Abstract
Introduction
Management of airway emergencies is a core skill for critical care fellows. There is no standardized training mechanism for difficult airway management among critical care fellowships, although fellows frequently cite management of airway catastrophes as an area of educational need.
Methods
Three simulation cases that are each approximately 15 minutes in length are presented. The cases represent airway emergencies encountered in the intensive care unit consisting of angioedema, endotracheal tube dislodgement, and endotracheal tube occlusion. Incorporated into the scenarios are planned incidents of interpersonal conflict requiring negotiation by the learner during a crisis event. The case descriptions are complete, with learning objectives and critical actions as well as all necessary personnel briefs and required equipment.
Results
The cases were completed over multiple simulation sessions on different days by 11 first-year critical care fellows during the 2016–2017 academic year. All participants demonstrated improvement in self-perceived confidence in airway management skills.
Discussion
The cases were felt to be realistic and beneficial and led to perceived improvement in management of airway emergencies and leadership during crisis scenarios.
Keywords: Simulation, ICU, Critical Care, Airway, Intensive Care Unit
Educational Objectives
By the end of the curriculum, first-year critical care fellows will be able to:
-
1.
Manage critical care airway emergency scenarios in a simulation setting.
-
2.
List noninvasive airway management techniques.
-
3.
Outline a systematic approach to endotracheal intubation.
-
4.
Describe a stepwise approach to endotracheal tube exchange.
-
5.
Run a debrief session with a multidisciplinary team after a crisis event.
Introduction
Management of airway emergencies is an essential skill for critical care fellows.1 For many fellow trainees, managing the airway is a daunting challenge. Training in airway management varies widely among fellowship programs, and intubations in the intensive care unit (ICU) carry particularly high rates of severe complications.2,3 Airway management is often interdisciplinary, involving nurses, respiratory therapists, and other providers in the ICU. Fellows are frequently thrust into a leadership role in emergent patient scenarios, often without formal training or developed skills. Airway complications are among the most stressful patient crises, potentially further compounding trainee apprehension in the leadership position. An internal needs assessment of pulmonary and/or critical care fellows confirmed that more training around airway complications is an educational priority. Simulation was chosen as the educational modality to provide a safe learning environment that closely replicated the complex ICU environment and allowed hands-on practice during high-stakes scenarios that incorporated health care team dynamics. In our review of the literature, we found no such curriculum for fellow education. The difficult airway curricula that exist in MedEdPORTAL are primarily focused on anesthesiology resident training.4–7 The only published curriculum specific to airway management in the ICU involves a single simulation scenario with a spontaneously breathing patient with a difficult airway due to poor glottic visualization.4 The current resource fills an educational gap by addressing important airway emergencies encountered in the ICU environment, including complications that arise with an endotracheal tube already in place, which have not been addressed in previously published curricula. In addition, there is emphasis on the multidisciplinary nature of care in the ICU environment, and the simulation scenarios require learners to lead a team in crisis scenarios.
These simulations were developed to offer critical care fellows additional practice and experience in managing three high-stakes airway emergencies that are more specific to the ICU environment: angioedema, endotracheal tube occlusion, and endotracheal tube dislodgement. The simulations require a systematic approach to intubation by the learner, specifically with an anticipated difficult airway in mind. Each scenario is approximately 15 minutes in length and utilizes SimMan (Laerdal Medical) and the Ingmar ASL-500 lung simulator as the platform, along with standard ICU equipment. The simulations are interdisciplinary, including nurses, respiratory therapists, and residents, to better reflect the true ICU environment. There are moments of conflict scripted into the scenarios to foster development of fellows' leadership skills.
Methods
Development
Three cases are included as appendices: angioedema (Appendix A), endotracheal tube dislodgement (Appendix B), and endotracheal tube occlusion (Appendix C). Each case features learning objectives, critical actions, role descriptions, patient information including physical examination and other ancillary studies, and debriefing material. The roles played by confederates representing other ICU personnel are fully defined. The scenarios assume competence in basic airway management and intubation skills, as well as understanding of a difficult airway management algorithm. In our institution, prior to the simulation session, most fellows had completed a dedicated airway rotation, learning intubation skills in the operating room, although they had not practiced managing more complex airway complications. The study was determined to be exempt by the University of Washington Institutional Review Board.
Personnel
We targeted content to first-year critical care fellows and introduced key principles of airway management, with a focus on emergent complications. We designed the cases for two fellows to participate: the lead fellow and the support fellow. The lead fellow was primarily responsible for the management of the case, and the support fellow provided procedural or other accessory support as directed by the lead fellow. We also incorporated confederate staff, including nurses, respiratory therapists, residents, interns, and a faculty observer, to improve the realism of the ICU scenario.
Equipment/Environment
We developed the scenarios for use in a simulated ICU room including a manikin with intubation and mechanical ventilation capabilities. In addition, we used a lung simulator to drive the mechanical ventilator. We displayed the patient's vital signs on a monitor visible to participants so that dynamic changes could readily be seen. Individual simulations had specific equipment needs, although each included items commonly encountered in the ICU.
Implementation
At our institution, we implemented the three scenarios as part of four half-day simulation courses distributed throughout the academic year for first-year critical care fellows. Each simulation session included one of the three difficult airway management scenarios as well as two to three other critical care management scenarios. Survey data were collected following the sessions at the beginning of the academic year (session 1) and the end of the academic year (session 4). We provided a brief orientation to the fellows before the scenarios. Two critical care fellows (one lead fellow and one support fellow) took part in each simulation using a simulated ICU room, with confederates representing additional ICU staff. We represented the patient using SimMan (Laerdal Medical) and the Ingmar ASL-500 lung simulator attached to a ventilator at the manikin's bedside. The remaining fellows observed the simulation in real time along with faculty members. We instructed the lead fellow to conduct a team debrief with the simulated team at the end of the simulation. Finally, the participating fellows joined the observing fellows and faculty for a facilitated discussion of the observed clinical management and leadership behaviors.
Assessment
We evaluated fellows completing the simulations using the critical actions checklist. The checklist components were integrated into each act of the simulation scenarios as a prompt to the facilitator. The incorporated critical action steps did not necessarily occur within the act but were meant to cue the facilitator to the relative time points for the critical interventions. The included debriefing material is designed to encompass the components of the critical actions checklist and can be used by faculty to provide formative feedback to learners while also highlighting the key aspects of clinical management. We evaluated participants' subjective experiences with a survey distributed at the end of the sessions held at the beginning of the academic year (session 1) and the end of the academic year (session 4). The survey questions specific to the difficult airway management scenarios are included in Appendix D.
Debriefing
While staying in character, the lead fellow led a clinical debrief with the patient care team after each scenario. After the clinical debrief, the entire team reconvened in an adjacent conference room where the faculty led fellows through a debrief of both the leadership and medical management aspects of the case. In our practice, we typically gave the lead fellow the first opportunity to share reflections on the case, specifically as to what aspects went well and what could be done better. Other fellows and faculty then contributed to the discussion with regard to the important leadership aspects of the case as well as the medical management.
Results
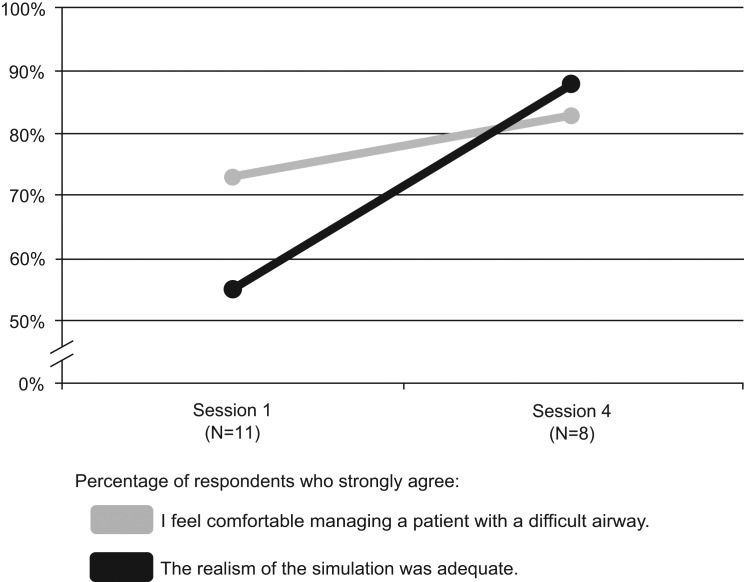
During the 2016–2017 academic year, all first-year fellows in the pulmonary and critical care program completed the airway emergency simulations as part of an ICU emergencies simulation curriculum. A total of 11 critical care fellows experienced the curriculum during four half-day sessions throughout the academic year. Comparing session 1 at the beginning of the academic year to session 4 at the end, self-perceived comfort in managing patients with difficult airways increased from 73% in strong agreement to 83% (see the Figure). The perceived realism of the simulation also improved over the course of the academic year, with 55% of fellows in strong agreement after session 1 and 88% in strong agreement after session 4 (see the Figure). The improvement in perceived realism reflects changes made to the curriculum to increase verisimilitude, including modifications to the manikin and the environment. Anonymous fellow comments described the debriefing of medical and leadership skills as “invaluable” and the specific practice in airway emergencies as “high yield.”
Figure. Fellow perceptions following simulation sessions. Session 1 was completed at the beginning of the academic year, and session 4 was completed at the end of the academic year. A survey (Appendix D) was distributed after completion of session 1 and again after completion of session 4.
Sample comments from the fellows included the following:
-
•
“I think leadership is hard to refine without being in actual situations so I really enjoy the simulations.”
-
•
“The case-based simulations sessions have been INCREDIBLE—arguably the best educational experience I have had in medicine.”
-
•
“I enjoy these simulations, although they do make me quite nervous being on the spot and watched by co-fellows and attendings. Not sure how to minimize that feeling, but I get over it. Better to feel dumb during a simulation than in real life.”
-
•
“This was a great workshop. I felt like it was nonthreatening and allowed me to hone my leadership skills.”
Discussion
Implementation of a simulation curriculum for first-year critical care fellows focused on airway emergencies is feasible and was well received by our trainees. At our institution, the simulation sessions have become a core component of the first-year critical care fellowship curriculum. After fellows participated in the simulations, their self-perceived confidence in these skills improved. In addition, the ability to manage a team and negotiate conflict during high-stakes settings was seen as highly advantageous.
During the first year of implementation, fellows were assigned to be the lead fellow for a particular simulation. Based on feedback, participation as the lead fellow was changed to a volunteer system in subsequent years, while still ensuring that all fellows rotated through the leadership role.
We found simulation of angioedema to be the most difficult scenario with regard to realism of the manikin. Our manikin was unable to display any external physical findings such as swollen or discolored lips, which we overcame by securing red pieces of foam on the manikin's lips as cues to the participants. Prior to all simulation sessions, the fellows were encouraged to suspend reality so as to be able to engage fully in the simulation environment. This included remaining in character during the clinical debrief sessions in order to practice words and phrases they might use in actual leadership roles.
There are several limitations to our curriculum. First, the total number of learners assessed during the curriculum was small, making evaluation difficult. The small size of the learner cohort, however, reflects the goal of focused education specifically for critical care fellow trainees, which necessitates inherently small programs by its nature. While the simulation content is oriented to first-year critical care fellows, the scenarios could be adapted to other learner groups, such as residents in anesthesiology, emergency medicine, internal medicine, and general surgery. Second, learner assessment was limited by evaluating changes in perceived comfort. Improvement in self-reported comfort with management of difficult airway scenarios is confounded by a maturation effect, as progression in fellowship alone could have accounted for the improvement. Ideally, assessment of skill or knowledge acquisition would be performed to evaluate the effect of the curriculum, although our use of the curriculum was primarily that of formative development and these specific metrics were not captured. The included critical actions checklists could be used in a more rigorous manner to demonstrate skill acquisition if desired. Third, the presented scenarios focus on the management of difficult airway scenarios by encouraging the learner to progress through an algorithmic approach during a time of crisis. Two of the three scenarios conclude in surgical airways by design, reflecting the goal of progressing through the airway management approach to the final common pathway. Since the emphasis is on clinical reasoning, the trainees did not actually perform simulated surgical airways, although the scenarios could be adapted to include this. Finally, there are other points during the scenarios where training in technical skills could be further emphasized, such as intubation over a bronchoscope during the endotracheal tube dislodgement scenario. We chose not to include these specific skill maneuvers during the simulation scenarios as they are assessed elsewhere in the fellowship program at our institution.
Appendices
A. Angioedema Simulation Case.docx
B. Endotracheal Tube Dislodgement Simulation Case.docx
C. Endotracheal Tube Occlusion Simulation Case.docx
D. Postscenario Survey.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
None to report.
Prior Presentations
Steinbach TC, Adamson R, Carlbom D, Johnson NJ, Kritek PA, Çoruh B. Leadership education for critical care fellows using simulation. Presented at: American Thoracic Society (ATS) International Conference; May 24, 2017; Washington, DC.
Ethical Approval:
The University of Washington Institutional Review Board approved this study.
References
- 1.Fessler HE, Addrizzo-Harris D, Beck JM, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: report of a multisociety working group. Chest. 2014;146(3):813–834. https://doi.org/10.1378/chest.14-0710 [DOI] [PubMed] [Google Scholar]
- 2.Joffe AM, Liew EC, Olivar H, et al. A national survey of airway management training in United States internal medicine-based critical care fellowship programs. Respir Care. 2012;57(7):1084–1088. https://doi.org/10.4187/respcare.01540 [DOI] [PubMed] [Google Scholar]
- 3.Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34(9):2355–2361. https://doi.org/10.1097/01.CCM.0000233879.58720.87 [DOI] [PubMed] [Google Scholar]
- 4.Murray A, Konia M. ICU difficult airway simulation. MedEdPORTAL. 2010;6:8091 https://doi.org/10.15766/mep_2374-8265.8091 [Google Scholar]
- 5.Straker T, Vick A. Simultaneous resident and faculty evaluation of an airway objective structured clinical examination (OSCE). MedEdPORTAL. 2011;7:9020 https://doi.org/10.15766/mep_2374-8265.9020 [Google Scholar]
- 6.Lefebvre C, Manthey D. Advanced airway management classroom course. MedEdPORTAL. 2014;10:9960 https://doi.org/10.15766/mep_2374-8265.9960 [Google Scholar]
- 7.Lombaard S, Metzner J, Ross B, Kim S, Sherman M. Team training: unanticipated difficult airway. MedEdPORTAL. 2008;4:1654 https://doi.org/10.15766/mep_2374-8265.1654 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Angioedema Simulation Case.docx
B. Endotracheal Tube Dislodgement Simulation Case.docx
C. Endotracheal Tube Occlusion Simulation Case.docx
D. Postscenario Survey.docx
All appendices are peer reviewed as integral parts of the Original Publication.