads among the outer diameter sizes were calculated with a 1-way analysis for variance. The levels of statistical significance corresponding to the differences in average deviation and average deviation rate were calculated with Mann-Whitney rank sum tests. Analyses were performed to determine the strength of the correlations between demographic data (age, BMI, LOI, and reason for revision) and the damage scores and average deviation. A separate analysis was run to determine the strength of correlation between LOI and the lever out load. Pearson’s coefficient and Spearman’s rank order coefficients were applied depending on the distribution of the data. In all analyses, P < .05 was deemed significant.
Results
Lever Out
The average LOI of the specimens which underwent lever out test was 5.9 months (range, 0.06–26). The average lever out load for the 12 specimens tested was 261 ± 52 N, and the average lever out moment was 26 ± 5 Nm. No significant difference was found in the lever out load among the outer diameter sizes (P¼ .122). No correlation was found between the lever out load or lever out moment and the LOI of these retrievals (R2 ¼ 0.037).
Visual Assessment
The average damage score for the inner polyethylene bearings was 15.4 ± 5 (maximum score of 84). Damage to the inner polyethylene bearing was dominated by scratching, pitting, and embedded debris with average damage scores of 9.4 ± 3, 4.0 ± 2, and 1.5 ± 2, respectively (Fig. 5B). The average damage score for the outer polyethylene bearings was 48.3 ± 14 (maximum score of 252). Damage to the outer polyethylene bearing was predominately scratching and pitting with average scores of 21.3 ± 7 and 22.2 ± 8, respectively (Fig. 5A). Burnishing, deformation, and embedded debris were minimally present, with average scores of 1.7 ± 4, 2.3 ± 3, and 0.63 ± 1, respectively. The average damage score was highest at the equator (16.7 ± 5.0), followed by the rim (15.9 ± 6.6) and the pole (14.5 ± 5.5). The total damage score at the equator was significantly greater than the total damage at the pole (P .01), but no different than the total damage at the rim (P .31). The total damage at the pole was not different than the total damage of the rim (0.10).
Fig. 5.

(A) Images of retrieved polyethylene outer bearings showed pitting and scratching (left), embedded debris (middle), and machining lines (right). (B) Images of inner bearings showed furrowing (left), scratching (middle), and embedded debris (right).
To compare damage scores between the inner and outer polyethylene bearings, all scores were normalized as percentages of the maximum possible score. The outer polyethylene bearings had significantly higher deformation scores (P¼.039) than the inner polyethylene bearings, whereas the inner polyethylene bearings had significantly higher scratching, pitting, and embedded debris scores (P¼ .012 for scratching; P < .001 for both pitting and embedded debris). No difference in burnishing scores was found between the bearings surfaces (P¼ .26). Abrasion and delamination were not present on either bearing surface. Machining marks were still visible on 29 out of the 33 (87.9%) outer polyethylene bearings but on a significantly lower proportion of 10 out of the 33 (30.3%) inner polyethylene bearings (P < .001).
Scanning electron microscopy imaging showed embedded metallic particles on both outer and inner polyethylene bearing surfaces; particle sizes ranged from 100 to 350 microns (Fig. 6A. The composition of these particles was confirmed as titanium alloy using energy dispersive x-ray analysis (Fig. 6B). Embedded metallic particles were visible on 10 out of 33 (30.3%) outer polyethylene bearings, a significantly smaller proportion than the 21 out of 33 (63.6%) inner polyethylene bearings (P ¼ .007).
Fig. 6.
(A) A particle of embedded debris is shown in this scanning electron photomicrograph of a polyethylene bearing surface. (B) The corresponding spectrum from energy dispersive x-ray analysis of the particle included a titanium peak.
Deviation Measurements
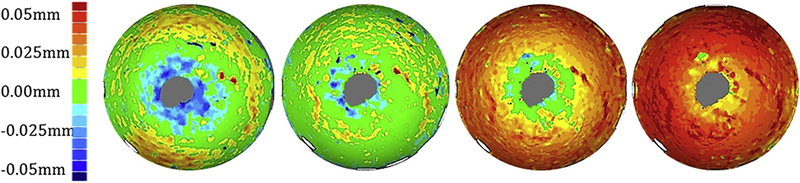
Average deviation was significantly higher for the inner polyethylene bearing surfaces than the outer polyethylene bearings (0.04 ± 0.01 mm vs 0.02 ± 0.03 mm; P < .001). Of the 25 outer polyethylene bearings analyzed, 21 (84%) appeared unworn, 2 (8%) showed evidence of edge loading, 1 (4%) showed evidence of concentric wear, and 1 (4%) showed evidence of both edge loading and concentric wear (Fig. 7). Of the 16 inner polyethylene bearings analyzed, 14 (87.5%) showed evidence of concentric wear, and 2 (12.5%) appeared unworn (Fig. 8).
Fig. 7.

Deviation maps of outer bearing CMM data showed bearings with no wear, edge loading, concentric wear, and edge loading and concentric wear (left to right).
Fig. 8.
Deviation maps of inner bearing CMM data showed 2 bearings with no wear (left 2 images) and 2 with concentric wear (right 2 images).
CMM of all of the inner polyethylene bearings that underwent lever out testing showed evidence of impingement and damage to the locking mechanism (Fig. 9). The locking mechanisms of these inner polyethylene bearings reached an average maximum deviation from their intact state of 0.65 mm (range from 0.091 to 1.001 mm).
Fig. 9.

Three-dimensional analysis of the inner polyethylene bearing of a specimen after lever out testing showed a negative deviation at the point of impingement (arrow) and a ring of positive deviation where the locking mechanism was so severely deviated that the femoral head was able to escape from the liner.
Discussion
Dual mobility constructs were clinically introduced for THAs to increase stability and range of motion while decreasing the risk of dislocation. The incorporation of highly cross-linked polyethylene may allow for excellent wear resistance and may minimize polyethylene wear debris-induced osteolysis. Although ex vivo testing demonstrated reduced wear rates in comparison to standard fixed modular systems using conventional polyethylene, little is known about the in vivo performance of highly crossed-linked dual mobility systems [8]. We used retrieval analysis to compare the accumulation of in vivo damage on the inner and outer polyethylene bearing surfaces of polyethylene dual mobility liners. We combined lever out mechanical testing, damage scoring [15], and CMM deviation analysis [17] to evaluate the surface damage and dimensional changes of these retrievals to gain a better understanding of their performance in vivo.
Our study has limitations. As with any retrieval study, our work is retrospective and includes implants that were revised for various reasons and, therefore, may not reflect well-functioning devices. Furthermore, most of our retrievals were coupled with a modular stem that has been associated with adverse local tissue reactions, requiring revision surgery, but were otherwise well-functioning before revision. As such, these retrievals had short LOIs (15.7 ± 19 months). Future analyses of implants with longer LOIs should be performed to assess whether the results of this study reflect longer implantation times. The objective of this study was to examine the polyethylene bearing surfaces, particularly in regard to motion at these bearings, which should not have been effected by the stem type with which they were coupled. Embedded titanium debris was observed in a large proportion of the polyethylene liners. Two potential sources of this debris exist: the femoral stem and the acetabular shell. A recent study of retrieved Rejuvenate modular neck stems showed that material loss only occurred at the male taper of the cobalt-chromium modular neck. No material loss was observed at the female taper of the Ti-12Mo-6Zr-2Fe (TMZF beta titanium alloy; Stryker) stem [1]. This indicates the embedded debris likely originates elsewhere. We suspect but cannot confirm that these come from the backside of the titanium acetabular shell. Another limitation to our study is inherent within the CMM deviation assessment. Probe scans were set 30o off of the pole, leaving a small gap at the most deep region of the inner polyethylene bearing and at the most superficial region of the outer polyethylene bearing that was not accounted for in our analysis. Additionally, the iterative closest point algorithm used to achieve a best fit minimizes the sum of the squared values of the differences between the retrieval and the pristine surfaces. As a result of this best fit algorithm, alignment between the retrieved and pristine models may have been minimized enough to substantially reduce the deviations measured between the 2 surfaces.
In answer to our first research question, we found polyethylene surface damage consistent with in vivo motion at both the inner and outer articulations in our series of retrieved dual mobility constructs. However, our results suggested that more motion occurred at the inner polyethylene bearing than at the outer polyethylene bearing when considering damage scores, machining marks, and CMM deviation analysis. When damage scores were normalized and compared between the inner and outer articulations, scratching, pitting, and embedded debris were all higher on the inner polyethylene bearings than the outer polyethylene bearings. Although the outer polyethylene bearing out-scored the inner polyethylene bearing for deformation, we attribute this to the ease of visualization when looking at the outer polyethylene bearing under the microscope. The curvature of the inner polyethylene bearing impeded the light source from the microscope and made it difficult to detect small changes in geometry. Machining marks were still visible on most outer polyethylene bearings but on a significantly lower proportion of inner polyethylene bearings, again consistent with more motion at the inner articulation. Finally, the CMM data showed a much higher occurrence of concentric wear on the inner polyethylene bearings than the outer polyethylene bearings. This, in addition to higher damage scores and fewer machining marks, suggests greater motion at the inner polyethylene bearing.
In answer to our second question, differences were found in the modes of damage between the inner and outer articulation. The average damage score of 48 (out of 252) for the outer polyethylene bearing was dominated by scratching and pitting. The average damage score for the inner polyethylene bearing was 15 (out of 84) and, though similarly dominated by scratching and pitting, included embedded debris. The debris seen was identified as a titanium alloy using energy dispersive x-ray analysis, suggesting that the source of the embedded particles was likely the plasma spray coating on the metallic acetabular shell or from wear at the head and/or neck or modular neck junctions. Results in the literature for highly cross-linked fixed bearing acetabular liners match our results for the outer polyethylene bearing. For example, Schroder et al [18] examined 39 cross-linked polyethylene liners retrieved after an average of about 2 years. Polyethylene surface damage on the bearing surface was dominated by scratching, burnishing, and pitting with little evidence of embedded debris.
Damage assessment of retrieved bearing surfaces in dual mobility components by other investigators is limited. Adam et al [18] assessed visual damage on 40 polyethylene inserts from retrieved dual mobility cup components removed at an average of 8 years of implantation. They assessed macroscopic damage and deformation by loss of machining grooves and changes in the shapes of the inner and outer surfaces. Using manufacturers’ tolerance for these implants, linear wear and wear volume were determined by comparing the measured dimensions with the theoretical dimensions of new liners. They found motion in the outer polyethylene bearing surface corroborated by the loss of machining grooves and a mean annual outer polyethylene bearing linear wear of 9 mm; in contrast, the mean annual wear of inner polyethylene bearing was 73 mm. Adams et al concluded that motion was occurring at the outer, convex bearing despite the disparate annual linear wear. Our findings contradict this conclusion and indicate the inner polyethylene bearing as the predominant source of motion. Two possible explanations exist for this difference. The first is that the Adams et al study had dual mobility retrievals with longer implantation times, so perhaps the behavior of these components changes with time. The second is that the indications for revision in the Adams et al study were mainly mechanical failure, suggesting that these components likely functioned suboptimally in vivo.
In answering our third and final research question, the deformation and damage experienced in vivo in the retrieved dual mobility components in our study were insufficient to lead to IPD; none of the components experienced IPD in vivo. IPD is a specific to dual mobility components. In a series of 81 cases of IPD, the average time of occurrence was 9 years postoperatively [4]. Three main failure mechanisms were described in that series: pure IPD without arthrofibrosis and without cup loosening; IPD secondary to failure of the bearings to articulate; and IPD associated with acetabular component loosening [4]. Nonetheless, all 33 components assessed in our series of short-term retrievals did show visual evidence of damage at the inner polyethylene bearing. Our lever out testing of 12 specimens showed a failure load of 261 ± 52 N (an average lever out moment of 26 ± 5 Nm). No other peer-reviewed literature exists to provide an estimate of the force necessary to dislocate the femoral head from the retentive polyethylene component in dual mobility designs.
Our lever out testing provides an explanation of 1 failure mechanism that produces IPD. If the outer articulation is stationary or the motion at this bearing is impeded, the femoral neck can impinge on the liner and lever the femoral head out of the retentive liner as the locking mechanism deforms. As most of the motion occurs at the inner polyethylene bearing, after sufficient time and sufficient polyethylene wear, the potential exists for failure of the locking mechanism and subsequent dislocation of the femoral head. As previously described, this mechanism can be exacerbated by failure of the outer polyethylene bearing to articulate or by loosening of the acetabular component [19]. However, our data show that the locking mechanism remains intact in the short term regardless of liner size, although failure may occur in the long term and should be assessed in future studies.
Our short-term retrieval data of 33 highly cross-linked polyethylene dual mobility components suggest that although motion occurs at both bearing articulations, the motion of the femoral head against the inner polyethylene bearing dominates. This is supported by higher damage scores and average deviations, lack of machining lines, and higher incidence of concentric wear at the polyethylene bearing. The presence of damage and deviation at the outer polyethylene bearing indicates motion at this articulation as well, although minimal in comparison to the inner polyethylene bearing. The propensity of the inner polyethylene bearing to trap embedded debris is of concern and warrants additional analysis as to the origin and potential complications. In this series of shortterm retrievals, the in vivo damage was insufficient to lead to IPD. Lever out testing and analysis should be completed again as longer term retrievals become available.
Acknowledgments
The authors acknowledge the use of The City College of New York electron microscopy facility. They acknowledge Elexis Baral for her assistance in data collection.
This work was done under a research contract with Stryker (Mahwah, NJ). Financial support was also provided from the Mary and Fred Trump Institute for Implant Analysis.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.arth.2016.01.039.
References
- 1.Prudhon JL, Ferreira A, Verdier R. Dual mobility cup: dislocation rate and survivorship at ten years of follow-up. Int Orthop 2013;37(12):2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grazioli A, Ek ET, Rudiger HA. Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop 2012;36(12):2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langlais FL, Ropars M, Gaucher F, et al. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res 2008;466(2):389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Philippot R, Boyer B, Farizon F. Intraprosthetic dislocation: a specific complication of the dual-mobility system. Clin Orthop Relat Res 2013;471(3):965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farizon F, de LAvison R, Azoulai JJ, Bousquet G. Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop 1998;22(4):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klingenstein GG, Yeager AM, Lipman JD, et al. Computerized range of motion analysis following dual mobility total hip arthroplasty, traditional total hip arthroplasty, and hip resurfacing. J Arthroplasty 2013;28(7):1173. [DOI] [PubMed] [Google Scholar]
- 7.Hailer NP, Weiss RJ, Stark A, et al. Dual-mobility cups for revision due to instability are associated with a low rate of re-revisions due to dislocation: 228 patients from the Swedish Hip Arthroplasty Register. Acta Orthop 2012;83(6): 566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loving L, Lee RK, Herrera L, et al. Wear performance evaluation of a contemporary dual mobility hip bearing using multiple hip simulator testing conditions. J Arthroplasty 2013;28(6):1041. [DOI] [PubMed] [Google Scholar]
- 9.Lachiewicz PF, Watters TS. The use of dual-mobility components in total hip arthroplasty. J Am Acad Orthop Surg 2012;20(8):481. [DOI] [PubMed] [Google Scholar]
- 10.Combes A, Migaud H, Girard J, et al. Low rate of dislocation of dual-mobility cups in primary total hip arthroplasty. Clin Orthop Relat Res 2013;471(12): 3891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Odland AN, Sierra RJ. Intraprosthetic dislocation of a contemporary dual-mobility design used during conversion THA. Orthopedics 2014;37(12): e1124. [DOI] [PubMed] [Google Scholar]
- 12.Banka TR, Ast MP, Parks ML. Early Intraprosthetic Dislocation in a Revision Dual-mobility Hip Prosthesis. Orthopedics 2014;37(4):e395. [DOI] [PubMed] [Google Scholar]
- 13.Wegrzyn J, Tebaa E, Jacquel A, et al. Can dual mobility cups prevent dislocation in all situations after revision total hip arthroplasty? J Arthroplasty 2015;30(4):631. [DOI] [PubMed] [Google Scholar]
- 14.Burge AJ, Gold SL, Lurie B, et al. MR Imaging of Adverse Local Tissue Reactions around Rejuvenate Modular Dual-Taper Stems. Radiology 2015;277:142. [DOI] [PubMed] [Google Scholar]
- 15.Hood RW, Wright TM, Burstein AH. Retrieval analysis of total knee prostheses: a method and its application to 48 total condylar prostheses. J Biomed Mater Res 1983;17(5):829. [DOI] [PubMed] [Google Scholar]
- 16.Stoner KE, Nassif NA, Wright TM, et al. Laser scanning as a useful tool in implant retrieval analysis: a demonstration using rotating platform and fixed bearing tibial inserts. J Arthroplasty 2013;28(8 Suppl):152. [DOI] [PubMed] [Google Scholar]
- 17.Goldvasser D, Hansen VJ, Noz ME, et al. In vivo and ex vivo measurement of polyethylene wear in total hip arthroplasty: comparison of measurements using a CT algorithm, a coordinate-measuring machine, and a micrometer. Acta Orthop 2014;85(3):271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schroder DT, Kelly NH, Wright TM, et al. Retrieved highly crosslinked UHMWPE acetabular liners have similar damage as conventional UHMWPE. Clin Orthop Relat Res 2011;469:387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adam P, Farizon F, Fessy MH. Dual mobility retentive acetabular liners and wear: surface analysis of 40 retrieved polyethylene implants. Rev Chir Orthop Reparatrice Appar Mot 2014;100(1):85. [DOI] [PubMed] [Google Scholar]



