Abstract
Social anxiety disorder (SAD) tends to emerge during the early teenage years and is particularly refractory to change even when standard evidence-based CBT treatments are delivered. Efforts have been made to develop novel, mechanistic-driven interventions for this disorder. In the present study, we examined Attention Bias Modification Treatment (ABMT) for youth with SAD. Participants were 58 adolescents (mean age = 14.29 years) who met diagnostic criteria for SAD and who were randomized to ABMT or a placebo control condition, Attention Control Training (ACT). We predicted that ABMT would result in greater changes in both threat biases and social anxiety symptoms. We also explored potential moderators of change including the severity of social anxiety symptoms, the level of threat bias at pre-treatment, and the degree of temperament-defined attention control. Contrary to our hypotheses, changes in attention bias were not observed in either condition, changes in social anxiety symptoms and diagnosis were small, and significant differences were not observed between the ABMT and ACT conditions. Little support for the proposed moderators was obtained. Reasons for our failure to find support for ABMT and its potential moderators are explored and recommendations for changes in the ABMT paradigm are suggested.
Keywords: social anxiety disorder, attention bias modification training, dot probe, adolescents
In recent years the efficacy of cognitive-behavioral therapy (CBT) for the treatment of anxiety disorders in youth has been well established (see Higa-McMillan, Francis, Rith-Najarian, & Chorpita, 2016 and James, James, Cowdrey, Soler & Choke 2013 for reviews). For the most part, this evidence has been obtained from “standard” CBT interventions that typically consist of 10–16 weekly sessions delivered on an outpatient basis in either individual or group format. Although effective for a majority of youth, between 25% and 40% do not remit and are not diagnosis free following standard CBT treatment (Higa-McMillan et al., 2016; James et al., 2013). Moreover, it has been shown that over half of those who are diagnosis free following this treatment approach are no longer diagnosis free at long-term follow up (Ginsburg et al., 2014). Furthermore, these remission rates are considerably lower for youth with social anxiety disorder (SAD) than youth with other anxiety disorders as documented in major clinical trials in the United States and Australia (Ginsburg et al., 2011, 2014; Hudson et al., 2015; Walkup et al., 2008).
SAD consists of a marked and persistent fear of social or performance situations in which embarrassment or humiliation might occur and its average age of onset in early to mid-adolescence (American Psychiatric Association, 2013). Indeed, it is the most common anxiety disorder seen in adolescence and adulthood and ranks third in lifetime prevalence among all psychiatric disorders, following only major depressive disorder and alcohol dependence (APA, 2013). It is estimated that the prevalence of SAD during adolescence is between 10 and 15% in the United States (Merikangas et al., 2010) and Europe (Essau, Conradt, & Petermann, 1999). Findings suggest that SAD follows a chronic, unremitting course in the absence of effective treatment (Ginsburg et al., 2014; Ollendick, Benoit, & Grills-Taquechel, 2014).
In partial response to the prevalence of SAD and its long-term prognosis, recent trends have witnessed the development of novel interventions as supplements to “standard” CBT treatments or as standalone treatments (see Öst & Ollendick, 2017). One such treatment is Attention Bias Modification Treatment (ABMT), a computer-based treatment which has its origins in the seminal work of MacLeod, Mathews, and Tata (1986), who showed an attentional bias toward threat in individuals with an anxiety disorder. This bias has been affirmed in systematic qualitative reviews and meta-analyses with adults (MacLeod & Clarke, 2015) and youth (Dudeney, Sharpe, & Hunt, 2015; Field & Lester, 2010; Puliafico & Kendall, 2006). However, it should be noted that these reviews indicate that biases are not present in all anxiety disordered individuals. Indeed, up to 50% of anxious children and adolescents do not show a bias toward threat. Attempts to determine which youth show the bias and which ones do not have been largely unsuccessful (see Eldar et al., 2012), although some promising findings have been reported. First, in their meta-analysis of youth with anxiety disorders, Dudeney and colleagues (2015) concluded that this bias was greater in adolescents than in children (although some exceptions exist, see Carmona et al., 2015). Second, Roy et al. (2008) and Waters, Mogg, Bradley and Pine (2011) have shown this threat bias tends to exist primarily in youth with higher levels of anxiety symptoms. Thus, both age of the participants and their level of anxiety severity may be important in determining which anxious youth are likely to display threat-related attentional bias.
ABMT protocols use the dot-probe task developed by MacLeod et al. (1986) to both assess the threat bias and then to treat the bias by systematically redirecting attention away from the threat stimuli. Threat (i.e., anger, disgust) and neutral stimuli are presented simultaneously (either verbally or pictorially), withdrawn, and then a probe is presented in the location of where either the neutral or threat stimulus was located. During assessment, the probe is presented equally often in the location of the neutral and threat stimulus. Bias is indicated by a faster reaction time to probes in the location of the threat stimulus relative to probes following the neutral stimulus. In treatment, neutral and threat stimuli once again appear simultaneously but the probe is presented at the location of the neutral stimulus in 80 to 100% of the trials. This systematic pairing of the probe with the neutral stimulus is thought to create a contingency between the neutral stimulus and the target location facilitating change in attentional processes away from threat (see Bar-Haim, 2010).
Several randomized controlled trials (RCTs) comparing ABMT to active control conditions, most often Attention Control Training(ACT) as a placebo, have been conducted with adults with SAD as well as other anxiety disorders. Meta-analyses have largely shown small-to-medium effects on changes in both attention bias and anxiety symptom measures in these studies (Hakamata et al., 2010; Linetzky, Pergamin-Hight, Pine, & Bar-Haim, 2015; Mogoaşe, David, & Koster, 2014; Schmidt, Richey, Buckner, & Timpano, 2009). In children and adolescents, the results have been more mixed with one recent meta-analysis of 23 RCTs indicating that although small to medium effects were demonstrated for changes in threat biases, small and nonsignificant effects were observed for changes in self-report, parent-report, and clinician-report of anxiety (Cristea, Mogoaşe, David, & Cuijpers, 2015). These authors also reaffirmed that not all youth with an anxiety disorder in these studies demonstrated the threat bias, that age-related differences in attentional biases exist, and that much of the inconsistency in findings might be related to the common practice of lumping youth with different anxiety disorders together (e.g., not only SAD, but also generalized anxiety disorder, separation anxiety disorder, specific phobia, and panic disorder) in the same clinical trials. Recently, Pergamin-Hight and colleagues (2015) demonstrated the content specificity of attentional biases and distorted beliefs associated with the various anxiety disorders, suggesting that it might be important for the threat stimuli used in these studies to be tailored to the specific disorders under study. In the usual dot-probe paradigm, the facial stimuli which depict anger and disgust might be more salient to SAD (Abend et al., 2018) and less so, for example, to specific phobia or separation anxiety disorder, thus potentially masking the effects of the potential bias in these studies.
In a recent study with youth diagnosed with SAD as their primary anxiety disorder, Pergamin-Hight, Pine, Fox, and Bar-Haim (2016) explored the efficacy of ABMT against ACT. They also examined several possible moderators of treatment outcome (i.e., age of the participant, baseline threat-related attentional biases, and attention control as measured by the Attention subscale of the Early Adolescent Temperament Questionnaire – Revised; EATQ-R; Ellis & Rothbart, 2001; Putnam, Ellis, & Rothbart, 2001). Adolescents were randomly assigned to ABMT and ACT conditions. Youth in both conditions received 8 training sessions delivered twice a week over four weeks. Unexpectedly, both conditions resulted in significant reductions in threat biases, as well as reductions in clinician-rated and self-reported anxiety. Age was found to moderate the social anxiety outcomes with older youth showing a greater response to ABMT than ACT on self-reported but not clinician-rated anxiety – affirming age-related findings as suggested by Dudeney et al. (2015) and Cristea et al. (2015). Significant moderating effects of attention control were also found such that youth whose parents reported them as being lower in the ability to shift and control attention benefitted more from ABMT than did youth whose parents rated them as higher in attention control. However, baseline attentional bias scores were not found to moderate treatment outcomes associated with either self-report or clinician-rated anxiety.
Given these mixed findings, we set about comparing ABMT to ACT in this RCT with the aim of addressing the specific shortcomings identified in the earlier trials. First, we enrolled only adolescents between 12 and 16 years of age who were reliably diagnosed with SAD via a semi-structured diagnostic interview. Second, we used a set of pictorial stimuli expressing angry or neutral adolescent faces since these expressions may be particularly salient to SAD in adolescence (see Coffman et al., 2015, and Wieckowski et al., 2016). This is novel as other ABMT studies have used adult face stimuli. Third, we delivered both conditions twice a week over a 5-week period for a total of 10 sessions in an attempt to provide sufficient trials to more firmly create the contingency between the neutral stimuli and the target location to facilitate change in attentional processes away from threat (as recommended by Bar-Haim, 2010). Fourth, we explored moderators of change on measures of both self-report and clinician-rated social anxiety as recommended by Pergamin-Hight et al. (2016). Fifth, preliminarily, we endeavored to determine if changes in threat appraisal mediated changes in social anxiety, as suggested by the underlying assumptions of ABMT.
Specific hypotheses were as follows: 1) ABMT would produce greater reductions in threat biases than ACT; 2) ABMT would produce greater reductions in self-report, parent-report, and clinician-report social anxiety symptoms relative to ACT; and 3) again, preliminarily, changes in attentional biases would mediate changes in social anxiety symptoms. In addition, we conducted exploratory analyses related to the potential moderating roles of baseline threat related attentional bias, social anxiety severity, and attention control.
Method
Participants
Participants were male and female adolescents between 12 and 16 years of age who met diagnostic criteria for SAD (see below). Adolescents were recruited through referrals from child psychiatric services, local mental health clinics, school health services, primary care practices, and community advertisements. Recruitment occurred over a 3-year period (2014 – 2016). Prior to enrollment, parents completed a brief telephone screen to determine the potential fit of their daughter or son for the study. If the telephone screen suggested potential fit, the adolescents and their parents were invited to complete pretreatment measures at our university affiliated clinic. Prior to completing any measures, all adolescents provided informed written assent while their parents/caregivers provided parental permission for their son or daughter to participate.
Seventy-five adolescents were referred to the study and completed the initial eligibility assessment at the university clinic. Inclusion criteria for participation consisted of: 1) individuals 12–16 years of age, 2) a clinical diagnosis of SAD as determined by a semi-structured diagnostic interview, 3) full scale IQ of 80 or above, 4) stable psychotropic medication as determined by no dosage changes for at least four weeks, and 5) no ongoing psychosocial intervention for social anxiety-related concerns. Participants were excluded from the trial if they met criteria for autism spectrum disorder, childhood schizophrenia, and/or psychopathology that warranted more immediate clinical care such as suicidal ideation.
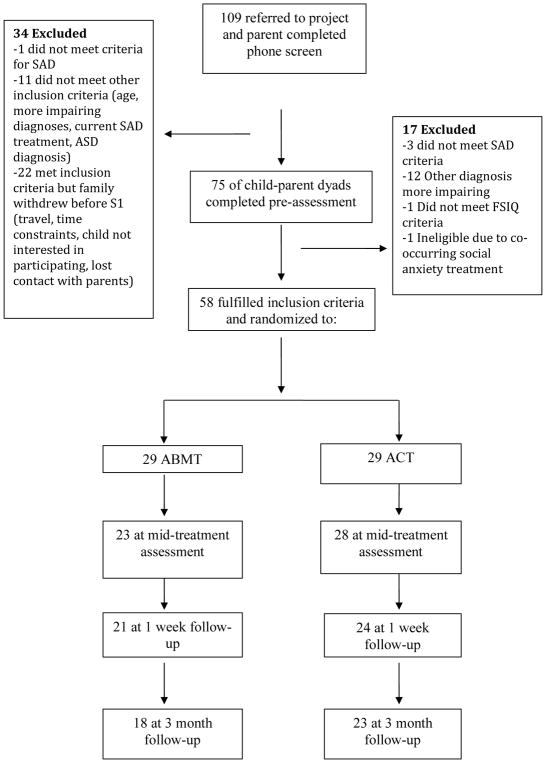
Fifty-eight adolescents were advanced to the clinical trial (see Figure 1 for CONSORT Flow Chart). Although all participants met criteria for SAD, comorbidity with other anxiety disorders was common: 65.5% also met criteria for generalized anxiety disorder, 44.8% for a specific phobia, and 5.2% for separation anxiety disorder. Other non-anxiety diagnoses were present but in more limited numbers (< 10%). SAD was the primary diagnosis for 62% of participants; however, SAD was the reason for referral in all instances.
Figure 1.
Consort Flow Chart
Descriptive statistics for demographic variables of the participants are presented in Table 1. Adolescents were primarily female (70.7%) and averaged 14.29 years of age (range = 12–16, SD = 1.30). The racial breakdown was primarily White (84.5%), followed by Black/African-American, Hispanic/Latino, and Asian. Mean gross family income was relatively high, averaging $93,804 (range = $23,000–$285,000, SD = $54,037.51). Two adolescents were prescribed anti-anxiety medication (both selective serotonin reuptake inhibitors) while they were enrolled in the study; however, per our inclusion criteria the dosage had not been changed for at least four weeks preceding their first appointment or was not changed during the clinical trial.
Table 1.
Sample Characteristics
| Variable | ACT (n= 29) | ABMT (n = 29) | Total Sample (n = 58) | T-test or Chi-square comparing treatment conditions |
|---|---|---|---|---|
| Mean age | 14.24 | 14.34 | 14.29 | t(56) = .301, p = .764 |
| % Female | 72.4% | 69% | 70.7% | x2(1) = 0.083, p = .500 |
| % Caucasian | 89.7% | 79.3% | 84.5% | x2(1) = 0.277, p = .470 |
| Mean Family Income | $91,416 | $96,192 | $93,804 | t(50) = .316, p = .753 |
| Family Income (%) | ||||
| Less than $25,000 | 0 | 3.85% | 1.96% | |
| $25,000 to $49,999 | 12% | 19.23% | 15.69% | |
| $50,000 to $99,999 | 44% | 30.77% | 37.25% | |
| $100,000 or more | 44% | 46.15% | 54.10% | |
Measures
Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions (ADIS-IV-C/P; Silverman & Albano, 1996)
The ADIS-IV-C/P is a semi-structured interview designed to assess anxiety and related disorders in childhood and adolescence. Trained and research-reliable clinicians, supervised by a licensed clinical psychologist, assigned a severity rating (CSR) on a 9-point scale (0–8, with any rating ≥ 4 indicating diagnostic presence) on both the child and parent interviews. Psychometric properties of the ADIS-C/P are good (Silverman, Saavedra & Pina, 2001). For purposes of this study, separate clinicians administered the ADIS-C and ADIS-P. Final diagnoses were derived based on composite rules recommended by Silverman and Albano such that the higher CSR of the adolescent or parent was used to determine diagnosis and for subsequent analyses. The ADIS-IV-C/P was administered at the pre-treatment, post-treatment, and follow-up assessment sessions.
Training on the ADIS-IV-C/P consisted of a workshop, practice interviews, and observation of administration conducted by a reliable clinician. The administrations were videotaped and approximately 30% (n = 17) of the diagnostic interviews were reviewed by a second clinician. Inter-rater agreement on the CSR score was high; across the child and parent interviews, agreement (i.e., CSR within one point of each other) was 94% and 100%, respectively.
Screen for Child Anxiety Related Disorders, Child and Parent Version (SCARED; Birmaher et al., 1997)
The SCARED is a self-report and parent-report measure used to assess various facets of anxiety in youth. The SCARED consists of 41-items and yields scores for Panic Disorder, Generalized Anxiety, Separation Anxiety, Social Anxiety, and School Avoidance, in addition to a Total Score. The test-retest reliability, internal consistency, and discriminant validity are well-established (Birmaher et al., 1997). Additionally, the SCARED has been used as a measure of treatment outcome (Birmaher et al., 1997). In the current sample, internal consistency was good for both parent-report of the Social Anxiety subscale (α = 0.81) and adolescent-report (α = 0.83). The self-report and parent-report SCARED was administered at pre-treatment, midpoint, post-treatment, and follow-up assessment sessions.
Early Adolescent Temperament Questionnaire-Revised Short Form (EATQ-R; (EATQ-R; Ellis & Rothbart, 2001; Putnam, Ellis, & Rothbart, 2001)
EATQ-R measure targets common experiences for adolescents and assesses temperament and self-regulation. Both adolescents and parents completed this questionnaire by rating a list of statements on a 5-point scale (1= Almost always untrue to 5= Almost always true). We used the Attention Control subscale (6 items) that assesses the capacity to focus attention as well as the ability to shift attention when desired. In the current sample, internal consistency was acceptable for both parent-report of the Attention Control subscale (α = 0.79) and adolescent-report (α = 0.71). The self-report and parent-report EATQ-R were administered at pre-treatment, midpoint, post-treatment, and follow-up assessment sessions.
Dot Probe Task
All participants completed a dot probe task at the pre-treatment, mid-treatment, post-treatment, and follow-up sessions in order to assess changes in attentional threat bias. In probe detection tasks, stimulus durations for both faces and probes have varied considerably across studies. Within the adult-focused literature, a vigilance effect for negative faces has been consistently found for shorter durations (175ms–200ms; Pishyar, Harris, Menzies, 2008), with somewhat more mixed results as presentation times approach 500ms to 600ms (Bradley et al., 1997; Mogg, Phillippot, & Bradley, 2004; Stevens, Rist, & Gerlach, 2010; Vassilopoulos, 2005), and virtually no effects at longer durations (1000–1250ms; Mogg, Bradley, Miles, & Dixon, 2004; Mogg et al., 2004). This gradient also generally mirrors patterns observed in community samples (Cooper & Langston, 2006). Thus, the likelihood of measuring attentional bias appears to depend heavily on timing, with somewhat stronger evidence for briefer as compared to longer stimulus durations (c.f. Bantin, Stevens, Gerlach, & Hermann, 2016).
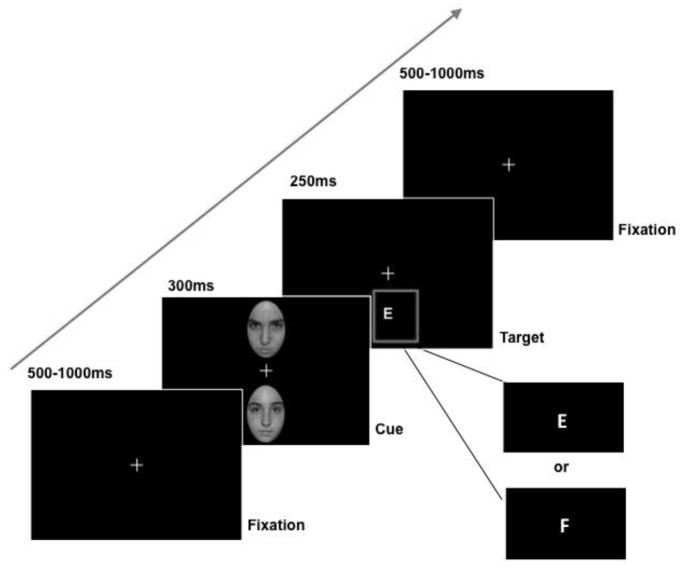
Each trial of the dot probe task started with viewing a central fixation cross, with an inter-trial interval of 500–1000ms. Next, participants viewed a pair of adolescent facial images from the NIMH-CheFS adolescent stimulus set (Egger et al., 2011), which were adapted for purposes of the present project (Coffman et al., 2015). The faces were positioned above and below the former location of the central fixation. Facial images remained on the screen for 300ms. Images were either neutral or angry adolescent faces. Adolescents were instructed to watch the screen, look for a letter ‘E’ or ‘F’, and press the left or right mouse button, which corresponded to the letter ‘E’ and ‘F’ respectively, as quickly and accurately as possible. Consistent with previous studies, a letter replaced the neutral face in 50% of the trials and remained on the screen for 250ms. Each dot probe task consisted of 160 trials, which lasted approximately 12 minutes. For the 160 trials, 32 trials included pairs of neutral faces, and 128 trials included one neutral face and one angry face.
Procedure
Assessment Sessions
Adolescents and their parents completed 5 separate assessment sessions throughout the study. The first two sessions were pre-treatment assessments, with each lasting approximately 2 and ½ hours. During the first pre-treatment assessment, both child and parent participants consented to the study’s procedures. Participants were informed about the study design and the randomization process which would assign individuals to either an experimental computer-based treatment (ABMT) or a control condition (ACT). Pretreatment assessments consisted of the adolescent completing the ADIS-C, dot-probe task, and self-report questionnaires, in addition to several other experimental tasks and questionnaires not examined in this study. Trained graduate-level clinicians served as the assessment evaluators. During the pre-treatment assessments, one clinician administered the adolescent battery, while a second clinician obtained information from the parent. The adolescent’s parent completed the ADIS-IV-P and several questionnaires regarding their daughter or son. After the second session, eligibility was determined, and the adolescent was randomized to one of the two conditions, ABMT or ACT. The assessment clinicians were privy to the study’s aims, yet they remained blind to the participant’s treatment condition after randomization. The randomization was completed by research staff not directly involved in assessment or treatment sessions. The third assessment, the midpoint session, took approximately one hour to complete, and occurred after the 5th treatment session, midway between the 10 sessions. The midpoint assessment consisted of the adolescent completing the dot probe task and several self-report questionnaire measures while their parent completed several questionnaires regarding their child, including the SCARED and the EATQ-R. The endpoint assessment occurred approximately one week following treatment, and the follow-up assessment was scheduled for approximately 3 months thereafter. Both the endpoint and follow-up sessions took approximately two hours to complete and consisted of adolescents and their parents completing the majority of the same measures completed at pre-treatment, including the dot-probe and ADIS-IV modules that were clinically significant at pre-treatment. At the end of the 3-month follow-up session, participants and their parents were informed of which condition they were randomized to and were provided further resources for treatment if desired/needed. Participants were unblinded by a member of the research team who was not involved in treatment administration.
Treatment Sessions
The ABMT consisted of a modified dot probe task, adapted from Schmidt and colleagues (2009) for adult participants. Our ABMT task was modified to include adolescent faces from the same stimulus set as those used in the dot probe. Each participant was randomly assigned a graduate clinician who administered the computerized intervention (described below). Assessment evaluators and treatment clinicians remained distinct for all participants. Both the participant and the clinician were blind to the participant’s treatment status(i.e., ABMT or ACT). Participants completed the treatment sessions twice a week, for five weeks (total of 10 sessions). Before each session participants and their parents completed a questionnaire about the adolescent’s anxiety. Each treatment session took approximately 30 minutes.
During the computerized interventions, each trial started with viewing a central fixation cross, which was presented for 500–1000ms. Next, participants viewed a pair of adolescent facial images, which were oriented above and below the former location of the central fixation. Images remained on the screen for 300ms. Images were either neutral or angry adolescent faces. In the ABMT condition, a letter replaced the neutral face in 100% of the trials, and in the ACT condition the letter replaced the neutral face in 50% of the trials. The instructions for the task were the same as described above for the dot probe task. Each condition consisted of 160 trials, which lasted approximately 12 minutes. For the 160 trials, 32 trials included pairs of neutral faces, and 128 trials included one neutral face and one angry face. A visual schematic of a sample ABMT trial is depicted in Figure 2.
Figure 2.
Example of an ABMT trial where attention is directed towards the neutral face (bottom) rather than the angry face (top).
Subsequent to the training, the clinician engaged the adolescent in casual conversation for about 5 minutes to foster ongoing rapport. Clinicians were instructed to discuss neutral topics (e.g., school, hobbies), to not ask about specific social challenges, to not engage in any CBT techniques, and to not provide any general advice on how to deal with their social anxiety. These conversations were videotaped. Two independent reviewers (trained graduate clinicians) reviewed the tapes. To ensure protocol adherence, all videos of the training sessions were reviewed and coded for neutrality of conversation content as well as presence of any CBT elements. The neutrality of conversation content scale examined the extent to which the participant’s social or performance concerns were discussed during the session. For the presence of CBT elements scale, potential components consisted of therapeutic strategies such as psychoeducation, cognitive challenging, and introduction of coping skills. Both categories were evaluated on a 1 – 5 point Likert scale developed by the study’s research team, in which the highest value (5) was optimal for each scale. For example, “social anxiety or performance topics were not raised by the adolescent or initiated by the clinician” and “the clinician employed no elements of CBT” were the highest values for the neutrality of content scale and absence of CBT components scale, respectively.
In order to test for inter-rater reliability, a randomly selected subsample of videos (21.6%, n = 108) was coded by two reviewers independently. For the absence of CBT components scale, no conversation was coded as consisting of any of the related therapeutic strategies. Thus, the intraclass correlation coefficient was not calculated for this scale. We found high agreement between raters for the neutrality of content scale (single ICC = 0.93).
Data Analyses
Data were analyzed with IBM SPSS Statistics Version 23. Missing values at both the post-treatment and 3-month follow-up assessments were imputed using the multiple imputation procedure in SPSS (IBM Corp.). As suggested by Enders (2016), it is questionable practice to drop those participants with missing data (possibly biasing the results in favor of those who completed the trial and lowering power for analyses). Enders has shown that multiple imputation estimations provide reliable results and work especially well for testing interactions between categorical and continuous variables as we do in this study. There were no significant differences between the two conditions in percentage of missing data at the post-treatment, χ2 (1, n = 58) = 0.89, p = .345, or three month follow-up assessments, χ2 (1, n = 58) = 0.70, p = .401. Adolescent sex was included in all hierarchical regression analyses and Analyses of Covariance (ANCOVAs) as a covariate due to the sample being predominantly, but not entirely, female. Additionally, independent samples t-tests indicated significant differences between males and females on ADIS CSRs and self-reported social anxiety on the SCARED. The pre-treatment score for the outcome variable being assessed in each regression analysis was also included as a covariate. Repeated Measures ANOVAs were used to assess change in attentional biases and social anxiety severity across assessment sessions. Adolescent sex (0 = Male, 1 = Female) and treatment condition (0 = ABMT; 1 = ACT) were included as dichotomous variables, while all other variables were continuous. Significant moderation effects were explored at three levels of the moderator variable: one standard deviation below the mean, mean, and one standard deviation above the mean. As noted above, social anxiety ADIS CSRs used in the analyses were the composite CSRs at each assessment session. SCARED social anxiety scores were analyzed separately for adolescent and parent report.
Results
Descriptive Analyses
See Table 2 for means and standard deviations of study variables. The ABCT and ACT groups did not differ from one another at pre-treatment assessment. See Table 2 for test statistics and p-values. Differences at post-treatment and follow-up are commented upon below.
Table 2.
Descriptive Statistics for Study Variables across Treatment Condition and Time
| Variable/Timepoint | ACT (n = 29) | ABMT (n = 29) | |||
|---|---|---|---|---|---|
|
| |||||
| Range | M(SD) | Range | M(SD) | t-value | |
| SAD Clinical Severity (ADIS-C/P) | |||||
| Pre-treatment | 4–7 | 5.52(0.79) | 4–7 | 5.41(0.98) | −0.44† |
| Post-treatment | 2–6 | 4.83(0.97) | 2–6 | 4.77(0.94) | |
| 3-month Follow-up | 1–6 | 4.55(1.12) | 1–7 | 4.75(1.14) | |
| SCARED SAD Adolescent Rating | |||||
| Pre-treatment | 3–14 | 10.76(3.25) | 0–14 | 9.07(3.87) | −1.80† |
| Post-treatment | 0–14 | 7.88(3.65) | 1–14 | 8.17(3.10) | |
| 3-month Follow-up | 0–14 | 8.08(3.79) | 1–13 | 7.10(2.90) | |
| SCARED SAD Parent Rating | |||||
| Pre-treatment | 3–14 | 10.90(3.20) | 5–14 | 11.76(2.63) | 1.12† |
| Post-treatment | 2–14 | 9.64(2.82) | 3–14 | 10.24(2.54) | |
| 3-month Follow-up | 2–14 | 8.11(3.11) | 4–14 | 9.47(2.69) | |
| Dot Probe Threat Bias Score | |||||
| Pre-treatment | −.46–.35 | −0.032(0.210) | −.44–.35 | −0.021(0.210) | 0.20† |
| Post-treatment | −.28–.30 | 0.019(0.149) | −.32–.31 | 0.018(0.175) | |
| 3-month Follow-up | −.48–.43 | −0.023(0.252) | −.37–.32 | 0.022(0.184) | |
| EATQ-R Attention Control Adolescent Rating | |||||
| Pre-Treatment | 1.67–4.83 | 3.24(0.79) | 1.83–4.67 | 3.26(0.66) | 0.15† |
| EATQ-R Attention Control Parent Rating | |||||
| Pre-Treatment | 1.67–4.33 | 3.01(0.74) | 1.33–5.00 | 3.16(0.88) | 0.70† |
Note.
p > .05
Hypothesis 1: ABMT would produce greater reductions in threat biases relative to the placebo
A repeated measures ANCOVA assessing change in threat biases across time indicated that neither the time effect, F(3, 53) = 0.88, p = .460, η2 = .05, nor the time by treatment condition interaction effect, F(3, 53) = 1.16, p = .333, η2 = .06, were significant.
Hypothesis 2: ABMT would produce greater reductions in self-report, parent-report, and clinician-report social anxiety symptoms relative to the placebo
Using repeated measures ANCOVAs, for ADIS CSRs, the time effect, F(2, 54) = 1.52, p = .229, η2 = .05, and the time by treatment condition interaction was not significant, F(2, 54) = 0.52, p = .60, η2 = .02. For SCARED social anxiety scores based on parent report, the time effect was significant, F(3, 53) = 3.49, p = .022, η2 = .17, but the time by treatment condition interaction was not, F(3, 53) = 0.54, p =.655, η2 = .03. When SCARED social anxiety scores based on the child report are considered, the time effect was not significant, F(3, 53) = 1.83, p = .154, η2 = .09, while the time by treatment condition interaction was significant, F(3, 53) = 3.31, p =.027, η2 = .16. Specifically, while on average SCARED scores for participants in the ACT condition gradually reduced from pre-treatment to post-treatment and then remained consistent at 3-month follow-up, SCARED scores for participants in the ABMT condition continued to decrease linearly from pre-treatment to post-treatment to the 3-month follow-up assessment.
Hypothesis 3: Changes in attentional biases would mediate changes in social anxiety symptoms
Because we did not find significant changes in threat biases across time (Hypothesis 1), we did not test whether changes in attentional biases mediated changes in social anxiety symptoms.
Exploratory Moderation Analyses
Baseline threat related attentional bias
Baseline threat bias scores did not significantly moderate the relationship between treatment condition and ADIS CSRs at post treatment, ΔR2= .01, F(1, 52) = 0.54, p = .468, or 3-month follow-up, ΔR2= .00, F(1, 52) = 0.02, p = .902. Results were consistent for SCARED social anxiety scores based on both parent and child report. Baseline threat bias scores did not significantly moderate the relationship between treatment condition and post-treatment SCARED scores per parent, ΔR2= .00, F(1, 52) = 0.12, p = .732, or child report, ΔR2= .00, F(1, 52) = 0.09, p = .767 for child, or between treatment condition and 3-month follow-up SCARED scores per parent, ΔR2= .00, F(1, 52) = 0.11, p = .747, or child report, ΔR2= .00, F(1, 52) = 0.02, p = .897.
Baseline Social anxiety severity
Severity of social anxiety symptoms did not significantly moderate the relationship between treatment condition and ADIS CSRs at post-treatment, ΔR2= .02, F(1, 53) = 1.06, p = .308, or 3-month follow-up, ΔR2= .02, F(1, 53) = 1.36, p = .249. Likewise, severity of social anxiety symptoms, as measured by parent reported SCARED, did not significantly moderate the relationship between treatment condition and SCARED scores at post-treatment, ΔR2= .04, F(1, 53) = 2.56, p = .115, or 3-month follow-up, ΔR2= .02, F(1, 53) = 1.47, p = .231, and severity of social anxiety symptoms, as measured by child reported SCARED, did not significantly moderate the relationship between treatment condition and SCARED scores at post-treatment, ΔR2= .05, F(1, 53) = 3.77, p = .057. However, severity of social anxiety symptoms as measured by adolescent reported SCARED did significantly moderate the relationship between treatment condition and SCARED scores at 3-month follow-up, ΔR2= .11, F(1, 53) = 9.79, p = .002.
Specifically, adolescents whose self-reported SCARED social anxiety scores were one SD below the sample’s mean at the pre-treatment assessment showed significantly lower SCARED scores at 3-month follow-up if they received ABMT than if they received the ACT condition (B= −2.26, SE = 1.10, p = .046). No significant differences between treatment conditions were found at mean levels of pre-treatment social anxiety (B= −0.20, SE = 0.75, p = .791). However, at high levels of pre-treatment social anxiety scores (e.g., one SD above the mean), adolescents’ 3-month follow-up SCARED scores were higher if they received the ABMT condition (B = 2.66, SE = 1.07, p = .016).
Baseline Attention control
Pre-treatment attention control, as reported by the parent on the EATQ-R, did not significantly moderate the relationship between treatment condition and ADIS CSRs at post-treatment, ΔR2= .00, F(1, 52) = 0.03, p = .864, or 3-month follow-up, ΔR2= .06, F(1, 52) = 3.82, p = .056, When adolescent self-reported attention on the EATQ-R was considered, attention did not significantly moderate the relationship between treatment condition and ADIS CSRs at post-treatment, ΔR2= .01, F(1, 52) = 0.39, p = .534, or 3-month follow-up, ΔR2= .00, F(1, 53) = 0.08, p = .782.
Pre-treatment attention control, as reported by the parent on the EATQ-R, did significantly moderate the relationship between treatment condition and parent-rated SCARED social anxiety at post-treatment, ΔR2= .12, F(1, 52) = 8.10, p = .006, but not at 3-month follow-up, ΔR2= .00, F(1, 52) = 0.17, p = .682. Specifically, adolescents whose pre-treatment attention control scores were high (i.e., one SD above the sample’s mean) had significantly lower SCARED social anxiety at post-treatment if they received the ABMT condition than if they received the control condition (B= −2.30, SE = 0.94, p = .018). No significant differences between treatment conditions were found at mean (B= −0.40, SE = 0.66, p = .545) and low (B= 1.50, SE = 0.93, p = .115) levels of attention.
Discussion
Although ABMT has shown considerable promise in the treatment of anxious adults, findings for adolescents show less promise (Cristea et al., 2015; Dudeney et al., 2015). Given that SAD often onsets during early adolescence (APA, 2013; Ollendick et al., 2014), that the vast majority of teens with SAD either do not receive evidence-based treatments or do not respond to these treatments (Ginsburg et al., 2011, 2014; Higa-McMillan et al., 2016), and that many adolescents indicate preference for technology-driven interventions such as ABMT over traditional clinic-based therapy (Spence, Donovan, March, Kenardy, & Hearn, 2017), it is crucial that alternative treatments are developed and rigorously evaluated. The primary focus of this RCT was to compare one such technology-based treatment, ABMT, to an attention placebo control condition, ACT, in the treatment of SAD in adolescents. In doing so, we attempted to address several of the shortcomings noted in previous studies by enrolling only adolescents who had a confirmed diagnosis of SAD, using pictorial stimuli designed specifically for adolescents expressing SAD–relevant angry faces, and providing 10 sessions of treatment to more firmly establish the contingency between the neutral stimuli and the target location to produce changes in attentional processes away from threat, as recommended by Bar-Haim (2010) and Pergamin-Hight and colleagues (2016). Contrary to our expectations, we found no evidence for change in threat biases on the dot-probe task or changes in clinical severity ratings on the ADIS-C/P in either our ABMT or ACT conditions. Moreover, although we found changes in social anxiety symptoms in both conditions, the reduction in symptoms were small and comparable over time in both conditions based on parent and adolescent reports. Furthermore, very few of the youth were diagnosis free following treatment (between 10 and 14%). These findings are consistent with the majority of findings reviewed by Cristea and colleagues (2015) in their recent meta-analysis.
Recent research in this area (e.g., Dudeney et al., 2015; Pergamin-Hight et al., 2016) has suggested that one of the reasons for the lack of salutatory effects for ABMT among teens is related to characteristics of the adolescents that might serve to moderate treatment outcomes. Person-specific variables such as the extent of pre-treatment attention bias, the severity of social anxiety symptoms, and the level of attention control have been suggested. In this study, we explored each of these variables and found limited to no support for them. Severity of social anxiety as determined by the ADIS-C/P failed to moderate the relationship between treatment condition and parent-reported social anxiety symptoms at either post-treatment or 3-month follow-up; however, for adolescent self-report of social anxiety symptoms, adolescents who self-reported less social anxiety prior to treatment reported significantly less social anxiety at 3-month follow-up (but not at post-treatment) if they received ACT and not ABMT. Although intuitive that the less impaired youth would continue to be relatively less anxious following treatment, it is not clear why this was seen only for those in the attention control condition. It is certainly conceivable that the ACT condition used in our study provided the necessary contingency between the neutral stimuli and the target location (50% of the trials) to produce subsequent changes in self-reported social anxiety, especially so for those individuals low in social anxiety. This finding however, has not been reported previously and replication is needed to determine if this finding is a robust one.
In addition, parent-reported attention control significantly moderated the relationship between treatment condition and parent rated social anxiety at post-treatment but not at 3-month follow-up. Specifically, adolescents whose pre-treatment attention control scores were high had significantly lower social anxiety, as rated by their parents, at post-treatment if they were randomized to the ABMT condition. That is, if the adolescents who had the pre-treatment capacity to focus their attention as well as shift their attention away from threat received ABMT they did better than youth in the control condition. Although interesting and again intuitive, these findings are in contrast to those reported by Pergamin-Hight and colleagues (2015), who found that youth whose parents reported them as lower in attention control benefitted more from ABMT than youth whose parents rated them as higher in attention control. It should be noted, however, that the Pergamin-Hight review did not focus on SAD specifically, but rather a range of disorders (e.g., PTSD, specific phobia). This is important because of the strong association between social anxiety and self-focused attention and negative affect. Lonigan and colleagues (2004), for example, have postulated that the interaction of negative affect and effortful control determines patterns of attentional allocation toward threatening stimuli. In particular, attention control may promote resilience, even in psychologically vulnerable youth (e.g., Lonigan & Vasey, 2009). In our study, it is conceivable that teens with higher attention control were better able to more fully assimilate the retraining and thereby experience reduced social anxiety. However, once again, replication is needed to determine if this finding is robust across samples.
Limitations
Although we based our ABMT design on experimental techniques that have met with success in modifying attention and anxiety symptoms in adults with SAD (e.g., Schmidt et al., 2009), it is possible that the executive functioning capacities needed to benefit from this design are underdeveloped in early and middle adolescence (see Monk et al., 2003). As such, it is possible that underdeveloped executive control systems played a role in our failure to find group differences. However, with the exception of a relatively briefer duration (e.g., 300msec vs 500msec), our ABM protocol mirrored the procedures used successfully in adults. Most prior work in the attention modification literature with both youth and adults has focused on the middle range of presentation times (500ms; see Heeren, Mogoaşe, Philippot, & McNally, 2015 for review). In light of the generally mixed evidence for such protocols, we opted to use a presentation time of 300ms for facial stimuli in our study. This decision was not only informed by reaction-time based studies which have suggested that the early vigilance effect decreases as stimulus duration increases (c.f. Bantin et al., 2016), but also electrophysiological data focusing on automatic neural processing of threat stimuli in social anxiety. Data from event-related potentials (ERPs) collectively suggests that an early automatic stage of processing associated with enhanced early ERPs to threat-related stimuli occur within 100–200ms of onset (P1, P2, N2; Straube, Mothes-Lasch, & Miltner, 2011). These early potentials are associated with automatic perceptual orienting, whereas more controlled and conscious stages of processing are associated with enhanced responses of late positive components beginning around 300ms (Schupp et al., 2000; Straube et al., 2011). Thus we reasoned that if ABM truly targets “biased” attention, which is premised upon enhancements in neural systems for rapid orientation toward threat, then the training effect should be potentiated by relatively briefer stimulus durations in the range of 100–300ms. Thus, we believe that our choice of 300msec was warranted and that it provided a better test of biased attention than does the use of 500msec. Of course, this too awaits further inquiry, perhaps even a study directly comparing stimulus durations of not only 300msec and 500mec but also a longer duration of up to 800msec for youth.
In addition, it is important to consider how procedural elements of the trial may have provided inadvertent exposure, particularly for socially anxious youth. Specifically, the procedural 5-minute conversations between the therapists and the participating youth might have resulted in therapeutic effects (i.e., exposure). Further, videotaping the conversations could also constitute exposure for social anxiety. This additional exposure was unavoidable as videotaping of the sessions was required per the institution’s review board protocol. Together, these factors may account for a portion of the noted treatment effects, although once again the treatment effects were not robust ones. Finally, it is important to note that due to the stimulus set used in our study (adolescent facial images from the NIMH-CheFS adolescent stimulus set, Egger et al., 2011), we were not able to explore whether utilization of disgust stimuli as opposed to anger stimuli would have resulted in different outcomes. Since disgust has also been found to be associated with attention in social anxiety (e.g., Amir, Najmi, Bomyea, & Burns, 2010; Buckner, Maner, & Schmidt, 2010), it is important to explore this socially threatening emotion in future studies.
Future Directions
Although attention bias was initially conceptualized as heightened attention orienting (MacLeod et al., 1986), recent work has suggested the involvement of alternative attention processes, such as difficulty in disengagement of attention, which may involve a longer time course (Cisler & Koster, 2010). In support of this hypothesis, neuroimaging work has suggested the most common ABM paradigm, the dot probe, is instead a measure of attention disengagement (Price et al., 2014). Further research is needed to elucidate the attention processes addressed by ABMT, and the optimal stimuli duration to target these processes.
Further, given that a growing body of literature raises concern about the sensitivity and reliability of reaction time scores on the dot probe task, use of alternative research methodologies, such as eye tracking, should be considered in future ABMT work in order to determine if overt indices of attention are more sensitive to the measurement and thus change in attention biases to threat.
Conclusions
In sum, this RCT includes one of the largest and most rigorously characterized samples of adolescents with SAD participating in ABMT to date. Our results suggest ABMT, as we implemented it, is no more effective than an attention control placebo in reducing social anxiety or targeting the mechanism of interest - attention bias. Clinically, observed changes were modest and very few of the youth were diagnosis free following treatment or three months thereafter. Our findings, along with those of others, suggest that ABMT as it is currently used may not be effective and that modifications in the ABMT paradigm may be necessary before more substantial effects can be obtained with adolescents.
Highlights.
We compared Attention Bias Modification Treatment to a control for youth with SAD
No differences in ABMT and the control in reducing social anxiety or attention bias
Need for modifications within ABMT to enhance salutatory effects for SAD
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abend R, de Voogd L, Salemink E, Wiers RW, Pérez-Edgar K, Fitzgerald A, … Pettit JW. Association between attention bias to threat and anxiety symptoms in children and adolescents. Depression and Anxiety. 2018;35:229–238. doi: 10.1002/da.22706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Amir N, Najmi S, Bomyea J, Burns M. Disgust and anger in social anxiety. International Journal of Cognitive Therapy. 2010;3:3–10. doi: 10.1521/ijct.2010.3.1.3. [DOI] [Google Scholar]
- Bantin T, Stevens S, Gerlach AL, Hermann C. What does the facial dot-probe task tell us about attentional processes in social anxiety? A systematic review. Journal of Behavior Therapy and Experimental Psychiatry. 2016;50:40–51. doi: 10.1016/j.jbtep.2015.04.009. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y. Research review: Attention bias modification (ABM): A novel treatment for anxiety disorders. Journal of Child Psychology and Psychiatry. 2010;51:859–870. doi: 10.1111/j.1469-7610.2010.02251.x. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, McKenzie Neer S. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Bradley BP, Mogg K, Millar N, Bonham-Carter C, Fergusson E, Jenkins J, Parr M. Attentional biases for emotional faces. Cognition & Emotion. 1997;11:25–42. doi: 10.1080/026999397380014. [DOI] [Google Scholar]
- Buckner JD, Maner JK, Schmidt NB. Difficulty disengaging attention from social threat in social anxiety. Cognitive Therapy and Research. 2010;34:99–105. doi: 10.1007/s10608-008-9205-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmona AR, Kuckertz JM, Suway J, Amir N, Piacentini J, Chang SW. Attentional bias in youth with clinical anxiety: The moderating effect of age. Journal of Cognitive Psychotherapy. 2015;29:185–196. doi: 10.1891/0889-8391.29.3.185. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Koster EH. Mechanisms of attentional biases towards threat in anxiety disorders: An integrative review. Clinical psychology Review. 2010;30:203–216. doi: 10.1016/j.cpr.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffman MC, Trubanova A, Richey JA, White SW, Kim-Spoon J, Ollendick TH, Pine DS. Validation of the NIMHChEFS adolescent face stimulus set in an adolescent, parent, and health professional sample. International Journal of Methods in Psychiatric Research. 2015;24:275–286. doi: 10.1002/mpr.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper RM, Langton SR. Attentional bias to angry faces using the dot-probe task? It depends when you look for it. Behaviour Research and Therapy. 2006;44:1321–1329. doi: 10.1016/j.brat.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Cristea IA, Mogoaşe C, David D, Cuijpers P. Practitioner review: cognitive bias modification for mental health problems in children and adolescents: a meta-analysis. Journal of Child Psychology and Psychiatry. 2015;56:723–734. doi: 10.1111/jcpp.12383. [DOI] [PubMed] [Google Scholar]
- Dudeney J, Sharpe L, Hunt C. Attentional bias towards threatening stimuli in children with anxiety: A meta-analysis. Clinical Psychology Review. 2015;40:66–75. doi: 10.1016/j.cpr.2015.05.007. [DOI] [PubMed] [Google Scholar]
- Eldar S, Apter A, Lotan D, Edgar KP, Naim R, Fox NA, … Bar-Haim Y. Attention bias modification treatment for pediatric anxiety disorders: A randomized controlled trial. American Journal of Psychiatry. 2012;169:213–230. doi: 10.1176/appi.ajp.2011.11060886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis LK, Rothbart MK. Revision of the early adolescent temperament questionnaire. Poster presented at the 2001 biennial meeting of the Society for Research in Child Development; Minneapolis, Minnesota. 2001. Apr, [Google Scholar]
- Egger HL, Pine DS, Nelson E, Leibenluft E, Ernst M, Towbin KE, Angold A. The NIMH Child Emotional Faces Picture Set (NIMH-ChEFS): A new set of children’s facial emotion stimuli. International Journal of Methods in Psychiatric Research. 2011;20:145–156. doi: 10.1002/mpr.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Mistler SA, Keller BT. Multilevel multiple imputation: A review and evaluation of joint modeling and chained equations imputation. Psychological Methods. 2016;21:222–240. doi: 10.1037/met0000063. [DOI] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency and comorbidity of social phobia and social fears in adolescents. Behaviour Research and Therapy. 1999;37:831–843. doi: 10.1016/S0005-7967(98)00179-X. [DOI] [PubMed] [Google Scholar]
- Field AP, Lester KJ. Is there room for ‘development’ in developmental models of information processing biases to threat in children and adolescents? Clinical Child and Family Psychology Review. 2010;13:315–332. doi: 10.1007/s10567-010-0078-8. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Becker EM, Keeton CP, Sakolsky D, Piacentini J, Albano A, … Kendall PC. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry. 2014;71:310–318. doi: 10.1001/jamapsychiatry.2013.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM, … March J. Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. Journal of Consulting and Clinical Psychology. 2011;79:806–813. doi: 10.1037/a0025933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, … Pine DS. Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeren A, Mogoaşe C, Philippot P, McNally RJ. Attention bias modification for social anxiety: A systematic review and meta-analysis. Clinical Psychology Review. 2015;40:76–90. doi: 10.1016/j.cpr.2015.06.001. [DOI] [PubMed] [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, Chorpita BF. Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child & Adolescent Psychology. 2016;45:91–113. doi: 10.1080/15374416.2015.1046177. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Keers R, Roberts S, Coleman JR, Breen G, Arendt K, … Eley TC. Clinical predictors of response to cognitive-behavioral therapy in pediatric anxiety disorders: the Genes for Treatment (GxT) study. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54:454–463. doi: 10.1016/j.jaac.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James AC, James G, Cowdrey FA, Soler A, Choke A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Systematic Reviews. 2013;6:1–104. doi: 10.1002/14651858.CD004690.pub3. [DOI] [PubMed] [Google Scholar]
- Linetzky M, Pergamin-Hight L, Pine DS, Bar-Haim Y. Quantitative evaluation of the clinical efficacy of attention bias modification treatment for anxiety disorders. Depression and Anxiety. 2015;32:383–391. doi: 10.1002/da.22344. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW. Negative affectivity, effortful control, and attention to threat-relevant stimuli. Journal of Abnormal Child Psychology. 2009;37:387–399. doi: 10.1007/s10802-008-9284-y. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW, Phillips BM, Hazen RA. Temperament, anxiety, and the processing of threat-relevant stimuli. Journal of Clinical Child and Adolescent Psychology. 2004;33:8–20. doi: 10.1207/S15374424JCCP3301_2. [DOI] [PubMed] [Google Scholar]
- MacLeod C, Clarke PJ. The attentional bias modification approach to anxiety intervention. Clinical Psychological Science. 2015;3:58–78. doi: 10.1177/2167702614560749. [DOI] [Google Scholar]
- MacLeod C, Mathews AM, Tata P. Attentional bias in emotional disorders. Journal of Abnormal Psychology. 1986;95:15–20. doi: 10.1037/0021-843X.95.1.15. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J. Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogg K, Bradley B, Miles F, Dixon R. Brief report: Time course of attentional bias for threat scenes: Testing the vigilance-avoidance hypothesis. Cognition and Emotion. 2004;18:689–700. doi: 10.1080/02699930341000158. [DOI] [Google Scholar]
- Mogg K, Philippot P, Bradley BP. Selective attention to angry faces in clinical social phobia. Journal of Abnormal Psychology. 2004;113:160–165. doi: 10.1037/0021-843X.113.1.160. [DOI] [PubMed] [Google Scholar]
- Monk CS, McClure EB, Nelson EE, Zarahn E, Bilder RM, Leibenluft E, … Pine DS. Adolescent immaturity in attention-related brain engagement to emotional facial expressions. Neuroimage. 2003;20:420–428. doi: 10.1016/S1053-8119(03)00355-0. [DOI] [PubMed] [Google Scholar]
- Mogoaşe C, David D, Koster EH. Clinical efficacy of attentional bias modification procedures: An updated meta-analysis. Journal of Clinical Psychology. 2014;70:1133–1157. doi: 10.1002/jclp.22081. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Benoit KE, Grills-Taquechel AE. Social anxiety disorder in children and adolescents. In: Weeks J, editor. The Wiley Blackwell handbook of social anxiety disorder. New York: John Wiley & Sons, Inc; 2014. pp. 179–200. [DOI] [Google Scholar]
- Öst LG, Ollendick TH. Brief, intensive and concentrated cognitive behavioral treatments for anxiety disorders in children: A systematic review and meta-analysis. Behaviour Research & Therapy. 2017;97:134–145. doi: 10.1016/j.brat.2017.07.008. [DOI] [PubMed] [Google Scholar]
- Pergamin-Hight L, Naim R, Bakermans-Kranenburg MJ, van IJzendoorn MH, Bar-Haim Y. Content specificity of attention bias to threat in anxiety disorders: A meta-analysis. Clinical Psychology Review. 2015;35:10–18. doi: 10.1016/j.cpr.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Pergamin-Hight L, Pine DS, Fox NA, Bar-Haim Y. Attention bias modification for youth with social anxiety disorder. Journal of Child Psychology and Psychiatry. 2016;57:1317–1325. doi: 10.1111/jcpp.12599. [DOI] [PubMed] [Google Scholar]
- Pishyar R, Harris LM, Menzies RG. Responsiveness of measures of attentional bias to clinical change in social phobia. Cognition and Emotion. 2008;22:1209–1227. doi: 10.1080/02699930701686008. [DOI] [Google Scholar]
- Price RB, Siegle GJ, Silk JS, Ladouceur CD, McFarland A, Dahl RE, Ryan ND. Looking under the hood of the dot-probe task: An fMRI study in anxious youth. Depression and Anxiety. 2014;31:178–187. doi: 10.1002/da.22255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puliafico AC, Kendall PC. Threat-related attentional bias in anxious youth: A review. Clinical Child and Family Psychology Review. 2006;9:162–180. doi: 10.1007/s10567-006-0009-x. [DOI] [PubMed] [Google Scholar]
- Putnam SP, Ellis LK, Rothbart MK. The structure of temperament from infancy through adolescence. In: Eliasz A, Anglietner A, editors. Advances in research on temperament. Lengerich, Germany: Pabst Science Publishers; 2001. pp. 164–182. [Google Scholar]
- Roy AK, Vasa RA, Bruck M, Mogg K, Bradley BP, Sweeney M, … CAMS Team Attention bias toward threat in pediatric anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:1189–1196. doi: 10.1097/CHI.0b013e3181825ace. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Buckner JD, Timpano KR. Attention training for generalized social anxiety disorder. Journal of Abnormal Psychology. 2009;118:5–14. doi: 10.1037/a0013643. [DOI] [PubMed] [Google Scholar]
- Schupp HT, Cuthbert BN, Bradley MM, Cacioppo JT, Ito T, Lang PJ. Affective picture processing: the late positive potential is modulated by motivational relevance. Psychophysiology. 2000;37:257–261. doi: 10.1111/1469-8986.3720257. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV (Child and Parent Versions) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan CL, March S, Kenardy JA, Hearn CS. Generic versus disorder specific cognitive behavior therapy for social anxiety disorder in youth: A randomized controlled trial using internet delivery. Behaviour Research and Therapy. 2017;90:41–57. doi: 10.1016/j.brat.2016.12.003. [DOI] [PubMed] [Google Scholar]
- Stevens S, Rist F, Gerlach AL. Eye movement assessment in individuals with social phobia: Differential usefulness for varying presentation times? Journal of Behavior Therapy and Experimental Psychiatry. 2011;42:219–224. doi: 10.1016/j.jbtep.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Straube T, Mothes-Lasch M, Miltner WH. Neural mechanisms of the automatic processing of emotional information from faces and voices. British Journal of Psychology. 2011;102:830–848. doi: 10.1111/j.2044-8295.2011.02056.x. [DOI] [PubMed] [Google Scholar]
- Vassilopoulos SP. Social anxiety and the vigilance-avoidance pattern of attentional processing. Behavioural and Cognitive Psychotherapy. 2005;33:13–24. doi: 10.1017/S1352465804001730. [DOI] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, … Kendall P. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AM, Mogg K, Bradley BP, Pine DS. Attention bias for angry faces in children with social phobia. Journal of Experimental Psychopathology. 2011;2:475–489. doi: 10.5127/jep.018111. [DOI] [Google Scholar]
- Wieckowski AT, Coffman MC, Kim-Spoon J, White SW, Richey JA, Ollendick TH. Impaired fear recognition and social anxiety symptoms in adolescence. Journal of Child and Family Studies. 2016;25:3381–3386. doi: 10.1007/s1082. [DOI] [PMC free article] [PubMed] [Google Scholar]