Abstract
Patient: Male, 27
Final Diagnosis: Appendicitis
Symptoms: Abdominal discomfort
Medication: —
Clinical Procedure: —
Specialty: Surgery
Objective:
Rare disease
Background:
Left-sided acute appendicitis, although well described in the literature, is still an easily missed diagnosis. Midgut malrotation and situs inversus are 2 known leading conditions that contribute to misdiagnosis of appendicitis.
Case Report:
Here is the case of a 27-year-old male without any previous medical history, who presented with left lower quadrant tenderness and was misdiagnosed with gastroenteritis as an outpatient and sent home; the patient presented the next day to the emergency department where he was found to have acute appendicitis with situs inversus. He underwent laparoscopic appendectomy where a phlegmon was identified. Pathology came back as peri-appendiceal mucocele with no signs of malignancy.
Conclusions:
This case report aimed to revisit the idea of left-sided acute appendicitis and discuss the management of a perforated appendiceal mucocele contained by a phlegmon.
MeSH Keywords: Abdominal Pain, Appendectomy, Appendicitis
Background
Acute appendicitis is still of the most frequently diagnosis that requires emergency surgery. The diagnosis is simple and straightforward, and it depends on multiple previously well-established criteria including physical symptoms, findings on imaging modalities, and a surgeon’s clinical experience [1,2]. The current gold standard for diagnosis is radiological investigation with an abdominal-pelvic computed tomography (CT) scan with intravenous contrast and CT scan signs of acute appendicitis were described and overall, CT scan was found to be highly accurate for diagnosis of acute appendicitis [3]. Mortality increases if surgical treatment is delayed, which is most often caused by misdiagnosis of acute appendicitis and is more likely to occur with patients who present atypically, are not thoroughly examined, are given narcotic pain medication and then discharged from the emergency department, are diagnosed as having gastroenteritis, and with patients who do not receive appropriate discharge or follow-up instructions. Some studies have reported misdiagnosis rates to be as high as 24% [4]. Another increasing cause of misdiagnosis is left-sided acute appendicitis.
Left lower quadrant tenderness caused by acute appendicitis is a rare phenomenon. It can be caused by an abnormal left-sided location of the appendix, usually as a result of a congenital malformation, or by a right-sided long appendix, projecting into the left lower quadrant area [5]. Major etiologies of left-sided acute appendicitis include 2 congenital anomalies: midgut malrotation and situs inversus totalis [6].
We report here the case of a 27-year-old male who presented with symptoms of left lower quadrant pain; the patient was diagnosed, eventually, with left-sided acute appendicitis.
The aim of this report was to revisit the idea of left-sided acute appendicitis and delayed definitive management in patients with left lower quadrant pain and to present an unusual cause of acute appendicitis.
Case Report
A previously healthy 27-year-old male patient presented to our emergency department with 3-day severe left lower quadrant pain.
His pain started 3 days prior to admission in the periumbilical area and was crampy in nature. He had no signs of fever and no change in bowel habits. On the second day of pain, he consulted his physician and was diagnosed with a case of gastroenteritis and was given antibiotics (ciprofloxacin and metronidazole) for treatment.
On the day of admission, his pain did not improve and migrated to the left lower quadrant area which then prompted his visit to our institution. On physical examination, his abdomen was non-remarkable except for guarding in the left lower quadrant area. McBurney sign was negative. A complete blood count was done and showed a normal white count of 8500 mL of blood with a left shift. His C-reactive protein level was high at 196 mg/L. An abdominal-pelvic CT scan with intravenous contrast was done and showed that the patient had actually a congenital midgut malrotation of the small bowel to the right and a left-sided caecum (Figures 1, 2). The cause of his pain was actually an inflamed left-sided appendix complicated by a peri-appendiceal phlegmon formation (Figures 3, 4).
Figure 1.

Abdominal-pelvic computed tomography scan showing small bowels (white arrow) occupying the right side of the abdomen.
Figure 2.
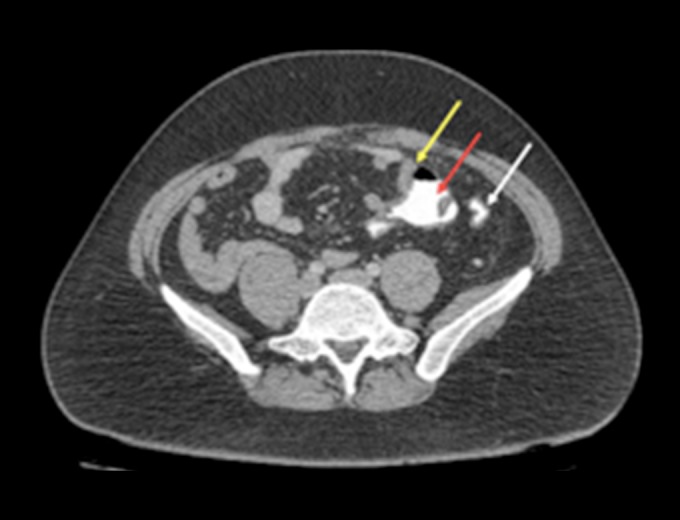
Abdominal-pelvic computed tomography scan showing the terminal ileum on the left side (yellow arrow) entering the caecum (red arrow) next to the sigmoid colon filled with contrast material (white arrow).
Figure 3.
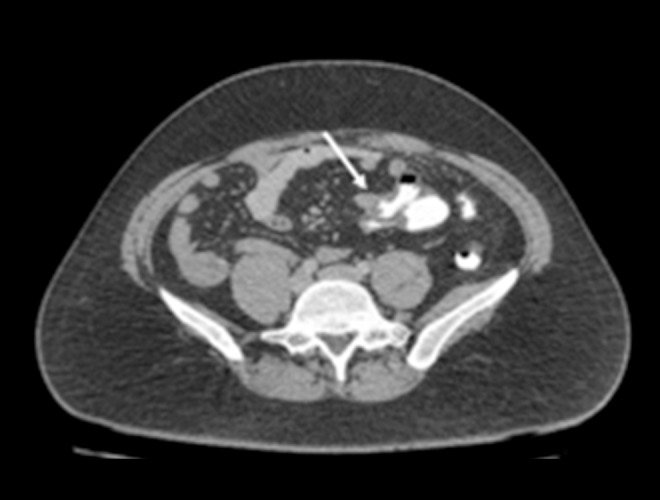
Abdominal-pelvic computed tomography scan with intravenous and PO contrast showing a thickened and inflamed appendix with a peri-appendiceal phlegmon and fat stranding with the caecum on the left side (white arrow).
Figure 4.

Coronal view of the same image of Figure 3.
We admitted the patient and subsequently operated on him with a laparoscopic appendectomy. We inserted our trocars in the following areas: 1×10 mm in the infraumbilical area, another 10 mm in the right lower quadrant area and a final 5 mm in the suprapubic area. We confirmed that the ileo-ceacal valve and caecum were present on the left side adjacent to the sigmoid (Figure 5). We identified the inflamed appendix and noted a hard structure encompassing its tip, reminiscent of a phlegmon. We proceeded to devascularize the mesoappendix and transect the appendix after using 2 endoloops. The specimen (Figure 6) was removed using an endobag. We assured hemostasis was adequate and then closed all the layers of the abdominal wall.
Figure 5.
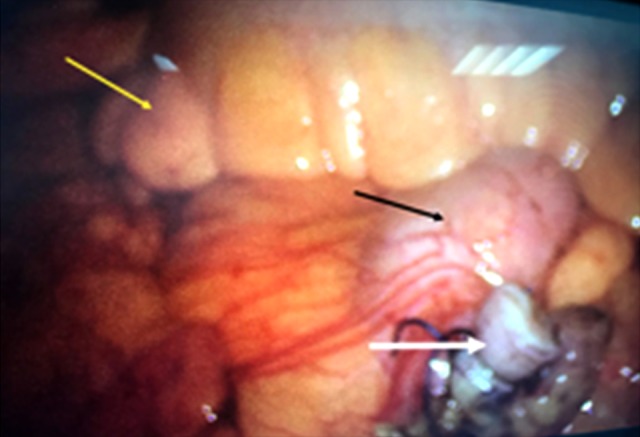
Intraoperative picture showing the appendiceal stump (white arrow) and the ceacum (black arrow) located next to the sigmoid colon (yellow arrow).
Figure 6.
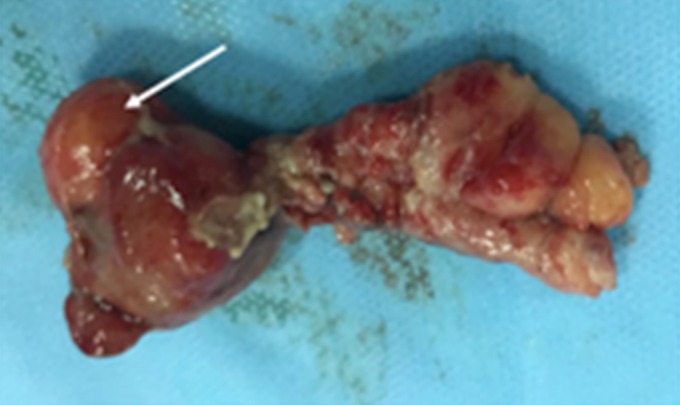
Photograph of the removed appendix with the phlegmon (white arrow).
The patient was started on clear fluid diet the following day, which was gradually progressed and was finally discharged home on post-operative day 1. Upon discharge, the patient was in very good physical condition and tolerating his diet. Pathology results came back for acute diverticular appendicitis with peri-appendiceal mucocele without any lymphovascular invasion or any signs of malignancy. Because we found during the operation that the patient had an appendiceal phlegmon, we concluded that this was a case of perforated yet contained appendiceal mucocele located at the tip.
Discussion
Multiple differential diagnosis can be cited for left lower abdominal pain including acute diverticulitis (which is most prominent in the elderly), and a long right-sided acute appendicitis and a left-side acute appendicitis, which are most likely encountered in the younger population) and left-sided primary epiploic appendagitis. Acute appendicitis is still the most common surgical emergency with low morbidity and mortality if surgical treatment is not delayed [1]. A delay in diagnosis is one of the main causes of perforated appendicitis. Physicians should be cautious of delaying surgery for acute appendicitis since after 36 hours of untreated symptoms, the risk of perforation is increased by 5% for every 12-hour period [7]. Abdominal CT should be used to prevent any type of misdiagnosis [3].
Midgut malrotation and situs inversus are 2 uncommon causes of left-sided acute appendicitis. Based on current literature, midgut malrotation has an incidence rate up to 0.5% [1,8–10]. Situs inversus totalis is a similarly uncommon condition with an incidence of up to 0.01% [11,12]. The latter may be complete situs inversus totalis, with transposition of thoraco-abdominal organs, or partial situs inversus, when the transposition concerns only one cavity [1]. The incidence of situs inversus totalis associated acute appendicitis is rarely found in up to 0.024% of appendicitis cases [11,12]. Due to having pain in the left lower quadrant area, physicians may misdiagnosis the condition and delay management. An abnormally placed appendix is the reason why left-sided acute appendicitis is still a problematic predicament and is one of the reasons why acute appendicitis is still misdiagnosed [13].
We presented an uncommon diagnosis of left-sided acute appendicitis which had also an uncommon cause being an appendiceal mucocele. The aim was to make resurface left-sided acute appendicitis as a differential diagnosis for left lower quadrant pain, decrease the risk of misdiagnosis and highlight the management plan concerning an appendiceal mucocele phlegmon. In our patient, the mucocele had no lymphovascular invasion and was limited to the appendiceal tip. Our management by laparoscopic appendectomy was in our opinion as for initial management without any need for subsequent follow up [14].
In our review of the literature, we concluded that a simple appendectomy is the most beneficial approach in scenarios with the following criteria: 1) benign appendiceal mucocele, 2) negative margins of resection, and 3) no signs of perforation and more than 2 cm away from the base.
On the other hand, for patients presenting with a perforated condition, and/or having positive resection margins, and/or presenting with appendiceal lymphadenopathy, the management would be different. The preferred approach to would be a right colectomy associated with a debulking cytoreductive surgery combined with intraperitoneal chemotherapy. The latter would be administered either by heated intra-peritoneal chemotherapy or early post-operative intra-peritoneal chemotherapy [15].
If perforation is present with positive resection margins, positive cytology, and negative appendiceal lymph nodes, then the surgical management would be limited to a caecectomy, debulking cytoreductive surgery, and heated intra-peritoneal chemotherapy or early post-operative intra-peritoneal chemotherapy.
Lastly, if the perforation is present with only a positive cytology (negative resection margins and negative appendiceal lymph nodes), the surgical approach would be limited to an appendectomy and debulking cytoreductive surgery combined with heated intra-peritoneal chemotherapy or early post-operative intra-peritoneal chemotherapy [15].
As the laparoscopic era continues to evolve, this method of re-section has been being more widely used as initial management for resection of appendiceal mucocele. The laparoscopic approach should be discontinued and replaced by the open approach for any of the following: 1) trauma to the surgical specimen while being grasped, 2) clear extension of the tumor beyond the appendix, and 3) signs of disseminated malignant disease including peritoneal deposits [16].
A recent small series of 8 patients with appendiceal mucocele showed similar long-term results if the excision was performed either by the laparoscopy or the open approach [17].
Our patient had an appendiceal mucocele phlegmon, which theoretically is a perforated mucocele, however, in our case the perforation was encompassed by the mesoappendix, limiting it from reaching the peritoneal cavity. We opted for a laparoscopic appendectomy and subsequent follow-up by a colonoscopy done 4 weeks post-operative and repeated with CT imaging 6 months later, which showed no signs of remnant or recurrent disease. CT imaging will be repeated in another 6 months. If later there are any signs of peritoneal dissemination found, we will refer the patient for heated intra-peritoneal chemotherapy treatment.
Conclusions
Acute appendicitis will always be a common surgical emergency. Swift diagnosis will lead to a favorable prognosis. A misdiagnosis, however, will lead to detrimental consequences. Left-sided acute appendicitis is a more and more frequent cause of misdiagnosis in acute appendicitis, and it should always be considered in any patient having left lower quadrant pain especially in the younger aged population. Appendiceal mucocele is also one of the causes of acute appendicitis. Management of appendiceal mucocele has been described in the literature, however, in borderline cases, similar to our case concerning patients with a mucocele phlegmon, information is still scarce.
References:
- 1.Akbulut S, Caliskan A, Ekin A, Yagmur Y. Left-sided acute appendicitis with situs inversus totalis: Review of 63 published cases and report of two cases. J Gastrointest Surg. 2010;14(9):1422–28. doi: 10.1007/s11605-010-1210-2. [DOI] [PubMed] [Google Scholar]
- 2.Hou SK, Chern CH, How CK, et al. Diagnosis of appendicitis with left lower quadrant pain. J Chin Med Assoc. 2005;68(12):599–603. doi: 10.1016/S1726-4901(09)70101-7. [DOI] [PubMed] [Google Scholar]
- 3.Rao PM, Rhea JT, Novelline RA. Sensitivity and specificity of the individual CT signs of appendicitis: Experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr. 1997;21(5):686–92. doi: 10.1097/00004728-199709000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Kryzauskas M, Danys D, Poskus T, et al. Is acute appendicitis still misdiagnosed? Open Med (Wars) 2016;11(1):231–36. doi: 10.1515/med-2016-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hou SK, Chern CH, How CK, et al. Diagnosis of appendicitis with left lower quadrant pain. J Chin Med Assoc. 2005;68(12):599–603. doi: 10.1016/S1726-4901(09)70101-7. [DOI] [PubMed] [Google Scholar]
- 6.Akbulut S, Ulku A, Senol A, et al. Left-sided appendicitis: Review of 95 published cases and a case report. World J Gastroenterol. 2010;16(44):5598–602. doi: 10.3748/wjg.v16.i44.5598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagner PL, Eachempati SR, Soe K, et al. Defining the current negative appendectomy rate: For whom is preoperative computed tomography making an impact? Surgery. 2008;144(2):276–82. doi: 10.1016/j.surg.2008.03.040. [DOI] [PubMed] [Google Scholar]
- 8.Franklin ME, Jr, Almeida JA, Pérez ER, et al. Cholecystectomy and appendectomy by laparoscopy in a patient with situs inversus totalis: A case report and review of the literature. Asoc Mex Cir Endoscopica. 2001;2(3):150–53. [Google Scholar]
- 9.Israelit S, Brook OR, Nira BR, et al. Left-sided perforated acute appendicitis in an adult with midgut malrotation: the role of computed tomography. Emerg Radiol. 2009;16(3):217–18. doi: 10.1007/s10140-008-0746-x. [DOI] [PubMed] [Google Scholar]
- 10.Welte FJ, Grosso M. Left-sided appendicitis in a patient with congenital gastrointestinal malrotation: A case report. J Med Case Rep. 2007;1:92. doi: 10.1186/1752-1947-1-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Golash V. Laparoscopic management of acute appendicitis in situs inversus. J Minim Access Surg. 2006;2(4):220–21. doi: 10.4103/0972-9941.28184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang SM, Yao CC, Tsai TP, Hsu GW. Acute appendicitis in situs inversus totalis. J Am Coll Surg. 2008;207(6):954. doi: 10.1016/j.jamcollsurg.2008.03.030. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed JU, Hossain GMZ, Karim MM, et al. Left sided acute appendicitis with situs inversus in an elderly – an unusual case. Journal of Chittagong Medical College Teachers’ Association. 2007;18(1):29–31. [Google Scholar]
- 14.Park KJ, Choi HJ, Kim SH. Laparoscopic approach to mucocele of appendiceal mucinous cystadenoma: feasibility and short-term outcomes in 24 consecutive cases. Surg Endosc. 2015;29(11):3179–83. doi: 10.1007/s00464-014-4050-4. [DOI] [PubMed] [Google Scholar]
- 15.Palanivelu C, Rangarajan M, John SJ, et al. Laparoscopic right hemicolectomy for mucocele due to a low-grade appendiceal mucinous neoplasm. JSLS. 2008;12(2):194–97. [PMC free article] [PubMed] [Google Scholar]
- 16.Navarra G, Asopa V, Basaglia E, et al. Mucous cystadenoma of the appendix: Is it safe to remove it by a laparoscopic approach? Surg Endosc. 2003;17(5):833–34. doi: 10.1007/s00464-002-4266-6. [DOI] [PubMed] [Google Scholar]
- 17.Rangarajan M, Palanivelu C, Kavalakat AJ, Parthasarathi R. Laparoscopic appendectomy for mucocele of the appendix. Indian J Gastroenterol. 2006;25:256–57. [PubMed] [Google Scholar]


