Abstract
Background
Geriatric acetabular fractures require fixation with sufficient primary stability to allow for immediate full-weight bearing. Minimally-invasive procedures would be desirable in order to keep perioperative morbidity low. The purpose of this study was to compare the biomechanical strength of lag screw-only fixation of anterior column posterior hemi-transverse (ACPHT) acetabular fractures to standard anatomical plate fixation.
Methods
Standardized ACPHT fractures were created in fourth generation synthetic pelvis models and stabilized by either an anatomical buttress plate (n = 4) or by a screw-only construct (n = 4). In a validated setup, a cyclic loading protocol was applied with increasing axial force (3200 cycles, 175 N to 2250 N). Construct survival, acetabular fracture motion, and mode of failure were assessed.
Results
The median number of cycles needed until failure of the construct occurred was 2304 cycles (range, 2020 to 2675) in the plate fixation group and 3200 cycles (range, 3101 to 3200) for the screw fixation constructs (p = .003). With regard to energy absorbed until failure, the plate fixation group resisted to 1.57 × 106 N*cycles (range, 1.21 × 106 to 2.14 × 106) and the screw fixation group to 3.17 × 106 N*cycles (range, 2.92 × 106 to 3.17 × 106; p = .001). All plate fixation specimens failed with a break-out of the posterior-column screw in the quadrilateral wing of the anatomical plate within a maximum load of 1750 N while the screw fixation constructs all survived loading of at least 2100 N. Acetabular fracture gap motion, acetabular rim angle, and medial femoral head subluxation as measures of fracture displacement were all not different between the two groups (p > 0.1).
Conclusions
In this in vitro biomechanical study, screw-only fixation of an ACPHT acetabular fracture resulted in at least as good construct survival as seen for standard buttress plate fixation. Both methods resisted sufficiently to forces that would be expected under physiologic conditions.
Electronic supplementary material
The online version of this article (10.1186/s12891-019-2422-6) contains supplementary material, which is available to authorized users.
Keywords: Acetabular fracture; Acetabulum; Pelvis; Osteoporosis; Biomechanical screw fixation, plate fixation
Background
Demographic changes in industrialized countries come along with an increase in fragility fractures [1]. The combination of impaired bone quality and a loss of postural stability frequently [2, 3] results in geriatric low-energy fractures also of the acetabulum, typically Judet and Letournel type anterior column posterior hemitransverse fractures (ACPHT) [4].
While the general principles of articular fracture reduction and fixation also apply to fragility fractures of the acetabulum, the goals can be different with injuries in the young. The aim is to restore the function of the hip joint, allow pain-free early mobilization to reduce the complications of bed rest, decrease early mortality and minimize the risk of post-traumatic arthritis. However, most geriatric patients may not be able to follow a postoperative partial weight-bearing regimen [5] and immobilization over more than a few days is associated with increased in-hospital complications [6] and mortality [7]. Hence, it is important to achieve an early and stable fixation to allow for immediate full weight bearing [8]. Second, surgical interventions too invasive may be associated with increased perioperative morbidity and mortality in elderly patients. Especially with open procedures, acetabular fractures in the elderly are associated with noticeable post-operative complication rates [9]. Thus, instead of open reduction and plate fixation, percutaneous procedures using screw-only constructs have been advocated [6, 10, 11].
There is much debate, however, about the standard fixation of ACPHT fractures and whether screw fixation alone is biomechanically stable enough in order to allow for immediate postoperative full-weight bearing. While there are biomechanical studies on the strength of different acetabular plate fixation constructs, only few address type ACPHT fractures [12, 13] and – to the authors’ knowledge – a direct comparison of plate and screw fixation is yet missing.
Hence, the purpose of this study was to compare the biomechanical strength of a lag screw-only fixation to a standard anatomical plate fixation of an ACPHT acetabular fracture in an in vitro experimental setup.
Methods
Specimens
Eight fourth-generation composite hemipelves (Sawbones; Pacific Research Laboratories, Vashon, WA, USA) were used for this biomechanical investigation.
Standardized left-sided acetabular fractures, Judet & Letournel type anterior column posterior hemi-transverse (ACPHT), were created and the specimens were randomly assigned to either screw or plate fixation (Fig. 1 A + B):
Fig. 1.
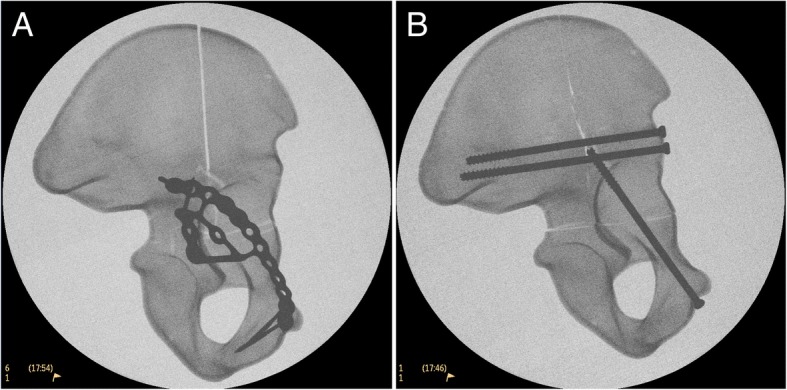
Testing samples. In the plate fixation group (a) an anatomically pre-shaped plate with a quadrilateral buttress was applied and fixed to the three fragments of a standardized ACPHT acetabular fracture using 3.5-cortical screws. In the screw fixation group (b), fracture configuration fixed using two 6.5 mm-cannulated LC2-screws and one 6.5 mm-cannulated retrograde anterior column screw
In the plate fixation group (n = 4), the fracture was reduced and an anatomical acetabular steel plate with quadrilateral buttress was applied (PRO Suprapectineal Plate, Stryker, Selzach, Switzerland) and fixed with seven 3.5 mm bicortical screws (at least two screws in each of the three fragments).
In the screw fixation group (n = 4), the fracture was reduced and one cannulated steel screw (6.5 mm, 32 mm-partially-threaded; DePuySynthes, West Chester, PA, USA) was inserted in terms of a retrograde anterior column screw and another two screws were placed along the supraacetabular canal in terms of two LC2-screws [10, 14].
Biomechanical testing
The experimental setup was designed to provoke implant failure or loosening of the screws by fatigue or damage accumulation in the area of the bone-implant interface [15]. The samples underwent mechanical testing of a previously described setup [16–18] using a universal testing machine (Zwick GmbH & Co, Ulm, Germany. Fig. 2). Each specimen was subjected to consecutive cyclic loadings at 1 Hz beginning with a sinusoidal axial force from 17.5 to 170 N. After every 500 cycles, the axial load was increased to simulate higher walking stresses (partial weight-bearing, full weight-bearing, climbing steps, stumbling) up to 1750 N and after that every 100 cycles up to 2250 N (Table 1). The force was applied in medio-superior direction through an endoprosthetic femoral head component on the left acetabulum [16]. Both ilium and pubic symphysis were allowed to freely rotate on the testing setup. Grease was used to decrease friction between the load applicator and the acetabular joint surface. Before testing, all specimens were pre-loaded with 175 N to level out initial subsidence.
Fig. 2.
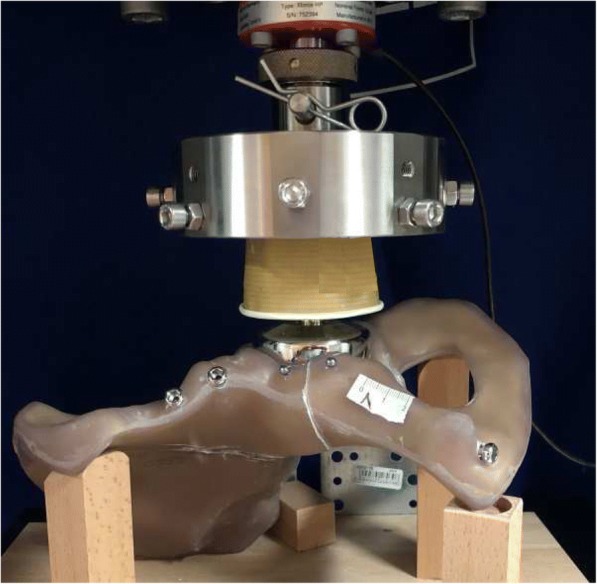
Testing setup. On an universal testing machine cyclic loadings were applied on the acetabular joint surface through an endoprosthetic femoral head that was linked to a load cell
Table 1.
Cyclic loading protocol
| Cycles | Load range (N) | |
|---|---|---|
| Min | Max | |
| 0–500 | 17.5 | 175 |
| 501–1000 | 35 | 350 |
| 1001–1500 | 70 | 700 |
| 1501–2000 | 105 | 1050 |
| 2001–2500 | 140 | 1400 |
| 2501–3000 | 175 | 1750 |
| 3001–3100 | 210 | 2100 |
| 3101–3200 | 245 | 2450 |
Visual markers were attached to the pelvis models prior to testing and digital imaging was obtained to allow for later opto-metric analysis.
Construct failure was defined as either a sudden loss of force resistance over 30% or visual breackage of the model or femoral head dislocation resulting in an immediate stop of testing.
Outcome variables
(1) Primary outcome parameter was construct survival, measured in cycles [n] to failure (as defined above) and in energy absorbed by the construct [N*cycles], defined as the number of cycles to failure multiplied with the force each cycle was applied with.
(2) Secondary outcome parameters were measures of acetabular fracture motion and were assessed opto-metrically between every series of cycles under loading with 175 N by the use of the calibration and caliper tool of ImageJ2 [19], including
acetabular fracture gap [mm], defined as width of the interfragmentary intrapelvic cortical gap just above the dome (Fig. 3),
acetabular rim angle [°], defined as the angle between the pubic and iliac part of the anterior acetabular rim, and
medial femoral head subluxation [mm], defined as the change in distance between the acetabular rim and the endoprosthetic femoral head component’s center of rotation.
Fig. 3.
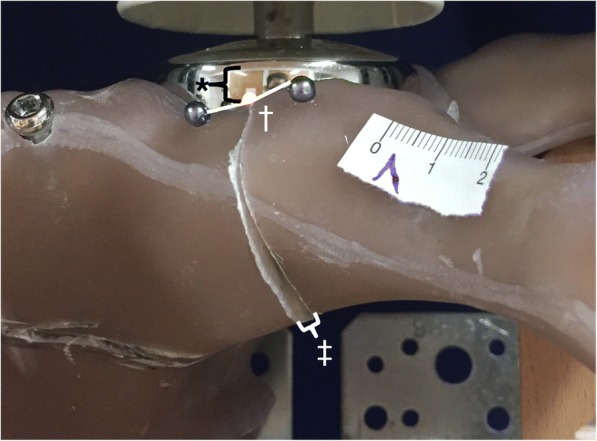
Measurement of fracture displacement. As measures of fracture displacement, the acetabular fracture gap (‡), the acetabular rim angle (†), and the medial femoral head subluxation (*) were measured under loading with 175 N every between every series of cycles
In case of construct failure, parameters of fracture displacement were assessed one last time under loading with 175 N. Hence, data was obtained only for the first five rounds of cyclic loading.
(3) An additional descriptive outcome parameter was the mode of failure.
Statistical analysis
Primary outcome was construct survival. It was our hypothesis that screw fixation provides comparable stability as plate fixation within the load ranges of partial weight-bearing (maximum 2.0 body weights [20]), but not beyond this. Hence, with an anticipated non-inferiority margin of 200′000 N*cycles, assuming a standard deviation of ±10% and with a significance level of α = 0.05 and a desired power of 0.80, a sample size calculation revealed a minimum sample size of 4 per group [21].
Post-test analysis was done using SPSS for Windows V25.0 (IBM, Chicago, IL, USA). All data is reported as medians with the minimum and maximum value (range). Parametric tests were used to compare differences between the two groups. The level of significance was defined as p < 0.05.
Results
Construct survival
The median number of cycles needed until failure of the construct occurred was 2304 cycles (range 2020 to 2675) in the plate fixation group and 3200 cycles (range, 3101 to 3200) for the screw fixation constructs (p = .003, Fig. 4). When comparing the median product of achieved cycles and force as a measure of energy absorbed until failure, the plate fixation group resisted to 1.57 × 106 N*cycles (range, 1.21 × 106 to 2.14 × 106) and the screw fixation group to 3.17 × 106 N*cycles (range, 2.92 × 106 to 3.17 × 106; p = .001).
Fig. 4.
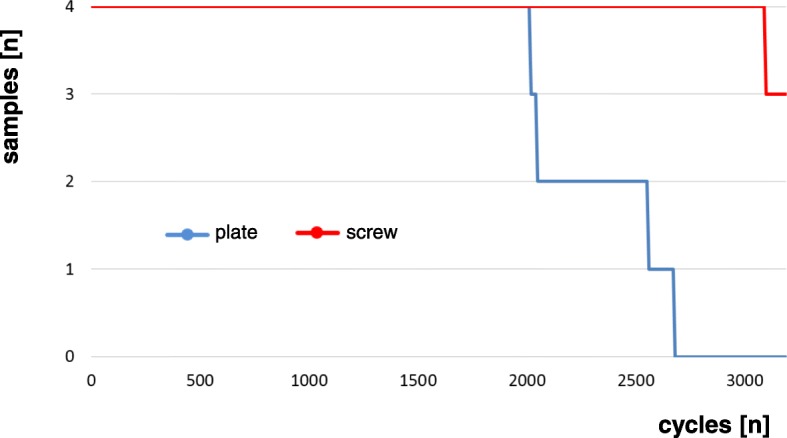
Construct survival
All specimens survived the first 2000 cycles of cyclic loading with up to 1050 N. All plate fixation specimens failed within the subsequent 1000 cycles with a maximum load of 1750 N. The screw fixation samples all survived loading up to 2100 N and 3 of 4 samples also survived the highest loading with 2450 N (Fig. 4).
Acetabular fracture gap
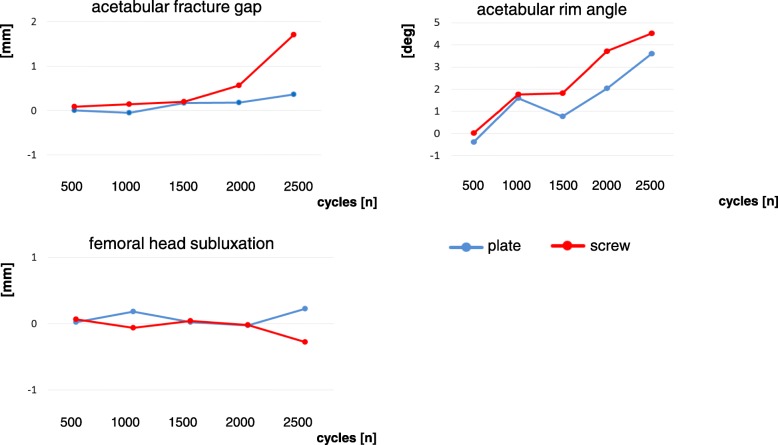
The increase in acetabular fracture gap formation under loading with 175 N was not statistically different between the two groups after 500 cycles (p = .704), 1000 cycles (p = .826), 1500 cycles (p = .196), 2000 cycles (p = .125), and 2500 cycles (p = .244, Fig. 5).
Fig. 5.
Fracture displacement
Acetabular rim angle
The decrease in acetabular rim angle formation was not statistically different between the two groups after 500 (p = .740), 1000 (p = .824), 1500 (p = .834), 2000 (p = .151), and 2500 (p = .651, Fig. 5).
Medial femoral head subluxation
The change in femoral head position relative to the acetabular rim was not statistically different at 500 cycles (p = .126), 1000 (p = .123), 1500 (p = .576), 2000 (p = .638), and 2500 (p = .120, Fig. 5).
Mode of failure
With regard to the mode of failure, all plate fixation constructs failed with a break-out of the posterior-column screw in the quadrilateral wing of the anatomical plate. This resulted in an angular posterior opening of the fracture gap and bending of the rim-part of the plate (Fig. 6A). None of the screw fixation constructs showed implant failure or cut-out of the screws. One construct failed by sudden loosening of the screw with an audible crack and widening of the fracture gap (Fig. 6A).
Fig. 6.
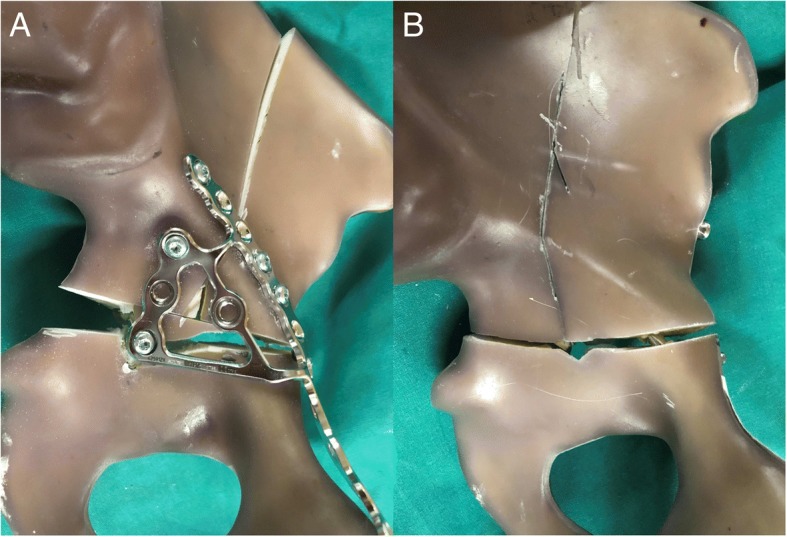
Mode of failure. All plate fixation constructs showed a very similar pattern of failure with a break-out of the posterior-column screw in the buttress-wing of the plate and consecutive opening of the fracture gap (a) None of the screw fixation constructs showed a sudden failure in terms of an implant cut-out but rather stepwise implant loosening and widening of the fracture gap (b)
Discussion
The purpose of this study was to compare the biomechanical strength of lag screw-only fixation versus a standard anatomical buttress plate fixation.
Most studies available investigated different screw and plate fixation constructs and found those to provide high degrees of stiffness and strength in the stabilization of acetabular fractures [16, 22, 23].
In our investigation, we observed superior strength and construct survival of the screw fixation technique. This is in line with findings of a biomechanical study on screw versus plate fixation constructs in iliac crescent fractures [24].
Kistler et al. [16] compared a combination of lag screw and column plates to the same quadrilateral surface buttress plate as used in our study in a very similar experimental setup. Their findings are consistent with our results in the plate fixation group. Before conducting their study in synthetic bone models, they had validated the setup in human cadaver pelvises [16].
The same setup for the testing of acetabular fracture fixation strength was also used by other studies [18, 25]. As, in the authors opinion, fracture fixation failure is a result of repetitive loads and not so much of sudden catastrophic loads, we did not test for load to failure. Instead, the number of cycles was expanded and cyclic loads up to 3.5 body weights were applied in order to approximate the conditions of full weight bearing [26].
This study was an in vitro study using synthetic bone models. The use of synthetic models brings limitations. There is a lack of surrounding soft tissues, which alters the physiological and anatomical behaviour compared to cadaver pelves or the biomechanics in real life. Next to economic and ethical considerations, we chose fourth generation Sawbone models for the advantage of better standardization in construct behaviour. The advantages of using a synthetic model are the homogeneous bone structure and the elimination of individual bone quality as a potential bias [12, 13, 27]. In addition, the pelvic models used in this study had previously been validated against osteoporotic human cadaver bone [16] and, hence, a similar setup has been used by other studies [18, 25]. It would be of interest, though, to repeat these tests with cadaver pelvises in order to assess the influence of different degress of bone quality.
In vitro studies can approximate the effect of fatigue on primary stability but they cannot provide information about the bone’s behaviour through healing and rehabilitation. The samples in this study were loaded to up to 3.5 body weights which may not be realistic in the context of postoperative painful mobilization, although some patients will reach these loads by accident [5].
Acetabular fracture gap, acetabular rim angle, and medial femoral head subluxation were not different between the two groups. However, the patterns of stress distribution may differ noticeably between the two fixation methods tested and the behaviour of acetabular fracture gap, rim angle, and medial femoral head subluxation may not be fully comparable. Construct survival is a result of all these three factors and, in addition, is a measure of the vulnerability of a construct to means of fatigue and accumulated failure. The most relevant finding of this study may not be a potential superiority of the screw fixation technique over a certain type of plate fixation. There are many other ways to use a plate in order to stabilize an acetabulum and the one investigated here may not be the strongest. More importantly, screw-only fixation seems to provide sufficient resistance to the forces that can be expected during immediate full-weight bearing. These in vitro data are in line with the findings in clinical cohorts. Stöckle et al. [28] observed a loss of reduction in only three of 51 fractures during a 2 year follow-up after acetabular fracture fixation with only 3.5 mm screws. Similar results were seen in a small cohort of 13 elderly patients with acetabular fractures treated with lag-screw fixation [11].
Future prospective clinical studies comparing percutaneous versus open fixation of this entity of acetabular fractures may help to identify potential candidates for the less-invasive technique.
Conclusions
In this in vitro biomechanical study, screw-only fixation of an ACPHT acetabular fracture resulted in at least as good construct survival as seen for standard buttress plate fixation. Both methods resisted sufficiently to forces that would be expected under physiologic conditions. Fixation of ACPHT fractures seems to be a biomechanically valid alternative, where a less invasive treatment is needed.
Additional file
Source data. This file provides measurement raw data of the sample testing. (PDF 45 kb)
Acknowledgements
Not applicable.
Funding
There is no external funding source.
Availability of data and materials
Source data is attached as electronic file in Additional file 1.
Abbreviations
- ACPHT
Anterior column and posterior hemi-transverse
- LC2
Young & Burgess lateral compression fracture type 2
Authors’ contributions
TB performed the biomechanical testing and participated in drafting the manuscript. MT, RP and PC participated in designing the study, helped with the testing setup and revised the manuscript. HCP participated in designing the study and revised the manuscript, GO had the idea for the study, participated in designing the study, helped with the testing setup and the biomechanical testing, did the statistical analysis and wrote the first draft of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
N/A
Consent for publication
N/A
Competing interests
GO is Associated Editor of BMC Musculoskeletal Disorders and has given payed lectures for Stryker & Co. The other authors declare that they have no conflicts of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tatjana Busuttil, Email: tatjana.busuttil@gmail.com.
Michel Teuben, Email: michel.teuben@usz.ch.
Roman Pfeifer, Email: roman.pfeifer@usz.ch.
Paolo Cinelli, Email: paolo.cinelli@usz.ch.
Hans-Christoph Pape, Email: hans-christoph.pape@usz.ch.
Georg Osterhoff, Email: georg.osterhoff@medizin.uni-leipzig.de.
References
- 1.Ferguson TA, Patel R, Bhandari M, et al. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J bone and joint surgery British volume. 2010;92(2):250–257. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 2.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Segev-Jacubovski O, Herman T, Yogev-Seligmann G, et al. The interplay between gait, falls and cognition: can cognitive therapy reduce fall risk? Expert Rev Neurother. 2011;11(7):1057–1075. doi: 10.1586/ern.11.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hessmann MH, Nijs S, Rommens PM. Acetabulumfrakturen im Alter Ergebnisse eines differenzierten Behandlungskonzeptes (Acetabular fractures in the elderly. Results of a sophisticated treatment concept) Unfallchirurg. 2002;105(10):893–900. doi: 10.1007/s00113-002-0437-0. [DOI] [PubMed] [Google Scholar]
- 5.Ruckstuhl T, Osterhoff G, Zuffellato M, et al. Correlation of psychomotor findings and the ability to partially weight bear. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:6. doi: 10.1186/1758-2555-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mouhsine E, Garofalo R, Borens O, et al. Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury. 2005;36(11):1330–1336. doi: 10.1016/j.injury.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 7.Kilci O, Un C, Sacan O, et al. Postoperative mortality after hip fracture surgery: a 3 years follow up. PLoS One. 2016;11(10):e0162097. doi: 10.1371/journal.pone.0162097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gänsslen A. Biomechanische Grundlagen bei osteoporotischer Frakturversorgung am Becken (biomechanical principles for treatment of osteoporotic fractures of the pelvis) Unfallchirurg. 2010;113(4):272–280. doi: 10.1007/s00113-010-1763-2. [DOI] [PubMed] [Google Scholar]
- 9.Jeffcoat DM, Carroll EA, Huber FG, et al. Operative treatment of acetabular fractures in an older population through a limited ilioinguinal approach. J Orthop Trauma. 2012;26(5):284–289. doi: 10.1097/BOT.0b013e31821e10a2. [DOI] [PubMed] [Google Scholar]
- 10.Starr AJ, Reinert CM, Jones AL. Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma. 1998;12(1):51–58. doi: 10.1097/00005131-199801000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Starr AJ, Jones AL, Reinert CM et al. (2001) Preliminary results and complications following limited open reduction and percutaneous screw fixation of displaced fractures of the acetabulum. Injury 32 Suppl 1: SA45–50. [DOI] [PubMed]
- 12.Spitler CA, Kiner D, Swafford R, et al. Generating stability in elderly acetabular fractures-a biomechanical assessment. Injury. 2017;48(10):2054–2059. doi: 10.1016/j.injury.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Culemann U, Holstein JH, Köhler D, et al. Different stabilisation techniques for typical acetabular fractures in the elderly--a biomechanical assessment. Injury. 2010;41(4):405–410. doi: 10.1016/j.injury.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Starr AJ, Borer DS, Reinert CM. Technical aspects of limited open reduction and percutaneous screw fixation of fractures of the acetabulum. Oper Tech Orthop. 2001;11(3):218–226. doi: 10.1016/S1048-6666(01)80008-2. [DOI] [Google Scholar]
- 15.Osterhoff G, Dodd AE, Unno F, et al. Cement augmentation in sacroiliac screw fixation offers modest biomechanical advantages in a cadaver model. Clin Orthop Relat Res. 2016;474(11):2522–2530. doi: 10.1007/s11999-016-4934-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kistler BJ, Smithson IR, Cooper SA, et al. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation? Clin Orthop Relat Res. 2014;472(11):3353–3361. doi: 10.1007/s11999-014-3800-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olson SA, Kadrmas MW, Hernandez JD, et al. Augmentation of posterior wall acetabular fracture fixation using calcium-phosphate cement: a biomechanical analysis. J Orthop Trauma. 2007;21(9):608–616. doi: 10.1097/BOT.0b013e3181591397. [DOI] [PubMed] [Google Scholar]
- 18.Khajavi K, Lee AT, Lindsey DP, et al. Single column locking plate fixation is inadequate in two column acetabular fractures. A biomechanical analysis. J Orthop Surg Res. 2010;5:30. doi: 10.1186/1749-799X-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rueden CT, Schindelin J, Hiner MC, et al. ImageJ2: ImageJ for the next generation of scientific image data. BMC Bioinformatics. 2017;18(1):529. doi: 10.1186/s12859-017-1934-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergmann G, Graichen F, Rohlmann A, et al. Realistic loads for testing hip implants. Biomed Mater Eng. 2010;20(2):65–75. doi: 10.3233/BME-2010-0616. [DOI] [PubMed] [Google Scholar]
- 21.Chow S, Shao J, Wang H. Sample size calculations in clinical research. In: CRC biostatistics series. 2nd ed. Boca Raton, FL: Chapman & Hall; 2008.
- 22.Sawaguchi T, Brown TD, Rubash HE, et al. Stability of acetabular fractures after internal fixation. A cadaveric study. Acta Orthop Scand. 1984;55(6):601–605. doi: 10.3109/17453678408992404. [DOI] [PubMed] [Google Scholar]
- 23.Shazar N, Brumback RJ, Novak VP, et al. Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Relat Res. 1998;(352):215–22. [PubMed]
- 24.Simonian PT, Routt ML, Harrington RM, et al. The unstable iliac fracture: a biomechanical evaluation of internal fixation. Injury. 1997;28(7):469–475. doi: 10.1016/S0020-1383(97)00112-5. [DOI] [PubMed] [Google Scholar]
- 25.Olsen MA, Nepple JJ, Riew KD, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90(1):62–69. doi: 10.2106/JBJS.F.01515. [DOI] [PubMed] [Google Scholar]
- 26.Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech. 2001;34(7):859–871. doi: 10.1016/S0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 27.Widmer BJ, Peters CL, Bachus KN, et al. Initial stability of the acetabular fragment after periacetabular osteotomy: a biomechanical study. J Pediatr Orthop. 2010;30(5):443–448. doi: 10.1097/BPO.0b013e3181e00c24. [DOI] [PubMed] [Google Scholar]
- 28.Stöckle U, Hoffmann R, Nittinger M, et al. Screw fixation of acetabular fractures. Int Orthop. 2000;24(3):143–147. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Source data. This file provides measurement raw data of the sample testing. (PDF 45 kb)
Data Availability Statement
Source data is attached as electronic file in Additional file 1.