Abstract
Background
Adverse childhood experiences (ACEs) affect adult mental health and tend to contribute to greater symptoms of depression and more frequent suicide attempts. Given the relationship between symptoms of depression and patient-reported outcomes (PROs), adversity in childhood might be associated with PROs in patients seeking care for musculoskeletal problems, but it is not clear whether in fact there is such an association among patients seeking care in an outpatient, upper extremity orthopaedic practice.
Questions/purposes
(1) Are ACE scores independently associated with variation in physical limitations measured among patients seen by an orthopaedic surgeon? (2) Are ACE scores independently associated with variations in pain intensity? (3) What factors are associated with ACE scores when treated as a continuous variable or as a categorical variable?
Methods
We prospectively enrolled 143 adult patients visiting one of seven participating orthopaedic surgeons at three private and one academic orthopaedic surgery offices in a large urban area. We recorded their demographics and measured ACEs (using a validated 10-item binary questionnaire that measured physical, emotional, and sexual abuse in the first 18 years of life), magnitude of physical limitations, pain intensity, symptoms of depression, catastrophic thinking, and health anxiety. There were 143 patients with a mean age of 51 years, 62 (43%) of whom were men. In addition, 112 (78%) presented with a specific diagnosis and most (n = 79 [55%]) had upper extremity symptoms. We created one logistic and three linear regression models to test whether age, gender, race, marital status, having children, level of education, work status, insurance type, comorbidities, body mass index, smoking, site of symptoms, type of diagnosis, symptoms of depression, catastrophic thinking, and health anxiety were independently associated with (1) the magnitude of limitations; (2) pain intensity; (3) ACE scores on the continuum; and (4) ACE scores categorized (< 3 or ≥ 3). We calculated a priori that to detect a medium effect size with 90% statistical power and α set at 0.05, a sample of 136 patients was needed for a regression with five predictors if ACEs would account for ≥ 5% of the variability in physical function, and our complete model would account for 15% of the overall variability. To account for 5% incomplete responses, we enrolled 143 patients.
Results
We found no association between ACE scores and the magnitude of physical limitations measured by Patient-Reported Outcomes Measurement Information System Physical Function (p = 0.67; adjusted R2 = 0.55). ACE scores were not independently associated with pain intensity (Pearson correlation [r] = 0.11; p = 0.18). Greater ACE scores were independently associated with diagnosed mental comorbidities both when analyzed on the continuum (regression coefficient [β] = 1.1; 95% confidence interval [CI], 0.32-1.9; standard error [SE] 0.41; p = 0.006) and categorized (odds ratio [OR], 3.3; 95% CI, 1.2-9.2; SE 1.7; p = 0.024), but not with greater levels of health anxiety (OR, 1.1; 95% CI, 0.90-1.3; SE 0.096; p = 0.44, C statistic = 0.71), symptoms of depression (ACE < 3 mean ± SD = 0.73 ± 1.4; ACE ≥ 3 = 1.0 ± 1.4; p = 0.29) or catastrophic thinking (ACE < 3 = 3.6 ± 3.5; ACE ≥ 3 = 4.9 ± 5.1; p = 0.88).
Conclusions
ACEs may not contribute to greater pain intensity or magnitude of physical limitations unless they are accompanied by greater health anxiety or less effective coping strategies. Adverse events can contribute to anxiety and depression, but perhaps they sometimes lead to development of resilience and effective coping strategies. Future research might address whether ACEs affect symptoms and limitations in younger adult patients and patients with more severe musculoskeletal pathology such as major traumatic injuries.
Level of Evidence
Level II, prognostic study.
Introduction
Greater adversity in childhood is associated with diminished adult mental health [10, 15]. The Adverse Childhood Experiences (ACEs) scale is a reliable and valid quantitative measure of childhood adversity [15]. The ACE scale assesses episodes of physical, emotional, and sexual abuse in the first 18 years of life. ACEs correlate with greater symptoms of depression in adult life, especially among people with limited self-reported social support [10]. In the United States, men who are sex offenders have at least three times greater odds of an ACE in at least one domain than the general population [25]. ACEs are associated with adult alcoholism, drug abuse, morbid obesity, suicide attempts, and poor self-rated health [16].
Given the correlation of symptoms of depression and patient-reported outcomes (PROs) in musculoskeletal illness, it is plausible that ACEs might affect PRO measures (PROMs) as well [5, 30, 33, 39]. A correlation of ACEs and PROMs among patients seeking care for a musculoskeletal problem might direct screening and treatment opportunities. However, to our knowledge, this possible association among patients seen by an orthopaedic surgeon has not been studied.
We therefore asked: (1) Are ACE scores independently associated with variation in physical limitations measured among patients seen by an orthopaedic surgeon? (2) Are ACE scores independently associated with variations in pain intensity? (3) What factors are associated with ACE scores when treated as a continuous variable or as a categorical variable?
Patients and Methods
After institutional review board approval of this prospective, cross-sectional, observational cohort study, we prospectively enrolled 143 adult patients between November 7 and November 20, 2017. Patients were seen at four orthopaedic surgery offices in a large urban area. We included all new and followup English-speaking patients who were aged between 18 and 89 years who visited one of seven orthopaedic surgeons (one lower extremity, one trauma, and five hand and upper extremity). The study population consisted of typical patients seen in outpatient offices with common diseases, many of which were age-related. They were not patients with major trauma, amputation, or major peripheral nerve injury. We excluded patients who were unable to speak and understand English because we did not have a complete set of validated questionnaires in other languages. Five research assistants (A-BD, EZB, JTPK, JSEO, LD), who were not involved with patient care, described the study to patients after the visit with the physician. Completion of the surveys represented informed consent. Two patients declined participation.
A priori power analysis indicated that a sample of 136 patients would provide 90% statistical power, with α set at 0.05, to detect a medium effect size (f2 = 0.15) for a regression with five predictors if ACEs would account for ≥ 5% of the variability in physical function, and our complete model would account for 15% of the overall variability. To account for 5% incomplete responses, we enrolled 143 patients.
Patients were asked to complete seven questionnaires at the end of their visit: (1) a demographic questionnaire consisting of age, sex, race-ethnicity, marital status, number of children, education status, work status, type of insurance, the presence of additional comorbidities, weight, and height; (2) the ACE scale; (3) the Patient-Reported Outcomes Measurement Information System (PROMIS) Physical Function (PF) Computer Adaptive Test (CAT); (4) an 11-point ordinal measure of pain intensity; (5) the Patient Health Questionnaire short form (PHQ-2); (6) the Pain Catastrophizing Scale short form (PCS-4); and (7) the Short Health Anxiety Inventory (SHAI-5).
After completing the questionnaires, the research assistant (A-BD, EZB, JTPK, JSEO, LD) filled out site of symptoms (arm/shoulder, leg, other site) and asked the surgeon if the diagnosis was specific or nonspecific.
The ACE scale is a validated 10-item binary questionnaire (“yes” or “no”) that retrospectively measures domains of physical, emotional, and sexual abuse in the first 18 years of life (Appendix, Supplemental Digital Content 1) [21]. Scores range from 0 to 10 with higher scores indicating more adverse experiences during patients’ childhood [2, 10]. The PROMIS PF CAT is a validated measure of physical limitations that can be completed with as few as four questions while still achieving high precision in scoring, thereby decreasing survey burden. PROMIS presents a continuous t-score with a mean of 50 and a SD of 10 with higher scores reflecting better physical function compared with the average of adults in the same age group [36]. Pain intensity was measured on an 11-point ordinal scale from 0 representing “no pain at all” to 10 representing “worst pain possible” [7, 22].
The PHQ-2, PCS-4, and SHAI-5 are all validated short-form measures of psychologic constructs (Appendix, Supplemental Digital Content 2). The PHQ-2 is a two-item measure of symptoms of depression over the past 2 weeks [8, 23, 26] (Appendix 2). The PCS-4 is a four-item measure with scores rating per item from 0 “not at all” to 4 “all the time” with total scores ranging from 0 to 16 with higher scores representing more catastrophic thinking (defined as mis- or overinterpretation of nociception) [6, 8, 37] (Appendix 2). The SHAI-5 is a five-item measure that assesses symptoms of health anxiety (the sense that one has a serious health problem despite reassurance to the contrary) [8, 24, 35]. Each item consists of four statements and has a score ranging from 0 to 3. Total scores range from 0 to 15 with higher scores representing greater symptoms of health anxiety (Appendix 2).
All questionnaires were administered on an encrypted tablet through a secure, HIPAA-compliant electronic platform: REDCap (Research Electronic Data Capture: a secure web-based application for building and managing online surveys and databases; Nashville, TN, USA) [18].
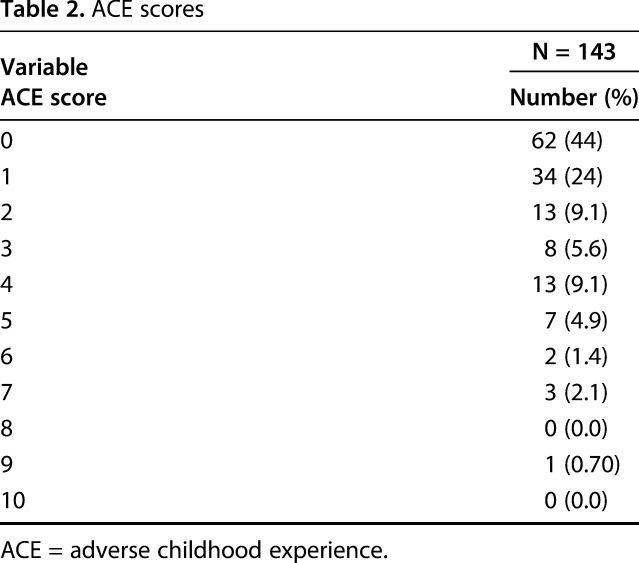
No patients were excluded from the analysis. The mean age of the 143 patients was 51 ± 16 years (range, 18-84 years) and 62 were men (43%; Table 1). One hundred patients (70%) had one or more children (mean 2.7 ± 1.9). Of all patients, 73 (50%) had one or more additional comorbidities. Of 143 patients, 112 (78%) presented with a specific diagnosis and the majority (55%) had symptoms of the arm or shoulder. Mean scores for pain intensity were 4.1 ± 2.5 and for PROMIS PF 47 ± 10. The mean ACE score was 1.5 ± 1.9 (range, 0-9). Thirty-four patients (24%) had ACE-scores of ≥ 3 (Table 1) and 62 patients (44%) did not experience any ACEs with scores of 0 (Table 2).
Table 1.
Patient and clinical characteristics
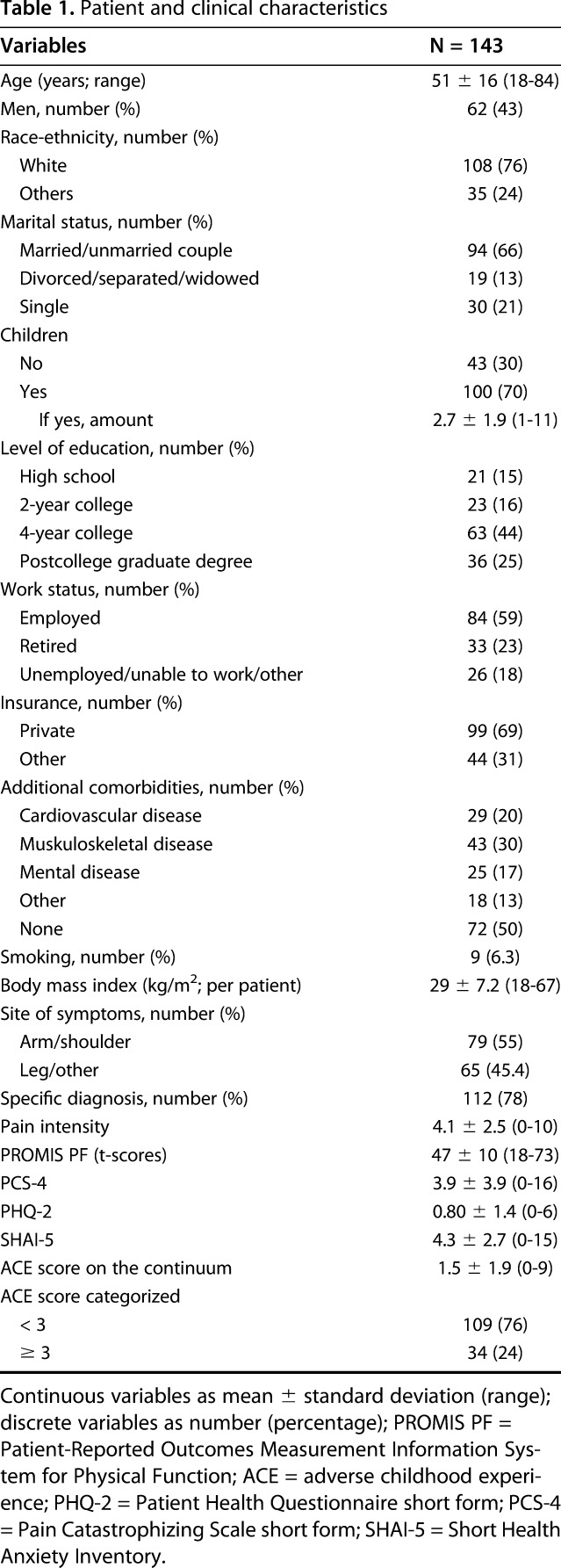
Table 2.
ACE scores
Statistical Analysis
Continuous variables are presented as mean ± SD and discrete data as proportions. We used the Student’s t-test to compare continuous and dichotomous variables, the Pearson correlation for two continuous variables, analysis of variance to compare continuous and ordinal variables, and Fisher’s exact test for two dichotomous variables.
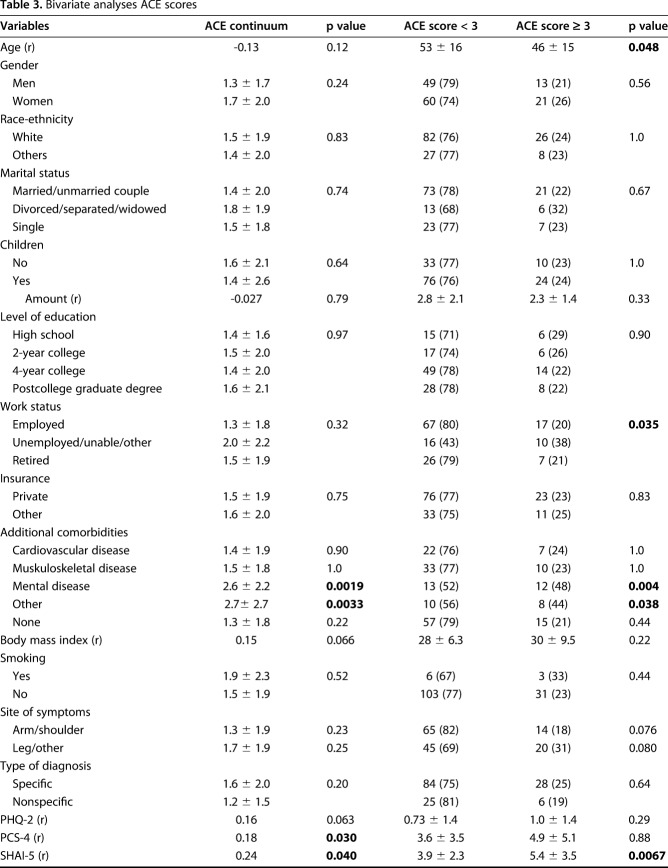
We analyzed ACE scores both on the continuum and categorized (Table 3). We created two groups: ACE scores of < 3 and of ≥ 3. In previous studies, ACE scores of ≥ 3 were combined into one category [2, 10, 14, 15].
Table 3.
Bivariate analyses ACE scores
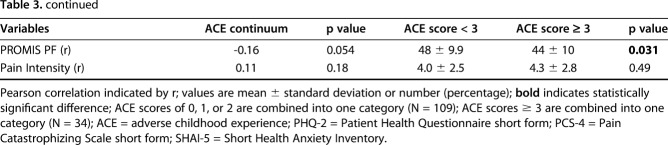
We created three backward stepwise regression models (Table 4) and one logistic regression model (Table 5) to identify independent factors associated with (1) the magnitude of limitations, measured with PROMIS PF; (2) pain intensity; (3) ACE scores on the continuum; and (4) ACE scores categorized (< 3 or ≥ 3). We included all factors with p < 0.10 on bivariate analysis (Table 3; Appendix, Supplemental Digital Content 3) in the final multivariable models. Regression coefficient (β) is the degree of change in a standardized outcome variable for every SD of change in the predictor variable. The higher the absolute value of the β coefficient, the stronger the effect. There are no set cutoff scores. Adjusted R2 indicates how much variability in the outcome variable the model accounts for. Semipartial R2 expresses the specific variability of a given independent variable in the model [1]. The C-statistic is a measure of goodness of fit in logistic regression models with a score between 0.50 and 1.00. Higher scores indicate a better goodness of fit with values > 0.7 indicating a good model and > 0.8 a strong model. We considered p < 0.05 significant.
Table 4.
Stepwise regression for predictors of PROMIS PF scores and Pain Intensity*
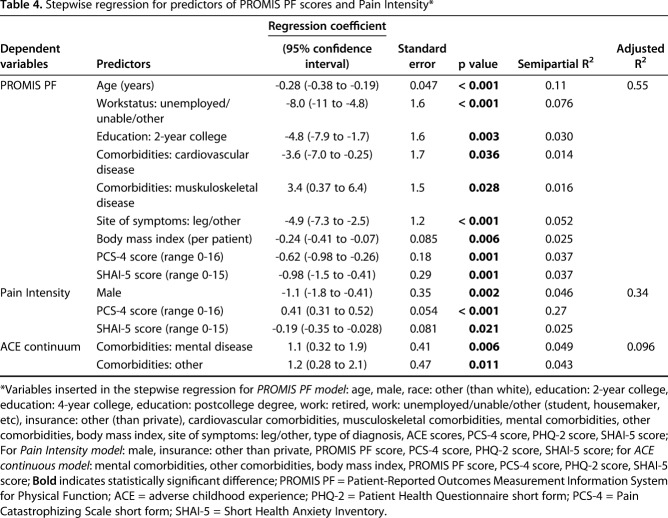
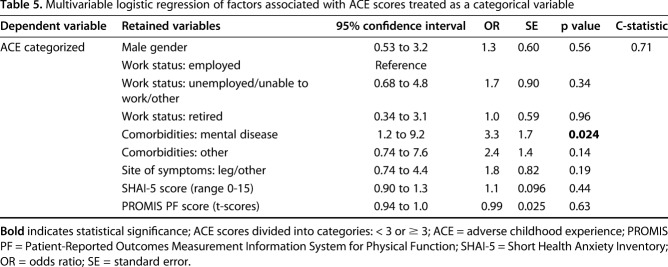
Table 5.
Multivariable logistic regression of factors associated with ACE scores treated as a categorical variable
Results
Association Between ACE Scores and PROMIS PF
After controlling for variables like age, race, catastrophic thinking, and type of diagnosis, we found no association between ACE scores and the magnitude of physical limitations measured by PROMIS PF (p = 0.67; adjusted R2 = 0.55). Greater physical limitations were independently associated with older age (regression coefficient [β] = -0.28; 95% confidence interval [CI], -0.38 to -0.19; standard error [SE] 0.047; p < 0.001; semipartial R2 = 0.11), being unemployed, unable to work, or having another work status than being retired or employed (β, -8.0; 95% CI, -11 to -4.8; SE 1.6; p < 0.001; semipartial R2 = 0.076), completing 2 years of college (β, -4.8; 95% CI, -7.9 to -1.7; SE 1.6; p = 0.003; semipartial R2 = 0.030), having cardiovascular comorbidities (β, -3.6; 95% CI, -7.0 to -0.25; SE 1.7; p = 0.036; semipartial R2 = 0.014), presenting with other symptoms than arm/shoulder (β, -4.9; 95% CI, -7.3 to -2.5; SE 1.2; p < 0.001; semipartial R2 = 0.052), greater body mass index (β, -0.24; 95% CI, -0.41 to -0.07; SE 0.085; p = 0.006; semipartial R2 = 0.025), greater health anxiety (β, -0.98; 95% CI, -1.5 to -0.41; SE 0.29; p = 0.001; semipartial R2 = 0.037), and greater catastrophic thinking (β, -0.62; 95% CI, 0.98 to -0.26; SE 0.29; p = 0.001; semipartial R2 = 0.025; adjusted R2 = 0.55; Table 4). Fewer physical limitations were independently associated with having musculoskeletal comorbidities (β, 3.4; 95% CI, 0.37-6.4; SE 1.5; p = 0.028; semipartial R2 = 0.016; Table 4). There are no set cutoff scores for the β regression coefficient. This model shows that, for example, 1 year of aging is accompanied with a decrease in physical function of 0.28 points measured by PROMIS PF.
ACE Scores and Pain Intensity
In bivariate analysis, ACE scores were not associated with greater pain intensity (Pearson correlation [r] = 0.11; p = 0.18). Accounting for potential interaction of variables like gender, insurance type, physical limitations, and symptoms of depression, greater pain intensity was independently associated with being a woman (β, -1.1; 95% CI, -1.8 to -0.41; SE 0.35; p = 0.002; semipartial R2 = 0.046), greater catastrophic thinking (β, 0.41; 95% CI, 0.31-0.52; SE 0.054; p < 0.001; semipartial R2 = 0.27), and less health anxiety (β, -0.19; 95% CI, -0.31 to -0.028; SE 0.081; p = 0.021; semipartial R2 = 0.025; adjusted R2 = 0.34; Table 4).
Factors Associated With ACE Scores Treated as Continuous or Categorical Variables
Accounting for the potential interactions of variables like comorbidities, symptoms of health anxiety, and symptoms of depression, we found greater ACE scores were independently associated with having mental comorbidities (β, 1.1; 95% CI, 0.33-1.9; SE 0.41; p = 0.006; semipartial, R2 = 0.049) or comorbidities other than cardiovascular, mental, or musculoskeletal diseases (β, 1.2; 95% CI, 0.28-2.1; SE 0.47; p < 0.011; semipartial R2 = 0.043; adjusted R2 = 0.096; Table 4) when treated as a continuous variable; when treated as a categorical variable, ACE scores ≥ 3 were independently associated with having mental comorbidities (odds ratio [OR], 3.3; 95% CI, 1.2-9.2; SE 1.7; p = 0.024) but not with health anxiety (OR, 1.1; 95% CI, 0.90-1.3; SE 0.096; p = 0.44, C statistic = 0.71; Table 5). These results can be interpreted as the following: having a mental comorbidity corresponds to an increase in ACE scores by 1.1 and increases the chance of having ≥ 3 ACEs by 3.3. In bivariate analysis treated as a categorical variable, we found no correlation between ACE scores and symptoms of depression (ACE < 3 mean ± SD = 0.73 ± 1.4; ACE ≥ 3 = 1.0 ± 1.4; p = 0.29; Table 3) or catastrophic thinking (ACE < 3 = 3.6 ± 3.5; ACE ≥ 3 = 4.9 ± 5.1; p = 0.88).
Discussion
Poor adult mental health is associated with ACEs, perhaps because adversity in childhood might reduce thresholds for depressive reactions to mild stressors [10, 29]. Given the correlation of symptoms of depression and PROs in musculoskeletal illness [5, 30, 33, 40], ACEs might be associated with PROMs as well. However, it is not clear whether in fact there is such an association among patients seeking care in an outpatient, upper extremity orthopaedic practice. We found no association between ACE scores and the magnitude of physical limitations measured by PROMIS PF nor between ACEs and pain intensity. This is potentially important because it is consistent with a body of research that suggests it is more helpful to measure and address current symptoms of stress and distress as well as effectiveness of effective coping strategies on their continuum in the moment than it is to address exposures or comorbidities.
We acknowledge some study limitations. First, most participants were white, married, employed, well-educated individuals (the majority had at least 4 years of college) with near average physical limitations (mean PROMIS PF t-scores of 47 ± 10; a score of 50 represents the population mean). Although enrolled in several outpatient offices and representative of the population living in the studied city, our results might not be generalizable to other populations, regions, and practice settings. Studies of patients with more severe disease or injury, greater ACEs, or specific types of ACEs might have different results. Our study addresses self-reported ACEs in what may be a group with relatively few ACEs or with ACEs of lesser severity. People might claim an ACE when reasonable observers would question whether it qualifies. Because the ACE is a mere count of perceived childhood events, one person might have a severe childhood event and another a relatively minor event, but each of those would be counted the same. This is a limitation both of our analysis (people with more difficult childhoods are likely underrepresented in our sample) and also of the ACE questionnaire. People may also feel uncomfortable acknowledging childhood adversity in the questionnaire and they may not answer honestly. Also, they may answer differently in private than they would if they were accompanied to the visit. This may be an instance in which an interview-based rating system would be preferable to a self-report questionnaire. Keeping these limitations in mind, our patients reported similar ACEs to prior studies. Forty-four percent (62 of 143) of our study population did not report any ACEs, which is lower than the 76% of patients who did not report ACEs in the study by Cheong et al. [10], but it is comparable to the 34% in an Irish study [28] and the 36% and 50% in American studies [9, 16]. To better understand the association of ACEs with symptom intensity and magnitude of limitations for musculoskeletal illness, we need studies of people who encountered a greater frequency and severity of adversity in childhood. It would also be useful to compare interview-based assessments with self-report questionnaires.
Another limitation was that our patients were generally older (with a mean age of 51 years), who generally had relatively minor (and certainly not limb- or life-threatening) conditions; most patients in this series had common problems such as trapeziometacarpal arthritis, rotator cuff tendinopathy, trigger finger, and carpal tunnel syndrome. Although psychologic and social determinants have a marked effect on symptoms and limitations for these illnesses, we might find different results if we studied people recovering from life-changing events such as major skeletal trauma or amputation. It is possible that people with more ACEs might have less reserve to manage the stress associated with severe pathology. The older age of our patients may also be important. Although our rate of ACEs was comparable to other studies, at this older age we may be studying patients who avoided major medical comorbidities, patients with a more adaptive response to ACEs, and people who have more opportunities to process their ACEs and put them aside. The effect of ACEs on PROs may be more pronounced in young adulthood in greater proximity to childhood adverse events. It is also important to note that we addressed pain intensity rather than persistence. Childhood adversity might have a stronger relationship to pain persistence and to pain intensity.
The lack of correlation of physical limitations with ACEs in our study is inconsistent with the findings of Felitti et al. [16], who found that patients in the primary care setting with an ACE score of ≥ 3 have greater physical inactivity (OR, 1.4). On the other hand, perceived limitations and physical activity are not interchangeable. Our patients had a comparably low prevalence of ACEs [9, 16, 28], but may have had less severe, more remote, and better accommodated ACEs than would be found in a younger adult population exposed to greater childhood adversity. It is also possible that the association of ACEs with PROs is mediated by symptoms of depression or resilience. Poole et al. [32] studied 4000 patients in a primary care setting and found that greater ACEs, of any type, increased the risk of anxiety later in life and that this process is mediated by greater emotional dysregulation (difficulties with impulse control and limited emotion regulation strategies). Patients with lower levels of resiliency have a stronger mediation effect of emotional dysregulation on the relationship between ACEs and anxiety in adulthood than patients with higher levels of resiliency [31, 32]. This suggests that effective coping strategies like resiliency influence the effect of ACEs later in life. A recent systematic review [17] confirms that individual-, family-, and community-level resilience factors reduce the risk of psychopathology later in life after childhood adversity. Howell and Miller-Graff [20] shows that during emerging adulthood, higher levels of resiliency are associated with greater intelligence, greater spirituality, and support from friends but not from family. This may help explain why a substantial percentage of people with ACEs have good mental health. For some, an ACE might even be a nidus for the development of enhanced resiliency in a supportive milieu. Our finding that magnitude of physical limitations was associated with greater health anxiety and greater catastrophic thinking is in line with previous evidence that consistently shows that psychologic factors account for variation in the magnitude of physical limitations for several specific and nonspecific upper extremity conditions [11, 13, 27, 30, 33, 34, 40].
The lack of a relationship between pain intensity and ACEs is inconsistent with evidence that sexual abuse in childhood—one item on the ACE questionnaire—is associated with greater persistent musculoskeletal pain [4, 12, 41]. We studied acute, not persistent, pain and studied a self-report count of ACEs, many of which may not have been as impactful as sexual abuse. Our initial application of ACEs in patients with musculoskeletal illness is not definitive and should be continued by studying different methods of quantifying childhood adversity, people with greater adversity, younger adults, and people with either persistent pain or more severe pathology. Anda et al. [3] found that patients with ACE scores > 4 have more frequent headaches (OR, 2.1) than those without any adversity in childhood. A possible explanation for variable relationships between ACEs and pain may be the varied definition of “childhood”, “abuse”, and “adversity” and the variety of surveys used to quantify them. Also, a study of musculoskeletal pain duration or persistence rather than pain intensity might have different findings. The finding that greater pain intensity was associated with greater catastrophic thinking is consistent with a strong body of evidence [34, 38].
The finding that ACEs, addressed on the continuum and in categories, are associated with diagnosed mental comorbidities is consistent with previous studies. Cheong et al. [10] reported a higher prevalence of estimated major depression among participants with at least one ACE (14%) compared with those who experienced no ACEs (6.0%). This adds another potential explanation for the lack of correlation between ACEs on PROMs: the influence of comorbid depression and anxiety may be diminished because these conditions were diagnosed and effectively treated. Again, it may not be as fruitful to focus on ACEs or diagnosed mental health comorbidities per se, but rather on current symptoms of stress and distress and current effectiveness of coping strategies.
Pending corroboration by others and testing in other populations, our findings suggest that ACEs may not contribute to greater pain intensity or magnitude of physical limitations unless they are accompanied by greater health anxiety or less effective coping strategies. Adverse events can contribute to anxiety and depression, but they can also lead to development of resilience and effective coping strategies [19, 20, 31, 32]. Future research might address whether ACEs affect symptoms and limitations in younger adult patients with less advantageous socioeconomic situations that may expose them to a greater number of ACEs or specific types of ACE that have greater impact and with more severe musculoskeletal pathology such as major traumatic injuries. Pending additional evidence, it seems that attention is best directed toward stress, distress, and less effective coping strategies, regardless of their potential origin.
Acknowledgments
We thank Lindy Derkzen and Anne-Britt Dekker for their help with enrolling patients at several orthopaedic surgery offices.
Footnotes
One of the authors certifies that he (DR), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Skeletal Dynamics (Miami, FL, USA), less than USD 10,000 USD from Wright Medical (Memphis, TN, USA) for royalties for elbow implants, is Deputy Editor for the Journal of Hand Surgery, is Deputy Editor for Clinical Orthopaedics and Related Research®, universities and hospitals, and lawyers outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at The Dell Medical School–University of Texas, Austin, TX, USA.
References
- 1.Abdi H. Part (semi partial) and partial regression coefficients . In: Salkind NJ, ed. Encyclopedia of Measurement and Statistics . 1st ed. Thousand Oaks, CA, USA: Sage Publications; 2007:736-740. [Google Scholar]
- 2.Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med . 2010;39:93-98. [DOI] [PubMed] [Google Scholar]
- 3.Anda RF, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache . 2010;50:1473-1481. [DOI] [PubMed] [Google Scholar]
- 4.Arnow BA. Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization. J Clin Psychiatry. 2004;65(Suppl 12):10-15. [PubMed] [Google Scholar]
- 5.Becker SJE, Makarawung DJS, Spit SA, King JD, Ring D. Disability in patients with trapeziometacarpal joint arthrosis: incidental versus presenting diagnosis. J Hand Surg Am. 2014;39:2009-2015. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein DN, Sood A, Mellema JJ, Li Y, Ring D. Lifetime prevalence of and factors associated with non-traumatic musculoskeletal pains amongst surgeons and patients. Int Orthop. 2017;41:31-38. [DOI] [PubMed] [Google Scholar]
- 7.Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8:1153-1157. [DOI] [PubMed] [Google Scholar]
- 8.Bot AGJ, Becker SJE, van Dijk CN, Ring D, Vranceanu A-M. Abbreviated psychologic questionnaires are valid in patients with hand conditions. Clin Orthop Relat Res. 2013;471:4037-4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. About the CDC-Kaiser ACE Study. 2016. Available at: https://www.cdc.gov/violenceprevention/acestudy/about.html. Accessed January 22, 2018.
- 10.Cheong E Von, Sinnott C, Dahly D, Kearney PM. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open . 2017;7:e013228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das De S, Vranceanu A-M, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am. 2013;95:76-81. [DOI] [PubMed] [Google Scholar]
- 12.Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. 2005;21:398-405. [DOI] [PubMed] [Google Scholar]
- 13.Denison E, Åsenlöf P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111:245-252. [DOI] [PubMed] [Google Scholar]
- 14.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA . 2001;286:3089-3096. [DOI] [PubMed] [Google Scholar]
- 15.Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med . 2003;37:268-277. [DOI] [PubMed] [Google Scholar]
- 16.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med . 1998;14:245-258. [DOI] [PubMed] [Google Scholar]
- 17.Fritz J, de Graaff AM, Caisley H, van Harmelen A-L, Wilkinson PO. A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Front Psychiatry . 2018;9:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hjemdal O, Vogel PA, Solem S, Hagen K, Stiles TC. The relationship between resilience and levels of anxiety, depression, and obsessive-compulsive symptoms in adolescents. Clin Psychol Psychother. 2011;18:314-321. [DOI] [PubMed] [Google Scholar]
- 20.Howell KH, Miller-Graff LE. Protective factors associated with resilient functioning in young adulthood after childhood exposure to violence. Child Abuse Negl. 2014;38:1985-1994. [DOI] [PubMed] [Google Scholar]
- 21.Kazeem OT. A validation of the adverse childhood experiences scale in Nigeria. Research on Humanities and Social Sciences. 2015;5:18-23. [Google Scholar]
- 22.Kersten P, White PJ, Tennant A. Is the pain visual analogue scale linear and responsive to change? An exploration using Rasch analysis. PLoS One. 2014;9:e99485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2. Med Care . 2003;41:1284-1292. [DOI] [PubMed] [Google Scholar]
- 24.LeBouthillier DM, Thibodeau MA, Alberts NM, Hadjistavropoulos HD, Asmundson GJG. Do people with and without medical conditions respond similarly to the Short Health Anxiety Inventory? An assessment of differential item functioning using item response theory. J Psychosom Res. 2015;78:384-390. [DOI] [PubMed] [Google Scholar]
- 25.Levenson JS, Willis GM, Prescott DS. Adverse childhood experiences in the lives of male sex offenders. Sex Abuse. 2016;28:340-359. [DOI] [PubMed] [Google Scholar]
- 26.Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58:163–171. [DOI] [PubMed] [Google Scholar]
- 27.Lozano-Calderon SA, Souer JS, Jupiter JB, Ring D. Psychological differences between patients that elect operative or nonoperative treatment for trapeziometacarpal joint arthrosis. Hand. 2008;3:271-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCrory C, Dooley C, Layte R, Kenny RA. The lasting legacy of childhood adversity for disease risk in later life. Health Psychol. 2015;34:687-696. [DOI] [PubMed] [Google Scholar]
- 29.Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychol Bull . 1991;110:406-425. [DOI] [PubMed] [Google Scholar]
- 30.Nota SPFT, Bot AGJ, Ring D, Kloen P. Disability and depression after orthopaedic trauma. Injury. 2015;46:207-212. [DOI] [PubMed] [Google Scholar]
- 31.Poole JC, Dobson KS, Pusch D. Childhood adversity and adult depression: the protective role of psychological resilience. Child Abuse Negl . 2017;64:89-100. [DOI] [PubMed] [Google Scholar]
- 32.Poole JC, Dobson KS, Pusch D. Anxiety among adults with a history of childhood adversity: psychological resilience moderates the indirect effect of emotion dysregulation. J Affect Disord. 2017;217:144-152. [DOI] [PubMed] [Google Scholar]
- 33.Ring D, Kadzielski J, Fabian L, Zurakowski D, Malhotra LR, Jupiter JB. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88:1983-1988. [DOI] [PubMed] [Google Scholar]
- 34.Ring D, Kadzielski J, Malhotra L, Lee S-GP, Jupiter JB. Psychological factors associated with idiopathic arm pain. J Bone Joint Surg Am. 2005;87:374-380. [DOI] [PubMed] [Google Scholar]
- 35.Salkovskis PM, Rimes KA, Warwick HMC, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. 2002;32:843-853. [DOI] [PubMed] [Google Scholar]
- 36.Schalet BD, Hays RD, Jensen SE, Beaumont JL, Fries JF, Cella D. Validity of PROMIS physical function measured in diverse clinical samples. J Clin Epidemiol. 2016;73:112-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sullivan M, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524-532. [Google Scholar]
- 38.Tunks ER, Crook J, Weir R. Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Can J Psychiatry . 2008;53:224-234. [DOI] [PubMed] [Google Scholar]
- 39.Vranceanu AM, Barsky A, Ring D. Psychosocial aspects of disabling musculoskeletal pain. J Bone Joint Surg Am. 2009;91:2014-2018. [DOI] [PubMed] [Google Scholar]
- 40.Vranceanu AM, Safren S, Zhao M, Cowan J, Ring D. Disability and psychologic distress in patients with nonspecific and specific arm pain. Clin Orthop Relat Res . 2008;466:2820-2826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walker EA, Keegan D, Gardner G, Sullivan M, Bernstein D, Katon WJ. Psychosocial factors in fibromyalgia compared with rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosom Med . 1997;59:572-577. [DOI] [PubMed] [Google Scholar]