Abstract
Purpose
To evaluate the prevalence and risk factors of myopia in adult Korean population.
Methods
Population-based cross-sectional data of 3,398 subjects aged 19 to 49 years was obtained using the Korea National Health and Nutrition Examination Survey 2013–2014 (KNHANES VI). Data, including refractive errors and potential risk factors were analyzed. The prevalence and risk factors of myopia, low myopia, and high myopia—defined as a spherical equivalent (SEQ) ≤ -0.5 diopters (D), -6.0 D < SEQ <-0.5 D, and SEQ ≤ -6.0 D, respectively—were evaluated.
Results
The prevalence of myopia and high myopia were 70.6 (standard error (SE), ±1.1)% and 8.0 (SE, ±0.6)%, respectively. In multivariable analysis, younger age, higher education (≥12 years), parental myopia, lower serum 25-hydroxyvitamin D (25(OH)D) concentration (<9 ng/mL), longer time spent on near work (≥3 hours/day), and higher white blood cell (WBC) count (5–8.9 x 103) were associated with increased prevalence of both myopia and high myopia. Serum 25(OH)D concentration of ≥ 9 ng/ml was significantly associated with decreased prevalence of high myopia in participants with near work of ≥3 hours/day, although the effect was not significant in myopia and low myopia.
Conclusions
The prevalence of myopia and high myopia in Korean adults was substantially high, which increased with decreasing age. In addition to parental myopia, the serum 25(OH)D concentration, near work and inflammation reflected by WBC counts may be associated with myopia.
Introduction
Myopia is one of the most common ophthalmologic disorders and a major public health concern worldwide [1–3]. The prevalence of myopia varies depending on ethnicity, region, and age group [4, 5]. A meta-analysis estimated that the crude prevalence rates for myopia of spherical equivalent (SEQ) ≤ -1.0 D ranged from 16.4%–26.6% among those aged ≥40 years in the United States, Western Europe, and Australia [6]. The prevalence of myopia of ≤ -0.5 D in East Asians ≥40 years was 26.2%–41.8% [7–10], which is substantially higher compared with Caucasians. Myopia prevalence has sharply increased in the younger generation in East Asia [5, 11–13]. It was reported to be as high as 79.3% in Singapore military conscripts aged 17–19 years, and 86.1% in Taiwan conscripts aged 18–24 years [5, 11]. This phenomenon was also observed in Korea, and the prevalence of myopia in a population of 19-year-old males was 96.5% and 93.3% in urban and rural areas of Korea, respectively [12, 13].
Research elucidating the pathogenesis of myopia and its risk factors would be necessary to prevent myopia and reduce the socioeconomic burden of the disease. Studies suggested that the risk of myopia was associated with parental myopia [14, 15], higher socioeconomic status [16–18], near work [11, 18], education [5, 12, 19], urban residence [1, 20], low serum vitamin D [4, 21], lesser outdoor activity [20, 22], and height [1, 19]. However, controversies exist among the studies, and the mechanism of myopia development remains unclear. Moreover, only few studies have been conducted regarding the risk factors of myopia in adult population.
In this study, we evaluated the prevalence and risk factors of myopia in a representative Korean adult population using the Korea National Health and Nutrition Examination Surveys (KNHANES), which is a series of nationwide cross-sectional health examination and survey conducted to monitor the general health and nutritional status of Koreans by the Division of Chronic Disease Surveillance, Korea Centers for Disease Control and Prevention (KCDC) [1].
Patients and methods
Study design and population
KNHANES are designed to produce a nationally representative data of the civilian, non-institutionalized Korean population [23]. KNHANES participants were sampled based on a stratified, multistage, cluster probability sampling, which uses the primary sampling units (PSU) as defined by the geographical areas in Korea [23]. In KNHANES VI that began in 2013, 192 enumeration districts were selected each year, and 20 households in each enumeration district were selected using a systematic sampling method [23].
KNHANES surveys consist of health interview survey, health examination survey, and nutrition survey. Information including age, sex, education level, education level of parents, annual income (quartile 1(lowest) to 4 (highest)), residential area (urban or rural), time spent on near work, occupational type, and parental myopia was obtained through health interviews. Anthropometric measurements were performed to yield variables, including height, weight, waist circumference and body mass index (BMI) calculated as weight (kg)/height2 (m2)[21]. Laboratory test results, including concentration of blood heavy metals, concentration of serum 25-hydroxyvitamin D (25(OH)D) concentration and complete blood count, were also collected.
The KNHANES was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (KCDC), and written informed consent was obtained from all participants in the survey. This study adhered to the tenets of the Declaration of Helsinki for biomedical research.
Ophthalmologic examination and data collection
In KNHANES VI, participants aged 19 to 49 years were selected and received ophthalmological examinations, including visual acuity testing and autorefraction. Noncycloplegic autorefraction was performed using an autorefractor-keratometer (KR-8800, Topcon, Tokyo, Japan) in both eyes by trained ophthalmologists. Autorefraction measurements were converted into spherical equivalents (SE), as calculated by the spherical value + 1/2 of cylinder value. Refractive error was defined based on the left eye [1]. Myopia was defined as an SEQ ≤ -0.5 diopters (D), and non-myopia was defined as an SEQ >-0.5 D. Myopia was subdivided into low myopia (-6.0 D < SEQ ≤ -0.5 D) and high myopia (SEQ ≤ -6.0 D).
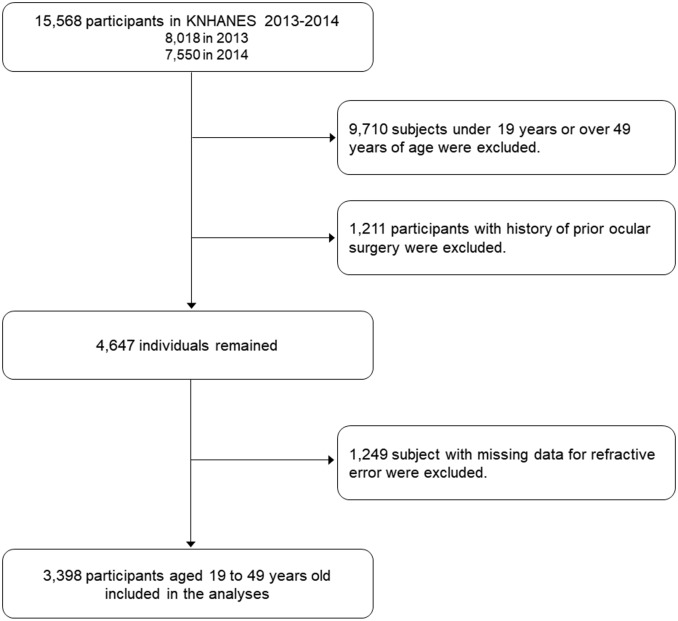
Data from the KNHANES VI (VI -1, 2013 & VI—2, 2014) studies were used to investigate the prevalence and risk factors of myopia in adult Korean population. Among 15,568 (8,018 in 2013 and 7,550 in 2014) participants, 5,858 subjects who were aged between 19 and 49 years received an ophthalmic examination. Among them, 1,211 individuals with s history of prior ocular surgery, such as refractive surgery or cataract extraction, were excluded. Among the remaining 4,647 participants, 1,249 with missing data for refractive error were also excluded; 3,398 subjects were finally included in this study (Fig 1).
Fig 1. Flow diagram describing the selection of participants included in the present study.
Cut-points of serum 25(OH)D concentration
At first, we classified the serum 25(OH)D concentration to 10 percentiles. Then, we defined a group with the serum 25(OH)D concentration > 90 percentile as the reference group and calculated the odds ratios (ORs) for myopia by the serum 25(OH)D category. Among the nine groups, the 0–10 percentile group (serum 25(OH)D < 9 ng/mL) showed the strongest association with myopia prevalence. However, no significant increase in myopia prevalence by serum 25(OH)D of 11–20 percentile was observed. Thus, we determined the serum 25(OH)D concentration of 9 ng/mL as the cut-point.
Categorization for time spent on near work
Responses to the question on time spent on near work were 1, 2, 3, and 4 hours/day in the KNHANES questionnaire. Because spending 3 or more hours/day on near work was significantly associated with increased myopia prevalence, we re-classified the four groups into two groups (≤2 hours/day and ≥3 hours/day) to ensure sufficient statistical power in stratified analysis by time spent on near work.
Statistical analysis
KNHANES is derived from the multi-stage clustered probability sampling to produce a nationally representative survey data. To calculate the proper estimates and standard errors of the estimates, sampling components (strata and cluster), and appropriate weight should be considered in the analyses. Briefly, strata based on administrative district and housing type (apartment and conventional dwelling) and primary sampling unit (PSU), the cluster which consists of about 60 households, were used for sampling in KNHANES. Sample weight calculated by multiplying inverse of selection probability and inverse of response rate and adjusting them by reflecting age- and sex-specific population structure was also considered. PROC SURVEY procedures in the SAS program were developed for complex survey data analysis, thus we used these procedures in this work [24].
Continuous variables were presented using the weighted mean and standard deviation (SD) or median with interquartile range (IQR) in case of variables not distributed normally, and categorical variables were expressed as weighted frequencies with standard errors (SE) (%). The difference with respect to the means or the proportions of potential risk factors of myopia between non-myopia group and myopia group was assessed using t-test for normally distributed continuous variable, the Mann-Whitney U test for not normally distributed continuous variables, and Pearson’s Chi-square test for categorical variables.
The prevalence of myopia, low myopia, and high myopia in the total study population and in each age group was presented with weighted frequency (%) and SE. To calculate prevalence relative risks and their corresponding confidence intervals, we set the prevalence of myopia as dependent variable and age groups as independent variable in the logistic regression model.
Association between potential risk factors and prevalence of myopia (non-myopia (reference) vs. myopia) was evaluated by calculating the odds ratios (ORs) and 95% confidence intervals (CIs) using the binary logistic regression model. Independent variables included in the above binary logistic regression model were as follows: age, education level (< 12 vs. ≥ 12 years), parental myopia, serum 25(OH)D level (< 9 vs. ≥ 9 ng/mL), time spent on near work (≤2 vs. ≥3 hours/day), and white blood cell (WBC) counts (<5 x 103, 5–8.9 x 103, ≥9 x 103). According to likelihood ratio test, logistic regression model including all independent variables above was the preferred model.
When it comes to analysis with consideration of myopia severity (low, and high myopia), binary logistic regression model was also used to assess the association between potential risk factors and low myopia (non-myopia (reference) vs. low myopia) or high myopia (non-myopia (reference) vs. high myopia).
Based on the results of multivariable analysis, the association between potential risk factors for the prevalence of total, high, and low myopia in a stratified group was also evaluated.
We set the type I error as 0.05 in this study. Statistical analyses were performed using SAS software (ver. 9.3; SAS Institute, Inc., Cary, NC, USA).
Results
General characteristics
The mean age of the study participants was 36.3 ± 8.6 (mean ± SD) years. The sex ratio was 54.5 ± 0.9% for male and 45.5 ± 0.9% for female, respectively. In univariable analysis, participants in the myopia group was significantly younger and on average 1 (95% CI, 0.3, 1.7) cm taller (P = 0.02), with lower serum 25(OH)D concentration than those in the non-myopia group. However, there was no significant difference in the height and serum 25(OH)D concentration between participants with low myopia and those with high myopia, although participants with high myopia were significantly younger than those with low myopia. The proportion of participants with parental myopia, high annual income, increased time of near work (≥3 hours/day), higher education level, and higher education levels of both parents were higher in the myopia group compared with the non-myopia group. Participants with high myopia were more likely to have parental myopia, increased time of near work, and higher education levels of both parents compared with those with low myopia (Table 1).
Table 1. General characteristics of study subjects aged 19–49 years old in the Korea National Health Examination and Nutritional Survey (KNHANES), Phase VI, 2013–2014.
| Variables | Non-myopia (N = 1,025) |
Myopia (N = 2,373) |
P1 | 95% CI for difference2 | Mild myopia (N = 2,112) |
High myopia (N = 261) |
P1 | 95% CI for difference2 |
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Height (cm) | 166.6 (8.8) | 167.6 (8.7) | 0.02 | 0.3–1.7 | 167.6 (8.7) | 167.6 (8.8) | 0.90 | -1.3–1.3 |
| Weight (Kg) | 66.3 (12.7) | 66.6 (13.6) | 0.56 | -0.7–1.3 | 66.5 (13.3) | 67.4 (15.2) | 0.46 | -1.2–3.0 |
| WC (cm) | 80.0 (10.0) | 79.7 (10.4) | 0.52 | -0.5–1.1 | 79.6 (10.3) | 80.1 (11.3) | 0.55 | -1.1–2.1 |
| BMI (Kg/m2) | 23.8 (3.6) | 23.6 (3.8) | 0.29 | -0.1–0.5 | 23.6 (3.7) | 23.8 (4.3) | 0.44 | -0.4–0.8 |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |||||
| Age (year) | 39.5 (31.5–44.8) | 33.8 (25.7–41.2) | <0.01 | 3.2–4.8 | 34.1 (26.2–41.5) | 31.3 (22.8–39.5) | <0.01 | 0.7–3.9 |
| Serum 25(OH) (ng/ml) | 14.9 (11.6–19.0) | 14.4 (11.3–18.1) | 0.02 | 0.2–2.2 | 14.4 (11.2–18.1) | 14.8 (11.3–18.1) | 0.27 | -1.0–1.4 |
| Calcium intake (g/day) | 449 (330–637) | 445 (303–631) | 0.23 | -16–49 | 445.9 (303–634) | 432.8 (303–600) | 0.97 | -58–59 |
| Energy intake (Cal/day) | 2005 (1521–2707) | 2014 (1510–2688) | 0.77 | -96–99 | 2011 (1502–2689) | 2069 (1605–2659) | 0.20 | -135–176 |
| Hemoglobin (mg/dl) | 14.4 (13.2–15.7) | 14.6 (13.3–15.7) | 0.19 | -0.1–0.1 | 14.6 (13.3–15.7) | 14.6 (13.3–15.8) | 0.90 | -0.2–0.2 |
| WBC count (x103) | 6.1 (5.0–7.3) | 6.1 (5.2–7.4) | 0.01 | -0.1–0.1 | 6.1 (5.2–7.3) | 6.3 (5.5–7.7) | <0.01 | 0.0–0.6 |
| N (%) | N (%) | N (%) | N (%) | |||||
| Parental myopia | 75 (8.3) | 347 (16.1) | <0.01 | 5.6–10.0 | 281 (8.3) | 66 (27.3) | <0.01 | 13.5–24.5 |
| Female | 599 (46.0) | 1,293 (45.4) | 0.76 | -3.1–4.3 | 1,148 (45.3) | 145 (45.6) | 0.94 | -6.1–6.7 |
| Higher income 3 | 452 (43.1) | 1,159 (47.9) | 0.03 | 1.2–8.4 | 1,018 (47.5) | 141 (51.2) | 0.33 | -2.7–10.1 |
| Near work ≥ 3 hour/day | 449 (45.2) | 1,438 (63.5) | <0.01 | 14.7–21.9 | 967 (48.3) | 147 (57.4) | <0.01 | 5.5–16.9 |
| Education ≥ 12 years | 372 (39.4) | 1,143 (49.3) | <0.01 | 6.3–13.5 | 1,000 (48.7) | 143 (54.1) | 0.11 | -1.0–11.8 |
| Father’s education ≥12 years | 746 (88.5) | 1,666 (78.7) | <0.01 | 7.2–12.4 | 1,502 (80.3) | 164 (66.6) | <0.01 | 7.7–19.7 |
| Mother’s education ≥12 years | 826 (95.8) | 1,894 (89.7) | <0.01 | 4.4–7.8 | 1,699 (90.7) | 195 (81.5) | <0.01 | 4.3–14.1 |
WC, Waist Circumference; BMI, Body mass index; WBC, White blood cell.
All data are expressed as mean (SD), median (interquartile range (IQR)) or weighted frequency
1. P value using independent t-test or Mann-Whitney test for continuous variable, and Pearson’s chi-square test for categorical variable
2. 95% confidence intervals for difference in mean or proportion of each variables
3. Above median annual household income in Korean population
Prevalence of myopia
The prevalence of myopia and high myopia were 70.6 ± 1.1% and 8.0 ± 0.6%, respectively, which decreased significantly with age, from 81.3 ± 0.8% and 13.3 ± 0.4% in the population aged 19 to 24 years to 55.2 ± 0.7% and 4.0 ± 0.2% in the population aged 45 to 49 years, respectively (Table 2).
Table 2. Prevalence of myopia in various age groups.
| Age (year) | Total | Myopia* | Low myopia | High myopia | Myopia* | Low myopia | High myopia |
|---|---|---|---|---|---|---|---|
| N | N, Prevalence (%±SE) |
N, Prevalence (%±SE) |
N, Prevalence (%±SE) |
PRR (95% CI) † | PRR (95% CI) † | PRR (95% CI) † | |
| Total | 3,398 | 2,373 (70.6±1.1) | 2,112 (62.6±1.0) | 261 (8.0±0.6) | |||
| 19–24 | 463 | 383 (81.3±0.8) | 325 (68.0±0.7) | 58 (13.3±0.4) | 3.53 (2.54, 4.92) | 3.19 (2.30, 4.42) | 7.96 (4.24, 14.95) |
| 25–29 | 339 | 269 (79.6±0.7) | 238 (70.5±0.7) | 31 (9.1±0.2) | 3.17 (2.22, 4.53) | 3.02 (2.10, 4.35) | 5.00 (2.67, 9.35) |
| 30–34 | 508 | 390 (76.9±0.7) | 346 (68.9±0.7) | 44 (8.0±0.2) | 2.70 (2.01, 3.65) | 2.61 (1.93, 3.54) | 3.86 (2.19, 6.80) |
| 35–39 | 664 | 472 (71.0±0.7) | 425 (64.3±0.6) | 47 (6.7±0.2) | 1.99 (1.57, 2.52) | 1.94 (1.54, 2.46) | 2.58 (1.47, 4.53) |
| 40–44 | 737 | 478 (65.3±0.7) | 423 (57.7±0.6) | 55 (7.6±0.2) | 1.53 (1.21, 1.94) | 1.46 (1.15, 1.85) | 2.45 (1.43, 4.20) |
| 45–49 | 687 | 381 (55.2±0.7) | 355 (51.2±0.6) | 26 (4.0±0.2) | 1.00 | 1.00 | 1.00 |
SE, standard error; PRR, prevalence relative risk
*Myopia was divided into low myopia and high myopia.
†Calculated based on the comparison with prevalence of non-myopia, with age group of 45–49 year as the reference level
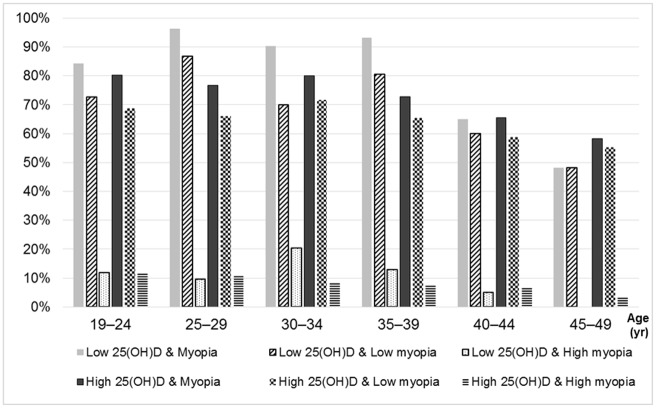
Myopia prevalence according to age in the stratified group by serum 25(OH)D level (< 9 vs. ≥ 9 ng/mL) is shown in Table 3 and Fig 2. The prevalence of myopia, low myopia, and high myopia in the low serum 25(OH)D group (82.0%, 71.7%, and 10.3%, respectively) were higher than the high serum 25(OH)D group (72.5%, 64.3%, and 8.2%, respectively). The prevalence of myopia, low myopia, and high myopia tended to be higher in the low serum 25(OH)D group compared with the high serum 25(OH)D group in each age group, particularly in younger age groups. Regardless of the serum 25(OH)D level, the group aged from 45 to 49 years was associated with the lowest prevalence of myopia compared with other age groups.
Table 3. Prevalence of myopia by various age groups in two stratified groups according to serum 25(OH)D concentration.
| Age (year) | Serum 25(OH)D concentration < 9 ng/mL | Serum 25(OH)D concentration ≥ 9 ng/mL | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | Myopia* | Low myopia | High myopia | Total | Myopia* | Low myopia | High myopia | |
| N | N, Prevalence (%±SE) |
N, Prevalence (%±SE) |
N, Prevalence (%±SE) |
N | N, Prevalence (%±SE) |
N, Prevalence (%±SE) |
N, Prevalence (%±SE) |
|
| Total | 141 | 114 (82.0±0.4) | 100 (71.7±0.4) | 14 (10.3±0.1) | 1,373 | 991 (72.5±0.9) | 881 (64.3±0.9) | 110 (8.2±0.4) |
| 19–24 | 38 | 32 (84.4±4.0) | 27 (72.7±3.8) | 5 (11.7±1.6) | 234 | 193 (80.2±1.3) | 167 (68.6±1.2) | 26 (11.5±0.6) |
| 25–29 | 27 | 26 (96.4±4.2) | 23 (86.8±4.2) | 3 (9.6±1.3) | 178 | 138 (76.7±1.2) | 120 (66.0±1.1) | 18 (10.6±0.4) |
| 30–34 | 21 | 18 (90.3±3.1) | 14 (69.9±2.8) | 4 (20.4±1.6) | 199 | 155 (80.0±0.9) | 137 (71.6±0.9) | 18 (8.4±0.3) |
| 35–39 | 15 | 14 (93.2±2.1) | 13 (80.4±1.8) | 1 (12.8±1.0) | 262 | 192 (72.8±0.8) | 171 (65.4±0.8) | 21 (7.5±0.3) |
| 40–44 | 21 | 14 (65.0±2.0) | 13 (60.0±1.9) | 1 (5.0±0.6) | 270 | 177 (65.6±0.8) | 157 (58.7±0.8) | 20 (6.9±0.3) |
| 45–49 | 19 | 10 (48.2±2.1) | 10 (48.2±2.1) | 0 (0.0±0.0) | 230 | 136 (58.2±0.8) | 129 (55.2±0.8) | 7 (3.0±0.2) |
SE, standard error
*Myopia was divided into low myopia and high myopia.
Fig 2. Prevalence of myopia, low myopia and high myopia by various age groups in two stratified groups according to serum 25(OH)D concentration (low 25 (OH)D = serum 25(OH)D concentration < 9 ng/mL; high low 25 (OH)D = serum (OH)D concentration ≥ 9 ng/mL).
Factors associated with myopia
The results of multivariable logistic regression to elucidate potential risk factors of myopia are summarized in Table 4. Younger age, education level ≥12 years, parental myopia, lower serum 25(OH)D concentration (<9 ng/mL), greater near work of ≥ 3 hours/day and WBC counts of 5,000 to 8,999 were significantly associated with increased myopia prevalence. Subjects aged 19 to 29 years and those aged 30 to 39 years showed 2.11-fold (95% CI, 1.64, 2.73) and 1.59-fold (95% CI, 1.31, 1.94) increased prevalence of myopia compared with those aged 40 to 49 years, respectively (Table 4).
Table 4. Association with potential risk factors for the likelihood of myopia among adults aged between 19 and 49 years in the Korea National Health Examination and Nutritional Survey (KNHANES) Phase VI, 2013–2014.
| Variables | Non-myopia (N = 1,025) N |
Myopia (N = 2,373) N |
OR (95% CI)1 |
|---|---|---|---|
| Age (years) | |||
| 19–29 | 150 | 652 | 2.11 (1.64, 2.73) |
| 30–39 | 310 | 862 | 1.59 (1.31, 1.94) |
| 40–49 | 565 | 859 | 1.00 |
| Education level (years) | |||
| <12 | 555 | 1,047 | 1.00 |
| 12+ | 372 | 1,143 | 1.49 (1.23, 1.80) |
| Parental myopia | |||
| No | 885 | 1,888 | 1.00 |
| Yes | 75 | 347 | 1.55 (1.12, 2.13) |
| Serum 25(OH)D (ng/ml) | |||
| <9 | 27 | 114 | 1.00 |
| 9+ | 382 | 991 | 0.62 (0.38, 1.01) |
| Near work (hours/day) | |||
| ≤2 | 576 | 935 | 1.00 |
| 3+ | 449 | 1,438 | 1.52 (1.28, 1.81) |
| WBC counts x103 | |||
| <5 | 251 | 453 | 1.00 |
| 5–8.9 | 645 | 1,622 | 1.26 (1.01, 1.56) |
| 9+ | 64 | 151 | 1.11 (0.75, 1.65) |
1. Adjusted for age, educational levels, parental myopia, serum 25(OH)D levels, time spent on near work, and WBC count
In a subgroup analysis by severity of myopia (low myopia and high myopia), younger age, higher education level (≥ 12 years), parental myopia, and longer time spent on near work were significantly associated with elevated prevalence of low myopia (Table 5). Participants aged 19 to 29 years and 30 to 39 years showed 2.04-fold (95% CI, 1.58, 2.63) and 1.62-fold (95% CI, 1.32, 1.98) increased low myopia prevalence compared with those aged 40 to 49 years, respectively. Near work of ≥ 3 hours/day was associated with increased prevalence of low myopia compared with near work of ≤2 hours/day (OR, 1.48; 95% CI, 1.24, 1.77).
Table 5. Association with potential risk factors for the likelihood of high and low myopia relative to non-myopia among adults aged between 19 and 49 years in the Korea National Health Examination and Nutritional Survey (KNHANES) Phase VI, 2013–2014.
| Variables | Non-myopia N |
Low myopia N |
OR (95% CI)1 | Non-myopia N |
High myopia N |
OR (95% CI)1 |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| 19–29 | 150 | 563 | 2.04 (1.58, 2.63) | 150 | 89 | 2.55 (1.62, 4.02) |
| 30–39 | 310 | 771 | 1.62 (1.32, 1.98) | 310 | 81 | 1.37 (0.92, 2.02) |
| 40–49 | 565 | 778 | 1.00 | 565 | 81 | 1.00 |
| Education level (years) | ||||||
| <12 | 555 | 943 | 1.00 | 555 | 104 | 1.00 |
| 12+ | 372 | 1,000 | 1.44 (1.19, 1.74) | 372 | 143 | 1.80 (1.30, 2.49) |
| Parental myopia | ||||||
| No | 885 | 1,706 | 1.00 | 885 | 182 | 1.00 |
| Yes | 75 | 281 | 1.41 (1.01, 1.95) | 75 | 66 | 3.11 (2.02, 4.77) |
| Serum 25(OH)D (ng/ml) | ||||||
| <9 | 27 | 100 | 1.00 | 27 | 14 | 1.00 |
| 9+ | 382 | 881 | 0.63 (0.38, 1.03) | 382 | 110 | 0.49 (0.25, 0.97) |
| Near work (hours/day), | ||||||
| ≤2 | 576 | 856 | 1.00 | 576 | 79 | 1.00 |
| 3+ | 449 | 1,256 | 1.48 (1.24, 1.77) | 449 | 182 | 2.17 (1.55, 3.04) |
| WBC counts x103 | ||||||
| <5 | 251 | 418 | 1.00 | 251 | 35 | 1.00 |
| 5–8.9 | 645 | 1,437 | 1.23 (0.98, 1.53) | 645 | 185 | 1.75 (1.04, 2.94) |
| 9+ | 64 | 125 | 1.00 (0.67, 1.49) | 64 | 26 | 2.69 (1.28, 5.66) |
1. Adjusted for age, educational levels, parental myopia, serum 25(OH)D levels, time spent on near work, and WBC count
Increased prevalence of high myopia showed a significant association with younger age, higher education level (≥ 12 years), parental myopia, lower serum 25(OH)D concentration (<9 ng/ml), longer time of near work, and greater WBC count (≥ 5,000). The young age group (age from 19 to 29 years) showed elevated prevalence of high myopia (OR, 2.55; 95% CI, 1.62, 4.02) compared with the group aged 40 to 49 years. Near work of ≥ 3 hours daily had a 2.17-fold (95% CI, 1.55, 3.04) increased prevalence of high myopia than near work of ≤2 hours daily (Table 5).
The association of the serum 25(OH)D concentration with total, low, and high myopia in a stratified group for time spent on near work (≤2 hours/day vs. ≥3 hours/day) are shown in Table 6. In subjects with near work of ≤2 hours, no significant influences of serum 25(OH)D on total, low, and high myopia were observed. In participants with near work of ≥3 hours/day, serum 25(OH)D concentration of ≥9 ng/ml was significantly related to decreased prevalence of high myopia, although the effect was not significant in myopia and low myopia.
Table 6. 2014 The association of the serum 25(OH)D concentration with total, low, and high myopia in two strata for time spent on near time work ≤2 hours/day vs. ≥3 hours/day) among adults at age 19–49 years old in the Korea National Health Examination and Nutritional Survey (KNHANES) Phase VI, 2013–2014.
| Variables | Non-myopia N |
Myopia N |
OR (95% CI)1 | Non-myopia N |
Low myopia N |
OR (95% CI)1 | Non-myopia N |
High myopia N |
OR (95% CI)1 |
|---|---|---|---|---|---|---|---|---|---|
| Near work ≤ 2 (hour/day) | |||||||||
| Serum 25(OH)D (ng/ml) | |||||||||
| <9 | 11 | 33 | 1.00 | 11 | 31 | 1.00 | 11 | 2 | 1.00 |
| 9+ | 211 | 373 | 0.90 (0.36, 2.20) | 211 | 345 | 0.87 (0.35, 2.15) | 211 | 28 | 1.45 (0.21, 9.98) |
| Near work ≥ 3 (hour/day) | |||||||||
| Serum 25(OH)D (ng/ml) | |||||||||
| <9 | 16 | 81 | 1.00 | 16 | 69 | 1.00 | 16 | 12 | 1.00 |
| 9+ | 171 | 618 | 0.44 (0.19, 1.05) | 171 | 536 | 0.47 (0.19, 1.13) | 171 | 82 | 0.28 (0.10, 0.80) |
1. Adjusted for age, educational levels, parental myopia, and WBC counts
Discussion
The results of this study revealed a high prevalence of myopia and high myopia, 70.6± 1.1% and 8.0 ± 0.6%, respectively, in Korean adults aged between 19 and 49 years. This prevalence was shown to decrease with age. A study using the KNHANES data of the year 2008–2011 showed a sharp decline in the prevalence of myopia with increasing age; from 78.9% in participants aged 20–29 years to 16.1% in those aged 60–69 years [25]. These findings suggest that the prevalence of myopia might be higher in younger age groups, which can possibly contribute to the overall increase in the prevalence of myopia.
In Caucasians, the prevalence of myopia is substantially lower compared with the results of studies using KNHANES data including ours [25, 26]. Using the US NHANES data of 1999–2004, Vitale et al [2]. reported that the prevalence of myopia of ≤ -1.0 D in a population of ≥ 20 year was 33.1%. In the Los Angeles Latino Eye Study, myopia prevalence was 16.8% in adults of ≥ 40 years old [27]. A British study showed that the prevalence of myopia of ≤ -0.75 D was 49% in the 44 year old birth cohort [28]. In Norway, myopia prevalence was 35.0% in the group of 20–25 years old [29].
Higher prevalence of myopia in East Asians, especially those in urban areas, compared with Caucasians has been reported [30]. In Singapore, the prevalence of myopia of ≤ -0.5 D in Malay, Indian and Chinese adults > 40 years was 26.2% [8], 28.0% [9], and 38.7% [7], respectively [7–9], suggesting that myopia might be more prevalent in Chinese than in other ethnic groups. The prevalence of myopia in Japanese adults between the ages of 40 and 79 years was 45.7% in men and 38.3% in women [16]. Another study showed that the prevalence of myopia of ≤ -0.5 D was 41.8% in Japanese adults ≥ 40 years [10]. The results of this study, as well as those of previous studies using KNHANES data, suggest that the prevalence of myopia in Korean adults might increase more sharply compared with those in other countries [25, 26, 31].
Multivariable logistic regression analysis revealed that both myopia and high myopia had significant association with younger age, higher education level, parental myopia, lower serum vitamin D concentration, increased time of near work, and higher WBC counts, though the association between low serum 25(OH)D and myopia prevalence was marginally significant. Previous studies using KNHANES data revealed that younger age, higher education level, lower serum vitamin D levels, and shorter daily sun exposure may be risk factors for myopia [25, 26, 31]. The results of the present study are consistent with those of prior studies, and also suggest the association between WBC counts and both myopia and high myopia.
Several studies demonstrated the association between parental myopia and the risk of myopia [11, 14, 15, 18, 32–36]. Low et al. [14] indicated that a family history of myopia might be the most important risk factor for early myopia. Parental myopia was suggested to influence the growth rate of children’s eye [15, 37]. Saw et al. [35] revealed that children with myopic parents tended to have increased axial length.
In this study, near work and higher education level were associated with both myopia and high myopia. A British study also revealed this association of myopia with near work and educational performance [28]. Several studies also indicated that near work including reading and computer use, may increase the risk of myopia [9, 11, 32, 38–40]. Saw et al [35]. reported that children who read > 2 books a week had longer axial lengths by 0.17 mm compared with those who read ≤2 books a week. Previous studies also suggested that myopia may be associated with higher educational level [7, 8, 16, 18, 19, 25, 27, 30, 41] or higher academic achievements [12, 13, 32]. Education level can be considered a surrogate for near work, as both the achievement and duration of education are conceivably closely correlated with time spent studying and reading [42]. A meta-analysis suggested that lower education level could attenuate the influence of risk alleles on myopia, which underscores the role of gene-environment interactions in the development of myopia [43]. High hereditability of myopia does not preclude strong environmental influence, and the environmental impact can increase the risk of myopia across the population to a similar extent, which results in rapid change in the prevalence of myopia [44]. For instance, due to environmental pressures, including education and near work in Singapore, a large number of children with non-myopic parents have high myopia.[37]. A sharp increase in the prevalence of myopia in younger age groups in Korea may also reflect this phenomenon.
In the present study, the low serum 25(OH)D concentration was also shown to be related to increased prevalence for both myopia and high myopia, which is consistent with previous studies using the KNHANES data [21, 31]. Other researchers also revealed that myopes had a significantly lower blood vitamin D concentration compared with non-myopes [4, 45], A large population-based study revealed that polymorphisms within vitamin D receptor (VDR) are related to a low-to-moderate degree of myopia [46]. As endogenous synthesis of vitamin D is induced by sunlight, it is often considered a biomarker of outdoor activity [46]. The prevalence of vitamin D insufficiency has been increasing worldwide [47, 48]. Data from KNHANES also showed that vitamin D deficiency was highly prevalent in Korean adolescents [49], which can be explained by reduced sunlight exposure caused by high educational pressure and decreased intake of vitamin D-rich foods [49, 50]. Given that vitamin D plays an important role in the intestinal absorption of calcium, mineral homeostasis, and bone growth in adolescence [51], it can be hypothesized that vitamin D deficiency may be associated with the development of myopia in adolescence [51]. Moreover, vitamin D deficiency can also result in the impairment of relaxation and contraction of the ciliary muscles caused by an alteration of intracellular calcium concentration, which may lead to myopia genesis [52]. Moreover, vitamin D initiates the formation of the VDR/retinoic acid heterodimer [53], which participates in the retinoscleral signal pathway that may influence myopic ocular growth [21]. The major product of novel cytochrome P450scc (CYP11A1)-initiated pathway of vitamin D3 metabolism, 20-hydroxyvitamin D3 (20(OH)D3), and its metabolites may have anti-proliferative, pro-differentiation, and anti-inflammatory effects, which could prevent myopia [54–56].
Several studies demonstrated the protective effect of outdoor activity in myopia development [20, 22, 57–62]. Although the mechanisms underlying the possible protective effect of outdoors activity is unclear, there have been two hypotheses to date: 1) Higher light intensity of the outdoors may stimulate retinal dopamine release [22], which was proven to suppress axial elongation in animal model [63]. 2) Brighter outdoor light intensity may increase the depth of focus through pupil constriction, leading to reduced accommodative demand [22, 57]. These may not directly be applicable to adults with full eyeball maturity [22]. The most plausible explanation would be that the results reflect a continuation in the occupation or behavior. Individuals who spend more time reading books during childhood are more likely to become office workers and be involved in work related to reading and using the computer [22].
Regarding the relationship between vitamin D and outdoor activity, Kwon et al [31]. showed that both factors may be independently associated with myopia in Korean adults. However, a cohort study demonstrated that there was no association between vitamin D and myopia, while outdoor activity had protective effect on myopia [64]. By contrast, another study revealed that the association between vitamin D and myopia retained after adjustment for conjunctival UV autofluorescence, an ocular sun-exposure biomarker [4]. We believe that further studies are needed to investigate the pathophysiology underlying the possible influence of vitamin D and outdoor activity on myopia [4].
Among the risk factors for myopia found in the present study, only serum 25(OH)D concentration and time of near work are controllable. Considering the high pressure for education and increased computer use, reducing the time of near work would be difficult. Given the possible association between higher serum 25(OH)D concentration and decreased risk of high myopia in adults with increased time of near work, it could be possible to prevent high myopia by increasing serum prevented concentration, possibly by vitamin D supplementation or vigorous outdoor activities.
Increased WBC counts were also associated with both myopia and high myopia, indicating the relationship between inflammatory response and myopia progression. Although only few studies have studied the association between myopia and inflammation, Lin et al.[65] showed that the inhibition of inflammatory response delayed myopia development and aggravation of inflammation accelerated myopia progression. We believe further studies are necessary to elucidate the influence of inflammation on myopia.
The present study has some limitations. First, refractive error was measured without cycloplegia, which could lead to the overestimation of the prevalence of myopia. However, this is a limitation shared by most of the studies on refractive errors in adults, as performing a cycloplegic refraction in a large population is almost impossible. Second, due to the cross-sectional design, a causal relationship could not be evaluated. We believe further prospective studies are needed for the evaluation of the effect of proposed risk factors of myopia. Third, this study did not evaluate the time of outdoor activity, serum calcium level, and bone parameters. Therefore, the potential protective effect of vitamin D supplementation or outdoor activity was never evaluated. Further studies including these variables are therefore warranted. Fourth, participants with a history of ocular surgery were excluded. However, considering that this study included patients aged 19 to 49 years, a substantial number of excluded subjects possibly have history of vision correction surgery for myopia, which could lead to underestimation of myopia prevalence.
In conclusion, this study showed a high prevalence of myopia and high myopia in Korean adults, which increased in younger age groups. In addition to parental myopia, low serum 25(OH)D concentration and near work may be associated with myopia. Inflammation reflected by WBC counts might also be related to myopia.
Data Availability
Data are available from the Korea Center for Chronic Disease and Control Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data. The authors obtained the data set from the Korea Center for Chronic Disease and Control, which owns the data. Readers can send requests for data to Tel: 82-43-719-7467 or Email: sun4070@korea.kr (Division of Health and Nutrition Survey, KCDC). Data can also be downloaded from the following website: https://knhanes.cdc.go.kr/knhanes/eng/index.do;jsessionid=Rz6lEQIMQE7y0V27jrTgtsBj1BW8sHOmiaOhJkYPQePH5kxA68xWDNCEdUzp7wj5.CDCPOWAS02_1.5_servlet_PUB.
Funding Statement
This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIP) (No. 2017R1A2B4011450) & by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant No. NRF-2017R1D1A1B03029983). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Rim TH, Kim SH, Lim KH, Kim HY, Baek SH (2016) Body Stature as an Age-Dependent Risk Factor for Myopia in a South Korean Population. Semin Ophthalmol 32:3260336. [DOI] [PubMed] [Google Scholar]
- 2.Vitale S, Ellwein L, Cotch MF, Ferris FL 3rd, Sperduto R (2008) Prevalence of refractive error in the United States, 1999–2004. Arch Ophthalmol 126:1111–9. 10.1001/archopht.126.8.1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mutti DO, Cooper ME, O’Brien S, Jones LA, Marazita ML, Murray JC, et al. (2007) Candidate gene and locus analysis of myopia. Mol Vis 13:1012–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Yazar S, Hewitt AW, Black LJ, McKnight CM, Mountain JA, Sherwin JC, et al. (2014) Myopia is associated with lower vitamin D status in young adults. Invest Ophthalmol Vis Sci 55:4552–9. 10.1167/iovs.14-14589 [DOI] [PubMed] [Google Scholar]
- 5.Wu HM, Seet B, Yap EP, Saw SM, Lim TH, Chia KS (2001) Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optom Vis Sci 78:234–9. [DOI] [PubMed] [Google Scholar]
- 6.Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, et al. (2004) The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol 122:495–505. 10.1001/archopht.122.4.495 [DOI] [PubMed] [Google Scholar]
- 7.Wong TY, Foster PJ, Hee J, Ng TP, Tielsch JM, Chew SJ, et al. (2000) Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci 41:2486–94. [PubMed] [Google Scholar]
- 8.Saw SM, Chan YH, Wong WL, Shankar A, Sandar M, Aung T, et al. (2008) Prevalence and risk factors for refractive errors in the Singapore Malay Eye Survey. Ophthalmology 115:1713–9. 10.1016/j.ophtha.2008.03.016 [DOI] [PubMed] [Google Scholar]
- 9.Pan CW, Wong TY, Lavanya R, Wu RY, Zheng YF, Lin XY, et al. (2011) Prevalence and risk factors for refractive errors in Indians: the Singapore Indian Eye Study (SINDI). Invest Ophthalmol Vis Sci 52:3166–73. 10.1167/iovs.10-6210 [DOI] [PubMed] [Google Scholar]
- 10.Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T, Tajimi Study G (2008) Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology 115:363–70. 10.1016/j.ophtha.2007.03.075 [DOI] [PubMed] [Google Scholar]
- 11.Lee YY, Lo CT, Sheu SJ, Lin JL (2013) What factors are associated with myopia in young adults? A survey study in Taiwan Military Conscripts. Invest Ophthalmol Vis Sci 54:1026–33. 10.1167/iovs.12-10480 [DOI] [PubMed] [Google Scholar]
- 12.Jung SK, Lee JH, Kakizaki H, Jee D (2012) Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in seoul, South Korea. Invest Ophthalmol Vis Sci 53:5579–83. 10.1167/iovs.12-10106 [DOI] [PubMed] [Google Scholar]
- 13.Lee JH, Jee D, Kwon JW, Lee WK (2013) Prevalence and risk factors for myopia in a rural Korean population. Invest Ophthalmol Vis 54: 5466–5471. [DOI] [PubMed] [Google Scholar]
- 14.Low W, Dirani M, Gazzard G, Chan YH, Zhou HJ, Selvaraj P, et al. (2010) Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol 94:1012–6. 10.1136/bjo.2009.173187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lam DS, Fan DS, Lam RF, Rao SK, Chong KS, Lau JT, et al. (2008) The effect of parental history of myopia on children’s eye size and growth: results of a longitudinal study. Invest Ophthalmol Vis Sci 49:873–6. 10.1167/iovs.06-1097 [DOI] [PubMed] [Google Scholar]
- 16.Shimizu N, Nomura H, Ando F, Niino N, Miyake Y, Shimokata H (2003) Refractive errors and factors associated with myopia in an adult Japanese population. Jpn J Ophthalmol 47:6–12. [DOI] [PubMed] [Google Scholar]
- 17.Lim HT, Yoon JS, Hwang SS, Lee SY (2012) Prevalence and associated sociodemographic factors of myopia in Korean children: the 2005 third Korea National Health and Nutrition Examination Survey (KNHANES III). Jpn J Ophthalmol 56:76–81. 10.1007/s10384-011-0090-7 [DOI] [PubMed] [Google Scholar]
- 18.Konstantopoulos A, Yadegarfar G, Elgohary M (2008) Near work, education, family history, and myopia in Greek conscripts. Eye (Lond) 22:542–6. [DOI] [PubMed] [Google Scholar]
- 19.Pan CW, Klein BE, Cotch MF, Shrager S, Klein R, Folsom A, et al. (2013) Racial variations in the prevalence of refractive errors in the United States: the multi-ethnic study of atherosclerosis. A m J Ophthalmol 155:1129–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, et al. (2013) Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 120:277–83. 10.1016/j.ophtha.2012.07.086 [DOI] [PubMed] [Google Scholar]
- 21.Choi JA, Han K, Park YM, La TY (2014) Low serum 25-hydroxyvitamin D is associated with myopia in Korean adolescents. Invest Ophthalmol Vis Sci 55:2041–7. 10.1167/IOVS.13-12853 [DOI] [PubMed] [Google Scholar]
- 22.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, et al. (2008) Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115:1279–85. 10.1016/j.ophtha.2007.12.019 [DOI] [PubMed] [Google Scholar]
- 23.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. (2014) Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43: 69–77 10.1093/ije/dyt228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis TH, Complex survey data analysis with SAS. 2016: Chapman and Hall/CRC press
- 25.Kim EC, Morgan IG, Kakizaki H, Kang S, Jee D (2013) Prevalence and risk factors for refractive errors: Korean National Health and Nutrition Examination Survey 2008–2011. PLoS One 8:e80361 10.1371/journal.pone.0080361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rim TH, Kim SH, Lim KH, Choi M, Kim HY, Baek SH, et al. (2016) Refractive Errors in Koreans: The Korea National Health and Nutrition Examination Survey 2008–2012. Korean J Ophthalmol 30:214–24. 10.3341/kjo.2016.30.3.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarczy-Hornoch K, Ying-Lai M, Varma R, Los Angeles Latino Eye Study G (2006) Myopic refractive error in adult Latinos: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci 47:1845–52. 10.1167/iovs.05-1153 [DOI] [PubMed] [Google Scholar]
- 28.Rahi JS, Cumberland PM, Peckham CS (2011) Myopia over the lifecourse: prevalence and early life influences in the 1958 British birth cohort. Ophthalmology 118:797–804. 10.1016/j.ophtha.2010.09.025 [DOI] [PubMed] [Google Scholar]
- 29.Midelfart A, Kinge B, Midelfart S, Lydersen S (2002) Prevalence of refractive errors in young and middle-aged adults in Norway. Acta Ophthalmol Scand 80:501–5. [DOI] [PubMed] [Google Scholar]
- 30.Tan CS, Chan YH, Wong TY, Gazzard G, Niti M, Ng TP, et al. (2011) Prevalence and risk factors for refractive errors and ocular biometry parameters in an elderly Asian population: the Singapore Longitudinal Aging Study (SLAS). Eye (Lond) 25:1294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwon JW, Choi JA, La TY, Epidemiologic Survey Committee of the Korean Ophthalmological S (2016) Serum 25-hydroxyvitamin D level is associated with myopia in the Korea national health and nutrition examination survey. Medicine (Baltimore) 95:e5012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K (2002) Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci 43: 3633–3640 [PubMed] [Google Scholar]
- 33.Jones-Jordan LA, Sinnott LT, Manny RE, Cotter SA, Kleinstein RN, Mutti DO, et al. (2010) Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci 51:115–21. 10.1167/iovs.08-3210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K (2007) Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci 2007;48:3524–32. 10.1167/iovs.06-1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saw SM, Carkeet A, Chia KS, Stone RA, Tan DT (2002) Component dependent risk factors for ocular parameters in Singapore Chinese children. Ophthalmology 2002;109:2065–71. [DOI] [PubMed] [Google Scholar]
- 36.Saw SM, Shankar A, Tan SB, Taylor H, Tan DT, Stone RA, et al. (2006) A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci 47:1839–44. 10.1167/iovs.05-1081 [DOI] [PubMed] [Google Scholar]
- 37.Saw SM, Chua WH, Gazzard G, Koh D, Tan DT, Stone RA (2005) Eye growth changes in myopic children in Singapore. Br J Ophthalmol 89:1489–94. 10.1136/bjo.2005.071118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saw SM, Chua WH, Hong CY, Wu HM, Chan WY, Chia KS, et al. (2002) Nearwork in early-onset myopia. Ophthalmol Vis Sci 43:332–9. [PubMed] [Google Scholar]
- 39.Liang YB, Wong TY, Sun LP, Tao QS, Wang JJ, Yang XH, et al. (2009) Refractive errors in a rural Chinese adult population the Handan eye study. Ophthalmology 116:2119–27. 10.1016/j.ophtha.2009.04.040 [DOI] [PubMed] [Google Scholar]
- 40.Fernandez-Montero A, Olmo-Jimenez JM, Olmo N, Bes-Rastrollo M, Moreno-Galarraga L, Moreno-Montanes J, et al. (2015) The impact of computer use in myopia progression: A cohort study in Spain. Prev Med 71:67–71. 10.1016/j.ypmed.2014.12.005 [DOI] [PubMed] [Google Scholar]
- 41.Wang Q, Klein BE, Klein R, Moss SE (1994) Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci 1994;35:4344–7. [PubMed] [Google Scholar]
- 42.Morgan I, Rose K (2005) How genetic is school myopia? Prog Retin Eye Res 24:1–38. 10.1016/j.preteyeres.2004.06.004 [DOI] [PubMed] [Google Scholar]
- 43.Fan Q, Wojciechowski R, Kamran Ikram M, Cheng CY, Chen P, Zhou X, et al. (2014) Education influences the association between genetic variants and refractive error: a meta-analysis of five Singapore studies. Hum Mol Genet 23:546–54. 10.1093/hmg/ddt431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rose KA, Morgan IG, Smith W, Mitchell P (2002) High heritability of myopia does not preclude rapid changes in prevalence. Clin Exp Ophthalmol 30: 168–172 [DOI] [PubMed] [Google Scholar]
- 45.Mutti DO, Marks AR (2011) Blood levels of vitamin D in teens and young adults with myopia. Optom Vis Sci 88:377–82. 10.1097/OPX.0b013e31820b0385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mutti DO, Cooper ME, Dragan E, Jones-Jordan LA, Bailey MD, Marazita ML, et al. (2011) Vitamin D receptor (VDR) and group-specific component (GC, vitamin D-binding protein) polymorphisms in myopia. Invest Ophthalmol Vis Sci 52:3818–24. 10.1167/iovs.10-6534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Braegger C, Campoy C, Colomb V, Decsi T, Domellof M, Fewtrell M, et al. (2013) Vitamin D in the healthy European paediatric population. J Pediatr Gastroenterol Nutr 56:692–701. 10.1097/MPG.0b013e31828f3c05 [DOI] [PubMed] [Google Scholar]
- 48.Muller DN, Kleinewietfeld M, Kvakan H (2011) Vitamin D review. J Renin Angiotensin Aldosterone Syst 12:125–8. 10.1177/1470320311410924 [DOI] [PubMed] [Google Scholar]
- 49.Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. (2011) Vitamin D insufficiency in Korea—a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab 96:643–51. 10.1210/jc.2010-2133 [DOI] [PubMed] [Google Scholar]
- 50.Lee YA, Kim HY, Hong H, Kim JY, Kwon HJ, Shin CH, et al. (2014) Risk factors for low vitamin D status in Korean adolescents: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008–2009. Public Health Nutr 17:764–71. 10.1017/S1368980013000438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chung M, Lee J, Terasawa T, Lau J, Trikalinos TA (2011) Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 155:827–38. 10.7326/0003-4819-155-12-201112200-00005 [DOI] [PubMed] [Google Scholar]
- 52.Lepple-Wienhues A, Stahl F, Willner U, Schafer R, Wiederholt M (1991) Endothelin-evoked contractions in bovine ciliary muscle and trabecular meshwork: interaction with calcium, nifedipine and nickel. Curr Eye Res 10:983–9. [DOI] [PubMed] [Google Scholar]
- 53.Tavera-Mendoza L, Wang TT, Lallemant B, Zhang R, Nagai Y, Bourdeau V, et al. (2006) Convergence of vitamin D and retinoic acid signalling at a common hormone response element. EMBO Rep 7:180–5. 10.1038/sj.embor.7400594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Slominski AT, Kim TK, Shehabi HZ, Semak I, Tang EK, Nguyen MN, et al. (2012) In vivo evidence for a novel pathway of vitamin D(3) metabolism initiated by P450scc and modified by CYP27B1. FASEB J 26: 3901–3915. 10.1096/fj.12-208975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slominski AT, Kim TK, Li W, Tuckey RC (2016) Classical and non-classical metabolic transformation of vitamin D in dermal fibroblasts. Exp Dermatol 25: 231–232. 10.1111/exd.12872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Slominski AT, Kim TK, Li W, Postlethwaite A, Tieu EW, Tang EK, et al. (2015) Detection of novel CYP11A1-derived secosteroids in the human epidermis and serum and pig adrenal gland. Sci Rep 5: 14875 10.1038/srep14875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dirani M, Tong L, Gazzard G, Zhang X, Chia A, Young TL, et al. (2009) Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol 93:997–1000. 10.1136/bjo.2008.150979 [DOI] [PubMed] [Google Scholar]
- 58.Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ (2012) The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology 119:2141–51. 10.1016/j.ophtha.2012.04.020 [DOI] [PubMed] [Google Scholar]
- 59.Guo Y, Liu LJ, Xu L, Tang P, Lv YY, Feng Y, et al. (2013) Myopic shift and outdoor activity among primary school children: one-year follow-up study in Beijing. PLoS One 8:e75260 10.1371/journal.pone.0075260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK (2013) Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 120:1080–5. 10.1016/j.ophtha.2012.11.009 [DOI] [PubMed] [Google Scholar]
- 61.Wu PC, Tsai CL, Hu CH, Yang YH (2010) Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol 17:338–42. 10.3109/09286586.2010.508347 [DOI] [PubMed] [Google Scholar]
- 62.Read SA, Collins MJ, Vincent SJ (2014) Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci 91:330–41. [DOI] [PubMed] [Google Scholar]
- 63.McCarthy CS, Megaw P, Devadas M, Morgan IG (2007) Dopaminergic agents affect the ability of brief periods of normal vision to prevent form-deprivation myopia. Exp Eye Res 84:100–7. 10.1016/j.exer.2006.09.018 [DOI] [PubMed] [Google Scholar]
- 64.Guggenheim JA, Williams C, Northstone K, Howe LD, Tilling K, St Pourcain B, et al. (2014) Does vitamin D mediate the protective effects of time outdoors on myopia? Findings from a prospective birth cohort. Invest Ophthalmol Vis Sci 55:8550–8. 10.1167/iovs.14-15839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lin HJ, Wei CC, Chang CY, Chen TH, Hsu YA, Hsieh YC, et al. (2016) Role of Chronic Inflammation in Myopia Progression: Clinical Evidence and Experimental Validation. EBioMedicine 10:269–81. 10.1016/j.ebiom.2016.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the Korea Center for Chronic Disease and Control Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data. The authors obtained the data set from the Korea Center for Chronic Disease and Control, which owns the data. Readers can send requests for data to Tel: 82-43-719-7467 or Email: sun4070@korea.kr (Division of Health and Nutrition Survey, KCDC). Data can also be downloaded from the following website: https://knhanes.cdc.go.kr/knhanes/eng/index.do;jsessionid=Rz6lEQIMQE7y0V27jrTgtsBj1BW8sHOmiaOhJkYPQePH5kxA68xWDNCEdUzp7wj5.CDCPOWAS02_1.5_servlet_PUB.