Abstract
Objective
To summarize the 2018 Diabetes Canada clinical practice guidelines, focusing on high-priority recommendations for FPs managing people who live with type 2 diabetes.
Quality of evidence
A prioritization process was conducted to focus the efforts of Diabetes Canada’s guideline dissemination and implementation efforts. The resulting identified key messages for FPs to consider when managing patients with type 2 diabetes are described. Evidence supporting the guideline recommendations ranges from levels I to IV and grades A to D.
Main message
Three key messages were identified from the 2018 guidelines as priorities for FPs: discussing opportunities to reduce the risk of diabetes complications, discussing opportunities to ensure safety and prevent hypoglycemia, and discussing progress on self-management goals and addressing barriers. A theme cutting across these key messages was the need to tailor discussions to the needs and preferences of each person. These important guideline recommendations are highlighted, along with information about relevant tools for implementing the recommendations in real-world practice.
Conclusion
High-quality diabetes care involves a series of periodic conversations about self-management and about pharmacologic and nonpharmacologic treatments that fit with each patient’s goals (ie, shared decision making). Incorporating these conversations into regular practice provides FPs with opportunities to maximize likely benefits of treatments and decrease the risk of harms, to support patients in initiating and sustaining desired lifestyle changes, and to help patients cope with the burdens of diabetes and comorbid conditions.
Family doctors and other primary care clinicians provide most of the care for Canadians living with diabetes and its complications.1 The increasing number and complexity of cases of this chronic disease2 provides an opportunity to ensure better supports are in place for persons with diabetes and their care providers. Given recent pharmacologic advances, as well as new evidence about the potential for specific benefits and harms, clinicians today are faced with a range of options when selecting the most appropriate treatment approach for people with diabetes. The challenge for FPs is compounded by the vast amount of new evidence available on a range of clinical topics relevant to the people with diabetes whom they see in their practices. Guidelines help to summarize evidence, but it is not feasible3 or appropriate4 for FPs to incorporate every single guideline recommendation relevant to primary care into practice. Which high-priority items deserve attention and action? Which recommendations should FPs make a special effort to understand and discuss with their patients?
Guidelines do not implement themselves.5 To integrate guideline recommendations into routine clinical care, FPs must not only be aware of and agree with them, but also must be able to adopt and adhere to them whenever applicable.6 To this end, a clinical practice guideline dissemination and implementation (D&I) committee, composed of interprofessional diabetes providers from across the country (some of whom contributed to writing the guideline but many of whom did not), was organized by Diabetes Canada to develop strategies for both people with diabetes and providers, hoping to support translating evidence-based recommendations into practice. Evaluation of the effects of these efforts is ongoing.7
The “Diabetes Canada 2018 clinical practice guidelines for the prevention and management of diabetes in Canada” were published in April 2018.8 As part of the dissemination effort, a series of readable articles summarizing high-priority recommendations for primary care providers and outlining easy-to-apply practices were planned. This article summarizes the new guidelines, focusing on high-priority recommendations for FPs managing people who live with type 2 diabetes. Herein, we present these guideline recommendations and link these recommendations to approaches and tools that will help FPs put them into practice.
Quality of evidence
Diabetes Canada is a health charity and advocacy organization that produces comprehensive national guidelines for the prevention and management of diabetes in adults and children, with a focus on special populations (those with renal failure, Indigenous peoples, women of child-bearing age, etc). Following a rigorous methodology,9,10 a guideline writing committee, composed of interprofessional diabetes experts, posed then answered clinically relevant questions, resulting in a series of recommendations.10 The evidence supporting the recommendations ranges from levels I to IV and grades A to D.8 The Diabetes Canada guideline committee includes primary care practitioners, endocrinologists, diabetes educators, other specialists, and people living with diabetes from across Canada. The resulting diabetes guideline is reviewed and launched in a 5-year cycle, with interim revisions in the event of important practice-changing evidence and treatment options. For the 2018 guidelines, 9 of the 10 authors responsible for developing recommendations for pharmacologic management of type 2 diabetes had no conflicts of interest with industry. In the case of disagreement about conflicts or outright conflicts of interest, committee members removed themselves from discussions. This article does not attempt to revise or critique the Diabetes Canada guideline recommendations but presents a family medicine–oriented approach to applying relevant recommendations in practice.
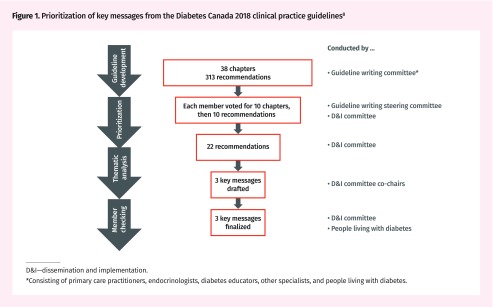
The guideline D&I committee co-chairs developed a process of prioritizing and distilling key messages relevant to primary care from 313 recommendations in 38 guideline chapters (Figure 1).8 The prioritization was completed anonymously by members of the guideline writing committee, people with diabetes, and members of the D&I committee. Given the large number of recommendations, the first step of the prioritization exercise was to select guideline chapters; each member was asked to select 10 chapters, then, from these chapters, to select and rank 10 recommendations. Based on the number of votes for each recommendation, a list of 22 recommendations was compiled. This was followed by thematic analysis and member checking to summarize key messages. Specifically, the co-chairs (endocrinologist C.H.Y. and FP N.M.I.) collaboratively sorted the recommendations into conceptually similar groups (themes) and drafted key messages that represented these themes. Next, they sought input from the committee members to refine the key messages, similar to the process of member checking in qualitative research.11
Figure 1.
Prioritization of key messages from the Diabetes Canada 2018 clinical practice guidelines8
D&I—dissemination and implementation.
*Consisting of primary care practitioners, endocrinologists, diabetes educators, other specialists, and people living with diabetes.
For this manuscript, we sought further input from FPs on the D&I committee to ensure that no important recommendations or concepts had been missed in summarizing the high-priority aspects of the guideline for the management of people with type 2 diabetes by FPs. This involved providing these FPs with the full list of recommendations via e-mail and asking them to identify any missing high-priority recommendations. During the process of converting themes into key messages, and during the process of writing this manuscript, input was sought from members of the D&I committee who live with diabetes to ensure that the content was informed by their needs and perspectives. As a final step, the entire committee identified tools that might support implementation of the key messages. To the extent possible, tools are informed by evidence regarding implementation of evidence in practice.12–15 Some of these tools are identified in this manuscript; these and many others can be accessed at guidelines.diabetes.ca.
Main message
The prioritization exercise resulted in 22 recommendations nominated for emphasis in dissemination and implementation efforts. These were then categorized into 3 key messages (Table 1)8,16 and a cross-cutting theme, as described below.
Table 1.
Selected high-priority type 2 diabetes recommendations and relevant tools for FPs: Highlighted recommendations were prioritized for dissemination by those involved in preparing this review. They are not presented in any particular order and are not necessarily the most important recommendations for a given practice or patient; the full guideline is available at guidelines.diabetes.ca.
| KEY MESSAGE | GUIDELINE RECOMMENDATION | RELEVANT TOOLS |
|---|---|---|
| Discuss opportunities to reduce the risk of diabetes complications | If glycemic targets are not achieved with existing antihyperglycemic medications, other classes of agents should be added to improve glycemic control. The choice should be individualized taking into account the information below and in Figure 28 (grade B, level II) In people without clinical CVD in whom glycemic targets are not achieved with existing antihyperglycemic medication, incretin agents (DPP4Is or GLP1RAs) or SGLT2Is should be considered as add-on medication over insulin secretagogues, insulin, and TZDs to improve glycemic control, if lower risk of hypoglycemia or weight gain are priorities (grade A, level IA). Acarbose and orlistat can also be considered as add-on medication to improve glycemic control with a low risk of hypoglycemia and weight gain (grade D, consensus) In people with clinical CVD in whom glycemic targets are not achieved with existing antihyperglycemic medication, an antihyperglycemic agent with demonstrated CV outcome benefit should be added to reduce the risk of major CV events (grade A, level IA for empagliflozin; grade A, level IA for liraglutide; grade C, level II for canagliflozin) |
Interactive tool for selecting agents for glycemic control: guidelines.diabetes.ca/bloodglucoselowering/pharmacologyt2 |
| Insulin can be used at any time in the course of type 2 diabetes (grade D, consensus) (see link in Relevant Tools column for examples of insulin initiation and titration in people with type 2 diabetes). In people not achieving glycemic targets with existing non-insulin antihyperglycemic medication, the addition of a once-daily basal insulin regimen should be considered over premixed insulin or bolus-only regimens to reduce weight gain and hypoglycemia (grade B, level II) Long-acting insulin analogues should be considered over NPH insulin to reduce the risk of nocturnal and symptomatic hypoglycemia (grade A, level IA) In people receiving insulin, doses should be adjusted or additional antihyperglycemic medication (non-insulin or bolus insulin) should be added if glycemic targets are not achieved (grade D, consensus)
|
Insulin prescription tool: guidelines.diabetes.ca/reduce-complications/insulin-prescription-tool Examples of insulin initiation and titration in people with type 2 diabetes: guidelines.diabetes.ca/docs/cpg/Appendix-9.pdf |
|
All individuals with diabetes should follow a comprehensive, multifaceted approach to reducing CV risk, including the following:
ACEIs or ARBs, at doses that have demonstrated vascular protection, should be used to reduce CV risk in adults with type 1 or type 2 diabetes with any of the following:
In people with established CVD, low-dose ASA therapy (81–162 mg) should be used to prevent CV events (grade B, level II) ASA should not be used routinely for the primary prevention of CVD in people with diabetes (grade A, level IA). ASA can be used in the presence of additional CV risk factors (grade D, consensus) Clopidogrel 75 mg can be used in people unable to tolerate ASA (grade D, consensus) In adults with type 2 diabetes with clinical CVD in whom glycemic targets are not achieved with existing antihyperglycemic medication, an antihyperglycemic agent with demonstrated CV outcome benefit should be added to reduce the risk of major CV events (grade A, level IA for empagliflozin; grade A, level IA for liraglutide; grade C, level II for canagliflozin) |
Flow sheets: guidelines.diabetes.ca/docs/cpg/Appendix-3.pdf Interactive tool for selecting agents for vascular protection: guidelines.diabetes.ca/vascularprotection/riskassessment |
|
| Discuss opportunities to ensure safety and prevent hypoglycemia | Drivers with diabetes treated with insulin secretagogues or insulin ...
If any of the following occur, health care professionals should inform people with diabetes treated with insulin secretagogues or insulin to no longer drive, and should report their concerns about the person’s fitness to drive to the appropriate driving licensing body:
|
Educational handout for safe driving: guidelines.diabetes.ca/docs/patient-resources/drive-safe-with-diabetes.pdf |
| BP targets should be individualized for older adults who are functionally dependent, or who have orthostasis, or who have a limited life expectancy (grade D, consensus) In older patients with diabetes and multiple comorbidities or frailty, strategies should be used to strictly prevent hypoglycemia, which include the choice of antihyperglycemic therapy and less-stringent HbA1c targets (grade D, consensus). Antihyperglycemic agents that increase the risk of hypoglycemia or have other side effects should be discontinued in these people (grade C, level III) A higher HbA1ctarget can be considered in older people with diabetes taking antihyperglycemic agents with risk of hypoglycemia, with any of the following (grade D, consensus for all) ...
In older people with type 2 diabetes with no other complex comorbidities but with clinical CVD and in whom glycemic targets are not achieved with existing antihyperglycemic medications, an antihyperglycemic agent with demonstrated CV outcome benefit could be added to reduce the risk of major CV events (grade A, level IA for empagliflozin; grade A, level IA for liraglutide; grade C, level II for canagliflozin) |
Interactive tool for individualizing HbA1c target: guidelines.diabetes.ca/reduce-complications/a1ctarget Interactive tool for selecting agents for glycemic control: guidelines.diabetes.ca/bloodglucoselowering/pharmacologyt2 Therapeutic considerations for renal impairment: guidelines.diabetes.ca/docs/cpg/Appendix-7.pdf |
|
| Adults with diabetes and CKD should be given a “sick-day” medication list that outlines which medications should be held during times of acute illness (grade D, consensus) | Sick-day planning handout: guidelines.diabetes.ca/docs/cpg/Appendix-8.pdf |
|
| Discuss progress on self-management goals and address barriers | Individuals with diabetes should be regularly screened for diabetes-related psychological distress (eg, diabetes distress, psychological insulin resistance, fear of hypoglycemia) and psychiatric disorders (eg, depression, anxiety disorders) by validated self-report questionnaire or clinical interview (grade D, consensus). Plans for self-harm should be asked about regularly as well (grade C, level III) | Handouts about self-management: guidelines.diabetes.ca/patientresources |
Collaborative care by interprofessional teams should be provided for individuals with diabetes and depression to improve the following:
|
Handouts about identifying and managing diabetes-related distress: guidelines.diabetes.ca/selfmanagementeducation/psychosocial |
|
| People with diabetes should ideally accumulate a minimum of 150 min of moderate- to vigorous-intensity aerobic exercise each wk, spread over at least 3 d of the wk, with no more than 2 consecutive d without exercise, to improve glycemic control (grade B, level II) and to reduce risk of CVD and overall mortality (grade C, level III). Smaller amounts (90–140 min/wk) of exercise or planned physical activity can also be beneficial for glycemic control but to a lesser extent (grade B, level II) Interval training (short periods of vigorous exercise alternating with short recovery periods at low to moderate intensity or rest from 30 s to 3 min each) can be recommended to people willing and able to perform such training to increase gains in cardiorespiratory fitness in type 2 diabetes (grade B, level II) People with diabetes (including elderly people) should perform resistance exercise at least twice a wk and preferably 3 times/wk (grade B, level II) in addition to aerobic exercise (grade B, level II). Initial instruction and periodic supervision by an exercise specialist can be recommended (grade C, level III) Setting specific exercise goals, problem solving potential barriers to physical activity, providing information on where and when to exercise, and self-monitoring should be performed collaboratively between the person with diabetes and the health care provider to increase physical activity and improve HbA1c levels (grade B, level II) In addition to achieving physical activity goals, people with diabetes should minimize the amount of time spent in sedentary activities and periodically break up long periods of sitting (grade C, level III) People with diabetes should be offered timely self-management education that is tailored to enhancing self-care practices and behaviour (grade A, level IA) Technologies, such as Internet-based computer programs and glucose monitoring systems, brief text messages, and mobile applications can be used to support self-management in order to improve glycemic control (grade A, level IA) |
Interactive tool to provide specific exercise advice: guidelines.diabetes.ca/selfmanagementeducation/patool Sample exercise prescriptions for patients with diabetes: guidelines.diabetes.ca/docs/resources/diabetes-and-physical-activity-your-exercise-prescription.pdf |
ACEI—angiotensin-converting enzyme inhibitor, ARB—angiotensin receptor blocker, ASA—acetylsalicylic acid, BG—blood glucose, BP—blood pressure, CGM—continuous glucose monitoring, CKD—chronic kidney disease, CV—cardiovascular, CVD—cardiovascular disease, DPP4I—dipeptidyl peptidase 4 inhibitor, GLP1RA—glucagonlike peptide 1 receptor agonist, HbA1c—hemoglobin A1c, LDL-C—low-density lipoprotein cholesterol, MR—modified release, NPH—neutral protamine Hagedorn, PCSK9—proprotein convertase subtilisin-kexin type 9, SGLT2I—sodium glucose transporter 2 inhibitor, SMBG—self-monitoring of blood glucose, TZD—thiazolidinedione.
Grades and levels of evidence are defined in the methods chapter of the guidelines (guidelines.diabetes.ca/browse/chapter2). Briefly, grade A and level I evidence is the strongest and most relevant. Level IV evidence is the weakest, and grade D recommendations are supported by level IV evidence or consensus.8
Data from the Diabetes Canada Clinical Practice Guidelines Expert Committee.8
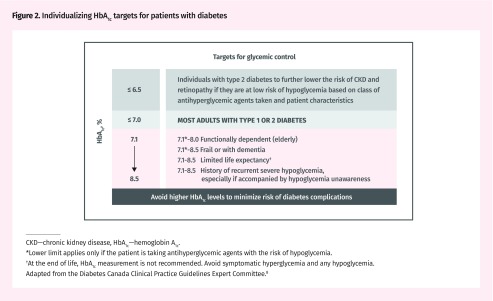
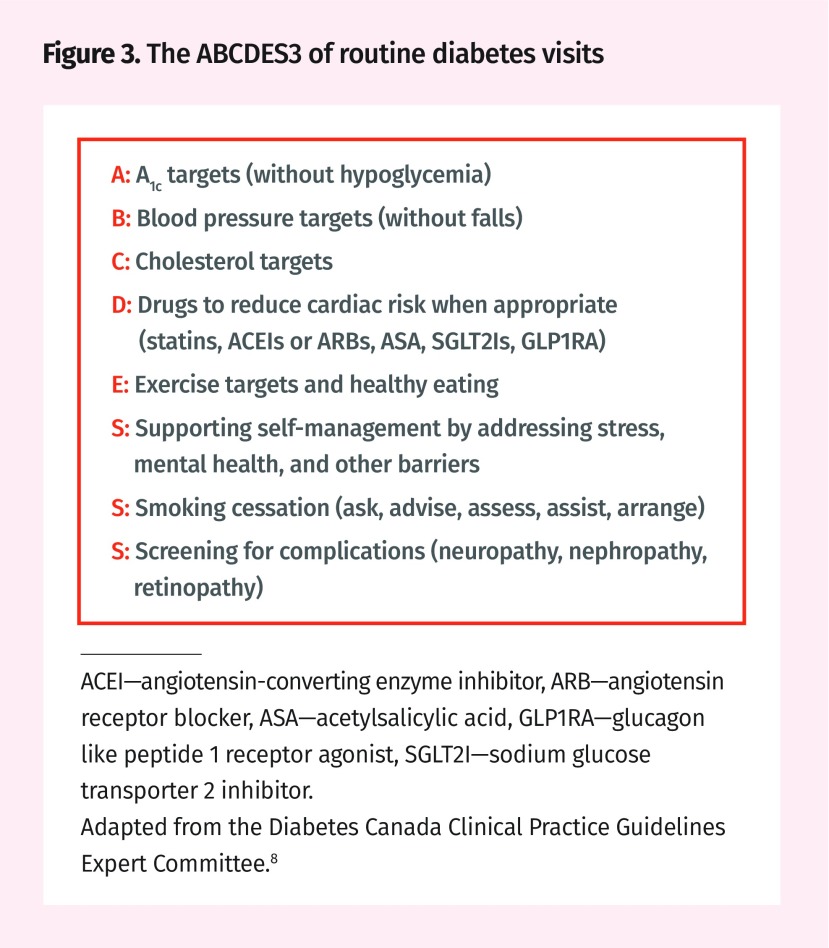
Providing care that is concordant with the latest guidelines requires repeated discussions featuring shared decision making with people with diabetes about opportunities to reduce the risk of diabetes complications, keep patients safe, and support self-management. For this reason, long-term and short-term risks must be balanced in a way that incorporates consideration of each person’s needs, preferences, and capabilities, along with the research evidence and clinician judgment. For example, glycemic targets will vary based on patient circumstances (Figure 2).8 The recommendations highlighted here presume that diabetes care is being provided in an ongoing, relationship-based primary care context, in which repeated consultations occur to routinely and iteratively set care goals and develop plans to achieve them. A revised acronym was developed as an aid to facilitate rapid assessment and action that incorporates the key messages presented here during these routine diabetes visits: ABCDES3 (Figure 3).8
Figure 2.
Individualizing HbA1c targets for patients with diabetes
CKD—chronic kidney disease, HbA1c—hemoglobin A1c.
*Lower limit applies only if the patient is taking antihyperglycemic agents with the risk of hypoglycemia.
†At the end of life, HbA1c measurement is not recommended. Avoid symptomatic hyperglycemia and any hypoglycemia.
Adapted from the Diabetes Canada Clinical Practice Guidelines Expert Committee.8
Figure 3.
The ABCDES3 of routine diabetes visits
ACEI—angiotensin-converting enzyme inhibitor, ARB—angiotensin receptor blocker, ASA—acetylsalicylic acid, GLP1RA—glucagon like peptide 1 receptor agonist, SGLT2I—sodium glucose transporter 2 inhibitor.
Adapted from the Diabetes Canada Clinical Practice Guidelines Expert Committee.8
As part of the guideline dissemination and implementation, Diabetes Canada produced updated diabetes care flow sheets, available online (guidelines.diabetes.ca/docs/cpg/Appendix-3.pdf); a quick version focusing on ABCDES3 has also been produced (guidelines.diabetes.ca/docs/CPG-quick-reference-guide-web-EN.pdf#page=10), and providers might consider adapting this for use as a “stamp” (or form or template) in electronic medical records.
Key message 1: discuss opportunities to reduce the risk of diabetes complications.
The guideline states that treatments should be added (as tolerated) to achieve hemoglobin A1c (HbA1c), blood pressure, and cholesterol targets in accordance with patient preferences and goals. Since the last guideline update in 2013, the main change in this aspect of the guideline reflects new evidence that canagliflozin, empagliflozin, and liraglutide reduce the risk of cardiovascular events in patients who have a history of vascular disease.8 (Similar evidence for additional medications was not available at the time of guideline development.) The guideline states that evidence-based medications for vascular protection should be prescribed whenever appropriate:
statins in those aged 40 or older or with complications;
angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in those aged 55 or older or with complications; and
acetylsalicylic acid plus a sodium glucose transporter 2 inhibitor or glucagonlike peptide 1 receptor agonist with proven cardiovascular benefit (canagliflozin, empagliflozin, liraglutide) for those with vascular disease.
Diabetes Canada has created several interactive clinical decision support tools to help reduce some of the barriers to implementing these recommendations, including an interactive tool to consider pharmacotherapy options for glycemic control that compares the relative advantages or limitations of different agents (guidelines.diabetes.ca/bloodglucoselowering/pharmacologyt2), an interactive tool for selecting agents for vascular protection (guidelines.diabetes.ca/vascularprotection/riskassessment), and a prescription for cardiovascular protection (guidelines.diabetes.ca/docs/resources/prescription-for-cardiovascular-protection-with-diabetes.pdf). People with diabetes also require routine monitoring (and relevant action) for neuropathy, nephropathy, and retinopathy, which can be facilitated with a flow sheet (guidelines.diabetes.ca/docs/cpg/Appendix-3.pdf).8
Key message 2: discuss opportunities to ensure safety and prevent hypoglycemia.
The guideline states that targets for HbA1c levels and treatments should be individualized based on goals, preferences, and functional status, as described in Figure 2.8 Lower targets are appropriate when priority is placed on reducing the risk of microvascular outcomes and when the treatments used do not place the patient at risk of hypoglycemia. Higher targets are appropriate when reducing the risk of long-term complications is a lower priority. Diabetes Canada has an interactive tool to help tailor glycemic targets to optimize relevant outcomes while avoiding hypoglycemia (guidelines.diabetes.ca/bloodglucoselowering/a1ctarget).
Two new high-priority recommendations in the 2018 guidelines involve preventing hypoglycemia. First, all people with diabetes who take agents that can cause hypoglycemia (ie, insulin or insulin secretagogues) should be counseled on safe driving (ie, having sugar on-hand to prevent lows). A new chapter in the 2018 guidelines (guidelines.diabetes.ca/cpg/chapter21) describes how to assess and manage private and commercial drivers, especially those who take insulin or insulin secretagogues.8 Diabetes Canada has handouts to support conversations regarding safe driving, and the guidelines feature a sample diabetes and driving educational resource to fill out with people who have diabetes (guidelines.diabetes.ca/docs/patient-resources/drive-safe-with-diabetes.pdf). Second, the guidelines recommend that medications that pose less risk of hypoglycemia should be used preferentially, especially in the elderly (ie, metformin or dipeptidyl peptidase 4 inhibitors in preference to insulin or insulin secretagogues). Likewise, risks of hypotension should be considered when managing blood pressure. As noted in the previous guideline, recommendations emphasize the safe use of medications when people with diabetes are unwell and when they are at risk of hypovolemia. Euglycemic ketoacidosis is a particular risk with sodium glucose transporter 2 inhibitors, and these should be held on sick days (ie, when patients are at risk of dehydration).17 The Diabetes Canada guidelines have an appendix to support sick-day planning (guidelines.diabetes.ca/docs/cpg/Appendix-8.pdf) and an appendix for therapeutic considerations for renal impairment (guidelines.diabetes.ca/docs/cpg/Appendix-7.pdf).8 The website also features patient resources for primary care physicians to use with their patients for sick-day management (guidelines.diabetes.ca/docs/patient-resources/stay-safe-when-you-have-diabetes-and-sick-or-at-risk-of-dehydration.pdf), as well as for hypoglycemia identification, treatment, and prevention (guidelines.diabetes.ca/docs/patient-resources/hypoglycemialow-blood-sugar-in-adults.pdf).
Key message 3: discuss progress on self-management goals and address barriers.
People with diabetes should have an individualized plan for activity and nutrition. Intensive, group-based behavioural interventions can help patients to achieve their goals. Patients should be encouraged to seek nutrition counseling from a registered dietitian; in some regions dietitian consultations are available free of charge (eg, Ontario [www.unlockfood.ca/en/default.aspx], British Columbia [www.healthlinkbc.ca/dietitian-services], and Manitoba [www.wrha.mb.ca/prog/nutrition/files/204DADStickerEnglish.pdf]).
There is evidence that FPs can influence exercise levels.18 The guidelines recommend routinely setting specific exercise goals with each patient, problem solving to address potential barriers to physical activity, providing information on where and when to exercise, and encouraging self-monitoring (eg, pedometer or other tracking system) are recommended. Diabetes Canada has an interactive tool that can help FPs to provide specific exercise advice (guidelines.diabetes.ca/selfmanagementeducation/patool), as well as various instructional videos demonstrating resistance and core exercises (guidelines.diabetes.ca/patient-videos).
Supporting self-management also involves helping people address barriers to a healthy lifestyle including diabetes-related distress and comorbid conditions, such as depression or pain. Family physicians are particularly well positioned to identify the stressors experienced by patients and to support them in addressing their highest-priority needs. More frequent visits for people struggling to achieve their goals, ideally involving a structured team-based approach, can enable more effective implementation of self-management support.19 For those not practising in contexts with easy access to a multidisciplinary team, resources from Diabetes Canada have been developed to help implement these recommendations in practice (guidelines.diabetes.ca/reduce-complications/the-5rs), including handouts for people about self-management in general, featuring ABCDES3 for patients (guidelines.diabetes.ca/docs/patient-resources/my-diabetes-care-not-just-about-blood-sugar.pdf), plus handouts and practice tools that assist in identifying and managing sources of diabetes-related distress (guidelines.diabetes.ca/selfmanagementeducation/psychosocial).
Cross-cutting theme: tailor discussions based on the needs and preferences of each person.
Family physicians play a key role in managing care and supporting people with diabetes throughout the lifespan. The Diabetes Canada guideline features numerous recommendations that are specific to stages in the lifespan and the cultural contexts of people with diabetes. Specific chapters detail issues relevant to children, women of childbearing age, functionally dependent or frail elderly, as well as Indigenous peoples; we encourage providers to review the key messages and recommendations from these chapters. Diabetes Canada has handouts in French (guidelines.diabetes.ca/ressourcesfrancaises) and Chinese (guidelines.diabetes.ca/chinese), covering, for example, dietary options for people with a range of backgrounds, and additional cultural adaptations are forthcoming. Diabetes Canada also offers a toll-free number (1 800 BANTING), as well as a resource manual (guidelines.diabetes.ca/financial-support-and-services), to support patients with diabetes who have low income or other need to identify local resources and services that might be helpful.
Discussion.
Guidelines are meant to support clinical judgment not replace it. They should support shared decision making in practice. In that spirit, we present thematic groupings of guideline recommendations for adults with type 2 diabetes that we believe FPs will find important and useful. Specifically, the guidelines encourage 3 crucial conversations that FPs can have regularly with their patients to identify key considerations for comprehensive primary care across the lifespan. Family physicians might like to ask themselves and their patients with diabetes whether there are opportunities at each visit for the following:
add treatments that might reduce the risk of diabetes complications,
adjust treatment strategies to keep patients safe, and
support patients in self-management by addressing their sources of stress and helping them set goals and plan accordingly.
Diabetes management typically requires adaptation over time by both the patient and the health professional with iterative goal setting. As biopsychosocial circumstances change, the treatment recommendations will also need to change. In the context of shared decision making, where the needs and preferences of the patient are considered, FPs can periodically identify opportunities to optimize treatment so that the risk of long-term complications is minimized and to prevent immediate symptoms or side effects. The recommendations highlighted here offer guidance on how to achieve this. However, the evidence suggests that the best possible outcomes are achieved when FPs organize their diabetes care in a way that incorporates the patient-centred and evidence-based approaches of the chronic care model.
Limitations
This summary tries to organize information from the full guideline relevant for FPs, but we understand that each practice and each patient is unique. The recommendations prioritized for emphasis in this document might not match the needs of each practice, and the needs of each patient must be assessed through shared decision making. Many patients with type 2 diabetes might not have coverage for medications, and the newer agents might be prohibitively expensive for such patients. It is also plausible that emergent evidence based on real-world data will identify issues with the newer agents that lead to changes in the guideline recommendations. We further recognize that access to supports to implement best practices is not equitably distributed.20,21 For example, some patients have more ready access to allied health professionals than others. These factors (and others) undoubtedly affect diabetes care and outcomes. While many clinical activities are appropriate and advisable in the primary care of a patient with diabetes, the starting point for this summary was the text of the Diabetes Canada clinical practice guidelines. Many other guidelines related to the care of patients who have diabetes exist. The Diabetes Canada guidelines are aligned with the Canadian Cardiovascular Society guidelines for lipids16 and the Hypertension Canada guidelines for blood pressure targets.22 However, not all guidelines have the same recommendations, likely owing to variable weighting of the importance of different outcomes in the evidence base. For instance, recent guidelines from the American College of Physicians encourage higher HbA1c targets owing to the lack of evidence that lower targets are associated with reduced risk of cardiovascular outcomes.23 Additionally, simplified lipid guidelines for FPs de-emphasize targets for low-density lipoprotein to focus on use of evidence-based medications (eg, statins).24 Finally, it is important to note that this manuscript seeks only to summarize Diabetes Canada guideline recommendations deemed most relevant for the primary care management of adults with type 2 diabetes by a selected, albeit multidisciplinary, group; further information about prevention and management of all types of diabetes can be accessed at guidelines.diabetes.ca.
Conclusion
High-quality diabetes care involves a series of periodic conversations about self-management and about both pharmacologic and nonpharmacologic treatments that fit with each patient’s goals (ie, shared decision making). Incorporating these conversations into regular practice provides FPs with opportunities to maximize likely benefits of treatments and decrease the risk of harms, to support patients in initiating and sustaining desired lifestyle changes, and to help patients cope with the burdens of both diabetes and comorbid conditions. Family physicians can access the guideline at guidelines.diabetes.ca and might consider downloading the free smartphone app for quick access to guideline chapters and interactive tools at guidelines.diabetes.ca/app.
Editor’s key points
▸ Family physicians are faced with a range of options when selecting the most appropriate treatment approach for people with diabetes. The challenge is compounded by the vast amount of new evidence that is disseminated to both clinicians and to people with diabetes. Guidelines are meant to summarize this evidence, but it is not feasible for FPs to implement every single guideline recommendation relevant to primary care.
▸ In this review the authors aimed to summarize the Diabetes Canada 2018 guidelines and identify key messages and recommendations for FPs. From the 313 recommendations in the guidelines, they highlight the 22 they deemed the highest priority for primary care.
▸ Providing care that is concordant with the latest guidelines requires repeated discussions featuring shared decision making with people with diabetes about opportunities to reduce the risk of diabetes complications, keep patients safe, and support self-management.
Footnotes
Contributors
All authors participated in the process of prioritizing the recommendations and contributed to preparing the manuscript for submission.
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de janvier 2019 à la page e8.
References
- 1.Harris SB, Ekoé JM, Zdanowicz Y, Webster-Bogaert S. Glycemic control and morbidity in the Canadian primary care setting (results of the Diabetes in Canada Evaluation Study) Diabetes Res Clin Pract. 2005;70(1):90–7. doi: 10.1016/j.diabres.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 2.Canadian Institute for Health Information. International comparisons: a focus on diabetes. Ottawa, ON: Canadian Institute for Health Information; 2015. Available from: https://secure.cihi.ca/free_products/oecd-diabetes-report-2015_en.pdf. Accessed 2018 Jul 3. [Google Scholar]
- 3.Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Upshur REG, Tracy S. Chronicity and complexity. Is what’s good for the diseases always good for the patients? Can Fam Physician. 2008;54:1655–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Gagliardi AR, Alhabib S, Guidelines International Network Implementation Working Group. Trends in guideline implementation: a scoping systematic review. Implement Sci. 2015;10:54. doi: 10.1186/s13012-015-0247-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pathman DE, Konrad TR, Freed GL, Freeman VA, Koch GG. The awareness-to-adherence model of the steps to clinical guideline compliance. The case of pediatric vaccine recommendations. Med Care. 1996;34(9):873–89. doi: 10.1097/00005650-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Ke CH, Gall Casey C, Yu CH. Disseminating the Canadian Diabetes Association 2013 clinical practice guidelines: guidelines.diabetes.ca in action. Can J Diabetes. 2014;38(5):S72–3. [Google Scholar]
- 8.Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2018;42(Suppl 1):S1–325. [Google Scholar]
- 9.Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839–42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bennett WL, Odelola OA, Wilson LM, Bolen S, Selvaraj S, Robinson KA, et al. Evaluation of guideline recommendations on oral medications for type 2 diabetes mellitus: a systematic review. Ann Intern Med. 2012;156(1 Pt 1):27–36. doi: 10.7326/0003-4819-156-1-201201030-00005. [DOI] [PubMed] [Google Scholar]
- 11.Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3):124–30. Epub 2000 Jun 24. [Google Scholar]
- 12.Jeffery R, Iserman E, Haynes RB, CDSS Systematic Review Team Can computerized clinical decision support systems improve diabetes management? A systematic review and meta-analysis. Diabet Med. 2013;30(6):739–45. doi: 10.1111/dme.12087. Epub 2013 Feb 28. [DOI] [PubMed] [Google Scholar]
- 13.Murphy ME, Byrne M, Galvin R, Boland F, Fahey T, Smith SM. Improving risk factor management for patients with poorly controlled type 2 diabetes: a systematic review of health-care interventions in primary care and community settings. BMJ Open. 2017;7(8):e015135. doi: 10.1136/bmjopen-2016-015135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tricco AC, Antony J, Ivers NM, Ashoor HM, Khan PA, Blondal E, et al. Effectiveness of quality improvement strategies for coordination of care to reduce use of health care services: a systematic review and meta-analysis. CMAJ. 2014;186(15):E568–78. doi: 10.1503/cmaj.140289. Epub 2014 Sep 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grudniewicz A, Kealy R, Rodseth RN, Hamid J, Rudoler D, Straus SE. What is the effectiveness of printed educational materials on primary care physician knowledge, behaviour, and patient outcomes: a systematic review and meta-analyses. Implement Sci. 2015;10:164. doi: 10.1186/s13012-015-0347-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson TJ, Grégoire J, Pearson GJ, Barry AR, Couture P, Dawes M, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32(11):1263–82. doi: 10.1016/j.cjca.2016.07.510. [DOI] [PubMed] [Google Scholar]
- 17.Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care. 2015;38(9):1638–42. doi: 10.2337/dc15-1380. [DOI] [PubMed] [Google Scholar]
- 18.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9(5):426–33. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- 19.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Clement M, Harvey B, Rabi DM, Roscoe RS, Sherifali D. Organization of diabetes care. Can J Diabetes. 2013;37(Suppl 1):S20–5. doi: 10.1016/j.jcjd.2013.01.014. Epub 2013 Mar 26. [DOI] [PubMed] [Google Scholar]
- 20.Glazier RH, Agha MM, Moineddin R, Sibley LM. Universal health insurance and equity in primary care and specialist office visits: a population-based study. Ann Fam Med. 2009;7(5):396–405. doi: 10.1370/afm.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glazier RH, Hutchison B, Kopp A, Dobell G. Primary care practice reports: administrative data profiles for identifying and prioritizing areas for quality improvement. Healthc Q. 2015;18(1):7–10. doi: 10.12927/hcq.2015.24251. [DOI] [PubMed] [Google Scholar]
- 22.Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34(5):506–25. doi: 10.1016/j.cjca.2018.02.022. [DOI] [PubMed] [Google Scholar]
- 23.Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA, et al. Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians. Ann Intern Med. 2018;168(8):569–76. doi: 10.7326/M17-0939. [DOI] [PubMed] [Google Scholar]
- 24.Allan GM, Lindblad AJ, Comeau A, Coppola J, Hudson B, Mannarino M, et al. Simplified lipid guidelines. Prevention and management of cardiovascular disease in primary care. Can Fam Physician. 2015;61:857–67. (Eng), e439–50 (Fr). [PMC free article] [PubMed] [Google Scholar]