Abstract
Background and Objectives:
Given the dynamic nursing home (NH) industry and evolving regulatory environment, depiction of contemporary NH culture-change (person/resident-centered) care practice is of interest. Thus, we aimed to portray the 2016/17 prevalence of NH culture change-related processes and structures and to identify factors associated with greater practice prevalence.
Research Design and Methods:
We administered a nationwide survey to 2,142 NH Administrators (NHA) at NHs previously responding to a 2009/10 survey. Seventy-four percent of administrators (1,583) responded (with no detectable non-response bias) enabling us to generalize (weighted) findings to US NHs. From responses, we created index scores for practice domains of resident-centered care, staff empowerment, physical environment, leadership, and family and community engagement. Facility-level covariate data came from the survey and the Certification and Survey Provider Enhanced Reporting system. Ordered logistic regression identified the factors associated with higher index scores.
Results:
Eighty-eight percent of administrators reported some facility-level involvement in NH culture change, with higher reported involvement consistently associated with higher domain index scores. NHs performed the best (82.6 /100 weighted points) on the standardized resident-centered care practices index, and had the lowest scores (54.8) on the family and community engagement index. Multivariable results indicate higher index scores in NHs with higher leadership scores and in states having Medicaid pay-for-performance with culture change-related quality measures.
Conclusion:
The relatively higher resident-centered care scores (compared to other domain scores) suggest an emphasis on person-centered care in many US NHs. Findings also support pay-for-performance as a potential mechanism to incentivize preferred NH practice.
Keywords: nursing home staffing, Medicaid reimbursement, person-centered care, nursing home leadership, nursing home turnover, culture change
INTRODUCTION
Efforts to enhance the quality of care and life in nursing homes (NHs) are long-standing, with varying success.(1) Given the challenging and complex regulatory and reimbursement environments in which NHs operate and the diversity of services provided, fundamental change that systematically addresses the structure and functioning of a NH (rather than change targeted to improve specific outcomes) is likely needed to achieve sustained quality improvement. The US NH culture change movement promotes such systematic change through its efforts aimed at advancing person-centered care and deinstitutionalizing NHs; and, the Pioneer Network and national NH associations have supported and promoted these efforts.(2, 3) Culture change-related practices align with the 2016 NH Medicare/Medicaid regulatory changes mandating person-centered care in NHs(4) and with the person-centered care directive of the Patient Protection and Affordable Care Act (ACA).(5)
Critical culture change practices encompass resident-centered care, physical environmental practices aimed at making NHs less institutional and more homelike, and workplace (i.e., staff empowerment) practices intended to empower staff. Additionally, central to culture change efforts are NH leadership practices to ensure leaders model and enable culture change, and family and community engagement practices designed to enable inclusion and involvement of family and community.(6) While more rigorous research supporting the efficacy of culture change transformation is needed,(7, 8) panel studies have found NH culture change adoption is associated with reductions in Medicare/Medicaid survey deficiencies, decreases in the prevalence of feeding tubes, restraints and pressure ulcers, and higher resident satisfaction with the quality-of-care and quality-of-life.(9–11)
Higher-tier NHs (i.e., those with greater financial resources and higher quality outcomes)(12) appear to have been early adopters of culture change transformation.(13, 14) In comparing NHs identified as “culture change providers” to non-identified NHs, Grabowski and colleagues(13) found culture change providers were more often nonprofit and affiliated with continuing care retirement communities (CCRCs), had more private-pay residents, higher nurse aide staffing rates, and fewer healthcare survey deficiencies. Additionally, this study and another(15) found higher adoption was associated with NHs being in states with higher Medicaid rates and with pay-for-performance (p4p) reimbursement programs that included culture change quality measures. Such programs may help to “level the playing field” by financially assisting lower-resourced NHs in their implementation efforts. In fact, a study of culture change adoption in Kansas (that has such a Medicaid p4p program) found that over time the p4p program was successful in expanding culture change adoption to NHs more representative of the states’ NHs as a whole, compared to the Kansas’ early adopters that were disproportionately higher-tier NHs.(14)
The last national snapshot of culture change practice adoption was provided through a 2009/10 national survey, when 85% of respondents reported some NH culture change practice implementation,(15) a substantial increase from a 2007 national survey when only 56% of respondents reported any implementation or leadership commitment to culture change practice.(16) Still, in 2009/10, only 13% of respondents reported that culture change transformation had “completely changed the way they care for residents” and 15% reported no practice adoption (considered “traditional” NHs).(15)
The research presented here updates this information for 2016/17 in the wake of the 2010 ACA legislation and the 2016 Medicare/Medicaid NH regulations.(4, 5) Using nationally representative NH survey data linked to other NH-, county-, and state-level information, we examine characteristics associated with greater practice implementation. Of particular interest is whether NHs with greater culture change practice implementation still represent higher tier NHs, (12–14, 17) and whether Medicaid p4p programs continue to be associated with greater practice implementation.(13, 15)
METHODS
Conceptual Framework
NHs are complex adaptive systems facing turbulent and chaotic regulatory and payment environments where diverse staff provide care to often highly diverse residents. Ecological models are often used to portray how factors at multiple levels (e.g., patient, provider, community and policy) are influence behavior or care.(18) Therefore, using an ecological framework we examined the multiple levels of influence and associations between culture change indices and NH characteristics, NH leadership, county (market) characteristics, and reimbursement and regulatory environments. As noted, we included the leadership index score as an explanatory variable influencing culture change adoption, rather than an outcome.
Survey Instrument
We refer to the survey’s measurement focus as “culture change” since this term is commonly used to describe this ongoing transformation in NHs; however, the survey focused on the processes and structures promoting person-centered care and deinstitutionalization of NHs.(3, 7) Our measurement was driven by the Holistic Approach to Transformational Change (HATCh) model that depicts six interrelated domains needed for NHs to make the transformational change from institutional to individualized care.(6) Using the five HATCh domain practices, we measured resident-centered care, staff-empowerment, physical environment, leadership and family and community engagement practices. We used other secondary data sources to quantify the sixth HATCh domain of government and regulations.
The data used in this study come from a 2016/2017 follow-up survey of Nursing Home Administrators (NHAs) from facilities that responded to a survey administered in 2009/10 to a stratified, proportionate random sample of NHs.(15) It is part of a larger panel study aimed at identifying NH practice change and how change may be associated with quality outcomes. In 2016/17, the culture change survey had an increased number of survey items included for the domains of physical environment, resident-centered care and staff empowerment, and new survey items for the leadership and family and community engagement domains (see Addendum Text, Supplemental Digital Content 1). We conceptualized and analyzed the five domains as representing composite variables-- indices reflective of each domain’s practice--rather than underlying latent variables (i.e., constructs).(19) The XXXX University Institutional Review Board reviewed and approved the study; however, it did not consider the qualitative interviews and survey to be human subjects research since we asked no personal questions of respondents.
While the 2009/10 survey included responses from both the NHA and Director of Nursing (DON) at each facility,(15) budget constraints allowed for only one survey per facility in 2016/2017. NHAs were chosen over DON respondents because our previous qualitative research showed administrators capable of answering culture change (care) practice questions,(20, 21) and more importantly, because our analyses of cognitive interviews of DONs and NHAs at the same NHs revealed NHAs to be the more credible respondents.(22)
An expert advisory committee assisted us in identifying and choosing survey items, and ensuring the survey’s content validity. Committee members included two NH researchers and leaders from the two national NH associations (American Health Care Association and LeadingAge) and culture change leadership from The Eden Alternative, Inc.,(23) CCAL: Advancing Person-Centered Living,(24) the National Cooperative Bank (25) and the Pioneer Network.(26) All relevant items from the 2009/10 questionnaire were included in the 2016/17 instrument. Also, we identified additional candidate survey items from existing culture change instruments/criteria, including the Commonwealth survey,(16) Artifacts of Culture Change(27) and Kansas PEAK 2.0 criteria.(28)
Cognitive interviews were conducted during the survey design process to reduce measurement error and increase data validity.(29, 30) Using the most recent Certification and Survey Provider Enhanced Reporting (CASPER) data (in the 2014 CASPER file), we randomly selected 15 NHs originally surveyed in 2009/10 that varied in terms of size, profit status, chain membership and hospital affiliation. Structured cognitive interviewing with follow-up probing was used.(29) Additional information about the cognitive interviews is available in Shield et al.(22) See Survey Instrument, Supplemental Digital Content 2 for the final survey instrument.
Survey Administration and Sample
The survey was administered to NHAs at 2,142 eligible facilities. (i.e., facility still in business) from our initial sample of 2,165 (the 2009/10 nationally-representative sample based on NHA respondents). Administrators were given the option of web, mail or telephone completion (see Addendum Text, Supplemental Digital Content 1). We received survey responses from 1,584 administrators for a response rate of 73.9%. Of the completed surveys, 55.9% were completed by web, 39.6% by mail, and 4.5% by telephone.
The sample was stratified into 19 groups based on the number of facilities in a state, owner type, bed size, and percent of nonwhite residents. We conducted analyses to assess potential non-response bias and concluded that we did not have evidence of detectable non-response bias requiring the use of additional post-stratification adjusted weighting beyond the stratum-specific, non-response adjusted weight (see Addendum Text, Supplemental Digital Content 1).
Variables of Interest and Other Data Sources
Overall Culture Change
Overall participation in culture change was assessed using responses to the survey question, “Please indicate your nursing home’s involvement in culture change or resident-centered care now.” NHs were characterized as traditional (those that had no discussion, or discussion and no action regarding culture change), strivers (those that reported culture change has partially changed the way they care for residents), complete adopters in some areas of the facility, and complete adopters in all areas of the facility.
Culture Change Domain Practices
Five unique culture change practice domain indices were created using survey data. The physical environment index included 12 items; the resident-centered care index 9 items; the staff empowerment index 13 items; the family and community engagement index 5 items; and, the leadership index 10 items. The survey items, the weighted responses to these items and the points assigned to response categories are shown in Weighted Distribution of Survey Items, Supplemental Digital Content 3.
To create each index score, we summed the values corresponding to each domain item response. Higher scores were reflective of more culture change practices being in place within a given domain. When survey items within a domain were missing, we imputed missing values for a NH when at least 60% of the domain items (e.g., 6 of 10 items for the leadership index) were completed; otherwise, index scores were reported as missing. For imputation, we first determined the mean point value for the completed items and then imputed this mean for the missing values. Imputations were performed for 34 to 187 NHs per index.
Covariates
Roger’s Diffusion of Innovation (DOI) theory(17) together with previous findings from related research(13–15) drove the inclusion of covariates likely to be associated with greater (versus lesser) culture change practice implementation (see Table 1). Multivariable models included facility-level characteristics related to ownership, structure, staffing and patient mix; the survey score reflecting a NH’s leadership practices; county-level variables on NH competition, rurality and geographic region; and, Medicaid payment policies (see Table 1).
Table 1:
NH Characteristics Included in Ordered Logit Models
| Variable | Coding | Data Source |
|---|---|---|
| For Profit | Yes/No | 2015 CASPER Survey |
| Bed Count | <80, 80–120, >120 | 2015 CASPER Survey |
| Occupancy Rate | Number of occupied beds/total number of beds Converted to 5 point increments regression model |
2015 CASPER Survey |
| Part of Chain | Yes/No | 2015 CASPER Survey |
| Religious Affiliation | Yes/No | 2015 CASPER Survey |
| Continuing Care Retirement Community |
Yes/No Yes indicates answered “Yes” to “Is your facility part of a Continuing Care Retirement Community?” or answered “No,” but indicated they have long- term care beds, assisted living residences, and independent living residences. |
2016/2017 NH CC Survey |
| Any Special Care Unit | Yes/No, Ventilator units not included | 2015 CASPER Survey |
| Directors of Nursing in Past Two Years |
One, Two, Three or More | 2016/2017 NH CC Survey |
| Administrators in Past Two Years |
One, Two, Three or More | 2016/2017 NH CC Survey |
| RN Hours per Resident Day |
Number of RN hours / number of residents in the facility Standardized in regression model |
2015 CASPER Survey |
| LPN Hours per Resident Day |
Number of LPN hours / number of residents in the facility Standardized in regression model |
2015 CASPER Survey |
| CNA Hours per Resident Day |
Number of RN hours / number of residents in the facility Standardized in regression model |
2015 CASPER Survey |
| State Pay for Performance |
No/Yes- without culture change measures/Yes with culture change measures |
MACPAC report and review of Medicaid websites |
| 2009 Medicaid Reimbursement Rate |
Dollars per resident day Converted to $10 increments in regression model |
2011 Medicaid Policy Survey |
| County Level Hirschman-Herfindahl Competition Index |
Based on # of NHs and beds in county; 0–1 (high to low); categorized into four quartiles in regression model |
2015 CASPER Survey |
| Located in a metropolitan county |
Yes/No | 2015 CASPER Survey |
| Census Sub-Region | 9 Sub-Regions: West North Central, West South Central, East North Central, East South Central, Middle Atlantic, Mountain New England, Pacific, South Atlantic |
2015 CASPER Survey |
| Percent of Residents who are Black |
Proportion, Categorized to lowest decile, below median, above median, top decile in regression model |
2015 LTCfocus |
| Percent of Residents who are Hispanic |
Proportion, Categorized to below median, above median, top decile in regression model |
2015 LTCfocus |
| Percent of Residents with Medicare |
Proportion with Medicare as primary payer, Categorized to lowest decile, below median, above median, top decile in regression model |
2015 LTCfocus |
| Percent of Residents with Medicaid |
Proportion with Medicaid as primary payer, Categorized to lowest decile, below median, above median, top decile in regression model |
2015 LTCfocus |
| Average Age of Residents |
Years | 2015 LTCfocus |
| Average RUGS NCMI (Prevalence) |
Average Resource Utilization Group Nursing Case Mix Index for all residents in the facility on the 1st Thursday in April Standardized in regression model |
2015 LTCfocus |
| Average Activities of Daily Living Score (Prevalence) |
Average Activities of Daily Living Score for all residents in the facility on the 1st Thursday in April Standardized in regression model |
2015 LTCfocus |
| Percent of Residents with High Cognitive Function Score (Prevalence) |
Percent of residents in the facility on the 1st Thursday in April with a cognitive function score of 4 (severe cognitive impairment) Converted to 10 percentage point increments in regression model |
2015 LTCfocus |
1. RN = Registered Nursing, LPN = Licensed Practical Nurse, CNA = Certified Nursing Assistant
NH survey data were merged with facility-level variables derived from the most recent CASPER data (2015) and resident case-mix variables were constructed from Medicare MDS, enrollment, and claims data covered under a CMS Data Use Agreement for this study, and modeled after variables found in the Long-Term Care Facts on Care in the United States (LTCfocUS) dataset.(31)
We obtained state Medicaid payment reimbursement rates from a 2011 policy survey conducted by Brown University. While we were unable to identify recent Medicaid rate data, the relative rate differences are likely to be similar over time. We determined whether states had Medicaid NH p4p programs and whether these programs included culture change-related quality indicators using a publicly available report compiled by the Medicaid and CHIP Payment and Access Commission.(32) These data were confirmed via website reviews and in some cases correspondence with state culture change leaders. Leadership index scores, DON and NHA tenure/turnover and whether a NH was part of a CCRC were obtained from the survey. (See “Weighted Descriptive Statistics for the 1,584 Nursing Homes that Completed the 2016–2017 Culture Change Survey,” Supplemental Digital Content 4 and “2014 Medicaid Pay for Performance Programs,” Supplemental Digital Content 5).
Statistical Analysis
Weighted and unweighted descriptive statistics described survey responses, and we calculated standardized means to better enable comparisons across domain index scores. We applied probability weights to adjust for the stratified sampling design. Given the ordinal nature of our survey data we used the psych package in R 3.2.3,(33) to calculate McDonald’s omega total for each domain.(34, 35) The omega totals reflect the internal consistency of a domain’s items--the maximum amount of variance explained by the items. We computed omega totals based on tetrachoric correlations for the indices derived from dichotomous variables, and polychoric correlations for the indices derived from ordinal variables.
We used ordered logistic regression to examine the associations between the covariates and outcomes of interest (a one quartile increase in a particular index score). These models account for the ordered nature of the data to produce coefficients that reflect the log-odds of a one-quartile increase in each domain index score (our outcomes) that is associated with a one-unit increase in each of the (specified) covariates. Prior to using this modeling approach, we examined likelihood ratios and Brant tests to confirm that the data met the proportional-odds assumption (i.e., the assumption that the relationship between each pair of outcome groups is the same). All models were adjusted by probability weights and confidence intervals were clustered by states. Also, we tested for profit status interactions and found no statistically significant interactions. All analyses (excluding McDonald’s Omegas) were conducted using Stata 14. For information on model n’s and missing data, (see Missing Data for Ordered Regression Analyses, Supplemental Digital Content 6).
RESULTS
NH Involvement in Culture Change
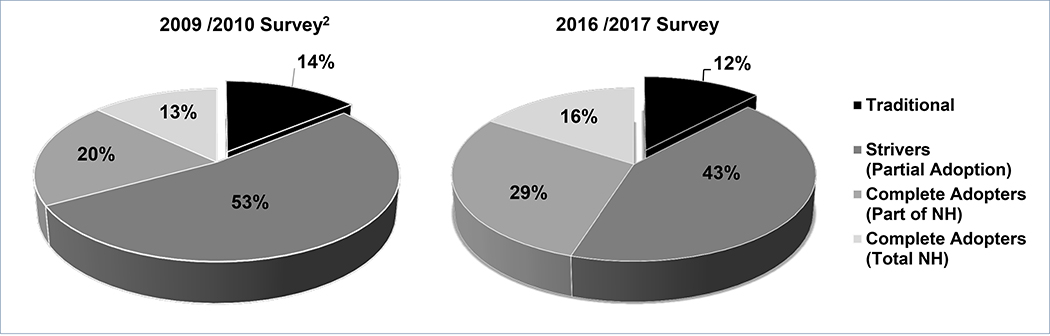
Figure 1 compares reported involvement in culture change in 2009/10 and 2016/17 for those NHs with responses to this question at both times (n=1,155). In 2016/17 fewer NHAs reported no or partial culture change involvement and more reported complete involvement (in part or all of the NH). In 2016/17, 88% of NHA respondents reported being at least partially involved in NH culture change and 16% reported culture change had “completely changed the way they care for residents” in all areas of the NH.
Figure 1: Reported Involvement in Culture Change Over Time for 1,155 NHs1.
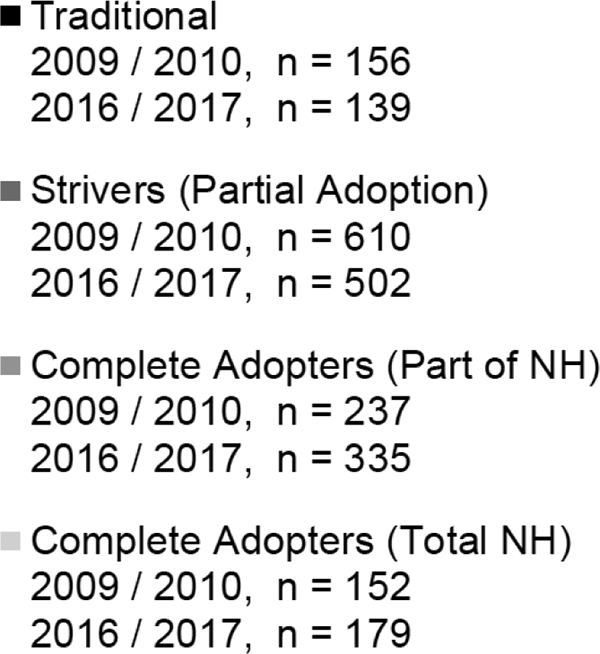
1. Only NHs with a response to the overall culture change question for both the 2009/10 and 2016/17 surveys are included in the figure.
2. More information about the 2009 /2010 NH culture change survey and results, is available in the Miller 2014.15
Culture Change Indices
As displayed in Table 2, resident-centered care practices had the highest standardized weighted mean index score (82.6 of 100) followed by physical environment practices (74.6 of 100). At 54.8, the domain representing family and community engagement practices had the lowest standardized index score.
Table 2:
Nursing Home Performance on Culture Change Indexes (2016–2017)
| Index | n | Total Possible Score |
Range of Scores (Unweighted) |
Weighted Mean (SE) | Standardized Mean (Weighted) |
Omega Total |
|---|---|---|---|---|---|---|
| Physical Environment | 1,460 | 24 | 14–24 | 17.91 (0.52) | 74.58 | 0.81 |
| Resident-Centered Care | 1,477 | 18 | 9–18 | 14.86 (0.05) | 82.56 | 0.87 |
| Staff Empowerment | 1,423 | 39 | 14–38 | 23.58 (0.12) | 60.46 | 0.86 |
| Staff Leadership | 1,407 | 30 | 11–30 | 18.27 (0.10) | 60.90 | 0.83 |
| Family and Community Engagement |
1,474 | 27 | 9–27 | 14.80 (0.10) | 54.81 | 0.91 |
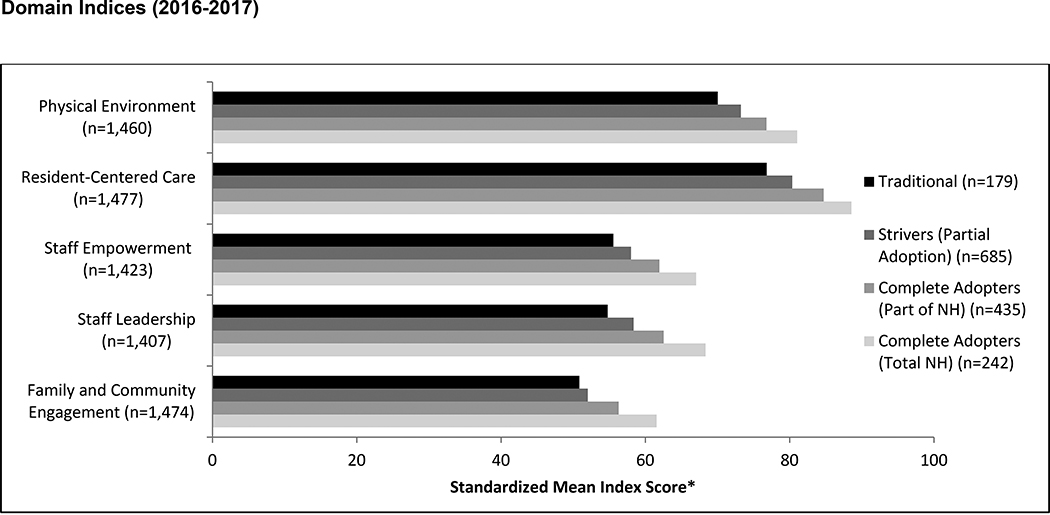
The indices had high internal consistency, with Omega totals ranging from 0.81 for physical environment practices to 0.91 for family and community engagement practices. Figure 2 shows consistently higher index scores across domains as the amount of reported culture change involvement increased, supporting the construct validity of the index scores (see Addendum Text, Supplemental Digital Content 1).
Figure 2: Reported Involvement in Culture Change and Performance on Culture Change.
*All Scores have been standardized to 100 point scales. The raw maximum possible scores vary by index.
Multivariable Adjusted Results
In ordered logistic regression analyses, the associations between covariates and index score outcomes varied by the domain index score being modeled. It is worth noting, however, that, compared to NHs in states without p4p programs, NHs in states with Medicaid p4p programs with culture change-related quality measures had a greater likelihood (adjusted odds ratios (AOR) ranging from 1.7 to 1.8) of being in a higher quartile for the physical environment, resident-centered care and staff empowerment indices (Table 3). Also, a 3-point increase in the leadership index score was associated with higher odds of being in a higher index quartile across the other four domains (AOR ranging from 1.7 to 3.7) (Table 3).
Table 3:
Facility Level Characteristics and Performance on Culture Change Indices, Ordered Logit Models
| Physical Environment1 | Resident Centered Care1 | Staff Empowerment1 | Family and Community1 | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Nursing Home Structure and Staffing | ||||
| For Profit | 0.640*** | 0.950 | 0.997 | 0.990 |
| (0.493 – 0.830) | (0.737 – 1.223) | (0.759 – 1.310) | (0.805 – 1.217) | |
| Bed Count | ||||
| <80 | Ref | Ref | Ref | Ref |
| 80–120 | 1.117 | 1.227 | 1.060 | 0.951 |
| (0.851 – 1.468) | (0.902 – 1.669) | (0.795 – 1.414) | (0.750 – 1.206) | |
| >120 | 1.328*** | 1.195 | 0.964 | 0.945 |
| (1.074 – 1.643) | (0.866 – 1.648) | (0.709 – 1.310) | (0.699 – 1.277) | |
|
Occupancy Rate (5 Point Increase) |
1.061*** | 1.044* | 1.007 | 1.020 |
| (1.021 – 1.104) | (0.999 – 1.090) | (0.971 – 1.045) | (0.977 – 1.065) | |
| Part of a Chain | 0.986 | 1.054 | 0.819** | 0.801* |
| (0.752 – 1.292) | (0.835 – 1.329) | (0.681 – 0.984) | (0.642 – 1.000) | |
| Religious Affiliation | 1.321 | 0.858 | 1.023 | 0.762 |
| (0.747 – 2.336) | (0.556 – 1.325) | (0.519 – 2.015) | (0.429 – 1.354) | |
| Continuing Care | 1.987*** | 1.182 | 0.926 | 0.978 |
| Retirement Community2 | (1.596 – 2.474) | (0.840 – 1.665) | (0.662 – 1.294) | (0.757 – 1.263) |
| Any Special Unit | 0.892 | 1.172 | 0.885 | 0.816 |
| (Except Ventilator Unit) | (0.681 – 1.168) | (0.866 – 1.586) | (0.683 – 1.146) | (0.604 – 1.103) |
| Directors of Nursing in Past Two Years | ||||
| One | Ref | Ref | Ref | Ref |
| Two or More | 0.753** | 0.741** | 0.976 | 0.909 |
| (0.605 – 0.937) | (0.561 – 0.978) | (0.719 – 1.324) | (0.728 – 1.133) | |
| Administrators in Past Two Years | ||||
| One | Ref | Ref | Ref | Ref |
| Two or More | 1.021 | 0.986 | 0.851 | 1.096 |
| (0.777 – 1.340) | (0.746 – 1.304) | (0.694 – 1.044) | (0.849 – 1.415) | |
| RN3 Hours / Resident | 1.089 | 1.042 | 0.876** | 0.894** |
| Day (Standardized) | (0.976 – 1.216) | (0.926 – 1.173) | (0.781 – 0.984) | (0.802 – 0.997) |
|
LPN3 Hours/Resident Day (Standardized) |
1.124* | 0.990 | 0.938 | 1.011 |
| (0.995 – 1.270) | (0.855 – 1.146) | (0.824 – 1.068) | (0.911 – 1.121) | |
|
CNA2 Hours/Resident Day (Standardized) |
1.060 | 1.132 | 1.157* | 1.066 |
| (0.951 – 1.181) | (0.973 – 1.316) | (0.983 – 1.363) | (0.941 – 1.207) | |
| Leadership Score | 1.693*** | 1.834*** | 3.650*** | 2.684*** |
| (3 Point Increase) | (1.525 – 1.880) | (1.676 – 2.007) | (3.328 – 4.003) | (2.405 – 2.995) |
| State Policy and Regional Characteristics | ||||
| State Pay for Performance (2014) | ||||
| No | Ref | Ref | Ref | Ref |
| Yes: No CC3 Measures | 0.780 | 0.827* | 0.994 | 1.605*** |
| (0.570 – 1.068) | (0.670 – 1.020) | (0.795 – 1.243) | (1.251 – 2.058) | |
| Yes: With CC3 Measures | 1.817*** | 1.718*** | 1.761*** | 1.206 |
| (1.307 – 2.528) | (1.246 – 2.369) | (1.369 – 2.266) | (0.789 – 1.843) | |
| Medicaid Rate | 1.009*** | 0.997 | 1.002 | 1.000 |
| ($10 increase) | (1.002 – 1.016) | (0.993 – 1.002) | (0.997 – 1.006) | (0.996 – 1.005) |
| County Hirschman-Herfindahl Index | ||||
| First Quartile | Ref | Ref | Ref | Ref |
| Second Quartile | 0.891 | 0.829 | 0.875 | 0.558*** |
| (0.640 – 1.241) | (0.595 – 1.157) | (0.636 – 1.205) | (0.412 – 0.755) | |
| Third Quartile | 1.079 | 1.067 | 0.895 | 0.635* |
| (0.713 – 1.633) | (0.743 – 1.531) | (0.627 – 1.277) | (0.401 – 1.006) | |
| Fourth Quartile | 1.006 | 0.719 | 1.096 | 0.612* |
| (0.648 – 1.560) | (0.445 – 1.163) | (0.743 – 1.617) | (0.363 – 1.033) | |
| Metropolitan County | 1.149 | 1.223 | 0.991 | 0.850 |
| (0.870 – 1.517) | (0.864 – 1.733) | (0.686 – 1.431) | (0.616 – 1.174) | |
| Census Sub-Region | ||||
| West North Central | Ref | Ref | Ref | Ref |
| West South Central | 0.701* | 0.885 | 0.986 | 0.927 |
| (0.488 – 1.007) | (0.451 – 1.739) | (0.671 – 1.448) | (0.531 – 1.617) | |
| East North Central | 0.520*** | 1.100 | 0.790* | 1.156 |
| (0.342 – 0.792) | (0.786 – 1.539) | (0.603 – 1.035) | (0.761 – 1.758) | |
| East South Central | 0.225*** | 0.925 | 1.253 | 1.991** |
| (0.144 – 0.352) | (0.350 – 2.445) | (0.822 – 1.910) | (1.149 – 3.450) | |
| Middle Atlantic | 0.250*** | 0.704* | 0.824 | 0.882 |
| (0.140 – 0.446) | (0.469 – 1.056) | (0.496 – 1.367) | (0.542 – 1.435) | |
| Mountain | 0.392*** | 0.909 | 0.748 | 2.060* |
| (0.203 – 0.758) | (0.524 – 1.577) | (0.492 – 1.138) | (0.995 – 4.267) | |
| New England | 0.277*** | 0.522*** | 1.135 | 0.597** |
| (0.141 – 0.542) | (0.338 – 0.807) | (0.658 – 1.957) | (0.359 – 0.992) | |
| Pacific | 0.0998*** | 0.771 | 1.227 | 1.052 |
| (0.0372 – 0.268) | (0.539 – 1.103) | (0.698 – 2.159) | (0.605 – 1.826) | |
| South Atlantic | 0.255*** | 1.081 | 1.084 | 1.377 |
| (0.129 – 0.503) | (0.740 – 1.581) | (0.645 – 1.821) | (0.874 – 2.170) | |
| Resident Case Mix | ||||
| Percent Black Residents | ||||
| Lowest Decile | Ref | Ref | Ref | Ref |
| Below Median | 0.581*** | 0.932 | 1.038 | 0.995 |
| (0.397 – 0.852) | (0.632 – 1.374) | (0.678 – 1.591) | (0.711 – 1.392) | |
| Above Median | 0.576*** | 0.755* | 0.880 | 1.056 |
| (0.431 – 0.771) | (0.569 – 1.002) | (0.578 – 1.338) | (0.797 – 1.400) | |
| Top Decile | 0.383*** | 0.767 | 0.997 | 0.936 |
| (0.238 – 0.619) | (0.504 – 1.167) | (0.551 – 1.804) | (0.600 – 1.463) | |
| Percent Hispanic Residents | ||||
| Below Median | Ref | Ref | Ref | Ref |
| Above Median | 0.986 | 1.082 | 1.007 | 0.861 |
| (0.790 – 1.231) | (0.833 – 1.405) | (0.801 – 1.267) | (0.669 – 1.107) | |
| Top Decile | 0.711* | 1.274 | 0.649* | 0.624** |
| (0.488 – 1.037) | (0.895 – 1.815) | (0.418 – 1.007) | (0.420 – 0.927) | |
| Percent with Medicare | ||||
| Lowest Decile | Ref | Ref | Ref | Ref |
| Below Median | 0.989 | 1.784** | 1.233 | 1.317* |
| (0.742 – 1.320) | (1.144 – 2.784) | (0.803 – 1.893) | (0.963 – 1.802) | |
| Above Median | 1.107 | 1.382 | 1.062 | 0.938 |
| (0.756 – 1.621) | (0.884 – 2.163) | (0.642 – 1.759) | (0.637 – 1.379) | |
| Top Decile | 1.676** | 1.752 | 1.239 | 1.054 |
| (1.038 – 2.707) | (0.872 – 3.520) | (0.666 – 2.306) | (0.652 – 1.702) | |
| Percent with Medicaid | ||||
| Lowest Decile | Ref | Ref | Ref | Ref |
| Below Median | 0.989 | 1.784** | 1.233 | 1.317* |
| (0.742 – 1.320) | (1.144 – 2.784) | (0.803 – 1.893) | (0.963 – 1.802) | |
| Above Decile | 1.107 | 1.382 | 1.062 | 0.938 |
| (0.756 – 1.621) | (0.884 – 2.163) | (0.642 – 1.759) | (0.637 – 1.379) | |
| Top Decile | 1.676** | 1.752 | 1.239 | 1.054 |
| (1.038 – 2.707) | (0.872 – 3.520) | (0.666 – 2.306) | (0.652 – 1.702) | |
| Age (1 Year Increase) | 1.019 | 1.022** | 1.009 | 1.011 |
| (0.990 – 1.049) | (1.002 – 1.042) | (0.986 – 1.032) | (0.986 – 1.038) | |
| Average RUGS NCMI3 | 1.001 | 1.085 | 0.909 | 1.069 |
| (Standardized) | (0.885 – 1.132) | (0.939 – 1.254) | (0.761 – 1.084) | (0.927 – 1.233) |
|
Average ADL3 (Standardized) |
0.899 | 1.022 | 1.089 | 0.984 |
| (0.760 – 1.064) | (0.894 – 1.167) | (0.904 – 1.312) | (0.840 – 1.152) | |
| Percent High CFS3 | 1.000 | 0.965 | 1.003 | 1.101* |
| (10 Percent Increase) | (0.861 – 1.161) | (0.844 – 1.103) | (0.917 – 1.097) | (0.983 – 1.233) |
p<0.01,
p<0.05,
p<0.1
Domain indices were included in the ordered logit model using quartiles of performance for the given index. NHs were divided into quartiles of performance based on the distribution of performance on the domain.
”Yes” response includes nursing homes that answered Yes to “Is your facility part of a Continuing Care Retirement Community?” as well as those that answered “No,” but indicated that they have long-term care beds, assisted living residences, and independent living residences.
RN = Registered Nurse, LPN = Licensed Practical Nurse, CNA = Certified Nursing Assistant, CC=Culture Change, RUGS NCMI =Resource Utilization Group - Average Nursing Case-Mix Index, ADL = Activities of Daily Living Score, CFS = Cognitive Function Score.
For-profit NHs, those with two or more DONs (versus one) in a two-year period, and NHs with higher proportions of Black residents had lower odds of having a higher physical environment index score (Table 3, Column 2). Conversely, NHs in states with higher Medicaid rates and with higher occupancy rates and part of a CCRC had greater odds of having a higher physical environment score. Last, compared to NHs in the West North Central Region, NHs in all other regions had lower physical environment scores.
The observed statistically significant associations with the other indices were fewer and less consistent across increasing values of a covariate. However, similar to the physical environment index, higher occupancy was associated with a greater likelihood of having a higher resident-centered care score; NHs with older residents also had a greater likelihood of having a higher resident-centered care score. On the other hand, greater DON turnover was associated with a lower score (Table 3, Column 3).
Being part of a NH chain and having more RN hours per resident day were associated with lower staff empowerment index scores (Table 3, Column 4) and higher family and community scores (Table 3, Column 5). Last, consistently higher Hirschman-Herfindahl Index scores (lesser NH market competition) were associated with lower family and community engagement index scores.
DISCUSSION
Our survey found that many US NHs appear to be embracing resident-centered care practices in 2016/17 (standardized score of 82.6 of 100) that reflect the provision of person-centered care in accordance with Medicare/Medicaid NH regulations(4) and the ACA.(5) We also found NHs with covariates indicative of lower-tier NH status such as those with lower occupancy, higher DON turnover and higher proportions of Black residents (12) had a significantly greater likelihood of having a lower physical environment domain score, but this finding did not extend to the other three practice domains. Across all domains, NHs with higher NH leadership scores and in states with a Medicaid p4p reimbursement program had higher scores (compared to similar NHs without these attributes). Thus, findings suggest that being a lower-tier NH is not a significant barrier to adoption of most culture change-related practices, that high-quality leadership promotes greater adoption, and that Medicaid p4p programs (with culture change-related quality measures) do appear to “level the adoption playing field.”(17)
While previous research(13) suggests that lower-tiered NHs are less likely to be “culture change providers,” our 2016/17 survey findings argue otherwise. Furthermore, our examination of culture change adoption by domains suggests that only physical environment practices are significantly lower for NHs with characteristics of lower-tier NHs. This finding likely reflects a cost barrier to adopting some physical environment practices (e.g., private rooms, elimination of nursing stations), especially for lower-resourced NHs.
Controlling for leadership practices, we found (as have others)(13, 15) that NHs in states with Medicaid p4p reimbursement (with culture change-related quality measures) are more likely to adopt culture change-related practices. This finding, together with the observation in Kansas showing Medicaid NH p4p reimbursement over time has resulted in less difference in NHs adopting and not adopting culture change,(14) supports the notion that NHs are responsive to Medicaid culture change financial incentives.
Leadership practices reflective of two-way communication, staff involvement in decision-making, staff education and training, respect for workers, good leadership-staff relationships and coaching (i.e., development of staff) were associated with higher scores on all indices, with the highest odds observed for the staff empowerment index. Research has often linked high-quality leadership with successful change, job satisfaction, staff retention and care quality.(36–39) For successful culture change in NHs, the need for coaching and staff involvement in decision-making has been identified,(40) and research by Castle and Decker(38) concludes that a consensus management style is more compatible with the implementation of resident-centered care in NHs. Therefore, leaders can likely advance person-centered care in NHs by adopting practices associated with successful NH change. A guide on these practices is available.(41)
Although the adoption of resident-centered care practices appears relatively high with a standardized score of 82.6, standardized, index scores of 60.5 and 54.8 for staff empowerment and family and community engagement (respectively) suggest lower practice adoption. These practices may be less emphasized (relative to resident-centered care practices) by regulatory/payment efforts and/or that their implementation is more difficult since practices may be more complex (i.e., involve more people in decision making and have less predictable outcomes).(42) Still, practices within these domains are considered important to achieving high-quality care and regulatory compliance. For example, federal regulations require nursing assistant participation in care planning,(4) but only 32% of NHAs reported that assistants often or always attend resident care plan meetings. Also, while the regulations emphasize person-centered care, 16% of NHAs reported that nursing assistants never or sometimes alter their work priorities to meet residents’ needs (see Staff Empowerment Index in Weighted Distribution of Survey Items, Supplemental Digital Content 3). Consequently, greater adoption of these and other culture change-related practices can not only advance more person-centered care and NH deinstitutionalization but also assist NHs to comply with regulations.
Potential limitations to this research include the possibility that NHAs’ responses may reflect some social desirability bias; although we did cognitive testing of our survey items, some administrators may have interpreted questions differently than we intended. However, NHAs demonstrated less social desirability bias when compared to DONs’ responses to the survey items.(22) Though we surveyed only the NHA and not managers and other staff who may have provided us with different perspectives, our survey had a high response rate (73.9%), our sample represented a nationally representative stratified sample of US NHs, and previous research has found administrators to be credible respondents for topics related to NH culture change-related practices.(20–22, 43)
In conclusion, our findings suggest an emphasis on person-centered care in many US NHs but do not discount the need for greater implementation of many other practices associated with high-quality care and/or needed to achieve regulatory compliance. Findings especially highlight the need for NH leadership practices that facilitate change, and support Medicaid pay-for-performance as a viable mechanism to incentivize adoption of culture change-related practices.
Supplementary Material
ACKNOWLEGMENTS:
We would like to acknowledge the advisory committee members who assisted us in identifying and choosing survey items for the 2016/17 survey instrument. They are Christine Bishop, Brandeis University; Lynda Crandall, (formally at) Pioneer Network; David Gifford, American Health Care Association; Robert Jenkens, National Cooperative Bank; Michael Lepore, RTI International; Chris Perna, The Eden Alternative, Inc.; Jackie Pinkowitz, CCAL: Advanced Person-Centered Living; Robyn Stone, LeadingAge.
Funding: Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Award Number R01AG048940. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. As required by the National Institute On Aging a repository including survey data and information on our analytic file creation can be accessed at https://repository.library.brown.edu/studio/item/bdr:788136/.
Footnotes
The authors declare no conflict of interest.
A symposium presenting project methodology and early survey findings was presented at the IAGG 2017 World Congress of Gerontology and Geriatric in San Francisco California.
REFERENCES
- 1.Commission on Long-Term Care. REPORT to the Congress. Washington, DC. 2013. Available from: https://www.gpo.gov/fdsys/pkg/GPO-LTCCOMMISSION/pdf/GPO-LTCCOMMISSION.pdf Accessed April 15, 2018.
- 2.Koren MJ. Person-centered care for nursing home residents: the culture-change movement. Health Aff (Millwood) 2010;29:312–317. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman S, Shier V, Saliba D. Transforming nursing home culture: evidence for practice and policy. Gerontologist 2014;54 Suppl 1:S1–S5 [DOI] [PubMed] [Google Scholar]
- 4.Medicare and Medicaid Programs. Reform of Requirements for LongTerm Care Facilities Federal Register. Rules and Regulations. 2016;81(192). [PubMed] [Google Scholar]
- 5.111th Congress. The Patient Protection and Affordable Care Act (PPACA). March 23, 2010. Code 3590; Bill Number Pub L. No. 111–148.
- 6.Quality Partners of Rhode Island. The Holistic Approach to Transformational Change (HATCh). Providence, RI. 2005:1–12.
- 7.Shier V, Khodyakov D, Cohen LW, et al. What does the evidence really say about culture change in nursing homes? Gerontologist 2014;54 Suppl 1:S6–S16. [DOI] [PubMed] [Google Scholar]
- 8.Zimmerman S, Bowers BJ, Cohen LW, et al. New Evidence on the Green House Model of Nursing Home Care: Synthesis of Findings and Implications for Policy, Practice, and Research. Health Serv Res 2016;51 Suppl 1:475–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grabowski DC, O’Malley AJ, Afendulis CC, et al. Culture change and nursing home quality of care. Gerontologist 2014;54 Suppl 1:S35–S45. [DOI] [PubMed] [Google Scholar]
- 10.Miller SC, Lepore M, Lima JC, et al. Does the introduction of nursing home culture change practices improve quality? J Am Geriatr Soc 2014;62:1675–1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poey JL, Hermer L, Cornelison L, et al. Does Person-Centered Care Improve Residents’ Satisfaction With Nursing Home Quality? J Am Med Dir Assoc 2017;18:974–979. [DOI] [PubMed] [Google Scholar]
- 12.Mor V, Zinn J, Angelelli J, et al. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q 2004;82:227–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grabowski DC, Elliot A, Leitzell B, et al. Who are the innovators? Nursing homes implementing culture change. Gerontologist 2014;54 Suppl 1:S65–S75. [DOI] [PubMed] [Google Scholar]
- 14.Hermer L, Cornelison L, Kaup ML, et al. The Kansas PEAK 2.0 Program Facilitates the Diffusion of Culture-Change Innovation to Unlikely Adopters. Gerontologist 2018;58:530–539. [DOI] [PubMed] [Google Scholar]
- 15.Miller SC, Looze J, Shield R, et al. Culture change practice in US Nursing homes: prevalence and variation by state medicaid reimbursement policies. Gerontologist 2014;54:434–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doty MM, Koren MJ, Sturla EL. Culture Change in Nursing Homes: How Far Have We Come? Findings from the Commonweath Fund 2007 National Survey of Nursing Homes. ed Commonwealth Fund. New York, NY: 2008. [Google Scholar]
- 17.Rogers EM. Diffusion of Innovations. New York, NY: Free Press, A Division of Simon & Schuster, Inc.; 2003. [Google Scholar]
- 18.Taplin SH, Anhang Price R, Edwards HM, et al. Introduction: Understanding and influencing multilevel factors across the cancer care continuum. J Natl Cancer Inst Monogr 2012;2012:2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edwards JR, Bagozzi RP. On the nature and direction of relationships between constructs and measures. Psychol Methods 2000;5:155–174. [DOI] [PubMed] [Google Scholar]
- 20.Shield RR, Looze J, Tyler D, et al. Why and how do nursing homes implement culture change practices? Insights from qualitative interviews in a mixed methods study. J Appl Gerontol 2014;33:737–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tyler DA, Shield RR, Miller SC. Diffusion of palliative care in nursing homes: lessons from the culture change movement. J Pain Symptom Manage 2015;49:846–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shield R, Tyler D, Berridge C, et al. Innovative Use of Cognitive Interviewing for Nursing Home Research. J Am Med Dir Assoc 2018. June 16 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23.Eden Alternative. Available from: http://www.edenalt.org/. Accessed May 16, 2018.
- 24.Advancing Person Centered Living (CCAL). Available from: http://ccal.org/. Accessed April 26, 2018.
- 25.National Cooperative Bank (NCB). BANKING SOLUTIONS FOR Senior Living, Aging Services And Health Care. Available from: https://ncb.coop/ncb/commercial/sectors-we-serve/health-care. Accessed April 26, 2018.
- 26.Pioneer Network. Pioneers in Culture Change and Person-Directed Care. Available from: https://www.pioneernetwork.net/about-us/overview/. Accessed April 26, 2018
- 27.Bowman CS, Schoeneman K. Development of the Artifacts of Culture Change Tool. ed. Centers for Medicare & Medicaid Services; 2006. [Google Scholar]
- 28.Kansas Department for Aging & Disability Services. Peak 2.0 Criteria. Kansas State University; 2018–2019. Available from: https://www.he.k-state.edu/aging/outreach/peak20/2018-19/peak-criteria.pdf. Accessed April 26, 2018. [Google Scholar]
- 29.Jobe JB, Mingay DJ. Cognitive research improves questionnaires. Am J Public Health 1989;79:1053–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rickards G, Magee C, Artino AR Jr. You Can’t Fix by Analysis What You’ve Spoiled by Design: Developing Survey Instruments and Collecting Validity Evidence. J Grad Med Educ 2012;4:407–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaping Long-Term Care in America Project Available from: http://ltcfocus.org/. Accessed February 4, 2016.
- 32.Medicaid and CHIP Payment and Access Commission (MACPAC). States’ Medicaid Fee-for-Service Nursing Facility Payment Policies. 2014. Available at: https://www.macpac.gov/publication/nursing-facilty-payment-policies/. Accessed February 24, 2018.
- 33.R Core Team. R: A language and environment for statistical computing. 2015. Available from: https://www.r-project.org/. Accessed February 24, 2018.
- 34.Revelle W An overview of the psych package. 2011. Available from: http://www.personalitytheory.org/r/book/overview.pdf. Accessed February 23, 2018.
- 35.Gadermann AM, Guhn M, Zumbo BD. Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. PARE 2012;17:1–13. [Google Scholar]
- 36.Jeon YH, Merlyn T, Chenoweth L. Leadership and management in the aged care sector: a narrative synthesis. Australas J Ageing 2010;29:54–60. [DOI] [PubMed] [Google Scholar]
- 37.Bishop CE, Squillace MR, Meagher J, et al. Nursing home work practices and nursing assistants’ job satisfaction. Gerontologist 2009;49:611–622. [DOI] [PubMed] [Google Scholar]
- 38.Castle NG, Decker FH. Top management leadership style and quality of care in nursing homes. Gerontologist 2011;51:630–642. [DOI] [PubMed] [Google Scholar]
- 39.Donoghue C, Castle NG. Leadership styles of nursing home administrators and their association with staff turnover. Gerontologist 2009;49:166–174. [DOI] [PubMed] [Google Scholar]
- 40.Corazzini K, Twersky J, White HK, et al. Implementing Culture Change in Nursing Homes: An Adaptive Leadership Framework. Gerontologist 2015;55:616–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bowers B, Nolet K, Roberts T, et al. Implementing Change in Long-Term Care: A Practical Guide to Transformation. 2003. Available from: https://www.nhqualitycampaign.org/files/Implementation_Manual_Part_1_Attachments_1_and_2.pdf. Accessed February 23, 2018.
- 42.Sterns S, Miller SC, Allen S. The complexity of implementing culture change practices in nursing homes. J Am Med Dir Assoc 2010;11:511–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tyler DA, Shield RR, Rosenthal M, et al. How valid are the responses to nursing home survey questions? Some issues and concerns. Gerontologist 2011;51:201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.