ABSTRACT
Background: Finding precise definitions of secondary traumatic stress, vicarious traumatization, and compassion fatigue is not easy. While some researchers define these terms differentially, others use them interchangeably. In the present review, we refer to all three phenomena as secondary traumatization.
Objectives: This systematic review aims to provide an overview of prevalence rates of secondary traumatization in first responders and to shed light on corresponding resilience and risk factors.
Methods: After identifying 219 studies within the searched databases and 2192 references via hand searching, 31 studies were included in this review. We systematically searched the electronic databases PubMed, PsychINFO, and PSYNDEX (German database). The following inclusion criteria were applied: (1) participants had to be first responders working on-site: police officers, firefighters, search and rescue personnel, or emergency and paramedic team members; (2) secondary traumatization (secondary traumatic stress/vicarious traumatization/compassion fatigue) was assessed quantitatively with a validated questionnaire or subscale explicitly measuring secondary traumatization; and (3) English or German language original papers.
Results: We found low levels of secondary traumatization in first responders. Several studies describe protective and risk factors for secondary traumatization, including pretraumatic (e.g. age, gender), peritraumatic (e.g. exposure, emotional exhaustion), and post-traumatic factors (e.g. social support, alcohol and tobacco use).
Conclusion: Next to an immunizing effect, the low prevalence of secondary traumatization in first responders could be explained by social desirability and job-loss concerns. Therefore, we may be underestimating the prevalence of secondary traumatization in first responders. Some resilience (social support) and risk factors (female gender) are consistent with previous research in other populations. However, owing to the cross-sectional study designs, we must interpret resilience and risk factors with caution. Future research should focus on longitudinal study designs and preventive as well as curative interventions.
KEYWORDS: First responders, secondary traumatization, vicarious traumatization, compassion fatigue, systematic review
HIGHLIGHTS
• First responders showed low levels of secondary traumatization, possibly due to an immunization effect. • Prevalence of secondary traumatization may be underestimated owing to social desirability and job-loss concerns. • Females show higher levels of secondary traumatization than males. • Secondary traumatization correlates with burnout and post-traumatic stress disorder (PTSD). • Risk factors include pretraumatic (e.g. higher age), peritraumatic (exposure, emotional exhaustion), and post-traumatic factors (lack of social support, alcohol and tobacco use).
Abstract
Antecedentes: No es fácil encontrar definiciones precisas de estrés traumático secundario, traumatización vicaria y fatiga de compasión. Mientras algunos investigadores definen estos términos de forma diferencial, otros los usan indistintamente. En esta revisión consideramos estos tres fenómenos como traumatización secundaria.
Objetivos: Esta revisión sistemática tiene por objetivo proveer de una visión general de la prevalencia de tasas de traumatización secundaria en personal encargado de prestar primeros auxilios y aclarar los factores de riesgo y resiliencia relacionadas.
Mtodos: Tras identificar 219 estudios en búsquedas en bases de datos y 2192 referencias identificadas a través de búsqueda manual, 31 estudios fueron incluidos en esta revisión. Sistemáticamente buscamos en las bases de datos electrónicas: PubMed, PsychInfo y PSYNDEX (base de datos alemana). Se aplicaron los siguientes criterios de inclusión: (1) los participantes tenían que ser personas encargadas de prestar primeros auxilios en terreno: oficiales de policía, bomberos, personal de búsqueda y socorristas, equipos paramédicos y de emergencia, (2) traumatización secundaria (estrés traumático secundario/traumatización vicaria/fatiga de compasión) evaluada cuantitativamente con un cuestionario o sub-escala validados para medir explícitamente traumatización secundaria, (3) artículos originales en inglés o alemán.
Resultados: Encontramos bajos niveles de traumatización secundaria en personal encargado de prestar primeros auxilios. Varios estudios describen factores de protección y de riesgo para traumatización secundaria, incluyendo factores pre- (ej. edad, género), peri- (ej. exposición, agotamiento emocional), y post-traumáticos (ej. apoyo social, uso de tabaco y alcohol).
Conclusión: Además de un efecto inmunizante, la baja prevalencia de traumatización secundaria en personal encargado de prestar primeros auxilios podría ser explicada por aceptación social y preocupaciones respecto a pérdida de empleo. Por lo tanto, podríamos estar subestimando la prevalencia de traumatización secundaria en esta población. Algunos factores de resiliencia (apoyo social) y de riesgo (género femenino) son consistentes con investigaciones previas en otras poblaciones. Sin embargo, al tratarse de diseños de estudios transversales, debemos interpretar la resiliencia y factores de riesgo con cautela. Investigaciones futuras deberían enfocarse en estudios de tipo longitudinal así como también en intervenciones preventivas y curativas.
PALABRAS CLAVE: personal primeros auxilios, traumatización secundaria, traumatización vicaria, fatiga de compasión, revisión sistemática
Abstract
背景: 对二次创伤应激、替代性创伤和同情疲劳进行精确定义并不容易。虽然一些研究人员对这些术语进行了不同的定义,但其他人使用中将它们互换。其在本综述中,我们将所有三种现象称为‘二次创伤’。
目标:本系统综述旨在概述急救人员出现二次创伤的患病率,并阐明相应的韧性和风险因素。
方法:在检索数据库中识别219项研究,通过手工检索识别2192项参考文献后,本研究纳入了31项研究。我们系统地检索了电子数据库PubMed,PsychInfo和PSYNDEX(德国数据库)的。采用以下纳入标准:(1)参与者必须是现场工作的急救人员:警察,消防员,搜救员,急救和护理团队,(2)二次创伤(二次创伤应激/替代性创伤/同情疲劳)是使用经验证的问卷或者子量表(3)英语或德语原始论文。
结果:我们发现急救人员的二次创伤水平较低。一些研究描述了二次创伤的保护和风险因素,包括创伤前(例如年龄,性别),创伤短期(例如暴露、情绪衰竭)和创伤后因素(例如社会支持、酒精和烟草使用)。
结论:除了免疫效果之外,急救人员中二次创伤的低患病率可以是因为社会期望和失业问题的考虑。因此,我们可能低估了急救人员中二次创伤的患病率。一些韧性(社会支持)和风险因素(女性)与之前在其他人群中的研究一致。然而,由于横断面研究设计,我们必须谨慎地解释弹性和风险因素。未来的研究应侧重于纵向研究设计以及预防性和治疗性干预。
Abbreviations: CF, compassion fatigue; CFST, Compassion Fatigue Self-Test; CS, compassion satisfaction; CS/CFST, Compassion Satisfaction/Compassion Fatigue Self-Test; DSM, Diagnostic and Statistical Manual of Mental Disorders; ProQOL, Professional Quality of Life Scale; PTSD, post-traumatic stress disorder; STS, secondary traumatic stress; STSS, Secondary Traumatic Stress Scale; STQ, Secondary Trauma Questionnaire; VT, vicarious traumatization.
关键词: 急救人员, 二次创伤, 替代性创伤, 同情疲劳, 系统性综述
1. Introduction
1.1. First responders: definition, tasks, and challenges
First responders protect and preserve ‘life, property, and the environment’ (Prati & Pietrantoni, 2010a) immediately after accidents and disasters. This definition typically encompasses specifically trained professionals and volunteers in traditional first responders’ groups, such as police officers, firefighters, search and rescue personnel, as well as emergency and paramedic teams (Argentero & Setti, 2011; Hargrave, 2010). As part of their job profiles, these different groups fulfil different roles when responding to a critical incident: emergency and paramedic teams attend to the casualties’ physical needs, while the police and firefighters generally take charge of safety issues and order among bystanders. However, all first responder groups have in common that they are among the first to be present at an incident and often the very first to attend to the victims following a traumatic event (Kleim & Westphal, 2011). First responders are therefore routinely exposed to emotionally challenging and unpredictable situations (Benedek et al., 2007). In a study by Alexander and Klein (2001), more than 80% of paramedics reported having experienced an ‘extraordinarily disturbing incident’ in the past 6 months. Unsurprisingly, the regular experience of life-threatening and potentially traumatic situations, working with survivors and their families, and the frequent recovery of the dead and injured may overwhelm the individuals’ capability to adapt and cope, resulting in high levels of stress. This elevated stress level may lead to mental and physical changes (Herman, 1997), such as emotional exhaustion, irritability, sleep disturbances, fatigue, problems with interpersonal relationships (Mahoney, 1997; Thoreson, Miller, & Krauskopf, 1989), concerns for individual safety (Eriksson, Kemp, Gorsuch, Hoke, & Foy, 2001), and even intrusive images (Burns, Morley, Bradshaw, & Domene, 2008). Hence, all facts considered, first responders themselves may be at high risk of developing symptoms of traumatization (Setti & Argentero, 2012).
1.2. Secondary traumatization
Figley (1983) was the first to describe the phenomenon of secondary traumatization, which he defined ‘as the stress deriving from helping others who are suffering or who have been traumatized’ (Figley, 1999, p. 10). He proposed that individuals who are in contact with trauma survivors might develop a traumatic response without having experienced a traumatic event themselves. Symptoms may be provoked by either repeated or extreme confrontation with details from a traumatic event without direct sensory impressions, often delayed in time. The latest version of the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition, DSM-5) (American Psychiatric Association, 2013) includes this concept as a potential aetiological origin within its definition of post-traumatic stress disorder (PTSD): individuals must either have experienced a traumatic event themselves or have been confronted with aversive details of a traumatic situation. In the late 1980s, the first questionnaire was developed explicitly to assess secondary traumatization (Figley, 1995). Before then, primary post-traumatic stress measures were used to assess both primary and secondary traumatization (Hargrave, 2010). As the two constructs only correlate moderately with each other, unsurprisingly, primary trauma measures do not seem to capture secondary traumatization in its full extent (Motta, Newman, Lombardo, & Silverman, 2004).
The terms secondary traumatic stress (STS) disorder, compassion fatigue (CF), and vicarious traumatization (VT) are used to describe these symptoms in the existing literature. While some researchers use these terms interchangeably, others make distinct definitions (Bourke & Craun, 2014). However, some definitions are overlapping, if not contradictory. Craig and Sprang (2010, p. 320) suggest a rough differentiation between STS/CF and VT, delimiting STS/CF as ‘socioemotional symptoms’ and VT as ‘changes in cognitive schemata’.
More particularly, STS describes symptoms identical to PTSD (intrusive symptoms, avoidance, and hyperarousal), also including depressive and anxiety symptoms. These symptoms are seen as natural and consequential to the first responders’ work environment (Bride, 2007). Compassion stress is defined as a normal reaction to helping and working with trauma survivors. It enfolds the feeling of helplessness, confusion, isolation, and symptoms of STS. An enduring or cumulative exposure to compassion stress may lead to CF, a ‘state of exhaustion and dysfunction, biologically, and emotionally’ (Figley, 1995, p. 253). Individuals are no longer able to feel and express sincere understanding, empathy, and support for others (Hofmann, 2009). In some publications, STS and CF are seen as interchangeable with regard to context, while others define CF as the combination of STS and burnout symptoms (Adams, Boscarino, & Figley, 2006). Vicarious traumatization (VT) was described by Pearlman and Saakvitne (1995) as permanent and cumulative changes of schemas based on empathetic work with trauma survivors. Schemas are cognitive structures used to integrate and interpret new experiences (Piaget, 1971). If new experiences are no longer compatible with existing schemas, individuals may develop their schemas to an unrealistic, negative view of the world, e.g. ‘Most people are trustworthy’ might change into ‘No one is trustworthy, I am on my own’. This in turn leads to depression, cynicism, and pessimism. These changes are not regarded as pathological, but are understood as a normal, inevitable reaction following contact with traumatized people.
Since there are no distinct definitions, we have decided to use the overall term secondary traumatization to describe all symptoms including STS, CF, and VT in this paper.
1.3. Resilience and risk factors
Only a minority of first responders develops symptoms of secondary traumatization. Several studies indicate resilience factors that prevent first responders from developing symptoms of secondary traumatization. One of the most researched protective factors is social support. Prati and Pietrantoni’s meta-analyses (2010a) showed its significant positive influence on the first responders’ mental health; the subjectively perceived social support had a stronger influence than the factual received support. In addition, internal control (Regehr, Hill, & Glancy, 2000), self-efficacy (Stamm, 2002), collective efficacy at an organizational level (a group’s capability to put effort into and accomplish goals) (Cicognani, Pietrantoni, Palestini, & Prati, 2009), mindfulness, and engagement (Vrklevski & Franklin, 2008) are further important resilience factors. Other studies focused on identifying risk factors associated with secondary traumatization of first responders.
In previous research about resilience and risk factors in first responders, two systematic reviews focused on mental health in first responders. They documented the positive influence of social support (Nordahl, 2016; Prati & Pietrantoni, 2010a). Walsh (2009) systematically reviewed rescue workers’ responses to disaster situations and identified debriefing, team building, and preparation as three helpful interventions. Furthermore, two narrative reviews focused on factors influencing mental health in firefighters (thinking patterns, social support, and self-efficacy) (Deppa & Saltzberg, 2016) and police officers (stressful work events and stress management approaches) (Patterson, 2009).
1.4. Aims of the study
Because of their job profiles, first responders may be at high risk of developing pathological secondary traumatization. However, unlike trauma victims, secondary traumatization in first responders has not yet been sufficiently researched (Kleim & Westphal, 2011). As far as we know, this review is the first that aims to provide a systematic overview of current literature on first responders’ symptoms of secondary traumatization by examining secondary traumatization prevalence rates in first responders and shedding light on corresponding resilience and risk factors.
2. Methods
2.1. Inclusion criteria
We included studies that met the following criteria: (1) participants had to be first responders working on-site: police officers, firefighters, search and rescue personnel, or emergency and paramedic team members; (2) STS/VT/CF were assessed quantitatively with a validated questionnaire or subscale explicitly measuring secondary traumatization; and (3) the article was written in the English or German language. Studies focusing on participants working with traumatized individuals off-site (e.g. psychotherapists and emergency doctors) were excluded.
2.2. Questionnaires
In this review, we only included studies applying self-report questionnaires explicitly measuring secondary traumatization.
2.2.1. Compassion Fatigue Self-Test (CFST)
The CFST was developed in the late 1980s to assess compassion fatigue risk, not actual symptoms (Figley, 1995). It consists of two subscales (CF/STS and burnout) comprising 40 items which the participants have to rate on a five-point Likert scale, e.g. ‘I have experienced intrusive thoughts of visits with especially difficult patients’. However, a factor analysis did not support a two-factor model (CF/STS and burnout); it is not possible to calculate one burnout score and one CF/STS score separately. A one-factor model was established, ‘characterized by depressed mood in relationship to work accompanied by feelings of fatigue, disillusionment, and worthlessness’ (Figley, 1995). Only one of the 31 studies reviewed (Bissett, 2002) used the CFST.
2.2.2. Compassion Satisfaction/Compassion Fatigue Self-Test (CS/CFST)
The CS/CFST was developed from the CFST and comprises three subscales: compassion satisfaction (CS), CF, and burnout, assessed via 66 items (e.g. ‘I feel estranged from others’), using a six-point Likert scale. The scales showed good internal consistency, with Cronbach’s α = .84–.87. Scores are grouped into different risk categories for each subscale. For CF (range 0–115), five risk categories were used: extremely low risk (0–26), low risk (27–30), moderate risk (31–35), high risk (36–40), and extremely high risk (41–115). For burnout (range 0–85), four risk categories were used: extremely low risk (0–36), moderate risk (37–50), high risk (51–75), and extremely high risk (76–85). The subscale CS (range 0–130) has five categories: low potential (0–36), modest potential (64–81), good potential (82–99), high potential (100–117), and extremely high potential (118–130) (Stamm & Figley, 1996). In the present systematic review, the CS/CFST was applied in one dissertation (Tracy, 2012), without giving a reference range but referencing another study.
2.2.3. Professional Quality of Life Scale (ProQOL)
The ProQOL (Stamm, 2010) measures positive and negative effects of working with traumatized people over the past 30 days. It was developed from the CFST in the late 1990s. It consists of 30 items (e.g. ‘I find it difficult to separate my personal life from my life as a [helper]’) assessed via a five-point Likert scale, and is divided into three subscales: CS, burnout, and STS. The combined average of burnout and STS is defined as CF. The scales are continuous, but cut-off scores are provided: CS (M = 37, SD = 7.3, low scores < 33, high scores > 42), burnout (M = 22, SD = 6.3, low scores < 18, high scores > 27), and CF (M = 13, SD = 6.3, low scores < 8, high scores > 17) (Stamm, 2005). Since 2010, the scores are converted into T-scores, with a mean score of M = 50, SD = 10 for each of the three subscales and cut-off scores at the 25th and the 75th percentiles (CS: 44 and 57; burnout: 43 and 56; CF: 42 and 56) (Stamm, 2010). The ProQOL shows good internal consistency, with Cronbach’s α = .72–.87 (Sprang, Clark, & Whitt-Woosley, 2007). There is a revised 22-item Italian version of the ProQOL (Palestini, Prati, Pietrantoni, & Cicognani, 2009). The Italian version shows good internal consistency, with Cronbach’s α = .71–.83 (Prati & Pietrantoni, 2010b).
Of the 31 included studies, 13 (including three dissertations) used the ProQOL. Not all studies specified which questionnaire version they applied. Four studies (Pietrantoni & Prati, 2008; Prati & Pietrantoni, 2010b; Prati, Pietrantoni, & Cicognani, 2010, 2011) specified working with the revised Italian version. Only one of them (Prati et al., 2011) compared scores to the scale midpoint, while the other three studies did not provide a reference range. Two studies (Amjad & Rafique, 2013; Battle, 2011) used sum scores with the reference score M = 13, SD = 6.3. Two studies (Howell, 2016; Turgoose, Glover, Barker, & Maddox, 2017) divided scores into low (≤ 22), average (23–41), and high (≥ 42) scores without specifying the derivation of the cut-off scores. Tehrani (2016) referred to two cut-off scores (10 and 15), but also failed to provide their derivation. Two studies (Chiappo-West, 2017; Robinson, 2017) calculated T-scores (cut-off 56 or higher defined in the manual) (Stamm, 2010). Robinson interpreted the scores above the cut-off as risk factors for CF development. LaFauci Schutt and Marotta (2011) also defined scores above the cut-off as risk factors. One study (Crampton, 2014) did not provide any reference scores.
2.2.4. Secondary Traumatic Stress Scale (STSS)
The STSS is a 17-item questionnaire designed for professionals working with traumatized clients. The STSS is a part of the ProQOL: combined with the burnout scale, it forms the scale for CF (Döllinger, 2014). It is based on the diagnostic criteria of PTSD of the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), but focuses on the negative impact of indirect exposure to traumatic events. It assess intrusion (five items), avoidance (seven items), and arousal (five items) via a five-point Likert scale over the past 7 days (e.g. ‘I feel emotionally numb’). The STSS has been validated in a study including social workers, showing a mean score of M = 29.49, SD = 10.76, with the following means and standard deviations for the subscales: intrusion (M = 8.11, SD = 3.03), avoidance (M = 12.49, SD = 5.00), and arousal (M = 8.89, SD = 3.57) (Bride, 2004). The STSS has good internal consistency, with Cronbach’s α = .94, the subscales’ internal consistency ranging from Cronbach’s α = .83 to .85 (Bride, Robinson, Yegidis, & Figley, 2004). Döllinger (2014) noted that the STSS has no psychometric values of its own as the scale is part of another questionnaire (ProQOL). There is a revised Italian version (Setti & Argentero, 2012) with only two subscales: arousal (nine items) and intrusion (six items), also assessed via a five-point Likert scale.
Eight included studies worked with the STSS. One (Setti & Argentero, 2012) used the Italian version, giving no reference range. One study (Burruss, Holt, & Wall-Parker, 2017) used the scale, but did not report any descriptive data. Three further studies failed to provide a reference range (Argentero & Setti, 2011; Döllinger, 2014; Setti, Lourel, & Argentero, 2016). Two studies (Bourke & Craun, 2014; Turgoose et al., 2017) categorized scores into no/little, mild, moderate, high, and severe levels of secondary trauma, as suggested by Bride (2007). One study (Setti & Argentero, 2014) referenced that the higher the scores the more posttraumatic symptoms had been reported. None of the included studies reported above used the mean scores.
2.2.5. Secondary Trauma Questionnaire (STQ)
The STQ (Motta & Joseph, 1998) is based on the DSM-IV criteria (American Psychiatric Association, 1994), as well as the CFST. It assesses the main criteria of post-traumatic stress (arousal, re-experiencing, emotional distress, and avoidance) with the help of 18 items via a five-point Likert scale. The questionnaire also measures CF. The cut-off score is 38, with a possible score range from 18 to 90. The STQ has been validated (Motta, Kefer, Hertz, & Hafeez, 1999) using students with a traumatized family member or close friend (Cronbach’s α = .88) and professionals working with patients with human immunodeficiency virus (HIV) (Cronbach’s α = .75). The German version of the STQ has been validated by Reinhard and Maercker (2004); the items load on two factors: post-traumatic symptoms (explained variance R2 = 31.9%) and attendant symptoms (emotional burden, depressive and anxious thoughts; explained variance R2 = 10.3%).
In the present review, the STQ was used in four studies: two of them referred to a cut-off score of 38 (Krutolewitsch & Horn, 2017; Krutolewitsch, Horn, & Maercker, 2016), while two further studies provided no reference range (Krutolewitsch, Horn, & Maercker, 2015; Reinhard & Maercker, 2004).
2.2.6. Secondary Trauma Scale
The Secondary Trauma Scale (Motta, Hafeez, Sciancalepore, & Diaz, 2001) was specifically designed to assess secondary trauma in non-clinicians and was applied in a sample of Holocaust survivors’ grandchildren and psychotherapists. The original questionnaire consisted of 20 items based on PTSD symptoms as defined in the DSM-IV and the CFST (Figley, 1995). The latest version (Motta et al., 2004) comprises 18 items to be rated on a five-point Likert scale with a possible range of 18–90 and a cut-off score of 38 (moderate secondary traumatic response). A score of 45 or higher is considered to be a severe response (Motta et al., 2004). The Secondary Trauma Scale was validated (Motta et al., 2001); it shows good internal consistency, good reliability, and good discriminant validity with non-traumatic measures. Scores of primary traumatized students in primary trauma questionnaires did not correlate strongly with Secondary Trauma Scale scores, suggesting satisfactory differentiation between primary and secondary trauma.
In the present review, one study (Hargrave, 2010) assessed secondary trauma with the Secondary Trauma Scale, referring to the cut-off scores as described above.
2.3. Search strategies
We systematically searched the electronic databases PubMed, PsychINFO, and PSYNDEX (a German database) using the following search terms: (‘psychosocial support’ OR ‘crisis intervention’ OR ‘first responder’ OR ‘police’ OR ‘fire fighter’ OR ‘firefighter’ OR ‘emergency care’ OR ‘ambulance’ OR ‘rescue service’ OR ‘paramedics’) AND (‘secondary trauma’ OR ‘secondary traumatization’ OR ‘vicarious trauma’ OR ‘vicarious traumatization’ OR ‘compassion fatigue’). We also searched using the equivalent German search terms. The search covered all studies between 1994 and 7 February 2018. During the hand search, we excluded the terms ‘therapist’, ‘social worker’, ‘nurse’, ‘doctor’, and ‘hospital’ from the search to diminish the results. In addition, we searched reviews and meta-analyses found within the mentioned databases for relevant literature. All identified studies were screened by title and abstract according to the inclusion criteria.
2.4. Study selection and procedure
We identified 219 studies within the databases and 2192 by hand searching. After screening on title level and removing duplicates, 378 studies were screened at an abstract level. We assessed 125 full-text studies for eligibility. Of these, 40 studies failed to collect data on a quantitative basis, and 29 studies used psychometric instruments/questionnaires that were not appropriate for the assessment of secondary traumatization. In 12 studies, participants did not meet the inclusion criteria. The full text was not retrievable for 10 studies, even though we contacted the authors, and three studies were reported in languages other than German or English (see flowchart, Figure A1 in Appendix). In total, we were able to include 31 studies in our systematic review (see Appendix, Table A1). Three of these used the same data set (Krutolewitsch & Horn, 2017; Krutolewitsch et al., 2015, 2016), but reported different aspects. Two of the authors (AG and CDG) reviewed all studies. In the case of disagreements regarding the inclusion of studies, three authors (AG, CDG, and CN) discussed and decided in consensus.
3. Results
We merged the studies’ results into descriptive data, group comparisons, and correlation and regression analysis. Only two studies distinguished between professional and voluntary participants with regard to the symptoms of secondary traumatization. Hargrave (2010) did not find any difference in symptoms between police officers and volunteer crisis workers, while professional rescue workers scored higher in STSS than volunteers (Setti et al., 2016). Seven studies (Argentero & Setti, 2011; Pietrantoni & Prati, 2008; Prati & Pietrantoni, 2010b; Prati et al., 2010, 2011; Setti & Argentero, 2012; Setti et al., 2016) assessed both professionals and volunteers. However, psychological stress data were only provided for the group as a whole. In five studies (Bissett, 2002; Crampton, 2014; Döllinger, 2014; Robinson, 2017; Setti & Argentero, 2014), the participants were described as full-time first responders.
3.1. Descriptive data
In total, 26 of the 31 included studies reported descriptive data (see Appendix, Table A2) on CF, STS, VT, and single symptoms of the diagnostic criteria applied (e.g. intrusion). Ten studies reported descriptive data but failed to discuss them in the article (Amjad & Rafique, 2013; Argentero & Setti, 2011; Battle, 2011; Bourke & Craun, 2014; Pietrantoni & Prati, 2008; Prati & Pietrantoni, 2010b; Prati et al., 2010; Reinhard & Maercker, 2004; Setti & Argentero, 2012, 2014). Eight provided no reference range (Argentero & Setti, 2011; Pietrantoni & Prati, 2008; Prati & Pietrantoni, 2010a; Prati et al., 2010, 2011; Reinhard & Maercker, 2004; Setti & Argentero, 2012, 2014). Four studies reported risk factors for the development of CF (Bissett, 2002; LaFauci Schutt & Marotta, 2011; Robinson, 2017; Tracy, 2012).
Two studies used questionnaires (CFST, CS/CFST) to assess the risk of participants developing STS, with the result that up to 60% of participants (firefighters and paramedics; emergency medical technicians) were at extremely low risk (Bissett, 2002; Tracy, 2012). Two studies used subthreshold sum scores indicating between 15% and 35% of the first responders (emergency management professionals and firefighters) to be at risk of developing secondary traumatization (LaFauci Schutt & Marotta, 2011; Robinson, 2017). Crampton (2014) reported that 32% of rural paramedics and 46% of urban paramedics scored high on CF. A clinical level of secondary traumatization was reported by four studies (Krutolewitsch & Horn, 2017; Krutolewitsch et al., 2015, 2016; Tehrani, 2016) with prevalence rates ranging from 4% to 13% in rescue service, firefighters, and police officers investigating against Internet child abuse. Four studies highlighted the low reported burden in the assessed first responders: Bourke and Craun (2014) reported that symptoms ‘rarely’ occur in Internet crime against children investigators; Döllinger (2014) mentioned ‘no high strains’ in rescue service and paramedics, while Hargrave (2010) found that only 3.5% of police officers and volunteer crisis workers showed mild to severe scores. Prati et al. (2011), in turn, reported mean scores below the scale midpoint in emergency workers. One study (Turgoose et al., 2017) reported no high scores on CF, but found 16% of their sample of police officers to show high and severe scores on STS. Howell (2016), in contrast, reported low levels of STS but high levels of CF in dual-skilled firefighters/paramedics. Setti et al. (2016) reported the occurrence of post-traumatic symptoms in rescuers: intrusion (63%), avoidance (28%), and hyperarousal (40%). For a detailed description, see Table A2.
3.2. Group comparisons
Twelve of the identified studies compared psychological burden in different first responder groups (for a detailed description, see Appendix, Table A3). Five studies differentiated between occupations: rescue service workers showed a six times higher risk of developing secondary traumatization compared to assessed firefighters (Krutolewitsch et al., 2015). However, in another study, firefighters showed more CF symptoms than emergency and medical service personnel (Prati & Pietrantoni, 2010a). There was no difference in STS when comparing police officers to volunteers who had attended a sudden death crisis (Hargrave, 2010). Police officers working with traumatized adults experienced higher levels of STS compared to police officers working with children (Turgoose et al., 2017). Professional rescue workers (among others: ambulance operators, military, first aid operators, firefighters, and police officers) scored higher on the STSS than volunteers (Setti et al., 2016).
Three studies (Scott, 2016; Setti & Argentero, 2012; Tehrani, 2016) tried to uncover differences in secondary traumatization based on age, gender, and ethnicity. Female participants (rescue service and firefighters, ambulance operators, police officers, and Internet child abuse officers) (Krutolewitsch et al., 2015; Setti & Argentero, 2012; Tehrani, 2016) showed significantly more symptoms of secondary traumatization than males. While first responders of English origin investigating Internet crime against children showed lower levels of STS than American investigators (Bourke & Craun, 2014), there was no difference in CF between rural and urban paramedics (Crampton, 2014). Two studies compared first responders who had seen a traumatic situation or were on duty during a disaster with first responders who had not experienced a traumatic situation. Police officers who reported having experienced past trauma showed higher levels of CF than police officers without trauma experience (Battle, 2011). No difference in CF could be shown between paramedics who were on duty during the storm Allison disaster response effort in June 2001 and paramedics who were not on duty during the storm (Bissett, 2002).
3.3. Correlations and regression analyses
3.3.1. Correlations
Nineteen studies analysed correlations to show relationships between secondary traumatization and other variables (see Appendix, Table A4). Secondary traumatization was correlated with other facets of psychological strain in nine studies. All of them (Amjad & Rafique, 2013; Bissett, 2002; Lane, Lating, Lowry, & Martino, 2009; Pietrantoni & Prati, 2008; Prati & Pietrantoni, 2010b; Reinhard & Maercker, 2004; Tracy, 2012; Turgoose et al., 2017; Prati et al., 2011) found a strong relationship between secondary traumatization and burnout. STS also correlated moderately with primary PTSD symptom load (Bissett, 2002; Lane et al., 2009; Reinhard & Maercker, 2004). One study (Amjad & Rafique, 2013) found a relationship between CF and CS, whereas another one (Tracy, 2012) did not.
The intensity of secondary traumatization is related to specific peritraumatic characteristics. Hargrave (2010) found an association between STS and the amount of distress at the survivors’ reaction, emotional and cognitive identification, peritraumatic stress, lower peritraumatic needs, and younger age of the deceased. There was no connection between STS and specific traumatic events. However, there was a significant relationship between the number of traumatic events and STS symptoms (Reinhard & Maercker, 2004). The injury or death of a colleague (Krutolewitsch et al., 2015), as well as of children, during an assignment is particularly straining (Reinhard & Maercker, 2004), especially when connected to feelings of helplessness and horror. Unsurprisingly, working with exploited or abused children seems to be especially challenging. Turgoose et al. (2017) found that the longer people worked in this area, the higher were the reported symptom levels. However, this connection was not found when the years of overall working experience were considered.
The correlations with personality traits, coping mechanisms, and resources were described in 12 studies. High levels of neuroticism seem to be connected with STS (Howell, 2016; Tehrani, 2016), while there was no connection with extraversion or psychoticism. Two studies (Prati et al., 2010, 2011) found a positive relationship between CF and stress appraisal. In addition, current distress is connected to STS (Hargrave, 2010). Several resources correlate with STS: mindfulness, vigour, dedication, and affective commitment (Setti & Argentero, 2014; Setti et al., 2016). Empathy and self-fulfilment however, do not seem to be connected with STS (Turgoose et al., 2017). Several coping strategies are associated with higher levels of CF: denial, self-blame, self-distraction, religion, cognitive restructuring, and problem and emotional focused coping (Prati et al., 2011).
Regarding interpersonal aspects, finding it helpful to talk to family and friends for support (Hargrave, 2010), support from colleagues (Setti et al., 2016), workplace support, and social support in general (Argentero & Setti, 2011) are negatively connected with STS. Collective efficacy correlated negatively with CF (Prati et al., 2011). Several other interpersonal aspects had no connection to STS: spending quality time with a partner, being able to share emotional intimacy or open communication (Lane et al., 2009), family support (Setti et al., 2016), and having children (Krieger III, 2017).
The studies also report contradictory results: one study found a negative correlation between age and CF (Pietrantoni & Prati, 2008), while two other studies found no effect (Howell, 2016; Turgoose et al., 2017). Pietrantoni and Prati (2008) found a positive relationship between self-efficacy and CF, while Prati et al. (2010) found a negative association. There are also divergent results regarding positive correlations (Prati et al., 2010) and no correlations (Howell, 2016; Krieger III, 2017) between CF and the length of service. In one study (Krieger III, 2017), alcohol was shown to be connected to higher levels of CF, while in another (Krutolewitsch et al., 2015) no significant relationship could be found.
3.3.2. Regression analysis
Regression analysis, path analysis, or mediation analysis was used in 21 of the 31 selected studies to find predictors or mediators of STS symptoms (for a detailed description, see Table A4). Several studies found demographic variables to be predictors of secondary traumatization, such as female gender (Argentero & Setti, 2011; Krutolewitsch et al., 2016; Pietrantoni & Prati, 2008; Tehrani, 2016), higher age (Pietrantoni & Prati, 2008), work seniority (Setti & Argentero, 2014), ethnicity (Pietrantoni & Prati, 2008), marital status (Argentero & Setti, 2011), and professional rank (Tracy, 2012). STS and CS (LaFauci Schutt & Marotta, 2011) are predicted by personality traits, such as neuroticism and extraversion (LaFauci Schutt & Marotta, 2011; Robinson, 2017; Tehrani, 2016), and other psychological burdens, such as burnout (LaFauci Schutt & Marotta, 2011), emotional exhaustion (Bissett, 2002; Reinhard & Maercker, 2004), and peritraumatic stress. Distress at the survivor’s reaction (Hargrave, 2010) and exposure to potentially traumatic material (Burruss et al., 2017) also predict STS and CS (LaFauci Schutt & Marotta, 2011).
Certain coping strategies seem to have a negative effect on STS: coping through denial, increase in tobacco and alcohol use (Bourke & Craun, 2014), and humour at the expense of the victims (Craun & Bourke, 2015). The ability to recognize emotions also predicts higher levels of CF. On the contrary, social support (Prati & Pietrantoni, 2010b), affective commitment, collegial support (Setti et al., 2016), job role clarity (Argentero & Setti, 2011), and mindfulness (Setti & Argentero, 2014) are resilience factors.
Indicating a buffering effect (Prati et al., 2010), self-efficacy predicts post-traumatic stress symptoms (Pietrantoni & Prati, 2008) and seems to have an interactional effect with stress appraisal. Three studies used mediator analysis: Krutolewitsch and Horn (2017) found a partly mediating role of disclosure and co-rumination in the relationship between STS and post-traumatic growth; Prati et al. (2011) could show an association between stress appraisal and CF, which is partially mediated by emotion- and support-based coping, self-blame, and self-distraction; and STS could not be confirmed as a mediator in the relationship between trauma exposure and post-traumatic stress (Döllinger, 2014). Furthermore, Chiappo-West (2017) not only found predictors for STS, but could also show that STS predicts work engagement.
4. Discussion
This systematic review aimed to provide an overview of prevalence rates of secondary traumatization in first responders and to elucidate corresponding resilience and risk factors. The participants in the included studies had to be first responders working on-site as police officers, firefighters, search and rescue personnel, or emergency or paramedic team members. The first challenge lay in the identification of a precise definition of the term ‘first responders’. Many studies surveyed single occupational groups or used their own categories to cluster them. Furthermore, questionnaires had to explicitly assess secondary traumatization quantitatively, and the definitions of STS, VT, and CF were not always precise. Some publications used concepts interchangeably, while others differentiated them. Most authors defined VT as a change in schemas and cognitions, while STS and CF anchored on the symptoms: intrusion, avoidance, and hyperarousal. We included 31 studies in this review.
As one of our review’s main research questions, we wanted to assess the occurrence of secondary trauma symptoms in first responders. Only two studies (Hargrave, 2010; Setti et al., 2016) investigated differences in symptoms of secondary traumatization between professional and voluntary first responders. All other studies either assessed professionals and volunteers and computed results for the whole group or only included professional or volunteers in turn. Further research is needed to assess possible differences in symptoms of secondary traumatization between professional and voluntary first responders. It will be a challenge to find a differentiated definition for professional and voluntary first responders. Many volunteers receive training equivalent or comparable to the training of professionals (e.g. firefighters) (Schmidt, 2012).
Surprisingly, many studies reported low psychological strain across the different occupational groups of first responders. The general prevalence of secondary traumatization was reported to be between 4% and 13%. While two studies used questionnaires (CFST, CS/CFST) assessing the risk of developing STS (up to 60% of the participants showed no risk or a low risk), two studies used subthreshold sum scores indicating up to 35% of the first responders to be at risk of developing secondary traumatization. Several authors (Bissett, 2002; Crampton, 2014; Krieger III, 2017; Lane et al., 2009; Scott, 2016) assumed these results to be a positive response bias due to social desirability. First responders often work in a culture that is generally reluctant to endorse symptoms of psychological burden. Hence, the assessed volunteers may be concerned about appearing incapable of doing their job and may have exhibited a positive response bias when completing the questionnaires. However, these findings are congruent with the view of Summerfield, Kleber, Figley, and Gersons (1995) that the level of secondary traumatization is always lower than PTSD caused by an experienced traumatic event. Furthermore, the level of secondary traumatization in first responders is similar to the level of symptoms in therapists specialized in trauma therapy; for example, Daniels (2006) reported that 71% of the therapists did not suffer from secondary traumatization, 20% showed moderate symptoms, and 9% showed high symptoms. Reinhard and Maercker (2004) introduced the concept of an immunizing effect: first responders are confronted with traumatic experiences on a regular basis. This may lead to an immunization and, therefore, to a lower level of secondary trauma symptoms.
Next to the descriptive data, group comparisons were performed to gain a better understanding of particularly burdened groups. Female first responders showed higher STS symptoms than males, which suggest that females may be more vulnerable to secondary traumatization. This finding was reported in several studies and is consistent with previous research (e.g. Daniels, 2006). Other publications compared different occupational groups of first responders and their psychological strain. These studies showed partially contradicting results. However, none of the presented results (except for results regarding gender) was replicated in further studies or reported more than once. Therefore, it is not possible to make any generalized conclusions about these preliminary results, and further research is needed in the future.
Most of the identified studies analysed factors connected to and influencing secondary traumatization. Secondary traumatization consistently correlated with burnout in 19 studies. The close connection of these two constructs becomes apparent if the definitions of CF and burnout are called to mind. Bellolio et al. (2014, p. 630) associated CF with ‘psychic exhaustion, depersonalization, and reduced personal accomplishment’, which are also indicators of burnout. Both constructs are closely associated and can be caused by the same stressful situations. However, it is important to note that CF is a results of one or more traumatic experiences, while the development of burnout needs continuous negative experiences without a necessarily traumatic character (Tracy, 2012). Secondary traumatization also correlated moderately with primary traumatization. This connection can be explained by the fact that first responders’ occupational profiles are characterized by both the experience of traumatic situations and taking care of traumatized survivors. The resilience and risk factors included pretraumatic (e.g. age, gender), peritraumatic (exposure, emotional exhaustion), and post-traumatic factors (social support, alcohol and tobacco use). They show a great similarity to factors influencing primary traumatic stress reactions and are in agreement with previous studies (e.g. Becker-Nehring, Witschen, & Bengel, 2012; Brewin, Andrews, & Valentine, 2000). Although many predictors were found, it is important to consider that all studies used a cross-sectional design. Therefore, we can only interpret the results with caution, and future research focusing on longitudinal studies is necessary. Furthermore, studies focusing on preventive or curative interventions may prove insightful.
In the included studies, six different self-report questionnaires were applied to assess secondary traumatization: the ProQOL and the STSS, a subscale of the ProQOL, were often used (12 and eight times, respectively). The STQ was applied in four German publications while the CFST, the CS/CFST, and the Secondary Trauma Scale were used only once each. The CFST and the CS/CFST evaluated the risk of developing secondary traumatization, while the other questionnaires evaluated the symptom load. Since all questionnaires are based on self-report, no objective criterion to measure secondary traumatization was included in this review. Nevertheless, all questionnaires were validated and showed good performance criteria, with the exception of the CFST, for which factor analysis did not support the assumed two-factor model. Regrettably, the questionnaires have different reference ranges, and the ProQOL reference range even changed from a sum score to a T-score while the questionnaire was further evolved. Almost half of the publications stated the descriptive results without any explanation or interpretation, and most of them did not even report the reference range. A few studies defined cut-off scores without giving the sources. Therefore, the interpretation of the results is challenging.
4.1. Limitations of the study
To date, it is common to evaluate secondary traumatization with questionnaires that were originally designed to assess primary traumatization, even though there is only a moderate correlation between these two constructs (Motta et al., 2004). In this review, we excluded studies that measured secondary traumatization with questionnaires originally designed for primary traumatization. Therefore, many studies were excluded from the review. In addition, owing to the exclusion of qualitative studies, information may have been lost.
4.2. Conclusion
This study is the first systematic review on secondary traumatization in first responders including all groups of first responders. In the existing literature, it is difficult to find precise definitions of STS, CF, and VT. While some researchers emphasize precise definitions, others use the terms interchangeably. This systematic review shows low levels of secondary traumatization in first responders. However, it is possible that we have underestimated the prevalence rates owing to a positive response bias caused by social desirability or job-loss concerns (Kronenberg et al., 2008). Several studies described protective and risk factors for secondary traumatization, including pretraumatic, peritraumatic, and post-traumatic factors. Unfortunately, we can only interpret results with caution because of the unanimous use of cross-sectional designs. Future research should focus on implementing longitudinal designs as well as preventive and curative interventions.
Acknowledgement
We would like to thank Dipl. Psych. Anna Cranz for proofreading this manuscript.
Appendix.
Table A1.
Reviewed studies: characteristics and statistical design
| Study | Participants (N) | Questionnaire | Descriptive statistics | Group comparisons | Correlations | Regressions | Limitations reported by authors and further limitations |
|---|---|---|---|---|---|---|---|
| Amjad and Rafique (2013) | N = 60 rescue workers | ProQOL | x | x | x | Generalizability, only workers with 10 or more years of formal education; measures developed for western society, some items may be culturally biased (assessment in India) Further limitations: sample size, cross-sectional design |
|
| Argentero and Setti (2011) | N = 782 rescue workers | STSS | x | x | x | Generalizability due to social and cultural context (assessment in Italy); previous experience of personal trauma not considered, cross-sectional design | |
| Battle (2011) Dissertation | N = 1390 police officers | ProQOL | x | x | Trauma defined as self-perceived trauma, measured via self-report (yes–no items); no representative sample (single-centre assessment) | ||
| Bissett (2002) Dissertation | N = 240 firefightersand paramedics | CFST | x | x | x | Homogeneity of responses and lack of symptom reporting (potential social desirability bias due to group data collection); possible history effect due to tropical storm (more symptoms reported shortly after the disaster); cross-sectional design; generalizability | |
| Bourke and Craun (2014) | N = 965 ICAC investigators | STSS | x | x | x | Unclear response rate; cross-sectional design; previous personal trauma not assessed; generalizability | |
| Burruss et al. (2017) | N = 360 ICAC police officers | STSS | x | Study participants: trainees; prior work experience not assessed; only quantitative measures employed Further limitation: cross-sectional design |
|||
| Chiappo-West (2017) | N = 153 police officers | ProQOL | x | x | ProQOL had no published validity statistics at time of submission; organizational environment unknown; no cause determined; self-report measures: not generalizable to the law enforcement profession | ||
| Crampton (2014) Dissertation | N = 87 paramedics | ProQOL | x | x | Stigma associated with PTSD may hinder participants’ responses; generalizability; cross-sectional design; several questionnaires rejected due to positive bias scores; low sample size | ||
| Craun and Bourke (2015) | N = 350 ICAC taskforce members | STSS | x | Cross-sectional design; generalizability | |||
| Döllinger (2014) Dissertation | N = 110 rescue services and paramedics | STSS | x | x | Items on sexual traumatic experiences excluded due to violation of privacy concerns; no information on non-responders; participants: short length of service; social bias; not representative participants; generalizability Further limitation: cross-sectional design |
||
| Hargrave (2010) Dissertation | N = 165 police officers + N = 148 volunteer crisis workers | Secondary Trauma Scale | x | x | x | x | Retrospective recall; possible confounding variables; only police officers and crisis workers who had attended sudden death were assessed; cross-sectional design |
| Howell (2016) Dissertation | N = 73 dual-skilled firefighters/paramedics | ProQOL | x | x | Short period of time to collect data: sample size, individuals on sick leave not included; limited demographic information due to participants’ anonymity; generalizability | ||
| Krieger III (2017) Dissertation | N = 228 CAC law enforcement investigators and forensic interviewers | STSS | x | Non-random sample; positive response bias | |||
| Krutolewitsch and Horn (2017)* | N = 168 rescue service and firefighters | STQ | x | x | Self-report measures developed for western society, some items may be culturally biased (assessment in Russia); cross-sectional design | ||
| Krutolewitsch et al. (2015)* | N = 168 rescue service and firefighters | STQ | x | x | x | Cross-sectional design; no Russian norm sample available | |
| Krutolewitsch et al. (2016)* | N = 168 rescue service and firefighters | STQ | x | x | x | Self-report measures developed for western society, some items may be culturally biased (assessment in Russia); cross-sectional design | |
| LaFauci Schutt and Marotta (2011) | N = 269 emergency management professionals | ProQOL | x | x | Non-random, fairly homogeneous volunteer sample; Internet survey (return rate unknown, possible differences between responders and non-responders); self-report measures; potential social desirability bias Further limitation: cross-sectional design |
||
| Lane et al. (2009) | N = 47 detectives investigating sexual child abuse and assault cases | ProQOL | x | Only two participants scored above cut-off score on PCL (positive response bias); data gathered at a conference; personal sexual abuse history not assessed; sample size | |||
| Pietrantoni and Prati (2008) | N = 961 first responders | ProQOL | x | x | x | Cross-sectional design; no qualitative methods | |
| Prati and Pietrantoni (2010a) | N = 586 rescue workers | ProQOL | x | x | x | x | Retrospective self-reports of critical incident exposure (recall bias); cross-sectional design |
| Prati et al. (2010) | N = 451 rescue workers | ProQOL | x | x | x | Self-report measures; only one single item to assess stress appraisal; cross-sectional design | |
| Prati et al. (2011) | N = 463 emergency workers | ProQOL | x | x | x | Self-report measures; only one single item to assess stress appraisal; cross-sectional design; lack of information on larger population and sampling method | |
| Reinhard and Maercker (2004) | N = 92 rescue service workers | STQ | x | x | x | Questionnaires: possibly blurred validity; return rate c. 29% (no information on non-responders) Further limitation: cross-sectional design |
|
| Robinson (2017) Dissertation | N = 129 full-time firefighters | ProQOL | x | x | Return rate 49.8%; population size experiencing CF; generalizability Further limitation: cross-sectional design |
||
| Scott (2016) Dissertation | N = 21 parole officers | STSS | x | Sample size; clustering participants into groups based on specific offer types; contact not possible; self-report measure; potential social desirability bias | |||
| Setti and Argentero (2012) | N = 724 ambulance operators | STSS | x | x | Generalizability, only internal validity reported | ||
| Setti and Argentero (2014) | N = 176 firefighters | STSS | x | x | x | Cross-sectional design; lack of symptoms (other protective factors not considered); self-report measures; population not fully representative | |
| Setti et al. (2016) | N = 782 rescuers, e.g. ambulance, first aid operators, military, firefighters, police officers | STSS | x | x | x | x | Cross-sectional design; no missing data procedure; self-report measures; sample heterogeneous |
| Tehrani (2016) | N = 126 police officers; Internet child abuse investigators | ProQOL | x | x | x | x | Low levels of traumatic stress symptoms reported Further limitation: cross-sectional design |
| Tracy (2012) Dissertation | N = 40 emergency medical technicians | CS/CFST | x | x | x | 75% of participants were assistant emergency medical technicians (lowest ranking staff); single-centre assessment; exposure to trauma low; self-report measures Further limitations: sample size; cross-sectional design, generalizability |
|
| Turgoose et al. (2017) | N = 142 police officers | ProQOL | x | x | x | Cross-sectional design; validity; many participants may have had little contact with victims |
CF, compassion fatigue; CFST, Compassion Fatigue Self-Test; CS, compassion satisfaction; CS/CFST, Compassion Satisfaction/Compassion Fatigue Self-Test; (I)CAC, (Internet) Crime Against Children; PCL, PTSD Checklist; ProQOL, Professional Quality of Life Scale; PTSD, post-traumatic stress disorder; STQ, Secondary Trauma Questionnaire; STSS, Secondary Traumatic Stress Scale.
* Same set of data.
Table A2.
Reviewed studies: descriptive statistics and reported references range
| Study and participants (N) | Reported reference range | Descriptive statistics |
|---|---|---|
| ProQOL | ||
| Amjad and Rafique (2013) N = 60 rescue workers |
CF: M = 13, SD = 6.3 | CF: M = 28.56, SD = 4.63 |
| Battle (2011) Dissertation N = 1390 police officers |
CF: M = 13, SD = 6.3 | CF: M = 13.75, SD = 7.45 (officers who had experienced perceived trauma); M = 10.69, SD = 5.99 (officers who had not experienced perceived trauma) |
| Chiappo-West (2017) N = 153 police officers |
t-Scores: M = 50; cut-off 57 | STS: M = 49.8, SD = 9.5 |
| Crampton (2014) Dissertation N = 87 paramedics |
No reference range | CF: evaluated via self-report: 43% of urban paramedics, 23% of rural paramedics; questionnaire: 46% of urban paramedics, 32% of rural paramedics STS: urban: 34% average, 66% high; rural paramedics: 32% average, 68% high |
| Howell (2016) Dissertation N = 73 dual-skilled firefighter/paramedics |
< 22: low score 23–41: average score > 42: high score |
CF: M = 38.44, SD = 5.86 (average bordering on high levels) STS: M = 20.63, SD = 5.14 (average bordering on low levels) |
| LaFauci Schutt and Marotta (2011) N = 269 emergency management professionals |
> 17: at risk of CF | CF: means comparable to manual’s reported levels; > 17: 14.7% indicating risk of CF; > 43: 13.2% indicating PTSD diagnosis in non-clinical population |
| Pietrantoni and Prati (2008) N = 961 first responders |
Revised Italian version No reference range |
CF: M = 2.04, SD = .58 |
| Prati and Pietrantoni (2010a) N = 586 rescue workers |
Revised Italian version No reference range |
CF: M = 1.85, SD = .58 (medical workers: M = 1.76, SD = .57; firefighters: M = 1.95, SD = .59) |
| Prati et al. (2010) N = 451 rescue workers |
Revised Italian version No reference range |
CF: M = 1.74, SD = .26 |
| Prati et al. (2011) N = 463 emergency workers |
Revised Italian version scale Midpoint: 2.50 |
CF: M = 1.74, SD = .57 |
| Robinson (2017) N = 129 career firefighters |
t-Scores, cut-off: ≥ 56 for burnout or STS | F: > 55: n = 45 at high risk of developing CF; < 56: n = 84 not at high risk of developing CF |
| Tehrani (2016) N = 126 police officers; Internet child abuse investigators |
CF: cut-off 1: 10; cut-off 2: 15 | CF: M = 9.7, SD = 6.0 (female); M = 6.1, SD = 5.2 (male) STS: 4% of males and 7% of females reported clinical levels |
| Turgoose et al. (2017) N = 142 police officers |
CF: subscales were categorized as low, average, and high STSS: reference to Bride (2007); little/no STS (scores < 50th percentile), mild, moderate, high, and severe STS |
CF: M = 18.4, SD = 4.7; 84% scores ranked as being low, 16% being average, and none as high STS: M = 32.5, SD = 10.6 (work experience ≥ 1 year M = 37.0, SD = 11.7, n = 67; work experience < 1 year M = 29.8, SD = 9.0, n = 40; working with adults: M = 34.3, SD = 10.7, n = 72; working with children: M = 27.4, SD = 8.5, n = 34); 74% no or mild level, 11% moderate, 8% high, and 8% severe; low levels of intrusion and avoidance, mild levels of arousal |
| STSS | ||
| Argentero and Setti (2011) N = 782 rescue workers |
No reference range | VT: intrusion: M = 2.02, SD = .80; avoidance: M = 2.07, SD = .81; arousal: M = 1.93, SD = .72 |
| Bourke and Craun (2014) N = 965 ICAC investigators |
Reference to Bride (2007); categorization into no/little, mild, moderate, high, and severe levels of STS | STS: M = 2.11 indicating that symptoms occur ‘rarely’ |
| Döllinger (2014) Dissertation N = 110 rescue service and paramedics |
No reference range | STS: M = 15.92, SD = 3.62, range 10–30; 95.5% low strain, 4.5% average strain |
| Setti and Argentero (2012) N = 724 ambulance operators |
Italian version, no reference range | Intrusion: M = 2.02, SD = .78 (females: M = 2.14, SD = .74; males: M = 1.98, SD = .77); avoidance: M = 1.93, SD = .69; arousal: M = 2.07, SD = .80 (younger participants: M = 2.20, SD = .87, older: M = 1.94, SD = .70) |
| Setti and Argentero (2014) N = 176 firefighters |
High scores: post-traumatic symptoms | Intrusion: M = 1.67, SD = .54; arousal: M = 1.85, SD = .51 |
| Setti et al. (2016) N = 782 rescuers |
No reference range | Intrusion: M = 2.02, SD = .80; 63.1% of respondents reported at least one intrusion symptom; avoidance: M = 1.93, SD = .72; 27.5% affirmed three items on the avoidance subscale; hyperarousal: M = 2.07, SD = .81; 39.8% affirmed at least two items on the hyperarousal subscale |
| CFST | ||
| Bissett (2002) Dissertation N = 240 firefighter paramedics |
< 27: extremely low risk 27–30: low risk 31–35: moderate risk 36–40: high risk > 40: extremely high risk |
CF: M = 32.65, SD = 9.07, range: 23–82; 25.4% extremely low risk (n = 60), 25.8% low risk (n = 61), 24.2% moderate risk (n = 57), 9.8% high risk (n = 23), 14.8% extremely high risk (n = 35) |
| STQ | ||
| Krutolewitsch and Horn (2017)* N = 168 rescue service and firefighters |
Cut-off: 38 | ST: 13.1% clinical level |
| Krutolewitsch et al. (2015)* N = 168 rescue services and firefighters |
No reference range | ST: 13.1% clinical level, 7.7% mild level, 5.4% severe level; (rescue services: 7.6% mild and average level, 13.2% severe level; firefighters: 6.7% mild and average level, 1.7% severe level) |
| Krutolewitsch et al. (2016)* N = 168 rescue services and firefighters |
Cut-off: 38 | ST: M = 29.95, SD = 7.96; 13.1% clinical level: 7.7% mild level, 5.4% severe level |
| Reinhard and Maercker (2004) N = 92 rescue service workers |
No reference range | STQ attendant symptoms: M = 10.93, SD = 4.26, range 1–30 Study-validated questionnaire |
| Secondary Trauma Scale | ||
| Hargrave (2010) Dissertation N = 165 police officers N = 148 volunteer crisis workers |
Cut-off: 38 moderate response; > 44 severe response | STS: M = 21.57, SD = 5.07, range 18–42 (police M = 21.92, SD = 5.37; volunteers M = 21.17, SD = 4.70); 3.5% scored in mild to severe range |
| CS/CFST | ||
| Tracy (2012) Dissertation N = 40 emergency medical technicians |
Reference to Conrad and Kellar-Guenther (2006) | CF: > 60% at extremely low risk, M = 25.18, SD = 14.08 |
CF, compassion fatigue; CFST, Compassion Fatigue Self-Test; CS, compassion satisfaction; CS/CFST, Compassion Satisfaction/Compassion Fatigue Self-Test; ICAC, Internet Crime Against Children; ProQOL, Professional Quality of Life Scale; PTSD, post-traumatic stress disorder; ST, secondary traumatization; STQ, Secondary Trauma Questionnaire; STS, secondary traumatic stress; STSS, Secondary Traumatic Stress Scale; VT, vicarious traumatization.
* Same set of data.
Conrad, D., & Kellar-Guenther, Y. (2006). Compassion fatigue, burnout, and compassion satisfaction among Colorado child protection workers. Child Abuse & Neglect, 30(10), 1071–1080.
Table A3.
Reviewed studies: group comparisons
| Study and participants (N) | Questionnaire | Group 1 | Group 2 | Statistics |
|---|---|---|---|---|
| ProQOL | ||||
| Battle (2011) Dissertation N = 1390 police officers |
ProQOL | Officers perceived trauma (M = 13.75, SD = 7.45) | Officers not perceived trauma (M = 10.69, SD = 5.99) | CF: F(1,1389) = 53.00, p < .0005, partial η2 = .040 |
| Crampton (2014) Dissertation N = 87 paramedics |
ProQOL | Rural paramedics | Urban paramedics | CF: no significant difference |
| Prati and Pietrantoni (2010a) N = 586 rescue workers |
ProQOL | Firefighters (M = 1.95, SD = .59) | Emergency and medical service personnel (M = 1.79, SD = .57) | CF: t(566) = −3.185, p = .002, d = .28 |
| Tehrani (2016) N = 126 police officers; Internet child abuse investigators |
ProQOL | Females (M = 9.70, SD = 6.00) | Males (M = 6.1, SD = 5.2) | CF: t-test, p = .007 |
| Turgoose et al. (2017) N = 142 police officers |
ProQOL | Police officers who had served in this function for ≥ 1 year (M = 37.0, SD = 11.7, N = 67) Police officers working with adults (M = 34.3, SD = 10.7, N = 72) |
Those in function for < 1 year (M = 29.8, SD = 9.0, N = 40) Police officers working with children (M = 27.4, SD = 8.5, N = 34) |
STS: t(104) = 3.6, p = .001; t(104) = 3.3, p = .001 |
| STSS | ||||
| Bourke and Craun (2014) N = 965 ICAC investigators |
STSS | Personnel in UK (M = 1.99) UK sample: more respondents in low/no category (USA: 26.4%; UK: 36.9%) |
Personnel in USA (M = 2.16) US sample: more respondents in severe category (USA: 15.3%; UK: 10.4%) |
STS: t(944) = 3.40, p < .001; χ2(4, n = 941) = 13.15, p = .01 |
| Scott (2016) Dissertation N = 21 parole officers |
STSS | Singular ethnic group | Multi-ethnic group | STS: multi-ethnic group showed higher resilience (χ2 = 11.422, p = .001) |
| Setti and Argentero (2012) N = 724 ambulance operators |
STSS | Females (M = 2.14, SD = .74) Younger participants (M = 2.20, SD = .87) |
Males (M = 1.98, SD = .77) Older participants (M = 1.94, SD = .70) |
Intrusive thoughts: (F = 6.14, p < .05) arousal: (F = 4.19, p < .01) |
| Setti et al. (2016) N = 782 rescuers |
STSS | Professionals (EE: M = 2.06, SD = 1.38; DP: M = 1.97, SD = 1.42; avoidance M = 2.08, SD = .79; hyperarousal M = 2.19, SD = .89) |
Volunteers (EE: M = 1.58, SD = 1.24; DP: M = 1.44, SD = 1.27; avoidance M = 1.86, SD = .67; hyperarousal M = 2.01, SD = .77) |
EE: F(1) = 24.27, p < .01; DP: F(1) = 26.84, p < .01; avoidance F(1) = 15.77, p < .01; hyperarousal F(1) = 8.05, p < .05 |
| CFST | ||||
| Bissett (2002) Dissertation N = 240 firefighter paramedics |
CFST | Paramedics on duty (M = 33.27, SD = 9.35, n = 147) during disaster response efforts in the wake of storm Allison | Paramedics not on duty (M = 31.69, SD = 8.61, n = 87) | CF: no significant difference |
| STQ | ||||
| Krutolewitsch et al. (2015) N = 168 rescue service and firefighters |
STQ | Rescue service (M = 32.75, SD = 9.75) Females |
Firefighters (M = 28.08, SD = 6.52) Males |
ST: t = −3.18, p = .002; risk 6× higher (odds ratio), χ2 = 15.73, df = 1, p = .000; ST: females at higher risk than males, odds ratio 4:2 |
| Secondary Trauma Scale | ||||
| Hargrave (2010) Dissertation N = 165 police officers; N = 148 volunteer crisis workers |
Secondary Trauma Scale | Police officers (M = 21.92, SD = 5.37) | Volunteer crisis workers (M = 21.17, SD = 4.70) | STS: no significant differences (t = 1.30) |
CF, compassion fatigue; CFST, Compassion Fatigue Self-Test; DP, depersonalization; EE, emotional exhaustion; ProQOL, Professional Quality of Life; ST, Secondary Traumatization; STQ, Secondary Trauma Questionnaire; STS, secondary traumatic stress; STSS, Secondary Traumatic Stress Scale.
Table A4.
Reviewed studies: correlation and regression analyses
| Study and participants N) | Questionnaire | Correlation and regression analyses |
|---|---|---|
| Amjad and Rafique (2013) N = 60 rescue workers |
ProQOL | Correlations: CF corr. with work life quality (r = −.85, p < .01), CS (r = −.39, p < .01), B (r = .76, p < .01) |
| Argentero and Setti (2011) N = 782 rescue workers |
STSS |
Correlations: VT corr. with social support: intrusion r = −.23, avoidance r = −.31, arousal r = −.26 (all p < .01); predictability of job support: intrusion r = −.09, avoidance r = −.16, arousal = −.18 (all p < .01; job support: avoidance r = −.20 (p < .01) Regressions: three regression models: individual and organizational factors influence intrusion (R2 = .083), avoidance (R2 = .133), arousal (R2 = .089); role clarity has most sig. influence on intrusion (β = −.251), avoidance (β = −.301), arousal (β = −.231, all p < .01) |
| Bissett (2002) Dissertation N = 240 firefighters and paramedics |
CFST |
Correlations: CF corr. with PTSD severity (r = .76, p < .05), B (EE: r = .50, p < .05; DP: r = .42, p < .05; PA: r = −.08, p > .05) Factor analysis: result supported three-factor model of PTSD severity (avoidance/distractibility, restlessness/irritability, and anxiety/intrusion), factors were not a strict representation of the three symptom clusters assessed for PTSD diagnosis Regressions: B predicts CF (R2 = .27, F(4,214) = 20.05, p < .01) with EE = primary predictor (β = .52, p < .01), other three burnout factors (DP, job skills, PA) not sig., EE score was entered into the regression model alone (β = .53, p < .01; R2 = .28) |
| Bourke and Craun (2014) N = 965 ICAC investigators |
STSS | Regressions: In UK personnel, predictors of STS explained 44% of variance [F(11,219) = 17.69, p < .001] and 52% of variance in US personnel [F(16,593) = 37.85, p < .001]; similarities, e.g. coping through denial (UK β = .21, p < .001; USA β = .13, p < .001), increase in tobacco use (UK β = .19, p < .01; USA β = .12, p < .001), increase in alcohol use (UK β = .17, p < .01; USA β = .12, p < .001); differences, e.g. more frequent use of coping through social support (USA β = −.10, p < .005), gender (USA β = −.06, p = .05) only in US sample |
| Burruss et al. (2017) N = 360 ICAC police officers |
STSS | Regressions: exposure to CAC (β = .221, p < .001) predicted ST (R2 = .074); female gender (β = .191, p < .001) and trauma (β = .393, p < .001) predicted coping behaviour (R2 = .212) |
| Chiappo-West (2017) N = 153 police officers |
ProQOL |
Correlations: STS corr. with work engagement (r = −.254, p = .000) Regressions: CS (β = .749, p < .01), B (β = −.010, p = .912), STS (β = −.076, p = .273) explained 59.7% of variance of work engagement [F(2,149) = 76.07, p < .001] |
| Craun and Bourke (2015) N = 350 ICAC taskforce members |
STSS | Regressions: frequency that humour is used at victim’s expense (β = .18, p < .001), joking about society/human behaviour (β = .11, p = .02); frequency (β = .21, p < .001) and difficulty with child exploitation material (β = .18, p < .001), increase in alcohol use (β = .20, p < .001), coping through denial (β = .15, p = .01) predict STS [R2 = .46; F(16,310) = 20.48, p < .001]; non-predictors: utilizing humour at expense of offenders (p = .97); more frequent use of humour with sexual innuendo (p = .10) |
| Döllinger (2014) Dissertation N = 110 rescue services and paramedics |
STSS | Regressions: STS is not a mediator between trauma exposition and post-traumatic stress (no sig. relationship between trauma exposure and PTSD [B = −.04, t(108) = −.68, p = .497] |
| Hargrave (2010) Dissertation N = 165 police officers + N = 148 volunteer crisis workers |
Secondary Trauma Scale |
Correlations: STS related to younger age of deceased (r = −.15), lower trauma resolution (r = −.18, p < .01), lower peri-event needs (r = −.17); emotional (r = .28, p < .01), cognitive (r = .36, p < .01), and total identification (r = .38); distress at survivor reactions (r = .45, p < .01), peritraumatic distress (r = .53, p < .01), current distress (r = .58, p < .01), finding it helpful talking to family/friends as support strategy (r = .16, p < .01), unrelated to specific traumatic experience Regressions: peri-event reaction (peritraumatic distress β = .21, and distress at survivor reactions β = .21) explained 11% of variance in STS, 1% pre-event and 1% post-event after controlling for current distress and group which explained 34% [R2 = .47, F(12,249) = 18.56, p < .01] |
| Howell (2016) Dissertation N = 73 dual-skilled firefighters/paramedics |
ProQOL | Correlations: neuroticism corr. with STS [r(70) = .409, p < .01]; no sig. corr. between extraversion and STS; no sig. corr. between psychoticism and CS, B, STS; no sig. corr. between age or length of service and CF, B, STS |
| Krieger III (2017) Dissertation N = 228 CAC law enforcement investigators and forensic interviewers |
STSS | Correlations: having unintended thoughts about victim corr. with alcohol use (Kendall’s τ = −.119, p = .038); non-sig. corr. between time in position and emotional numbness; non-sig. corr. between having children and emotional numbness |
| Krutolewitsch and Horn (2017) N = 168 rescue services and firefighters |
STQ | Mediation analysis: partly mediating role of disclosure and co-rumination between STS and post-traumatic growth (indirect effect of secondary PTSD via co-rumination on post-traumatic growth, Sobel Ztest: z = 2,89, p = 0,003; indirect effect of secondary PTSD via disclosure on post-traumatic growth (z = 5,94, p < .0001) |
| Krutolewitsch et al. (2015) N = 168 rescue services and firefighters |
STQ | Correlations: traumatic work situation (injury or death of colleague) corr. with STS (r = .19, p < .05); perceives appreciation corr. with ST (r = −.24, p < .01); no sig. corr. between alcohol consumption and ST |
| Krutolewitsch et al. (2016) N = 168 rescue services and firefighters |
STQ | Regressions: socio-interpersonal factors explain 50.4% of ST variance: demographics explain 9%, perceived appreciation 18%, disclosure 22%, co-rumination 2% (R2 = .50; p < .05); predictors: work experience (β = −.25, p < .05), familial lack of understanding (β = .15, p < .05), secretiveness (β = .17, p < .05), emotional reaction (β = .46, p < .001), co-rumination (β = .18, p < .05) |
| LaFauci Schutt and Marotta (2011) N = 269 emergency management professionals |
ProQOL |
Regressions: personality, frequency of trauma exposure, repeated exposure symptomology explained 41% of PTSD symptoms variance [R2 = .42, F(2,191) = 16.39, p < .0]; predictors: neuroticism (β = .38, p < .001), burnout (β = .42, p < .001), compassion satisfaction (β = .21, p < .001); predictor variables do not moderate relationship between trauma exposure frequency and PTSD symptoms; exploratory model: ethnic identity is an individual predictor in context of full model |
| Lane et al. (2009) N = 47 detectives investigating sexual child abuse and assault cases |
ProQOL |
Correlations: CF and CS not corr. with quality time, emotional intimacy, or ability to communicate openly with loved ones; PTSD symptoms corr. with B (r = .44, p < .01) and fatigue scores (r = .59, p < .01); females: emotional intimacy had no relation with B, CF, CS; no relation between open communication and B or CF |
| Pietrantoni and Prati (2008) N = 961 first responders |
ProQOL |
Correlations: CF corr. with age (r = .10, p < .01), self-efficacy (r = .11, p < .01), B (r = .57, p < .001) Regressions: sense of community (ns), collective efficacy (ns), and self-efficacy (β = −.10, p < .01) predict CF (ΔR2 = .01, p < .05) after controlling for gender (β = .18, p < .001) and age (β = .12, p < .001, R2 = .04, p < .001) |
| Prati and Pietrantoni (2010a) N = 586 rescue workers |
ProQOL |
Correlations: CF strongly corr. with B Path analysis: social support is resilience factor in aftermath of exposure to critical incidents; influence of receiving actual social support in a time of crisis on quality of life is mediated by perceived social support |
| Prati et al. (2010) N = 451 rescue workers |
ProQOL |
Correlations: CF corr. with length of service (r = .13, p < .01), stress appraisal (r = .34, p < .001), self-efficacy (r = −.24, p < .001) Regressions: length of service (β = .17, p < .001), stress appraisal (β = .29, p < .001), self-efficacy (β = −.23, p < .001) predict CF (R2 = .22, p < .05); stress appraisal had sig. effect on CF, B, CS, self-efficacy may have a buffering effect |
| Prati et al. (2011) N = 463 emergency workers |
ProQOL |
Correlations: CF corr. with B (r = .64, p < .001), denial (r = .26, p < .001), self-blame (r = .27, p < .001), self-distraction (r = .29, p < .001), religion coping (r = .16, p < .001), cognitive restructuring (r = .11, p < .05), problem-focused coping (r = .14, p < .01), emotion- and support-focused coping (r = .24, p < .001), collective efficacy (r = −.10, p < .05), stress appraisal (r = .33, p < .001) Mediation analysis: partial mediation model: relation between stress appraisal and CF partially mediated by emotion- and support-focused coping, self-blame and self-distraction |
| Reinhard and Maercker (2004) N = 92 rescue service workers |
STQ |
Correlations: attendant symptoms of STS corr. with PTSD: intrusion (r = .30), avoidance (r = .44), hyperarousal (r = .43, all p < .01), trauma dose (r = .22, p < .01), EE (r = .47, p < .01), DP (r = .42 p < .01), consternation (r = .36 p < .01), perceived social support (r = −.29, p < .01); no corr. with personal fulfilment; exceptionally straining: death and injury of children, often combined with feelings of helplessness and horror Regressions: B symptoms and social support predict STQ attendant symptoms (R2 = .28, F = 6.32, p < .001), predictors: emotional exhaustion (β = .27, p < .001) |
| Robinson (2017) Dissertation N = 129 full-time firefighters |
ProQOL | Regressions: personality type (neuroticism) predicts likelihood of developing a high risk of CF (R2 = 28.5%); EMS licence level and years of service were not sig. predictors for CF development |
| Setti and Argentero (2014) N = 176 firefighters |
STSS |
Correlations: mindfulness corr. with arousal (r = −.61, p < .01) and intrusion (r = −.45, p < .01); vigour (r = −.29, p < .01) and dedication (r = −.25, p < .01) corr. with arousal Regressions: mindfulness has inverse influence on arousal (β = −.59, p < .01) and intrusion (β = −.40, p = .01); seniority influences arousal (β = .40, p = .01) and intrusion (β = .38, p < .05); predictors explained 40% of arousal variance (R2 = .42, p = .01) and 18% of intrusion variance (R2 = .21, p < .01) |
| Setti et al. (2016) N = 782 rescuers |
STSS |
Correlations: affective commitment corr. with intrusion (r = −.081, p < .05), hyperarousal (r = −.183, p < .01), avoidance (r = −.277, p < .01); avoidance and hyperarousal not corr. with familial support; collegial support corr. with intrusion (r = −.077, p < .05), hyperarousal (r = −.139, p < .01), avoidance (r = −.196, p < .01) Regressions: social support and affective commitment explained 1.3% of intrusion variance (R2 = .02, p < .01), predictors: collegial support (β = −.094, p < .05), familial support (β = .089, p < .05); social support and affective commitment explained 10.3% of avoidance variance (R2 = .109, p < .01), predictors: affective commitment (β = −.239, p < .01), collegial support (β = −.116, p < .01), working position (β = −.095, p < .01); social support and affective commitment explained 4.8% of arousal variance (R2 = .054, p < .01), predictors: affective commitment (β = −.157, p < .01) |
| Tehrani (2016) N = 126 police officers; Internet child abuse investigators |
ProQOL |
Correlations: neuroticism positive corr. with anxiety (p < .001), depression (p < .001), PTSD (p < .001), B (p < .001), and STS (p < .001) Regressions: extraversion, neuroticism, and gender explained 20% of variance for anxiety, 30% for depression, 28% for PTSD, 20% for B, 22% for STS; neuroticism predicted anxiety (β = .42; p < .001), depression (β = .46; p < .001), PTSD (β = .40; p < .001), B (β = .35; p < .001), and STS (β = .40; p < .001); female gender predicted depression (β = −.15; p < .04), PTSD (β = −.25; p < .01), and STS (β = −.19; p < .05) |
| Tracy (2012) Dissertation N = 40 emergency medical technicians |
CS/CFST |
Correlations: CF corr. with B risk (R2 = .682, p < .01); not corr. with CS Regressions: facial expression and caregiver characteristics did not predict CF [F(9,39) = 1.249, p = .304], predictor: rank (β = .371, p < .05); personality measures and caregiver characteristics did not predict CF [F(8,39) = 1.886, p = .098], predictors: rank (β = .462, p < .05) and neuroticism (β = .432, p < .05) |
| Turgoose et al. (2017) N = 142 police officers |
ProQOL |
Correlations: CF, STS, B corr. with each other (r = .56–.66, all p < .001), but not strongly enough to warrant combining them into a single index; years working in training team of child exploitation and abuse corr. with CF (Spearman: r = .26, p < .01), STS (r = .40, p < .001) and B scores (r = .39, p < .001), results not replicated when comparing variables with years of overall experience; no corr. between CF or STS and empathy; no sig. relationships between CF, STS, B, and demographic variables of age, gender, and ethnicity |
B, burnout; CS, compassion satisfaction; CF, compassion fatigue; corr., correlation, correlated; CS/CFST, Compassion Satisfaction/Compassion Fatigue Self-Test; DP, depersonalization; EE, emotional exhaustion; EMS, emergency medical services; (I)CAC, (Internet) Crime Against Children; ns, not significant; PA, personal accomplishment; ProQOL, Professional Quality of Life; PTSD, post-traumatic stress disorder; sig., significant; ST, secondary trauma(tization); STQ, Secondary Trauma Questionnaire; STS, secondary traumatic stress; STSS, Secondary Traumatic Stress Scale.
Figure A1.
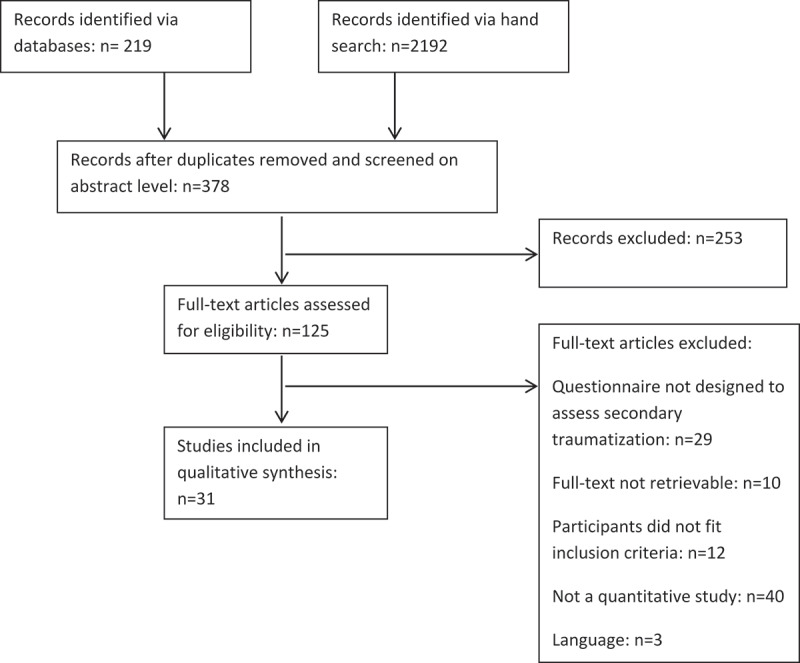
Flow diagram of study selection.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Adams R. E., Boscarino J. A., & Figley C. R. (2006). Compassion fatigue and psychological distress among social workers: A validation study. American Journal of Orthopsychiatry, 76(1), 103–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander D. A., & Klein S. (2001). Ambulance personnel and critical incidents. The British Journal of Psychiatry, 178(1), 76–81. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association Publishing. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Association Publishing. [Google Scholar]
- Amjad R., & Rafique R. (2013). Quality of life at work as predictor of job commitment in 1122 rescue workers. Pakistan Journal of Psychology, 44(1), 81–93. [Google Scholar]
- Argentero P., & Setti I. (2011). Engagement and vicarious traumatization in rescue workers. International Archives of Occupational and Environmental Health, 84(1), 67–75. [DOI] [PubMed] [Google Scholar]
- Battle L. (2011). Compassion fatigue, compassion satisfaction, and burnout among police officers who have experienced previous perceived traumas. (Doctoral dissertation). The University of Memphis, Memphis, TN; Retrieved from https://search.proquest.com/docview/923639624?pq-origsite=gscholar [Google Scholar]
- Becker-Nehring K., Witschen I., & Bengel J. (2012). Schutz- und Risikofaktoren für Traumafolgestörungen. Zeitschrift für Klinische Psychologie und Psychotherapie, 41, 148–165. [Google Scholar]
- Bellolio M. F., Cabrera D., Sadosty A. T., Hess E. P., Campbell R. L., Lohse C. M., & Sunga K. L. (2014). Compassion fatigue is similar in emergency medicine residents compared to other medical and surgical specialties. Western Journal of Emergency Medicine, 15(6), 629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedek D. M., Fullerton C., & Ursano R. J. (2007). First responders: Mental health consequences of natural and human-made disasters for public health and public safety workers. Annual Review of Public Health, 28, 55–68. [DOI] [PubMed] [Google Scholar]
- Bissett J. L. (2002). The relation between burnout and compassion fatigue in fire fighter-paramedics. (Doctoral dissertation). ProQuest Information & Learning. [Google Scholar]
- Bourke M. L., & Craun S. W. (2014). Coping with secondary traumatic stress: Differences between UK and US child exploitation personnel. Traumatology: An International Journal, 20(1), 57–64. [Google Scholar]
- Brewin C. R., Andrews B., & Valentine J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. [DOI] [PubMed] [Google Scholar]
- Bride B. E. (2004). The impact of providing psychosocial services to traumatized populations. Stress, Trauma, and Crisis, 7(1), 29–46. [Google Scholar]
- Bride B. E. (2007). Prevalence of secondary traumatic stress among social workers. Social Work, 52(1), 63–70. [DOI] [PubMed] [Google Scholar]
- Bride B. E., Robinson M. M., Yegidis B., & Figley C. R. (2004). Development and validation of the secondary traumatic stress scale. Research on Social Work Practice, 14(1), 27–35. [Google Scholar]
- Burns C. M., Morley J., Bradshaw R., & Domene J. (2008). The emotional impact on and coping strategies employed by police teams investigating internet child exploitation. Traumatology, 14(2), 20–31. [Google Scholar]
- Burruss G. W., Holt T. J., & Wall-Parker A. (2017). The hazards of investigating internet crimes against children: Digital evidence handlers’ experiences with vicarious trauma and coping behaviors. American Journal of Criminal Justice, 43(3), 433–447. [Google Scholar]
- Chiappo-West G. (2017). Compassion satisfaction, burnout, secondary traumatic stress, and work engagement in police officers in Arizona. (Doctoral dissertation). Grand Canyon University, Phoenix, AZ; Retrieved from https://search.proquest.com/docview/1947269887?pq-origsite=gscholar [Google Scholar]
- Cicognani E., Pietrantoni L., Palestini L., & Prati G. (2009). Emergency workers’ quality of life: The protective role of sense of community, efficacy beliefs and coping strategies. Social Indicators Research, 94(3), 449. [Google Scholar]
- Craig C. D., & Sprang G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress, & Coping, 23(3), 319–339. [DOI] [PubMed] [Google Scholar]
- Crampton D. J. (2014). Comparison of PTSD and compassion fatigue between urban and rural paramedics. (Doctoral dissertation). The University of the Rockies, Denver, CO; Retrieved from https://search.proquest.com/docview/1350627026?pq-origsite=gscholar [Google Scholar]
- Craun S. W., & Bourke M. L. (2015). Is laughing at the expense of victims and offenders a red flag? Humor and secondary traumatic stress. Journal of Child Sexual Abuse, 24(5), 592–602. [DOI] [PubMed] [Google Scholar]
- Daniels J. (2006). Sekundäre Traumatisierung: Kritische Prüfung eines Konstruktes. (Doctoral dissertation). Retrieved from http://www.sekundaertraumatisierung.de/sfSimpleBlog/show/stripped_title/materialien-und-artikel.html [Google Scholar]
- Deppa K. F., & Saltzberg J. (2016). Major factors that influence behavioral health in the fire service In Resilience training for firefighters (pp. 35–50). Cham: Springer. [Google Scholar]
- Döllinger A. (2014). Die Rolle personaler und sozialer Ressourcen bei posttraumatischer Belastung von Einsatzkräften des Roten Kreuzes Niederösterreich. (Diploma thesis). University of Vienna, Vienna, Austria; Retrieved from http://othes.univie.ac.at/32716/ [Google Scholar]
- Eriksson C. B., Kemp H. V., Gorsuch R., Hoke S., & Foy D. W. (2001). Trauma exposure and PTSD symptoms in international relief and development personnel. Journal of Traumatic Stress, 14(1), 205–212. [Google Scholar]
- Figley C. R. (1983). Catastrophes: An overview of family reactions In Figley C. R. & McCubbin H. I. (Eds.), Stress and the family: Vol. 2. Coping with catastrophe (pp. 3–20). New York, NY: Brunner/Mazel. [Google Scholar]
- Figley C. R. (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. Philadelphia, PA: Brunner/Mazel. [Google Scholar]
- Figley C. R. (1999). Compassion fatigue: Toward a new understanding of the cost of caring In Stamm B. H. (Ed.), Secondary traumatic stress (pp. 3–28). Towson, MD: Sidran Institute. [Google Scholar]
- Hargrave P. A.-L. (2010). Sudden death: The impact of the immediate aftermath on police officers, victim support workers, and bereaved survivors: A thesis presented in partial fulfilment of the requirements for the degree of doctor of philosophy in psychology at Massey University, Wellington. New Zealand: Massey University. [Google Scholar]
- Herman J. L. (1997). Trauma and recovery. New York, NY: Basic Books. [Google Scholar]
- Hofmann P. (2009). Addressing compassion fatigue. Healthcare Executive, 24(5), 40–41. [PubMed] [Google Scholar]
- Howell R. (2016). Investigating the relationship between personality factors and burnout in the Dublin Fire Brigade. (Diploma thesis). Retrieved from https://esource.dbs.ie/handle/10788/3165 [Google Scholar]
- Kleim B., & Westphal M. (2011). Mental health in first responders: A review and recommendation for prevention and intervention strategies. Traumatology, 17(4), 17–24. [Google Scholar]
- Krieger C. N., III (2017). Understanding the impact of secondary traumatic stress on crimes against children investigators. (Master's thesis). Tarleton State University, Stephenville, Texas; Retrieved from https://search.proquest.com/docview/1904391507?pq-origsite=gscholar [Google Scholar]
- Kronenberg M., Osofsky H. J., Osofsky J. D., Many M., Hardy M., & Arey J. (2008). First responder culture: Implications for mental health professionals providing services following a natural disaster. Psychiatric Annals, 38(2), 114–118. [Google Scholar]
- Krutolewitsch A., & Horn A. B. (2017). Posttraumatische Reifung nach berufsbezogener Traumatisierung bei Einsatzkräften. Die vermittelnde Rolle der sozio-interpersonellen Faktoren Disclosure und Co-Rumination. [Posttraumatic growth after profession-related traumatization in rescue workers. The mediating role of the socio-interpersonal factors disclosure and co-rumination] Psychotherapie, Psychosomatik, Medizinische Psychologie, 67(5), 203–211. [DOI] [PubMed] [Google Scholar]
- Krutolewitsch A., Horn A. B., & Maercker A. (2015). Trauma-Ausmaß und ausgewählte Prädiktoren in einer Studie mit Feuerwehr- und Rettungskräften. [Extent of trauma and some selected predictors in a study of rescue workers] Trauma. Zeitschrift für Psychotraumatologie und ihre Anwendungen, 13(3), 78–91. [Google Scholar]
- Krutolewitsch A., Horn A. B., & Maercker A. (2016). Co-Rumination im Kontext des sozio-interpersonellen Modells der PTBS. Zeitschrift für Klinische Psychologie und Psychotherapie, 45, 121–131. [Google Scholar]
- LaFauci Schutt J. M., & Marotta S. A. (2011). Personal and environmental predictors of posttraumatic stress in emergency management professionals. Psychological Trauma: Theory, Research, Practice, and Policy, 3(1), 8–15. [Google Scholar]
- Lane E. J., Lating J. M., Lowry J. L., & Martino T. P. (2009). Differences in compassion fatigue, symptoms of posttraumatic stress disorder and relationship satisfaction, including sexual desire and functioning, between male and female detectives who investigate sexual offenses against children: A pilot study. International Journal of Emergency Mental Health, 12(4), 257–266. [PubMed] [Google Scholar]
- Mahoney M. J. (1997). Psychotherapists’ personal problems and self-care patterns. Professional Psychology: Research and Practice, 28(1), 14–16. [Google Scholar]
- Motta R., & Joseph J. (1998). The secondary trauma questionnaire. Unpublished Scale. New York, NY: Hofstra University. [Google Scholar]
- Motta R. W., Hafeez S., Sciancalepore R., & Diaz A. B. (2001). Discriminant validation of the Modified Secondary Trauma Questionnaire. Journal of Psychotherapy in Independent Practice, 2(4), 17–25. [Google Scholar]
- Motta R. W., Kefer J. M., Hertz M. D., & Hafeez S. (1999). Initial evaluation of the secondary trauma questionnaire. Psychological Reports, 85(3), 997–1002. [DOI] [PubMed] [Google Scholar]
- Motta R. W., Newman C. L., Lombardo K. L., & Silverman M. A. (2004). Objective assessment of secondary trauma. International Journal of Emergency Mental Health, 6(2), 67–74. [PubMed] [Google Scholar]
- Nordahl S. (2016). Mental health in and psychosocial support for humanitarian field workers. A literature review. (Master's thesis). Retrieved from https://www.duo.uio.no/bitstream/handle/10852/51080/PSA4090-Master-thesis.pdf?sequence=1 [Google Scholar]
- Palestini L., Prati G., Pietrantoni L., & Cicognani E. (2009). La qualità della vita professionale nel lavoro di soccorso: Un contributo alla validazione italiana della Professional Quality of Life Scale (ProQOL). Psicoterapia Cognitiva e Comportamentale, 15(2), 205–227. [Google Scholar]
- Patterson G. T. (2009). Mental stress and workers’ compensation claims among police officers. Journal of Workplace Rights, 14(4), 441–455. [Google Scholar]
- Pearlman L. A., & Saakvitne K. W. (1995). Trauma and the therapist: Countertransference and vicarious traumatization in psychotherapy with incest survivors. New York, NY: WW Norton & Co. [Google Scholar]
- Piaget J. (1971). Psychology and epistemology. A. Rosin, trans New York, NY: Grossman. [Google Scholar]
- Pietrantoni L., & Prati G. (2008). Resilience among first responders. African Health Sciences, 8(Suppl 1), S14–S20. [PMC free article] [PubMed] [Google Scholar]
- Prati G., & Pietrantoni L. (2010a). The relation of perceived and received social support to mental health among first responders: A meta-analytic review. Journal of Community Psychology, 38(3), 403–417. [Google Scholar]
- Prati G., & Pietrantoni L. (2010b). An application of the social support deterioration deterrence model to rescue workers. Journal of Community Psychology, 38(7), 901–917. [Google Scholar]
- Prati G., Pietrantoni L., & Cicognani E. (2010). Self-efficacy moderates the relationship between stress appraisal and quality of life among rescue workers. Anxiety, Stress, & Coping, 23(4), 463–470. [DOI] [PubMed] [Google Scholar]
- Prati G., Pietrantoni L., & Cicognani E. (2011). Coping strategies and collective efficacy as mediators between stress appraisal and quality of life among rescue workers. International Journal of Stress Management, 18(2), 181–195. [Google Scholar]
- Regehr C., Hill J., & Glancy G. D. (2000). Individual predictors of traumatic reactions in firefighters. The Journal of Nervous and Mental Disease, 188(6), 333–339. [DOI] [PubMed] [Google Scholar]
- Reinhard F., & Maercker A. (2004). Sekundäre Traumatisierung, Posttraumatische Belastungsstörung, Burnout und Soziale Unterstützung bei medizinischem Rettungspersonal. Zeitschrift für Medizinische Psychologie, 13(1), 29–36. [Google Scholar]
- Robinson T. M. (2017). Predictive factors of compassion fatigue among firefighters. Ann Arbor, MI: ProQuest Information & Learning. [Google Scholar]
- Schmidt J. (2012). Feuerwehr. In C. Neitzel & K. Ladehof (Eds.), Taktische Medizin (pp. 307–311) Springer, Berlin: Heidelberg. [Google Scholar]
- Scott S. R. (2016). Prevalence of vicarious trauma in parole officers working with client specific caseloads. Ann Arbor, MI: ProQuest Information & Learning. [Google Scholar]
- Setti I., & Argentero P. (2012). Vicarious trauma: A contribution to the Italian adaptation of the secondary traumatic stress scale. Bollettino Di Psicologia Applicata, 264, 58–64. [Google Scholar]
- Setti I., & Argentero P. (2014). The role of mindfulness in protecting firefighters from psychosomatic malaise. Traumatology: An International Journal, 20(2), 134–141. [Google Scholar]
- Setti I., Lourel M., & Argentero P. (2016). The role of affective commitment and perceived social support in protecting emergency workers against burnout and vicarious traumatization. Traumatology, 22(4), 261–270. [Google Scholar]
- Sprang G., Clark J. J., & Whitt-Woosley A. (2007). Compassion fatigue, compassion satisfaction, and burnout: Factors impacting a professional’s quality of life. Journal of Loss and Trauma, 12(3), 259–280. [Google Scholar]
- Stamm B., & Figley C. (1996). Compassion satisfaction and fatigue test. Retrieved from https://cdn.ymaws.com/www.cpapsych.org/resource/resmgr/imported/files/clasp/articles/Compassion%20Satisfaction%20and%20Fatigue.pdf. [Google Scholar]
- Stamm B. H. (2002). Measuring compassion satisfaction as well as fatigue: Developmental history of the compassion satisfaction and fatigue test. In C. R. Figley (Ed.), Psychosocial stress series, no. 24. Treating compassion fatigue (pp. 107–119). New York, NY: Brunner-Routledge. [Google Scholar]
- Stamm B. H. (2005). The ProQol manual: The professional quality of life scale. Lutherville, MD: Sidran Press. Retrieved from http://compassionfatigue.org/pages/ProQOLManualOct05.pdf. [Google Scholar]
- Stamm B. H. (2010). The concise ProQOL manual. Pocatello, ID: Proqol.org. [Google Scholar]
- Summerfield D., Kleber R. J., Figley C. R., & Gersons B. P. (1995). Beyond Trauma: Cultural and societal dynamics. New York, NY: Plenum Press. [Google Scholar]
- Tehrani N. (2016). Extraversion, neuroticism and secondary trauma in Internet child abuse investigators. Occupational Medicine, 66(5), 403–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoreson R. W., Miller M., & Krauskopf C. J. (1989). The distressed psychologist: Prevalence and treatment considerations. Professional Psychology: Research and Practice, 20(3), 153–158. [Google Scholar]
- Tracy M. (2012). Behavioral and personality predictors of compassion satisfaction, compassion fatigue and burnout among Georgetown EMS providers. (Doctoral dissertation). Retrieved from https://repository.library.georgetown.edu/bitstream/handle/10822/556038/MTracy_Thesis_Final-1.pdf?sequence=1 [Google Scholar]
- Turgoose D., Glover N., Barker C., & Maddox L. (2017). Empathy, compassion fatigue, and burnout in police officers working with rape victims. Traumatology, 23(2), 205–213. [Google Scholar]
- Vrklevski L. P., & Franklin J. (2008). Vicarious trauma: The impact on solicitors of exposure to traumatic material. Traumatology, 14(1), 106–118. [Google Scholar]
- Walsh D. S. (2009). Interventions to reduce psychosocial disturbance following humanitarian relief efforts involving natural disasters: An integrative review. International Journal of Nursing Practice, 15(4), 231–240. [DOI] [PubMed] [Google Scholar]


