Abstract
Background: Surgical thoracic outlet syndrome (TOS) management involves decompression of the neurovascular structures by releasing the anterior and/or middle scalene muscles, resection of the first and/or cervical ribs, or a combination. Various surgical approaches (transaxillary, supraclavicular, infraclavicular, and transthoracic) have been used with varying rates of complications. The purpose of this study was to evaluate early postoperative outcomes following surgical decompression for TOS. We hypothesized that first and/or cervical rib resection would be associated with increased 30-day complications and health care utilization. Methods: The American College of Surgeons National Surgical Quality Improvement Program database was reviewed for all TOS cases of brachial plexus surgical decompression in the region of the thoracic inlet from 2005 to 2013. Results: There were 225 patients (68% females; mean age: 36.4 years ± 12.1; 26% body mass index [BMI] ⩾ 30). There were 205 (91%) patients who underwent first and/or cervical rib resection (±scalenectomy), and 20 (9%) underwent rib-sparing scalenectomy. Compared with rib-sparing scalenectomy, rib resection was associated with longer operative time and hospital stays (P < .001). In the 30 days postoperatively, 8 patients developed complications (rib-scalenectomy, n = 7). Only patients with rib resection returned to the operating room (n = 10) or were readmitted (n = 9). Conclusions: Early postoperative complications are infrequent after TOS decompression. Rib resection is associated with longer surgical times and hospital stays. Future studies are needed to assess the association between early and long-term outcomes, surgical procedure, and health care utilization to determine the cost-effectiveness of the various surgical interventions for TOS.
Keywords: thoracic outlet syndrome, outcome, complications, cohort, surgery, rib resection, scalenectomy
Introduction
Compression of neurovascular structures located in the region of the thoracic inlet, specifically the brachial plexus, subclavian artery, and/or subclavian vein, can produce a collection of symptoms that are clinically termed thoracic outlet syndrome (TOS).1-3 Symptoms arising from neurogenic TOS include upper limb paresthesia, pain, and muscle weakness, and are often precipitated or exacerbated by prolonged and abnormal postures, neck trauma, hypertrophy of neck musculature, and bony or soft tissue anomalies.2,3
The primary treatment approach for TOS is nonoperative management addressing postural abnormalities and muscle imbalances in the cervicoscapular region.2 When nonoperative management fails to provide symptom relief, operative treatment to decompress the constricting region involves release of the anterior and/or middle scalene muscles, resection of the first and/or cervical ribs, or a combination.4 To access the operative site, multiple surgical approaches have been described, including transaxillary, supraclavicular, infraclavicular, and transthoracic approaches.5 The type of operative management and the specific approach have varying rates of complications, such as pneumothorax, and neurovascular injuries to the subclavian vessels, brachial plexus, and long thoracic, intercostobrachial and phrenic nerves.6
Previous studies that have evaluated outcomes following surgical decompression of the brachial plexus have provided little emphasis on the cost-effectiveness and health economics aspect of the surgical interventions. The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) has instituted a prospective database of surgical procedures and this database has been used to assess 30-day outcomes of numerous surgical procedures.7-10 The NSQIP data have not been used to investigate the postoperative outcomes following surgical decompression for TOS.
The purpose of this study was to evaluate the incidence of early postoperative outcomes (complications and health care utilization) within 30 days following surgical decompression of the neurovascular structures in the region of the thoracic inlet, and secondarily to identify risk factors associated with these complications. We hypothesized that resection of the first and/or cervical rib would be associated with increased 30-day complications and health care utilization.
Methods
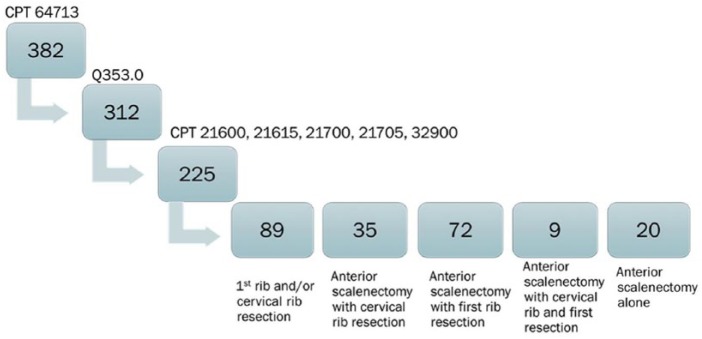
Following institutional review board approval, the NSQIP database was used to conduct a retrospective study on all cases of surgical decompression of the brachial plexus in the region of the thoracic inlet from 2005 to 2013. The NSQIP database contains perioperative surgical data collected from hospitals located in the United States and Canada. The Current Procedural Terminology (CPT) code 64713 was used to identify patients who underwent neuroplasty of peripheral nerves. Patients with brachial plexus lesions were identified based on the International Classification of Diseases, Ninth Revision (ICD-9) diagnostic code Q353.0. Patients who underwent surgical procedures associated with these CPT and ICD-9 codes included first and/or cervical rib resection, scalenectomy or combined rib resection and scalenectomy were identified and selected for analysis (Figure 1).
Figure 1.
Algorithm for patient selection.
Note. CPT = Current Procedural Terminology.
Data were collected on demographics (age, sex, body mass index [BMI], and year of surgery), health descriptors (American Society of Anesthesiology [ASA] physical status classification, functional status, emergent surgery, alcohol use, and smoking status), comorbidities (bleeding disorder, chronic obstructive pulmonary disease, diabetes, dyspnea, hypertension, sepsis, and steroid use), and 30-day outcomes (duration of surgery, length of hospital stay, types of complications, complications based on the NSQIP classification system, and return to care). The NSQIP complication classification system consisted of the following categories: surgical, major, infectious, adverse, and overall complications. Data were imported into SPSS version 20, and outcomes of interest were compared between patients who underwent first and/or cervical rib resection and those who had rib-sparing scalenectomy.
Results
There were 225 patients who underwent surgical decompression of the brachial plexus in the region of the thoracic inlet from 2005 to 2013, with the highest frequency of surgical management in 2010 (26.2% of included surgeries) (Table 1). The mean age of the patient population was 36.4 ± 12.1 years, 154 (68.4%) were females, 128 (56.9%) were overweight or obese based on BMI, and 28 (12.4%) met the ASA class 3 severe systemic disease physical status classification. Comorbidities and other health descriptors are reported in Table 1. None of these factors were associated with the overall complications.
Table 1.
Demographic Characteristics and Comorbidities; Total Sample (N = 225).
| Variable | Patients |
|---|---|
| Age | |
| Mean, years (± SD) | 36.4 (±12.1) |
| Sex, n (%) | |
| Female | 154 (68.4) |
| Male | 70 (31.1) |
| NR | 1 (0.4) |
| Body mass index, n (%) | |
| Underweight (<18.5) | 7 (3.1) |
| Normal (18.5-24.9) | 89 (39.6) |
| Overweight (25-29.9) | 70 (31.1) |
| Obese (⩾30) | 58 (25.8) |
| NR | 1 (0.4) |
| American Society of Anesthesiology Physical Status Classification, n (%) | |
| Class 1: Healthy patient | 39 (17.3) |
| Class 2: Mild systemic disease | 158 (70.2) |
| Class 3: Severe systemic disease | 28 (12.4) |
| Functional status, n (%) | |
| Partially dependent | 3 (1.3) |
| Independent | 222 (98.7) |
| Emergency surgery, n (%) | |
| Yes | 2 (0.9) |
| No | 223 (99.1) |
| Bleeding disorder, n (%) | |
| Yes | 21 (9.3) |
| No | 204 (90.7) |
| COPD (severe), n (%) | |
| Yes | 4 (1.8) |
| No | 221 (98.2) |
| Diabetes, n (%) | |
| Insulin | 2 (0.9) |
| Noninsulin/oral agent | 5 (0.9) |
| No | 218 (96.9) |
| Dyspnea, n (%) | |
| At rest | 1 (0.4) |
| Moderate exertion | 15 (6.7) |
| No | 209 (92.9) |
| Hypertension requiring medication, n (%) | |
| Yes | 44 (19.6) |
| No | 181 (80.4) |
| Alcohol use, n (%) | |
| Yes | 3 (1.3) |
| No | 176 (78.2) |
| NR | 46 (20.4) |
| Smoking, n (%) | |
| Yes | 42 (18.7) |
| No | 183 (81.3) |
| Steroid use (chronic), n (%) | |
| Yes | 2 (0.9) |
| No | 223 (99.1) |
| Year of surgery, n (%) | |
| 2005 | 6 (2.7) |
| 2006 | 15 (6.7) |
| 2007 | 19 (8.4) |
| 2008 | 21 (9.3) |
| 2009 | 42 (18.7) |
| 2010 | 59 (26.2) |
| 2011 | 12 (5.3) |
| 2012 | 24 (10.7) |
| 2013 | 27 (12.0) |
Note. NR = not recorded; COPD = chronic obstructive pulmonary disease.
Eighty-nine patients (28.6%) had first and/or cervical rib resection, 20 (6.4%) had rib-sparing anterior scalenectomy, 35 (16.6%) had anterior scalenectomy with cervical rib resection, 72 (23.2%) had anterior scalenectomy with first rib resection, and 9 (2.9%) had anterior scalenectomy with first and cervical ribs resection (Table 2). Overall, 205 (91.1%) of the study sample underwent rib resection (±scalenectomy), and 20 (6.4%) had rib-sparing scalenectomy.
Table 2.
Operative Management to Decompress Thoracic Inlet.
| Type of operative management | Patients, N = 225 (%) |
|---|---|
| First rib and/or cervical rib resection (CPT 21615 or 21600 or 32900)a,b | 89 (39.6) |
| Anterior scalenectomy without cervical rib resection (CPT 21700) | 20 (8.9) |
| Anterior scalenectomy with cervical rib resection (CPT 21705) | 35 (15.6) |
| Anterior scalenectomy with first rib resection (CPT 21615 + 21700)c | 72 (32.0) |
| Anterior scalenectomy with cervical rib and first rib resection ([CPT 21615 OR 32900] + 21705]b,d | 9 (4.0) |
Note. CPT = Current Procedural Terminology.
Includes 1 patient who underwent partial rib resection (CPT 21600).
Includes 1 patient with potentially multiple thoracic ribs resection (CPT 32900).
Assumed CPT 21615 to indicate first rib resection because CPT 21700 precludes cervical rib resection.
Assumed to be both cervical and first rib resection because CPT 21705 includes cervical rib resection; therefore, CPT 21615 must indicate first rib resection.
Patients who underwent first and/or cervical rib resection had significantly longer surgical operative time (mean 221.7 minutes vs 154.1 minutes, P < .001) and longer hospital stays (mean 4.2 days vs 2.9 days, P < .001) compared with patients who did not have a rib resection (Table 3).
Table 3.
Duration of Care Measures.
| Measure | Mean (SD) | Rib resection, n = 205 Mean (SD); median (range) |
Rib-sparing, n = 20 Mean (SD); median (range) |
P valuea |
|---|---|---|---|---|
| Length of surgery (min) |
215.65 (103.5) | 221.7 (105.5); 204.0 (689.0) | 154.1 (49.2); 142.5 (193) | .000 |
| Length of stay (days) |
4.10 (2.0) | 4.2 (2.0); 4 (12.0) | 2.9 (2.2); 2.0 (7.0) | .000 |
Shapiro-Wilk tests were conducted to assess normality; P < .05 obtained across both groups for both measures. Normality assumption was rejected, and Mann-Whitney U tests were conducted for pairwise comparison.
In the 30-day postoperative period, there were no occurrences of mortality, pulmonary embolism, myocardial infarction, cerebrovascular incident, or renal failure (Table 4). Both the sepsis and septic shock occurred in patients who also had superficial surgical site infections. Although no significant association between rib resection and specified complications was detected, all complications occurred in patients who underwent rib resections, excluding one superficial surgical site infection.
Table 4.
Types of Complications.
| Type | Patients, N = 225 (%) | N events | Rib resection patients, n = 205 (%) | Rib-sparing patients, n = 20 (%) | P valuea |
|---|---|---|---|---|---|
| Superficial surgical site infection | 4 (1.8) | 4 | 3 (1.5) | 1 (5.0) | .313 |
| Organ space surgical site infection | 1 (0.4) | 1 | 1 (0.5) | 0 (0) | 1.000 |
| Unplanned intubation | 1 (0.4) | 1 | 1 (0.5) | 0 (0) | 1.000 |
| Transfusion (intraoperatively or postoperatively) | 2 (0.9) | 2 | 2 (1.0) | 0 (0) | 1.000 |
| Sepsis | 1 (0.4) | 1 | 1 (0.5) | 0 (0) | 1.000 |
| Septic shock | 1 (0.4) | 1 | 1 (0.5) | 0 (0) | 1.000 |
| Any complication | 8 (3.6) | 10 | 7 (3.4) | 1 (5.0) | .551 |
P values obtained from Fisher exact test.
Based on the NSQIP complication classification, there were 8 patients (3.6%) with 10 overall complications, 8 patients (3.6%) with 9 surgical complications, 5 (2.2%) with 6 major complications, 5 (2.2%) with an adverse event, and 1 (0.4%) with an infectious complication (Table 5). No significant association was found between complication and adverse events, and operative management. However, of the 8 patients with overall or surgical complications, 7 underwent rib resection; of the 5 patients with major complications or adverse events, all 5 had rib resection; and the only patient with infectious complication (organ space infection) also had rib resection.
Table 5.
NSQIP Complication Classification.
| Classification | Patients, N = 225 (%) | N events | Rib resection patients, n = 205 (%) | Rib-sparing patients, n = 20 (%) | P valuea |
|---|---|---|---|---|---|
| Overall complications | 8 (3.6) | 10 | 7 (3.4) | 1 (5.0) | .551 |
| Surgical complications | 8 (3.6) | 9 | 7 (3.4) | 1 (5.0) | .531 |
| Major complications | 5 (2.2) | 6 | 5 (2.4) | 0 (0) | 1.000 |
| Infectious complications | 1 (0.4) | 1 | 1 (0.5) | 0 (0) | 1.000 |
| Adverse events | 5 (2.2) | 5 | 5 (2.4) | 0 (0) | 1.000 |
Note. NSQIP = National Surgical Quality Improvement Program.
P values obtained from Fisher exact test.
Ten patients (4.4%) after rib resection returned to the operating room (Table 6), and all readmissions from 2011 to 2013 occurred in patients following rib resection.
Table 6.
Return to Care Measures.
| Measure | Patients, N = 225 (%) | Rib resection patients, n = 205 (%) | Rib-sparing patients, n = 20 (%) | P valuea |
|---|---|---|---|---|
| Return to operating room | 10 (4.4) | 10 (4.9) | 0 (0) | .606 |
| Readmission to hospitalb | 9/63 (14.3) | 9/59 (15.3) | 0/4 (0) | 1.000 |
P values obtained from Fisher exact test.
Variable available for 2011 and onwards only, n = 4 for rib-sparing group, n = 59 for rib resection group.
Discussion
The NSQIP data provide information on a large, heterogeneous cohort of patients from across the United States and Canada. This study has highlighted that operative management of TOS is infrequent and the most common surgical intervention provided to relieve TOS symptoms is rib resection; only 6.4% patients had rib-sparing scalenectomies. Overall, the 30-day postoperative complications recorded by NSQIP are relatively rare after decompression of the brachial plexus in the thoracic inlet for TOS. Rib resection is associated with significantly longer surgical times and length of stay in hospital. All postoperative complications and return to hospital and operating room, with the exception of one superficial surgical site infection, occurred in patients with rib resection. This association was not statistically significant, which may be related to the low number of complications and requires further investigation in a larger sample size.
In a study of the current practice of TOS decompression, Rinehardt et al reviewed the NSQIP database and selected all cases of first or cervical rib resection.11 In our study, we initially used the CPT code 64713 to identify patients who underwent neuroplasty of peripheral nerves and the ICD-9 code to identify brachial plexus lesions and then the specific codes for rib resection and scalenectomy. In our subset of patients, we found low risk of complications which is similar to the results reported by Rinehardt et al. Similar to our study, Cheng et al found rib resection compared with scalenectomy was associated with longer hospital stays (mean 5.1 days vs 3.9 days, respectively).12 In another study that evaluated patients following rib-sparing scalenectomy and neurolysis, most were discharged within 24 hours and reported high satisfaction with results.13
Sanders compared outcomes following TOS decompression (between 1965 and 1988) with transaxillary first rib resection, supraclavicular first rib resection (with scalenectomies), and supraclavicular scalenectomies only, and found similar success rates among all groups, with 90% of patients experiencing improvement in symptoms postoperatively, and 65% maintaining these results 15 years following surgery.2,5,14-17 In another literature review by Sanders et al, no significant difference in symptom relief and functional improvement was reported following these surgeries.18 In a study by Landry et al, 79 patients were examined at a mean of 4.2 years after first rib resection surgery and approximately 34% of patients reported improvement in symptoms, but this did not significantly differ from patients who were managed nonoperatively,19 showing limited benefit of first rib resection. In another study, negative predictors of good functional outcome included extended first rib resection, acute ischemia, and sensory or motor deficit and severe postoperative complications.20
In contrast to the similar functional outcomes after any surgical management for TOS, differences in complications have been reported depending on the type of surgical management and approach. In a retrospective review of a national inpatient database, rib resection for neurogenic TOS, an overall low complication rate was reported.21 In one surgeon’s experience, first rib resection via a transaxillary approach led to a 10% incidence of pneumothorax, with half requiring insertion of chest tubes.22 The incidence of a pneumothorax was reported as high as 23% to 33% in other studies.23,24 Transaxillary first rib resection also presents risk of iatrogenic injury to the intercostobrachial nerves, long thoracic nerve, and C8 and T1 plexus roots.6,22,25 Although supraclavicular surgeries have their own risks, such as Horner syndrome, thoracic duct injury, and phrenic nerve traction,6,22,25 the incidence of long-lasting or severe complications is reported to be less, particularly in the absence of first rib resection.12,13,26,27
Functional outcome may not differ significantly between first rib resection and scalenectomy. However, the risk of postoperative complications may be higher with first rib resection, particularly with the transaxillary approach. Studies have identified supraclavicular scalenectomies to be the primary procedure in the decompression of TOS12,14,26-29; in the majority of TOS cases, the pathology involves compression between the scalene muscles.18,22,26 It has been suggested that first rib resection is effective only because it involves anterior and middle scalenotomy.18
Controversy remains regarding the selection of the optimal surgical approach for TOS. Some studies have suggested supplementing a supraclavicular scalenectomy with first rib resection to reduce the risk of recurrence and repeat surgeries.12,28,30 In contrast, other studies have suggested that first rib resection may lead to a higher rate of recurrence due to increased scar tissue deposition,12 particularly if a rib remnant remains.31 Sanders et al have advised removing the first rib only when anomalous and symptomatic (eg, previous rib fracture creating a callous,22 or when accompanied/fused with the cervical rib).26,32 Overall, it is essential to distinguish symptomatology resulting from compression of the brachial plexus and vessels from first and/or cervical ribs versus the scalene muscles.
The primary strength of this study is the utilization of a national prospective database, and it provides data on a large cohort of patients from a multicenter perspective, which increases the generalizability. There are limitations to this study. Because this is a retrospective study, selection bias is present based on our algorithm for identifying patients. Bias may also be present in the selection of patients for surgical intervention and the procedure performed (surgical approach: scalenectomy vs rib resection) dependent on surgical specialty and surgeon preference. Correlation of some data to the morbidity observed could not be analyzed, such as the specific surgical approach used (eg, transaxillary vs supraclavicular), as these data were not recorded. It could not be distinguished which patients had middle scalenectomy. Because only specific complications are recorded by the NSQIP data set,33 it is possible that complications specific to TOS surgical decompression were not captured, such as pneumothorax and nerve traction/injuries, particularly if these did not lead to readmission or return to the operating room. Despite using data from a national database, this study may be underpowered due to the low frequency of complications and may not detect differences in complications and return-to-care measures. A few recent studies have questioned the predictive value of the NSQIP database, after comparing the NSQIP complication rate with their institutional rates.34,35
This study found that first and/or cervical rib excision results in longer surgical times and hospital stays than other operative managements. Literature review is suggestive of limited functional gain from first rib excision in TOS. In the current era of health economics and cost-effectiveness, the utility of first and/or cervical rib resection for TOS needs to be re-considered. These data highlight the importance of proper preoperative evaluation to determine the location and etiology of compression to direct surgical management that reduces morbidity for patients and utilization of limited health care resources. It remains crucial to recognize the symptoms of TOS, and that surgical management can result in tremendous improvements in quality of life.36 Thus it is important to provide appropriate surgical management when deemed necessary. Further research studies emphasizing a combination of early and long-term patient outcomes and health care utilization are warranted to determine the cost-effectiveness of the various surgical interventions for TOS. Ultimately, this would enable expert consensus on appropriate patient selection and standardization of surgical management to provide patients with optimal outcome.
Footnotes
Authors’ Note: This work was presented at American Society of Peripheral Nerve, 2017 Annual Meeting, Kona, Hawaii.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kuhn JE, Lebus VG, Bible JE. Thoracic outlet syndrome. J Am Acad Orthop Surg. 2015;23:222-232. [DOI] [PubMed] [Google Scholar]
- 2. Novak CB. Thoracic outlet syndrome. Clin Plast Surg. 2003;30:175-188. [DOI] [PubMed] [Google Scholar]
- 3. Watson LA, Pizzari T, Balster S. Thoracic outlet syndrome part 1: clinical manifestations, differentiation and treatment pathways. Man Ther. 2009;14:586-595. [DOI] [PubMed] [Google Scholar]
- 4. Atasoy E. Combined surgical treatment of thoracic outlet syndrome: transaxillary first rib resection and transcervical scalenectomy. Handchir Mikrochir Plast Chir. 2006;38:20-28. [DOI] [PubMed] [Google Scholar]
- 5. Sanders RJ, Haug CE. Thoracic Outlets Syndrome: A Common Sequela of Neck Injuries. Philadelphia, PA: J.B. Lippincott; 1991. [Google Scholar]
- 6. Leffert RD. Complications of surgery for thoracic outlet syndrome. Hand Clin. 2004;20:91-98. [DOI] [PubMed] [Google Scholar]
- 7. Bronheim RS, Oermann EK, Cho SK, et al. Coagulation profile as a risk factor for 30-day morbidity and mortality following posterior lumbar fusion. Spine. 2017;42:950-957. [DOI] [PubMed] [Google Scholar]
- 8. Caras RJ, Lustik MB, Kern SQ, et al. Preoperative albumin is predictive of early postoperative morbidity and mortality in common urologic oncologic surgeries. Clin Genitourin Cancer. 2017;15:e255-e262. [DOI] [PubMed] [Google Scholar]
- 9. Cassie S, Okrainec A, Saleh F, et al. Laparoscopic versus open elective repair of primary umbilical hernias: short-term outcomes from the American College of Surgeons National Surgery Quality Improvement Program. Surg Endosc. 2014;28:741-746. [DOI] [PubMed] [Google Scholar]
- 10. Su HK, Ozbek U, Likhterov I, et al. Safety of transoral surgery for oropharyngeal malignancies: an analysis of the ACS NSQIP. Laryngoscope. 2016;126:2484-2491. [DOI] [PubMed] [Google Scholar]
- 11. Rinehardt EK, Scarborough JE, Bennett KM. Current practice of thoracic outlet decompression surgery in the United States. J Vasc Surg. 2017;66:858-865. [DOI] [PubMed] [Google Scholar]
- 12. Cheng SW, Reilly LM, Nelken NA, et al. Neurogenic thoracic outlet decompression: rationale for sparing the first rib. Cardiovasc Surg. 1995;3:617-623; discussion 624. [DOI] [PubMed] [Google Scholar]
- 13. Mattson RJ. Surgical approach to anterior scalenectomy. Hand Clin. 2004;20:57-60. [DOI] [PubMed] [Google Scholar]
- 14. Mackinnon SE, Novak CB. Thoracic outlet syndrome. Curr Probl Surg. 2002;39:1070-1145. [DOI] [PubMed] [Google Scholar]
- 15. Sanders RJ. Results of the surgical treatment for thoracic outlet syndrome. Semin Thorac Cardiovasc Surg. 1996;8:221-228. [PubMed] [Google Scholar]
- 16. Sanders RJ, Hammond SL. Complications and results of surgical treatment for thoracic outlet syndrome. Chest Surg Clin N Am. 1999;9:803-820. [Google Scholar]
- 17. Sanders RJ, Pearce WH. The treatment of thoracic outlet syndrome: a comparison of different operations. J Vasc Surg. 1989;10:626-634. [DOI] [PubMed] [Google Scholar]
- 18. Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist. 2008;14:365-373. [DOI] [PubMed] [Google Scholar]
- 19. Landry GJ, Moneta GL, Taylor LM, Jr, et al. Long-term functional outcome of neurogenic thoracic outlet syndrome in surgically and conservatively treated patients. J Vasc Surg. 2001;33:312-317; discussion 317-319. [DOI] [PubMed] [Google Scholar]
- 20. Degeorges R, Reynaud C, Becquemin JP. Thoracic outlet syndrome surgery: long-term functional results. Ann Vasc Surg. 2004;18:558-565. [DOI] [PubMed] [Google Scholar]
- 21. Chang DC, Lidor AO, Matsen SL, et al. Reported in-hospital complications following rib resections for neurogenic thoracic outlet syndrome. Ann Vasc Surg. 2007;21:564-570. [DOI] [PubMed] [Google Scholar]
- 22. Atasoy E. A hand surgeon’s further experience with thoracic outlet compression syndrome. J Hand Surg Am. 2010;35:1528-1538. [DOI] [PubMed] [Google Scholar]
- 23. Leffert RD, Perlmutter GS. Thoracic outlet syndrome. Results of 282 transaxillary first rib resections. Clin Orthop Relat Res. 1999;368:66-79. [PubMed] [Google Scholar]
- 24. Orlando MS, Likes KC, Mirza S, et al. A decade of excellent outcomes after surgical intervention in 538 patients with thoracic outlet syndrome. J Am Coll Surg. 2015;220:934-939. [DOI] [PubMed] [Google Scholar]
- 25. Christo PJ, McGreevy K. Updated perspectives on neurogenic thoracic outlet syndrome. Curr Pain Headache Rep. 2011;15:14-21. [DOI] [PubMed] [Google Scholar]
- 26. Sanders RJ, Hammond SL. Supraclavicular first rib resection and total scalenectomy: technique and results. Hand Clin. 2004;20:61-70. [DOI] [PubMed] [Google Scholar]
- 27. Sharan D, Moulton A, Greatrex GH, et al. Two-surgeon approach to thoracic outlet syndrome: long-term outcome. J R Soc Med. 1999;92:239-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Atasoy E. A hand surgeon’s advanced experience with thoracic outlet compression syndrome. Handchir Mikrochir Plast Chir. 2013;45:131-150. [DOI] [PubMed] [Google Scholar]
- 29. Wehbe MA, Leinberry CF. Current trends in treatment of thoracic outlet syndrome. Hand Clin. 2004;20:119-121. [DOI] [PubMed] [Google Scholar]
- 30. Likes KC, Orlando MS, Salditch Q, et al. Lessons learned in the surgical treatment of neurogenic thoracic outlet syndrome over 10 years. Vasc Endovascular Surg. 2015;49:8-11. [DOI] [PubMed] [Google Scholar]
- 31. Hooper TL, Denton J, McGalliard MK, et al. Thoracic outlet syndrome: a controversial clinical condition. Part 2: non-surgical and surgical management. J Man Manip Ther. 2010;18:132-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sanders RJ, Hammond SL. Management of cervical ribs and anomalous first ribs causing neurogenic thoracic outlet syndrome. J Vasc Surg. 2002;36:51-56. [DOI] [PubMed] [Google Scholar]
- 33. American College of Surgeons. User Guide for the 2014 ACS NSQIP Participant Use Data File (PUF). 2015. https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2014.ashx. Accessed August 22, 2018.
- 34. Prasad KG, Nelson BG, Deig CR, et al. ACS NSQIP risk calculator: an accurate predictor of complications in major head and neck surgery? Otolaryngol Head Neck Surg. 2016;155:740-742. [DOI] [PubMed] [Google Scholar]
- 35. Slump J, Ferguson PC, Wunder JS, et al. Can the ACS-NSQIP surgical risk calculator predict post-operative complications in patients undergoing flap reconstruction following soft tissue sarcoma resection? J Surg Oncol. 2016;114:570-575. [DOI] [PubMed] [Google Scholar]
- 36. Chang DC, Rotellini-Coltvet LA, Mukherjee D, et al. Surgical intervention for thoracic outlet syndrome improves patient’s quality of life. J Vasc Surg. 2009;49:630-635; discussion 635-637. [DOI] [PubMed] [Google Scholar]