Abstract
Objective.
Subjective age has been implicated in a range of health outcomes. The present study extends existing research by providing new data on the relation between subjective age and mortality in three large national samples.
Methods.
Participants (total N > 17,000) were drawn from the Health and Retirement Study (HRS, 2008–2014), the Midlife in the United State Survey (MIDUS, 1995–2014), and the National Health and Aging Trends Study (NHATS, 2011–2014). Subjective age, demographic factors, disease burden, functional limitations, depressive symptoms, and physical inactivity were assessed at baseline and mortality data were tracked for up to 20 years. Cognition was also included as a covariate in the HRS and the NHATS.
Results.
Individuals felt on average 15% to 16% younger relative to their chronological age. Feeling approximately 8, 11, and 13 years older in the MIDUS, HRS, and NHATS, was related to an 18%, 29% and 25% higher risk of mortality, respectively. This pattern was confirmed by a meta-analysis of the three samples (HR = 1.24; 95%CI = 1.17–1.31, p<.001). Multivariate analyses showed that disease burden, physical inactivity, functional limitations, and cognitive problems, but not depressive symptoms, accounted for the associations between subjective age and mortality.
Conclusions.
The present study provides robust evidence for an association between an older subjective age and a higher risk of mortality across adulthood. These findings support the role of subjective age as a biopsychosocial marker of aging.
Keywords: Subjective age, mortality, depression, disease burden, physical inactivity, functional limitations, cognition
INTRODUCTION
A growing literature indicates that subjective age, indexed by how old or young individuals feel relative to their chronological age, is associated with a range of health-related outcomes, such as incident hospitalization (1), cognitive impairment and dementia (2), and other chronic diseases and conditions (3). People who feel older also tend to have a higher vulnerability to stress (4), higher risk of depression (5), and poor sleep quality (6). In addition, an older subjective age is related to health-risk behavior, such as a sedentary lifestyle (7). At a biological level, an older subjective age is related to markers of physiological dysregulation, such as higher systemic inflammation and adiposity, and poor pulmonary and muscular functions (8,9). These health, behavioral, and physiological outcomes are in turn risk factors for mortality, which support the hypothesis that subjective age is related to life expectancy.
In line with this hypothesis that subjective age may predict survival, longitudinal studies found that an older subjective age culminates in higher mortality risk (10–12). While evidence to date is promising, past research on the association between subjective age and mortality has relied on small and selective samples, composed exclusively of older adults from Europe. There is a lack of longitudinal studies that examine this association in larger and more diverse samples. It is also unknown whether this association emerges in samples of older adults or whether it can be detected in samples of midlife adults. Previous studies were based on European samples and there are cross-cultural differences in subjective age. Indeed, there is a stronger tendency to feel younger in the US compared to Europe (13), and in its implications for functioning, with stronger link observed in the US (13). One meta-analysis has been conducted but it combined subjective age findings with those of other aging-related constructs such as attitudes toward one’s aging (14). While related, these constructs are distinct and should be considered separately (15).
The present study extends existing knowledge by examining the relation between subjective age and mortality using three new large national samples from the United States. Consistent with past research (10–12), it was hypothesized that an older subjective age is associated with a higher risk of mortality across the three samples that varied in terms of the age of the participants and the length of follow-up. Findings from these three samples were combined in a meta-analysis. Given that an older subjective age has been related to higher disease burden (3), depressive symptoms (5), lower cognitive abilities (2) and lower physical activity (7), which are risk factors for mortality (16–19), additional analyses tested whether the association between subjective age and mortality was accounted for by these mortality-related factors.
METHOD
Participants
HRS.
Data from the Health and Retirement Study (HRS), a nationally representative longitudinal study sponsored by the National Institute of Aging (grant number NIA U01AG009740) and conducted by the University of Michigan, were used. The HRS included Americans ages 50 and older and their spouses. Subjective age was first assessed in 2008. Therefore, the 2008 assessment was used in this study as the baseline measure. A total of 6510 participants aged 50 years and older provided subjective age data at baseline. Participants with subjective age, mortality and demographic data were included, resulting in a final sample of 6220 participants aged from 50 to 107 years (59.3% women, Mean age= 69.51, SD= 9.75).
NHATS.
Participants were also drawn from the National Health and Aging Trends Study (NHATS), a nationally representative prospective cohort study of Medicare enrollees aged 65 years and older. NHATS is funded by the National Institute on Aging (NIA-U01AG032947) and conducted by the Johns Hopkins Bloomberg School of Public Health. The baseline measure of subjective age was obtained from the first wave in 2011 among a total of 6669 participants. Complete data on subjective age, mortality and demographic were obtained from 6494 participants (57.8% women, Mean Age= 77.05, SD= 7.65, Age range= 65–105 years).
MIDUS.
Data were drawn from first (MIDUS I) and third wave (MIDUS III) of the Midlife in the United States longitudinal survey (MIDUS). The MIDUS I was conducted in 1994–1995 and was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. Participants completed a 30-minute telephone interview and a self-administered questionnaire, which included the subjective age assessment and demographic information. A total of 6163 participants had data on subjective age at baseline, and 4898 individuals (52.5% women; Mean age= 48.10; SD= 12.90; Age range= 24–75 years) had complete data on vital status, subjective age and demographic factors.
Measures
Subjective age.
In the MIDUS, participants were asked: “Many people feel older or younger than they actually are. What age do you feel most of the time?”. In the HRS, the following item was used: “Many people feel older or younger than they actually are. What age do you feel?” And in the NHATS, the question was: “Sometimes people feel older or younger than their age. During the last month, what age did you feel most of the time?”. In the three samples, participants were asked to specify this felt age in years. A proportional discrepancy score between chronological age and felt age was computed by subtracting chronological age from felt age and then dividing by chronological age (2, 20). A positive value indicated an older subjective age whereas a negative value indicated a younger subjective age. Consistent with past research (2), participants with discrepancy values three standard deviations above or below the mean were considered outliers and removed from analysis in the MIDUS (N= 77), the HRS (N= 100), and the NHATS (N=108).
Mortality.
In the HRS, vital status was obtained through the National Death Index (NDI) or proxy report, and was available as of April 2015. In the NHATS, mortality information was obtained as of November 2014 from proxy report. In the MIDUS, information on vital status was obtained from the NDI and longitudinal sample maintenance as of June 2014. In the three samples, survival time was computed from the month of baseline interview to the month of the last interview for living participants or the month of death for deceased participants.
Covariates.
Age, sex, marital status, and race were included as demographic covariates in the three samples. Education was reported on a scale ranging from 1 (no grade school) to 12 (doctoral level degree) in the MIDUS, on a scale from 1 (No schooling completed) to 9 (Master’s, professional or doctoral degree) in the NHATS, and in years in the HRS. In the three samples, disease burden was computed as the sum of diagnosed conditions, including high blood pressure, diabetes, cancer, lung disease, heart condition, stroke, osteoporosis or arthritis. In the MIDUS, the Composite International Diagnostic Interview Short Form scales (CIDI-SF; scores ranged from 0 to 7) (21) was used to assess depression. The Patient Health Questionnaire-2 (PHQ-2; scores ranged from 1 to 4) (22) was used to measure depressive symptoms in the NHATS. An 8-item version of the Centers for Epidemiologic Studies Depression (CES-D; scores ranged from 0 to 8) (23) was used in the HRS. In the MIDUS, participants were asked to indicate the frequency of their participation in moderate (e.g. brisk walking) and vigorous (e.g., running) physical activity during the summer and winter months on a scale ranging from 1 (several times per week or more) to 6 (never). In the HRS, participants reported frequency of both vigorous and moderate activities on a scale from 1 (more than once a week) to 4 (hardly ever or never); the average of these two items was used. In the NHATS, participants were asked to report whether they ever spent time on vigorous activities in the last month (e.g. working out, swimming, running or biking, or playing a sport) using a yes/no format. Functional limitations in MIDUS were assessed by asking participants how much their health limited their ability to do a number of activities of daily living (ADL; e.g., bathing, dressing) and instrumental activities of daily living (IADL; e.g., lifting or carrying groceries) using a scale ranging from 1 (not at all) to 4 (a lot). Answers were averaged, with higher scores indicating more functional limitations. In the HRS, participants were asked whether they had any difficulty with ADLs and IADLs because of physical, mental, emotional, or memory problems. The total number of activities with reported difficulty was used. In the NHATS, ADLs and IADLs were assessed by asking participants to report whether they have problems doing everyday activities without help. The total number of activities requiring help was computed. Baseline cognition was only available in the HRS and the NHATS. In the HRS, cognition was measured using the modified Telephone Interview for Cognitive Status (TICSm). A composite score ranging from 0 to 27 was computed from a test of immediate and delayed recall to assess short-term memory, a serial 7 subtraction test to assess working memory, and a backward counting test to assess mental processing speed (2). The clock drawing test was used in the NHATS. Scores ranged from 0 to 5. In both samples, higher scores indicated better cognition.
Data analysis
Cox proportional hazard ratio models were used to examine the association between subjective age and mortality in each of the three samples. Time to event was defined as the time (in years) from the subjective age assessment to the month of death or the month of last assessment. The analysis was adjusted for age, sex, education and race. The proportionality assumption was met in each of the three samples. Disease burden, depressive symptoms, functional limitations, and physical inactivity were further included in additional analyses. Cognition was included in both the NHATS and the HRS. Subjective age, education, depression, disease burden, physical inactivity, functional limitations, and cognition (HRS, NHATS) were converted to z-scores in each sample. The results from the three samples were combined using a random effects meta-analysis. Potential sources of heterogeneity between the three samples included age at baseline, age-related differences in health, and time to follow-up.
RESULTS
Descriptive statistics for the three samples are presented in Table 1. In the MIDUS, 960 individuals died (20%) over a median follow-up of 18 years (range: 2 months-19 years), for a total of 72,939 person-years. In the HRS, there were 1,120 deceased participants (18%), with a median follow-up of 5 years (range: 1 month-7 years), for a total of 33,001 person-years. There were 749 deaths in the NHATS (12%) over a median follow-up of 3 years (range: 1 month-3.50 years) for a total of 17,275 person-years. On average, individuals felt 15% to 16% younger relative to their chronological age (Table 1). The discrepancy scores indicate that the MIDUS, HRS, and NHATS participants felt on average 8 (average age*discrepancy score: 48*.16), 10 (69*.15), and 12 (77*.16) years younger, respectively. The proportion of individuals with an older subjective age (a felt age higher than chronological age) was 10% in both the MIDUS and the HRS, and 7% in the NHATS, whereas individuals with a younger subjective age (a felt age lower than chronological age) were 81%, 76% and 73% in the MIDUS, the HRS, and the NHATS respectively.
Table 1.
Descriptive Statistics in the MIDUS, the HRS and the NHATS
| MIDUS | HRS | NHATS | ||||
|---|---|---|---|---|---|---|
| Age, y | 48.10 (12.90) | 69.51 (9.75) | 77.05 (7.65) | |||
| Sex, female, n (%) | 2571(52.5) | - | 3690(59.3) | - | 3752(57.8) | - |
| Marital Status, married/living with a partner, n (%) | 3472(70.9) | - | 3824(61.5) | - | 3368(51.9) | - |
| Race, white, n (%) | 4570(93.3) | - | 5177(83.2) | - | 4591(70.7) | - |
| Education | 6.99(2.48) | 12.61 (3.10) | 5.08 (2.21) | |||
| Subjective Age | −0.16(0.16) | −0.15(0.16) | −0.16 (0.17) | |||
| Depressive Symptoms | 0.69 (1.81) | 1.36(1.92) | 1.48 (0.68) | |||
| Disease Burden | 2.40 (2.47) | 2.10 (1.35) | 2.52 (1.55) | |||
| Physical Inactivity | 2.31(1.23) | 2.65 (1.08) | 64% | - | ||
| Cognitive functioning | - | - | 15.20 (4.33) | 3.44 (1.07) | ||
| Functional limitations | 1.36(0.58) | 0.52(1.34) | 0.85(2.26) |
Note. MIDUS: N= 4898; HRS: N= 6220; NHATS: N= 6494
Ns differ for depressive symptoms, disease burden, physical inactivity, functional limitations, and cognition because data were missing. Education was reported on a scale ranging from 1 (no grade school) to 12 (doctoral level degree) in the MIDUS, on a scale from 1 (No schooling completed) to 9 (Master’s, professional or doctoral degree) in the NHATS, and in years in the HRS. See method section for differences in assessments and coding of each variables in each sample.
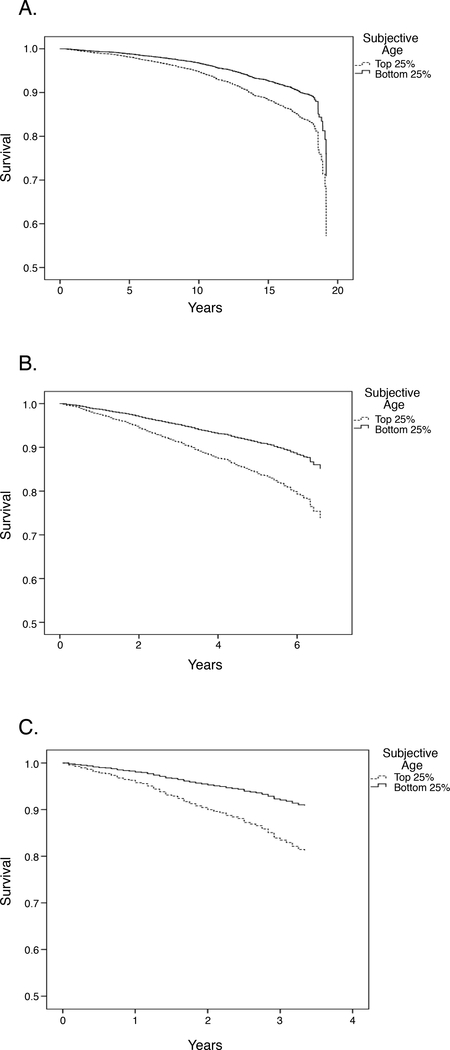
The Cox regression revealed that a 1SD older subjective age, which refers to feeling approximately 8, 11, and 13 years older respectively in the MIDUS, HRS, and NHATS, was related to an 18%, 29% and 25% higher risk of mortality in the MIDUS, HRS, and NHATS respectively, controlling for demographic factors (Table 2). Figure 1 plotted the survival curves for individuals in the top and bottom 25% of the distribution of subjective age discrepancy. The overall pattern was supported by the meta-analysis (HR = 1.24; 95%CI = 1.17–1.31, p<.001) (Table 2). We further examined the impact of terminal decline by excluding mortality cases that occurred one year after baseline assessment and found that the results were similar across the three samples (see Table S1, Supplemental Digital Content 1). The association between subjective age and mortality was attenuated and reduced to non-significance, except for the NHATS, after the inclusion of disease burden, depressive symptoms, physical inactivity, and functional limitations (Table 2).
Table 2.
Summary of Cox Proportional Hazard Ratio Analysis Predicting Mortality Risk from Subjective Age in the MIDUS, the HRS, and the NHATS
| MIDUS | HRS | NHATS | ||||
|---|---|---|---|---|---|---|
| Predictor | Model 1 | Model 2a | Model 1 | Model 2b | Model 1 | Model 2c |
| Hazard Ratios (95% CI) | Hazard Ratios (95% CI) | Hazard Ratios (95% CI) | Hazard Ratios (95% CI) | Hazard Ratios (95% CI) | Hazard Ratios (95% CI) | |
| Age | 1.09(1.09-1.10)*** | 1.09(1.08-1.09)*** | 1.09(1.08-1.10)*** | 1.07(1.06-1.07)*** | 1.10(1.08-1.11)*** | 1.07(1.06-1.08)*** |
| Sex | 1.60(1.41-1.83)*** | 1.84(1.61-2.10)*** | 1.55 (1.37-1.76)*** | 1.68(1.46-1.93)*** | 1.54(1.31-1.80)*** | 1.68(1.42-1.99)*** |
| Marital Status | .58(.51-.66)*** | .65(.57-.75)*** | .73(.64-.83)*** | .77(.67-.89)*** | .82(.69-.97)* | .81(.68-.97)* |
| Race | .70 (.55-.89)** | .80 (.63-1.02) | .90 (.77-1.06) | 1.22(1.01-1.47)* | .99 (.84-1.17) | 1.26 (1.05-1.50)* |
| Education | .78 (.73-.84)*** | .84 (.79-.90)*** | .90(.85-.95)*** | 1.04(.97-1.11) | .85(.79-.92)*** | .96(.88-1.04) |
| Subjective Age | 1.18 (1.10-1.26)*** | 1.07 (1.00-1.14) | 1.29(1.22-1.38)*** | 1.06(.99-1.13) | 1.25 (1.15-1.35)*** | 1.10 (1.01-1.19)* |
| Disease Burden | 1.08(1.01-1.15)* | 1.31(1.22-1.40)*** | 1.26(1.17-1.36)*** | |||
| Depression | 1.04(.97-1.11) | 1.06(1.00-1.14) | 1.05(.98-1.13) | |||
| Physical Inactivity | 1.14(1.07-1.21)*** | 1.41(1.30-1.52)*** | 1.35(1.11-1.63)** | |||
| Cognition | - | .80(.74-.86)*** | .84(.78-.91)*** | |||
| Functional | 1.29(1.21-1.36)*** | 1.14(1.09-1.21)*** | 1.25(1.18-1.32)*** | |||
| Limitations | ||||||
| Meta-Analysis | ||||||
| Random Effect | 1.24 (1.17-1.31)*** | |||||
| Heterogeneity I2 | 42.47 | |||||
Note. MIDUS: N= 4898; HRS: N= 6220; NHATS: N= 6494
Ns differ across the models because data were missing for disease burden, physical inactivity, cognition, functional limitations and depressive symptoms:
N= 4880
N= 5498
N= 6155
Cognition was available at baseline only in the NHATS and the HRS. Education, disease burden, depressive symptoms, physical inactivity (in the HRS and the MIDUS), cognition (in the HRS and the NHATS), functional limitations, and subjective age were z-scored in all analysis.
p<.05
p<.01
p<.00
Figure 1.
Survival curves by subjective age categories in the MIDUS (A), the HRS (B) and the NHATS (C). Subjective age categories are based on the quartiles of the distribution of the subjective age discrepancy: The bottom 25% corresponds to individuals with a younger subjective age and the top 25% refers to individuals with a relatively older subjective age. Curves are adjusted for demographic factors (age, sex, race, and education)
DISCUSSION
Using data from three large longitudinal samples, the present study provides consistent evidence for an association between an older subjective age and a higher risk of mortality. Across the three samples, this risk was twofold higher among individuals who felt older than their age compared to those who felt younger than their age. These findings extend past research in several ways. First, this association was observed not only in samples of older adults but also among middle-aged adults. Second, this relation was consistently observed over different follow-up times that spanned from three to twenty years and provides the longest longitudinal evidence in support of this association. Third, this study tested this association in the largest sample size to date, which was about sevenfold the previous meta-analysis on subjective age and mortality (14). Fourth, it is among the first to find support for this link in samples from the United States since past research focused mostly on European samples. Finally, our findings suggest that disease burden, depressive symptoms, functional limitations, physical inactivity and cognition are potential mediators of the association between subjective age and mortality.
Subjective age has been proposed as a biopsychosocial marker of aging because of its relation to a range of health-related processes. In the present study, adjustment for depressive symptoms, disease burden, functional limitations, cognition and physical inactivity fully accounted for the mortality risk in all but one sample. These findings are consistent with an evidence-based theoretical model in which subjective age is a biopsychosocial marker of aging. As suggested by such a model, an older subjective age is associated with more depressive symptoms (5), more chronic health conditions (3), less physical activity (7), and greater cognitive impairment (2) which are likely to be pathways through which feeling older may culminate in higher mortality risk. Other explanatory pathways are also likely to operate in this association. Indeed, an older subjective age is related to declines in sleep quality over time (6) and to physiological dysregulation (8, 9), which may convert into higher mortality risk over time. In addition, feeling older is associated with maladaptive personality trajectories (24) that have been found to increase mortality (25). Overall, the present study motivates more research to fully understand the pathways between subjective age and mortality, including biological, health-related and behavioral factors.
This study reveals that the age individuals feel is a marker of their risk of mortality in adulthood and old age over both the short term (3 years) and the long term (almost 20 years). This pattern also remained unchanged when people who died within 12 months of the assessment were excluded from the analysis. The present research, combined with past reports, suggests that this association is cross-culturally consistent. Although these findings suggest that the link between subjective age and mortality is consistent, the underlying mechanisms that operate in this relation may differ depending on individuals’ age and time of follow-up. For example, it is likely that behavior such as physical inactivity may play a stronger mediating role in old age. Indeed, the deleterious effect of this behavior may cumulate across the lifespan, and as a result it may be more salient for mortality in old age. In addition, although subjective aging contributes to health-related outcomes in middle and older age, this link is stronger in midlife and early old age (14). Therefore, it is likely that the link between an older subjective age and mortality among middle-aged adults may occur particularly through worse physical and mental health.
From a practical perspective, an assessment of subjective age may prove useful to identify individuals at risk of mortality who may benefit from an intervention. Interventions that reduce risk of declines in physical and mental health that ultimately lead to better health and well-being and longer survival could be targeted towards individuals with an older subjective age. For example, physical activity programs may be particularly beneficial among individuals with an older subjective age because it may promote overall physical, cognitive and mental health, resulting in lower mortality risk. Given that subjective age is modifiable (26), interventions through exercise could also be directly designed to change subjective age from older to younger. Such a shift may lead to changes in behavior and health status and ultimately longer survival.
This research has limitations to consider. While the three studies include large national cohorts, participants with complete data are self-selected subgroups. In addition, the cause of death was not identified. Of interest, one recent study found that an older subjective age was related to higher risk of cardiovascular death but not to cancer mortality (11). This association is complemented by findings of a link between subjective age and cardiovascular risk factors, such as inflammation, adiposity, and physical inactivity (7–9). However, the scarcity of research suggests a need for more studies to test whether the subjective age-mortality association varies depending upon the cause of death and whether feeling older increases risk of specific causes of mortality. In addition, the present study focused only on static level of subjective age and risk of mortality. Future research could examine the extent to which changes in subjective age is associated with mortality risk. Further, subjective age is a multidimensional construct (27), and more research is needed to examine whether specific aspects of subjective age, such as felt age in the domains of physical fitness, cognitive functioning or health, are predictors of mortality. Finally, future research could test for potential mediators of the relation between subjective age and mortality. Despite these limitations, the present study provides robust evidence that feeling older than one’s age is associated with increased risk of mortality across adulthood and old age.
Supplementary Material
Acknowledgments
Conflicts of Interest and Source of Funding: None
Abbreviations:
- MIDUS
Midlife in the United States
- HRS
Health and Retirement Study
- NHATS
National Health and Aging Trends Study
References
- 1.Stephan Y, Sutin AR, Terracciano A. Feeling older and risk of hospitalization: Evidence from three longitudinal cohorts. Health Psychol 2016; 35: 634–7 [DOI] [PubMed] [Google Scholar]
- 2.Stephan Y, Sutin AR, Luchetti M, Terracciano A. Feeling older and the development of cognitive impairment and dementia. J Gerontol B Psychol Sci Soc Sci 2017; 72 : 966–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demakakos P, Gjonca E, Nazroo J. Age identity, age perceptions, and health: Evidence from the English Longitudinal Study of Ageing. Ann N Y Acad Sci 2007; 1114: 279–87. [DOI] [PubMed] [Google Scholar]
- 4.Shrira A, Palgi Y, Ben-Ezra M, Hoffman Y, Bodner E. A youthful age identity mitigates the effect of post-traumatic stress disorder symptoms on successful aging. Am J Geriatr Psychiatry 2016; 24 :174–5. [DOI] [PubMed] [Google Scholar]
- 5.Choi NG, DiNitto DM. Felt age and cognitive-affective depressive symptoms in late life. Aging Ment Health 2014; 18: 833–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stephan Y, Sutin AR, Bayard S, Terracciano A. Subjective age and sleep in middle-aged and older adults. Psychol Health; 32 : 1140–51. [DOI] [PubMed] [Google Scholar]
- 7.Wienert J, Kuhlmann T, Fink S, Hambrecht R, Lippke S. Testing principle working mechanisms of the health action process approach for subjective physical age groups. Res Sports Med. 2016; 24: 67–83. [DOI] [PubMed] [Google Scholar]
- 8.Stephan Y, Sutin AR, Terracciano A. Younger subjective age is associated with lower C-reactive protein among older adults. Brain Behav Immun. 2015; 43: 33–6. [DOI] [PubMed] [Google Scholar]
- 9.Stephan Y, Sutin AR, Terracciano A. How old do you feel? The role of age discrimination and biological aging in subjective age. PLoS One 2015; 10:e0119293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotter-Grühn D, Kleinspehn-Ammerlahn A, Gerstorf D, Smith J. Self-perceptions of aging predict mortality and change with approaching death: 16-year longitudinal results from the Berlin Aging Study. Psychol Aging 2009; 24: 654–67. [DOI] [PubMed] [Google Scholar]
- 11.Rippon I, Steptoe A. Feeling old vs being old: Associations between self-perceived age and mortality. JAMA Intern Med 2015; 175: 307–9. [DOI] [PubMed] [Google Scholar]
- 12.Uotinen V, Rantanen T, Suutama T. Perceived age as a predictor of old age mortality: A 13-year prospective study. Age Ageing 2005; 34 : 368–72. [DOI] [PubMed] [Google Scholar]
- 13.Westerhof GJ, Barrett AE. Age identity and subjective well-being: A comparison of the United States and Germany. J Gerontol B Psychol Sci Soc Sci 2005; 60 : 129–36.14. [DOI] [PubMed] [Google Scholar]
- 14.Westerhof GJ, Miche M, Brothers AF, Barrett AE, Diehl M, Montepare JM, Wahl HW, Wurm S.: The influence of subjective aging on health and longevity: A meta-analysis of longitudinal data. Psychol Aging 2014; 29: 793–802. [DOI] [PubMed] [Google Scholar]
- 15.Kotter-Grühn D, Kornadt AE, Stephan Y. Looking beyond chronological age: Current knowledge and future directions in the study of subjective age. Gerontology 2015; 62: 86–93. [DOI] [PubMed] [Google Scholar]
- 16.Beltrán-Sánchez H, Jiménez MP, Subramanian SV. Assessing morbidity compression in two cohorts from the Health and Retirement Study. Journal Epidemiol Community Health 2016; 70 : 1011–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White J, Zaninotto P, Walters K, Kivimäki M, Demakakos P, Biddulph J, Kumari M, De Oliveira C, Gallacher J, Batty GD. Duration of depressive symptoms and mortality risk: The English Longitudinal Study of Ageing (ELSA). Br J Psychiatry 2016; 208 : 337–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perna L, Wahl HW, Mons U, Saum KU, Holleczek B, Brenner H. Cognitive impairment, all-cause and cause-specific mortality among non-demented older adults. Age Ageing 2015; 44 : 445–51. [DOI] [PubMed] [Google Scholar]
- 19.Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM, Lancet Physical Activity Series 2 Executive Committee, Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016; 388 : 1302–10. [DOI] [PubMed] [Google Scholar]
- 20.Brothers A, Miche M, Wahl HW, Diehl M. Examination of associations among three distinct subjective aging constructs and their relevance for predicting developmental correlates. J Gerontol B Psychol Sci Soc Sci. 2017; 72 : 547–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Andrews G, Mroczek D, Ustun TB, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods Psychiatr Res. 1998; 7: 171–85. [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003; 41:1284–92. [DOI] [PubMed] [Google Scholar]
- 23.Wallace R, Herzog AR, Ofstedal MB, Steffick D, Fonda S, Langa K Documentation of Affective Functioning Measures in the Health and Retirement Study. Survey Research Center, University of Michigan, Ann Arbor, MI, 2000 [Google Scholar]
- 24.Stephan Y, Sutin AR, Terracciano A Subjective age and personality development: A 10-year study. J Pers 2015; 83 : 142–54. [DOI] [PubMed] [Google Scholar]
- 25.Mroczek DK, Spiro A. Personality change influences mortality in older men. Psychol Sci. 2007; 18 :371–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stephan Y, Chalabaev A, Kotter-Grühn D, Jaconelli A. “Feeling younger, being stronger”: an experimental study of subjective age and physical functioning among older adults. J Gerontol B Psychol Sci Soc Sci. 2013;68(1):1–7. [DOI] [PubMed] [Google Scholar]
- 27.Kornadt AE, Hess TM, Voss P, Rothermund K. Subjective age across the life span: A differentiated, longitudinal approach. J Gerontol B Psychol Sci Soc Sci in press [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.