Abstract
Background
Marijuana use has become more accessible since its recent legalization in several states. However, its use in a total joint arthroplasty population to our knowledge has not been reported, and the implications of its use in this setting remain unclear.
Questions/purposes
We report (1) the self-reported use of marijuana in patients undergoing total joint arthroplasty both before and after its legalization; and (2) clinical and demographic factors associated with marijuana use in patients undergoing total joint arthroplasty.
Methods
One thousand records of patients undergoing primary total joint arthroplasty (500 consecutive before and 500 consecutive after the legalization of the commercial sale of marijuana in Colorado) were included for analysis. Preoperative medical history and physicals were retrospectively reviewed for self-reported and reasons (medicinal versus recreational) for use. Additionally, patient records were used to determine insurance type, age, gender, smoking status, history of substance abuse, preoperative narcotic use, alcohol intake, and the type of arthroplasty performed.
Results
Self-reported use after legalization dramatically increased from 1% (four of 500) to 11% (55 of 500) (odds ratio [OR], 15.3 [95% confidence interval, 5.5–42.6]; p < 0.001) after legalization. For those reporting use after legalization, 46% (25 of 55) of patients reported recreational use, 26% (14 of 55) medicinal use, 27% (15 of 55) did not report a reason for use, and 2% (one of 55) reported both recreational and medicinal use. Factors associated with use included younger age (with a 10-year mean difference between the groups [p < 0.001]), male gender (36 of 59 users [61%] versus 411 of 941 nonusers [44%]; OR, 2.02; p < 0.01), current smokers (22 of 59 users [37%] versus 54 of 941 [6%] nonusers; OR, 0.09; p < 0.01), a history of substance abuse (eight of 59 users [14%] versus 18 of 941 nonusers [2%]; OR, 8.04; p < 0.001), insurance type (Medicaid only, 28 of 59 [48%] users versus 56 of 941 [6%] nonusers; OR, 20.45; p < 0.01), and preoperative narcotic use (eight of 59 users [14%] versus 17 of 941 nonusers [2%]; OR, 2.4; p < 0.001). We did not find differences with regard to alcohol use, amount of alcohol consumption, or insurance types other than Medicaid.
Conclusions
These results suggest the legalization of marijuana has led to either more users or more patients who are willing to report its use given the lack of legal ramifications. Despite these findings, the evidence to date precludes the use of marijuana postoperatively in patients undergoing total joint arthroplasty. Further investigation, ideally in a prospective randomized manner, should focus on opioid consumption, nausea, sleep patterns, and outcomes in patients using marijuana who are undergoing total joint arthroplasty before recommendations can be made for its use.
Level of Evidence
Level III, therapeutic study.
Introduction
The past few decades have seen an alarming increase of opioid use in the United States [10, 14, 15]. Despite widespread use of multimodal pain protocols, opioid consumption often is needed to obtain adequate pain management after total joint arthroplasty. The pre- and postoperative use of narcotic medications has been associated with an increase in morbidity and mortality after elective orthopaedic surgery [13, 14, 19]. This has led both patients and surgeons to seek alternative pain management options to limit potential narcotic-associated complications.
It is the authors’ impression that marijuana use has gained greater societal acceptance since its recent legalization in several states. Marijuana may function to reduce sensitization of the nociceptive sensory pathways and induce alterations in cognitive and autonomic processing in chronic pain conditions [6, 12]. Additionally, it may have a role in decreasing the inflammatory cascade [6, 18]. In Canada, severe arthritis was cited as the diagnosis for 65% of persons holding a Health Canada authorization to possess marijuana as of June 2013 [4, 20]. For these reasons, an interest in marijuana as a potential treatment or adjunct to treatment in musculoskeletal conditions has emerged in the orthopaedic community [2, 4–6, 20]. No studies to our knowledge have evaluated the number of patients undergoing total joint arthroplasty using marijuana for medicinal and/or recreational purposes. These data may be confounded by patients’ reluctance to self-report use to healthcare providers [7, 8, 11, 16, 17, 21].
Given the potential implications associated with perioperative marijuana use in orthopaedic surgery, we sought to report (1) the self-reported use of marijuana in patients undergoing total joint arthroplasty before and after its legalization; and (2) clinical and demographic factors associated with marijuana use in patients undergoing total joint arthroplasty.
Patients and Methods
This study was approved by our institutional review board before its initiation. Colorado Amendment 64 legalized marijuana in 2012 with the commercial sale of marijuana to the general public initiated January 1, 2014, at establishments licensed under the regulatory framework. We retrospectively evaluated outpatient office charts for self-reported use of marijuana before and after legalization of the commercial sale in Colorado. The study period was from March 2012 to November 2013 (prelegalization) and July 2015 to December 2016 (postlegalization). We elected to start our postlegalization cohort 1.5 years after the commercial sale of legalization to allow ample time for patient perception and attitudes toward marijuana to potentially change with regard to both medicinal and/or recreational use. Each cohort consisted of 500 consecutive patients (500 pre- and postlegalization) who underwent primary total joint arthroplasty at our institution. The sample size was based on convenience and resources at our institution. All patients in this cohort underwent a preoperative medical history and physical with our internal medicine physicians. Each patient had a drug screen (intake form and questioning by the physician) as part of the social history that is standard practice at our institution. No patients were excluded for incomplete medical records concerning drug use (ie, missing drug screening in the social history) in this review.
Before the legalization of marijuana, our patient intake form inquired about illicit drug use. After legalization, our intake forms were changed to reflect marijuana as a drug, but not as an illegal drug. Both cohorts had a review of their social history, which included a drug history screening with a discussion about marijuana at the discretion of our internal medicine team during their preoperative visit. Patient medical records were reviewed for self-reported marijuana use from these medical preoperative histories and physicals. When applicable, in patients who reported marijuana use, we attempted to determine the reason for use (recreational versus medicinal) from our chart review. No attempt was made to determine frequency or duration of use because these questions were not asked by our medical team at the time of this study. Route of administration (inhalation, edible, topical, combination [ie, inhalation + edible]) was documented when available. For patients in whom this information was unavailable, we listed the route of administration as “unknown.” Lastly, patient records were used to determine insurance type (as a surrogate for socioeconomic status), age, gender, smoking status, history of substance abuse, preoperative narcotic use, alcohol intake, and type of arthroplasty performed. All charts were reviewed by one of the authors (DLL) not involved in patient care.
Descriptive statistics were used to derive means and SDs for continuous variables as well as frequencies and percentages for categorical variables. The primary outcomes were examined using Pearson’s chi-square test. Odds ratios and confidence intervals were examined with a logistic regression analysis. Comparisons of group samples in our secondary analysis were evaluated with either Pearson’s chi square tests or two-sample t-tests. Statistical analysis was performed using Minitab 17 (State College, PA, USA). Probability values < 0.05 were considered statistically significant. We were unable to perform a multivariant analysis secondary to our small sample size.
Results
Self-reported marijuana use dramatically increased from 1% (four of 500) to 11% (55 of 500) (odds ratio [OR], 15.3 [95% confidence interval, 5.5–42.6]; p < 0.001) after legalization. Of the 59 users, 27 (46%) reported recreational use, 16 (26)% medicinal use, 15 (27%) did not report a reason for use, and one (2%) reported both recreational and medicinal use.
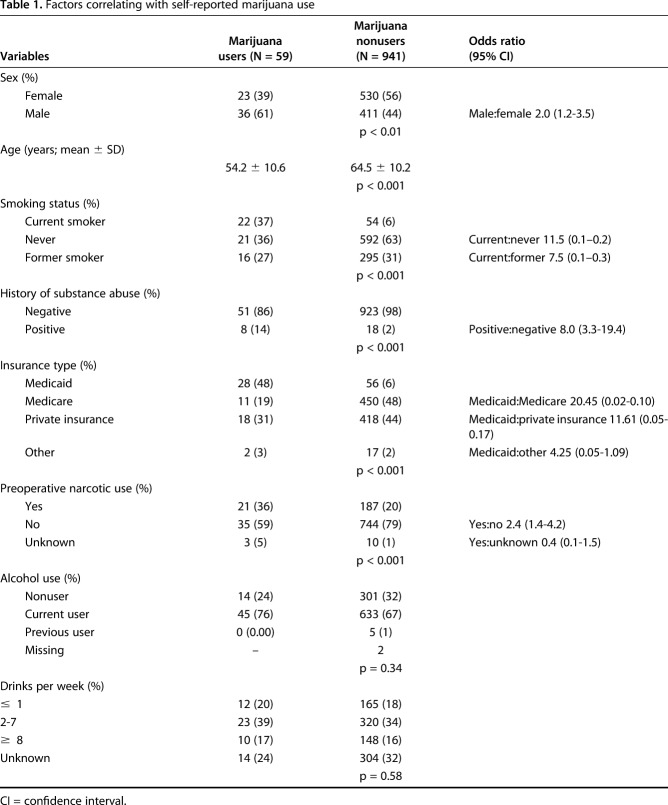
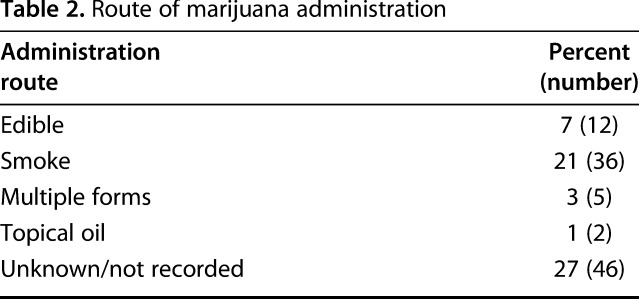
Younger patients, with a 10-year mean difference between the groups (54 ± 11 versus 65 ± 10 years, p < 0.001), were more likely to report marijuana use. Male gender (61% [36 of 59] users versus 44% [411 of 941]; OR, 2.02; p < 0.01), current tobacco smokers (37% [22 of 59] users versus 6% [54 of 941] nonusers; OR, 11.48; p < 0.01), a history of substance abuse (14% [eight of 59] users versus 2% [18 of 941] nonusers; OR, 8.04; p < 0.001), insurance type (Medicaid only, 48% [28 of 59] users versus 6% [56 of 941] nonusers; OR, 20.45; p < 0.01), and preoperative narcotic use (14% [eight of 59] users versus 2% [17 of 941] nonusers; OR, 2.4; p < 0.001) were also more likely to self-report use (Table 1). Alcohol use, the amount of alcohol consumed, and insurance types (other than Medicaid) were not associated with self-reported use of marijuana. Many modes of use were documented with inhalation being the most common reported route of administration (Table 2). We found no difference in the proportion of patients who self-reported marijuana use when comparing patients undergoing THA with those undergoing TKA.
Table 1.
Factors correlating with self-reported marijuana use
Table 2.
Route of marijuana administration
Discussion
Marijuana use may hold the potential as an adjuvant to pain management in patients with a variety of musculoskeletal disorders [1, 2, 4]. No studies to our knowledge have evaluated patients undergoing total joint arthroplasty using marijuana for medicinal and/or recreational purposes. Self-reported marijuana use dramatically increased from 1% to 11% after the legalization of the commercial sale in Colorado in this cohort of patients undergoing total joint arthroplasty. Nearly half of the patients who reported the type of use (ie, medicinal versus recreational) were recreational users. We sought to examine the implications of self-reported use of marijuana in patients undergoing total joint arthroplasty both before and after its legalization and the clinical and demographic factors associated with its use.
This study is not without limitations. We concede that assessment bias may exist. Drug use during the prelegalization period on our intake form was listed as illegal and there was not a specific focus on marijuana. Our history intake form changed at our institution after the legalization of the commercial sale of marijuana (to reflect marijuana as a legal drug), which may have encouraged some patients into disclosing its use in contrast to the time period when such use was listed as illicit. Additionally, our internal medicine providers may have probed further regarding details of marijuana use after legalization. Lastly, the mere fact that marijuana was legalized may have led many patients to self-report use without fear of legal consequences. These factors would tend to result in an underestimation of use before legalization. Furthermore, the author (DLL) conducting the chart review was not blinded to pre- and postlegalization status of the cohorts, which might have led to an inherent bias to look for evidence of use in the postlegalization group. We were unable to determine if patients were using marijuana for medical or recreational purposes in nearly half of the patients in this cohort and therefore the true motive for its use remains unknown for many of these patients. However, several studies have demonstrated a significant overlap between medicinal and recreational users with previous recreational marijuana use reported by many current medicinal users, which blurs the distinction between the reason for use in many patients [1, 20]. We also did not have documentation regarding the frequency, dosage, or duration of its use. These are important factors that future studies should investigate. The severity of degenerative disease symptoms or patient-perceived pain was not explored in this study, which has been shown to be associated with marijuana use in a rheumatologic population [20]. This study is also limited because a multivariate analysis based on confounding variables could not be performed given the nature of this retrospective design and small sample size. Additionally, insurance type was used as a surrogate for socioeconomic status; more information of this nature in this population should be an area of interest for future studies. Lastly, we were unable to correlate marijuana use and the amount of opioid consumption before and after surgical intervention.
Our data suggest that > 10% of the population undergoing total joint arthroplasty in our Colorado practice use marijuana and almost half of the patients in this cohort report marijuana use for recreational purposes. We believe the prevalence may be higher based on previous underreporting of drug and alcohol use in other studies [7, 8, 11, 16, 17, 21]. Additionally, the true distinction between medicinal and/or recreational use remains challenging because there seems to be significant overlap with regard to the reason for use [1, 20]. Alternatively, the decision to use medicinal marijuana may be secondary to familiarity of the product by recreational users. The role of marijuana in this patient population has yet to be defined with scientific studies to support its use as an adjuvant to many treatments after total joint arthroplasty (ie, opioid consumption, nausea control); however, surgeons should be aware that their patients may be currently using marijuana for medicinal and/or recreational purposes with or without reported use. Future studies should focus on the efficacy of marijuana use, particularly with regard to opioid consumption, and we are currently investigating this area in a prospective study at our institution.
Males, younger age, current smokers, socioeconomic status (Medicaid insurance), and patients with a history of substance abuse and/or preoperative narcotic use were more likely to use marijuana. These findings are similar to those reported in patients with rheumatologic conditions who were more likely to be younger males, current smokers, reported more opioid use, and were more likely to be unemployed or disabled [20]. These data provide orthopaedic surgeons clinical and demographic factors of patients more likely to self-report use of marijuana in our Colorado practice, but this may not be relevant to other geographic regions. Further investigation is warranted to determine the association between marijuana use and its potential relationship with demographic factors associated with a decrease in reported outcomes after total joint arthroplasty (ie, preoperative narcotic use, smokers, substance abuse).
There is a lack of education among healthcare providers regarding the mechanisms and clinical utility of marijuana use, which will continue to be an obstacle until further studies are performed. A recent study revealed rheumatologists prescribe but lack knowledge with regard to medicinal marijuana [5]. A systematic review of randomized controlled trials showed insufficient evidence on the recommendation of any cannabinoid preparation for symptom management in patients with chronic pain associated with rheumatic diseases [6]. However, these preparations may be superior to placebo in reducing chronic neuropathic-related pain [3, 9]. Overall, the use of marijuana appears to be well tolerated; however, side effects such as fatigue, dizziness, and dry mouth are commonly reported [6]. Severe side effects seem rare, but reports of cardiovascular compromise in patients with underlying heart disease and acute psychiatric effects such as psychosis have been noted [4]. To date there have been no randomized controlled trials in patients with osteoarthritis. As such, the authors believe many orthopaedic surgeons remain relatively uninformed about marijuana use in their patients despite an increased interest in this population.
In conclusion, the legalization of the commercial sale of marijuana in Colorado has led to either more users or more patients willing to self-report use given the lack of legal ramifications. To date, there remains a paucity of scientific evidence to adopt the use of medicinal marijuana for many conditions. If a clear benefit can be proven with respect to pain management, there may be potential to help stem the opioid epidemic. However, marijuana use is not innocuous and any synergistic effects and safety in combination with opioids and other medications must be explored before recommendations can be made for its perioperative use in orthopaedic surgery. Surgeons should develop an increased understanding of both medicinal and recreational marijuana use to allow for appropriate education of patients who may inquire about its use in the postoperative period. Further investigation, ideally in a prospective manner, should focus on opioid consumption, nausea, sleep patterns, and outcomes in patients using marijuana who are undergoing total joint arthroplasty.
Footnotes
One of the authors (DAD) has or may receive payments or benefits from DePuy (Warsaw, IN, USA), Innomed (Savannah, GA, USA), Joint Vue (Columbus, OH, USA), and Wolters Kluwer Health (Philadelphia, PA, USA) not related to this work. One of the authors (JMJ) has or may receive payments or benefits from DePuy, Total Joint Orthopedics (Salt Lake City, UT, USA), and Xenex (San Antonio, TX, USA) not related to this work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Colorado Joint Replacement, Denver, CO, USA.
References
- 1.Ablin J, Ste-Marie PA, Schafer M, Hauser W, Fitzcharles M-A. Medical use of cannabis products: lessons to be learned from Israel and Canada. Schmerz. 2016;30:3–13. [DOI] [PubMed] [Google Scholar]
- 2.Boehnke KF, Litinas E, Clauw DJ. Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain. 2016;17:739–744. [DOI] [PubMed] [Google Scholar]
- 3.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpää M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice ASC, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14:162–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fitzcharles M-A, Baerwald C, Ablin J, Häuser W. Efficacy, tolerability and safety of cannabinoids in chronic pain associated with rheumatic diseases (fibromyalgia syndrome, back pain, osteoarthritis, rheumatoid arthritis). Der Schmerz. 2016:47–61. [DOI] [PubMed] [Google Scholar]
- 5.Fitzcharles M-A, Häuser W. Cannabinoids in the management of musculoskeletal or rheumatic diseases. Curr Rheumatol Rep. 2016;18:76. [DOI] [PubMed] [Google Scholar]
- 6.Fitzcharles M-A, Ste-Marie PA, Clauw DJ, Jamal S, Karsh J, LeClercq S, McDougall JJ, Shir Y, Shojania K, Walsh Z. Rheumatologists lack confidence in their knowledge of cannabinoids pertaining to the management of rheumatic complaints. BMC Musculoskelet Disord. 2014;15:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghitza UE, Epstein DH, Preston KL. Nonreporting of cannabis use: predictors and relationship to treatment outcome in methadone maintained patients. Addict. Behav. 2007;32:938–949.16887281 [Google Scholar]
- 8.Glintborg B, Olsen L, Poulsen H, Linnet K, Dalhoff K. Reliability of self-reported use of amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone, and opiates among acutely hospitalized elderly medical patients. Clin Toxicol (Phila). 2008;46:239–242. [DOI] [PubMed] [Google Scholar]
- 9.Ko GD, Bober SL, Mindra S, Moreau JM. Medical cannabis—the Canadian perspective. J Pain Res. 2016;9:735–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leopold SS, Beadling L. Editorial: The opioid epidemic and orthopaedic surgery—no pain, who gains? Clin Orthop Relat Res. 2017;475:2351–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Livingston M, Callinan S. Underreporting in alcohol surveys: whose drinking is underestimated? J Stud Alcohol Drugs. 2015;76:158–164. [PubMed] [Google Scholar]
- 12.Marzo V Di, Bifulco M, Petrocellis L De. The endocannabinoid system and its therapeutic exploitation. Nat Rev Drug Discov. 2004;3:771–784. [DOI] [PubMed] [Google Scholar]
- 13.Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res. 2015;473:2402–2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris B. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015;23:267–271. [DOI] [PubMed] [Google Scholar]
- 15.O’Neal RM, Cryer KA, Edwards PK, Barnes CL, Mears SC. Narcotic use: a modifiable risk factor for hip and knee arthroplasty. J Surg Orthop Adv. 2016;25:227–233. [PubMed] [Google Scholar]
- 16.Palamar JJ, Martins SS, Su MK, Ompad DC. Self-reported use of novel psychoactive substances in a US nationally representative survey: Prevalence, correlates, and a call for new survey methods to prevent underreporting. Drug Alcohol Depend. 2015;156:112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Polich JM. The validity of self-reports in alcoholism research. Addict Behav. 1982;7:123–132. [DOI] [PubMed] [Google Scholar]
- 18.Richardson D, Pearson RG, Kurian N, Latif ML, Garle MJ, Barrett DA, Kendall DA, Scammell BE, Reeve AJ, Chapman V. Characterisation of the cannabinoid receptor system in synovial tissue and fluid in patients with osteoarthritis and rheumatoid arthritis. Arthritis Res Ther. 2008;10:R43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee G-C. Preoperative opiate use independently predicts narcotic consumption and complications after total joint arthroplasty. J Arthroplasty. 2017;32:2658–2662. [DOI] [PubMed] [Google Scholar]
- 20.Ste-Marie PA, Shir Y, Rampakakis E, Sampalis JS, Karellis A, Cohen M, Starr M, Ware MA, Fitzcharles M-A. Survey of herbal cannabis (marijuana) use in rheumatology clinic attenders with a rheumatologist confirmed diagnosis. Pain. 2016;157:2792–2797. [DOI] [PubMed] [Google Scholar]
- 21.Yacoubian GS, VanderWall KL, Johnson RJ, Urbach BJ, Peters RJ. Comparing the validity of self-reported recent drug use between adult and juvenile arrestees. J Psychoactive Drugs. 2003;35:279–284. [DOI] [PubMed] [Google Scholar]