Abstract
Neurocognitive and theory of mind deficits, dysfunctional attitudes, and negative symptoms have all been linked to poor functioning in schizophrenia, but interactions among these factors have not been extensively examined. We investigated whether dysfunctional attitudes (e.g., defeatist performance beliefs and social disinterest attitudes) moderated associations between neurocognition and theory of mind and poor everyday functioning and social competence in 146 participants with schizophrenia. We examined whether cognitive deficits are more likely to influence functioning in participants with more severe dysfunctional attitudes. Social disinterest, but not defeatist performance, attitudes were found to moderate associations between cognitive deficits and social competence but not everyday functioning, such that neurocognition and theory of mind deficits were only associated with poorer social competence in participants with more severe social disinterest attitudes. In contrast, no significant moderation effects were found for defeatist performance beliefs. Findings indicate that deficits in abilities were less likely to impact social competence in participants with greater interest in socializing. It may be that greater motivation for socializing engenders increased practice and engagement in social interactions, which then leads to greater social competence despite poor cognitive abilities. Treatments that target social disinterest attitudes may lead to greater social competence and engagement.
Keywords: neurocognition, theory of mind, dysfunctional attitudes, social disinterest attitudes, social competence
1.0. Introduction
Participants with schizophrenia frequently experience severe impairment in a range of functional domains, including recreational activities, interpersonal relationships, and vocational performance (Addington et al., 2003; Harvey et al., 2012; Kalin et al., 2015). These functional impairments are enduring in the prodromal and first episode stages of the disorder (Ventura et al., 2011) and persisting throughout adult life (Bergh et al., 2016). While current pharmacologic treatments are effective for alleviating some clinical symptom severity (i.e., positive symptoms), difficulties in everyday functioning largely remain intractable with pharmacologic treatment alone (Liberman and Kopelowicz, 2005; Robinson et al., 2004). A variety of factors have been identified as unique predictors of functional outcome, but the interaction among these factors and how they impact functioning has been less explored. This is an important area of research as it could aid in the identification of patients most likely to benefit from specific treatments and novel treatment targets to improve functioning for this population.
The vast majority of the literature on the correlates and predictors of functional impairment in schizophrenia has concentrated on cognitive processes such as neurocognition and social cognition (Bowie et al., 2008; Brekke et al., 2005; Green et al., 2004). Deficits in basic cognitive abilities (e.g., processing speed, memory, attention) have been robustly linked with disability in schizophrenia both concurrently and prospectively (Bowie et al., 2008; Green et al., 2004, 2000). More specifically, these neurocognitive deficits are reliably and highly associated with poorer social skills, higher unemployment rates, difficulty with independent living, less time spent in the community, and reduced success following rehabilitation programs (Green et al., 2000; Leifker et al., 2009). Investigators have also focused on alternative cognitive abilities that may explain additional variance in functioning in this population. Social cognition, broadly defined as the ability of individuals to perceive, interpret, and respond to the dispositions, intentions, and behaviors of others, has emerged as a likely mediator as it requires basic cognitive skills and has clear links to several indices of social functioning (Lam et al., 2014; Schmidt et al., 2011; Vauth et al., 2004). Of the myriad of social cognitive components, theory of mind (ToM), or the skills to understand the intentions and beliefs of others, appears to have the most robust associations with functional outcomes. For example, investigators have found that ToM predicts multiple domains of functioning above and beyond the influence of neurocognition (Couture et al., 2011; Fett et al., 2011), and accounts for greater variance in everyday functioning than neurocognition and other aspects of social cognition in several studies (Brüne et al., 2007; Pinkham and Penn, 2006).
While neuro- and social cognition explains a significant amount of the variance in functional outcomes, approximately 40–80% of the variance remains unaccounted for (Green et al., 2000). Recent evidence suggests that dysfunctional attitudes play a prominent role in functional outcomes in schizophrenia. Beck and colleagues (Grant and Beck, 2009; Rector et al., 2005) initially posited that cognitive deficits, stigma, and other illness-related factors precipitates failure experiences that consequently engenders dysfunctional attitudes (e.g. “If you cannot do something well, there is little point in doing it at all”), notably defeatist performance beliefs and social disinterest attitudes, which diminishes motivation and engagement in vocational, recreational, and social activities. Consistent with this model, Quinlan, Roesch, and Granholm (2014) utilized structural equation modeling to demonstrate the following pathway from neurocognition to functional outcome: Neurocognition ➔ defeatist performance beliefs ➔ negative symptoms ➔ real-world functioning. Elevations in defeatist performance beliefs and social disinterest attitudes, both of which are the most commonly researched dysfunctional attitudes and originally proposed by Beck and colleagues (Grant and Beck, 2009; Rector et al., 2005), have been reliably documented across the schizophrenia spectrum (Granholm et al., 2016; Kiwanuka et al., 2014; Luther et al., 2016; Ventura et al., 2014), and a recent meta-analysis (Campellone et al., 2016) revealed moderate associations between defeatist performance beliefs and negative symptoms (d = .25) and function (d = −.27).
As noted earlier, functioning encompasses a wide range of domains (e.g., recreational activities, interpersonal relationships, and vocational performance). Recent research suggests that these different domains of functioning, namely everyday and social, may have differential correlates and predictors (Strassnig et al., 2015). For instance, cognitive deficits have been found to largely predict impairments in vocational and everyday activities, while negative symptoms appear to be more related social activities than other components of functional outcomes (Leifker et al., 2009; Strassnig et al., 2015). Therefore, different dysfunctional attitudes (defeatist performance beliefs vs. social disinterest attitudes) may have unique relationships with different aspects of functional outcomes. Defeatist performance beliefs, or over-generalized negative beliefs regarding one’s own task-related abilities (e.g., “Why bother, I’ll just fail again”), have been more generally related to measures of everyday functioning (e.g., vocation, independent living; (Grant and Beck, 2009; Kiwanuka et al., 2014). Conversely, social disinterest attitudes such as increased preference for being alone over being with others (e.g., “I attach very little importance to having close friends”) and negative expectancies (e.g., “There are few things more tiring than to have a long, personal discussion with someone”) regarding pleasurable social experiences appear to be more related to measures of social functioning in schizophrenia. Social disinterest attitudes, which reflect negative attitudes regarding the consequences of close social interactions rather than the actual experienced pleasure from social interactions (i.e., social anhedonia), may develop from repeated failures in negative social experiences, leading to withdrawal from social activities and affiliation. Within the schizophrenia spectrum, individuals with greater social disinterest are more likely to be isolated, and experience more positive and less negative emotion when they are socially isolated (Brown et al., 2007). Consistent with this notion, Grant and Beck (2010) observed that social disinterest attitudes predicted real-world social functioning, but not vocational, above and beyond the influence of depression and neurocognition, and Thomas and colleagues (2017) found similar unique pathways for defeatist performance and asocial beliefs in a longitudinal study. Lastly, Granholm and colleagues (2013a) observed that greater endorsement of dysfunctional attitudes specifically pertaining to social performance at any point during the day were associated with decreased positive emotion and increased social withdrawal over subsequent hours using ecological momentary assessments.
Taken together, neurocognition, theory of mind, and dysfunctional attitudes have been identified as consistent, yet modest, predictors of functional outcomes in schizophrenia. However, interactions between these factors have yet to be thoroughly explored, and it is possible that combinations of these factors will result in stronger prediction. The primary aim of the current study was to investigate whether dysfunctional attitudes, specifically defeatist performance beliefs and social disinterest attitudes, moderate links between neurocognition and theory of mind and specific aspects of functioning (e.g., everyday functioning and social competence); that is, whether cognitive deficits (i.e., neurocognition and theory of mind) are more likely to influence functioning in participants with schizophrenia with varying levels of dysfunctional attitudes. The current study was motivated by the hypothesis that less severe dysfunctional attitudes would be associated with successful functional outcomes, even in the presence of cognitive impairments (i.e., neurocognitive and theory of mind deficits). Thus, we predicted that social disinterest attitudes would moderate the associations between cognition and social competence, defined as the capacity to solve interpersonal problems through verbal and non-verbal communication, while defeatist performance beliefs would moderate the associations between cognition and everyday functioning, defined as performing leisure, home-care, self-care, and vocational activities. More specifically, we hypothesized that the associations between neurocognitive and theory of mind abilities and functional outcomes would be stronger in participants with more severe dysfunctional attitudes compared to participants with less severe dysfunctional attitudes.
2.0. Methods
2.1. Participants
Participants included 146 adults with DSM-IV diagnoses of either schizophrenia (80%) or schizoaffective (20%) disorder based on a structured clinical interview (SCID; First et al., 2002). Community dwelling participants were originally recruited from a clinical trial study and measures reported in this study were collected at the baseline evaluation preceding randomization to treatment (Granholm et al., 2014, 2013b). All participants were living in the community, although a majority of the sample resided in “Assisted Housing” (75%), which were group homes that provided room and board and minimal other housing services. Exclusion criteria included the following: a) debilitating psychiatric (e.g., acutely ill or substance use) or medical conditions (e.g., traumatic brain injury, neurological illness) that would hinder participation outpatient psychotherapy or assessments and b) received previous psychosocial treatment (e.g., social skills training, cognitive behavioral therapy) within the preceding 5 years. Almost all participants (97%) endorsed taking at least one antipsychotic medication, and a modest portion (30%) endorsed taking at least one antidepressant or mood stabilizer. The Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987) was administered to evaluate positive (ICC = .87) and negative (ICC = .83) symptomatology. Table 1 presents demographic and clinical data of the study sample.
Table 1.
Characteristics of demographics and study variables (N = 146)
| Variable | Mean (SD) |
|---|---|
| Demographics | |
| Age | 41.5 (9.6) |
| Sex (% male) | 68% |
| Education (years) | 12.3 (1.7) |
| Ethnicity (% Caucasian) | 56% |
| Assisted Housing (%) | 75% |
| Married (%) | 7% |
| PANSS Positive Subscale Score | 19.0 (6.5) |
| PANSS Negative Subscale Score | 15.6 (6.1) |
| Study Variables | |
| Neurocognition Composite | 33.6 (7.6) |
| Hinting Task Total | 12.9 (4.2) |
| DPAS | 53.6 (17.3) |
| Social Disinterest Attitudes | 6.0 (2.9) |
| ILSS Total | .71 (.1) |
| MASC Effectiveness | 3.29 (1.1) |
Note. PANSS = Positive and Negative Syndrome Scale; DPAS = Defeatist Performance Attitude Scale; ILSS = Independent Living Skills Survey; MASC = Maryland Assessment of Social Competence.
2.2. Neurocognition
Multiple neurocognitive domains were evaluated using tests derived from the Delis–Kaplan Executive Functioning System (DKEFS; Delis et al., 2001) and the MATRICS Consensus Cognitive Battery (MCCB; Nuechterlein et al., 2008) in order to samples an array of neurocognitive domains. Each domain score (mean of age and sex corrected T scores from the respective DKEFS or MCCB batteries) were calculated by the following tests. Speed of Processing was assessed with the Brief Assessment of Cognition in Schizophrenia Symbol Coding (BACS; Keefe et al., 2004) and Trail Making Test A (Reitan and Wolfson, 2009). Verbal Learning was measured with the Hopkins Verbal Learning Test-Revised total score (HVLT-R; Benedict et al., 1998). Working Memory was evaluated via the Wechsler Memory Scale-Third Edition Spatial Span (WMS-III; (Wechsler, 1997a) and Wechsler Adult Intelligence Scale-Third Edition Letter–Number Sequencing subtest (WAIS-III; Wechsler, 1997). Visual Learning was measured with the Brief Visuospatial Memory Test-Revised total score (BVMT-R; Benedict et al., 1996). Finally, Executive Functioning was measured with the BACS Letter Fluency (Keefe et al., 2004) and the D-KEFS Card Sorting, 20 Questions, and Word Context (Delis et al., 2001). A global neurocognitive composite score was subsequently calculated by averaging every T score from each domain.
2.3. Theory of Mind (ToM)
Theory of mind was measured with The Hinting Task (Greig et al., 2004). The Hinting Task asks participants to deduce the intentions of others based on hints from 10 auditory vignettes of social interactions. For each vignette, participants are awarded two points on the first attempt if the participant correctly answers the question. However, if the participant does not successfully answer the question on the first attempt, then an additional hint is provided and one point is subsequently awarded if the participant gives the correct response on the second attempt. An incorrect response on second step results zero points. The study used a version of the Hinting task that included a speech intonation manipulation to emphasize the hint. Performance on two presentation styles (i.e., speech intonation emphasized hint vs. neutral tone) were not significantly different, t(192) = .63, p= .53, and the internal consistency of the 10-item measure had adequate reliability (α=.80); thus, a composite score for the 10 auditory vignettes were used in the present analyses.
2.4. Defeatist Performance Attitudes
The Defeatist Performance Attitude Scale (DPAS) is a 15-item self-report subscale selected from a factor analysis (Cane et al., 1986) of the Dysfunctional Attitude Scale (Weissman, 1979). The DPAS measures endorsement of defeatist attitudes regarding one’s own ability to complete goal-directed activities (e.g., “If you cannot do something well, there is little point in doing it at all,” “People will probably think less of me if I make mistakes and fail”). Items are rated on a 7-point Likert scale with higher scores indicating elevated defeatist performance attitudes.
2.5. Social Disinterest Attitudes
The Asocial Beliefs Scale (ABS), developed by Grant and Beck (2010), is a 15-item self-report subscale with face validity selected from the commonly used the Revised Social Anhedonia Scale (RSAS; Eckblad et al., 1982). The RSAS is comprised of 40 true or false questions that were proposed to measure social anhedonia, a heterogeneous construct that taps both disinterest and apathy for social contact and deficits experiential pleasure from interpersonal relationships and social interactions (Blanchard et al., 2000; Leak, 1991). The fifteen social disinterest attitudes items selected avoided items that assesses emotional experiences (i.e. pleasure from social contact or broad emotion dysregulation) and frequency of actual social interactions and focused on negative expectancies or apathy for close social contact and relationships, defined as performing leisure, home-care, self-care, and vocational activities. The ABS was observed to have comparable internal consistency (α=.65) to other RSAS subscales factor analyses (Blanchard et al., 2000). A list of the selected RSAS social disinterest items is provided in Granholm and colleagues (2009) and Grant and Beck (2010). Higher scores indicate elevated social disinterest attitudes.
2.6. Social Competence
The Maryland Assessment of Social Competence (MASC; Bellack et al., 2006) was used to index social competence. The MASC is a performance based, structured role-playing task that assesses the participant’s abilities to resolve interpersonal conflicts through productive conversations. Participants engaged in three simulated conversations (1 initiation, 2 assertiveness) with a live confederate for 3 minutes. Participant responses were videotaped and subsequently coded by blind raters on verbal content, nonverbal communication behaviors, and overall effectiveness. Exceptional interrater reliability (ICC = .86) was achieved due to regular supervision. Overall effectiveness was used in analyses as indicated with lower scores indicating poorer social problem-solving abilities.
2.7. Everyday Functioning
The Independent Living Skills Survey (ILSS; Wallace et al., 2000) is an interview based measure of self-report everyday functioning. The ILSS assesses the following ten domains of functioning (70 items overall) over the past 30 days: Personal hygiene, Care of personal possessions, Appearance, Food preparation, Leisure, Health Maintenance, Transportation, Money Management, Job Seeking, and Job Maintenance. Each item from the 10 domains is answered with a “yes” (activity performed = 1 point), a “no” (activity not performed =0 point), or “unable to demonstrate” (e.g., finances and meals prepared for participant residing in an assisted-living facility). An ILSS total score (range = 0 – 1) was calculated by taking the mean of all available domains (i.e., “yes” or “no” for an activity performed) and used in analyses as indicated.
2.8. Statistical Analysis
We examined potential demographic (e.g., age, gender, ethnicity) associations with study variables that might inform subsequent analyses. Pearson correlations were used to examine the inter-relationships between neurocognition, theory of mind, defeatist performance beliefs, social disinterest attitudes, social functioning, and every day functioning. Next, a series of separate linear regression models were used to test our main hypotheses. Moderation and simple slope analyses were assessed using PROCESS for SPSS (Hayes, 2013). The first set of linear regression models tested the moderating effects of defeatist performance beliefs on the relationship of cognition (neurocognition, theory of mind) to functional outcome. Defeatist performance beliefs and neurocognition were centered and entered along with their cross product as predictors for each functional outcome measure (ILSS and MASC). Next, defeatist performance beliefs and theory of mind were centered and entered along with their cross product as predictors for each functional outcome variable (ILSS and MASC). We then tested the moderating effects of social disinterest attitudes on the relationship between cognitive abilities and functional outcome using identical procedures listed for defeatist performance beliefs. Simple slope coefficients, produced by PROCESS, were used to evaluate the association between cognition and functional outcome at low (< −1 SD below the mean), moderate (between 1 SD below and 1 SD above the mean) and high (> 1 SD above the mean) levels of dysfunctional attitudes for any significant interactions (Aiken and West, 1991). The Johnson–Neyman technique (Hayes, 2013; Rast et al., 2014) was also used to demonstrate the specific point of dysfunctional attitudes where associations between the cognitive variables and functional outcomes were significant. For graphic illustrations of interaction effects, three subgroups based on low (<1 SD), moderate (between 1 SD below and 1 SD above the mean) and high (>1 SD) attitude scale scores were created and the associations between cognition and functioning variables were graphed for each subgroup. All tests were two-tailed and all variables normally distributed (skew < 1.5). See Footnote 1.0 and 2.0 for exploratory analyses.
3. Results
3.1. Associations among study variables
Table 1 presents descriptive statistics for all study variables in regression analyses, while correlations among study variables are presented in Table 2. Demographic data were unrelated to study variables. Modest but significant were found between neurocognition and defeatist performance beliefs (r = −.19, p < 0.05) and everyday functioning (r = .17, p < 0.05), while strong relationships were observed for neurocognition and theory of mind (r = .44, p < 0.01). Defeatist performance beliefs were related to social disinterest attitudes (r = .26, p < 0.01). Social competence was modestly related to defeatist performance beliefs (r = −.19, p < 0.05) and everyday functioning (r = .19, p < 0.05), and more strongly related to neurocognition (r = .36, p < 0.01), theory of mind (r = .41, p < 0.01), and social disinterest attitudes (r = −.25, p <0.01).
Table 2.
Pearson correlations among study variables.
| ToM | Defeatist Performance Beliefs | Social Disinterest Attitudes | Everyday Functioning | Social Competence | |
|---|---|---|---|---|---|
| Neurocognition | 0.44** | −0.19* | −0.13 | 0.17* | 0.36** |
| ToM | - | -0.10 | -0.13 | 0.14 | 0.41** |
| Defeatist Performance Beliefs | - | 0.26** | −0.09 | −0.19* | |
| Social Disinterest Attitudes | - | −0.13 | −0.25** | ||
| Everyday Functioning | - | 0.19* |
Note. ToM = Theory of Mind
p < 0.05
p < 0.01
3.2. Moderating effects of defeatist performance beliefs
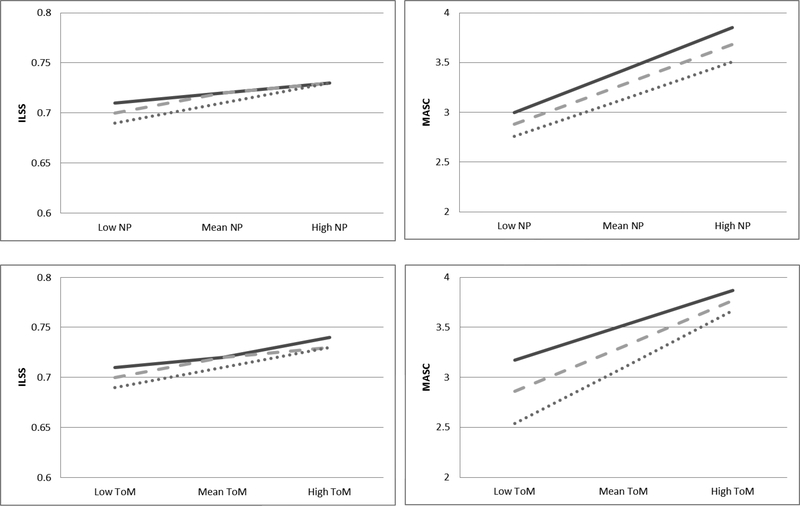
The interaction term of defeatist performance beliefs and neurocognition did not account for significant variance in everyday functioning or social competence (Table 3). The cross product of defeatist performance beliefs and theory of mind also did not significantly predict our everyday functioning or social competence as well (Table 3). Thus, our hypothesis that defeatist performance beliefs would moderate the associations between cognitive processes and functioning was not supported (see Figure 1).
Table 3.
Multiple regression for the prediction of functional outcome by cognition, defeatist performance beliefs, and their interaction.
| ILSS | MASC | |||||||
|---|---|---|---|---|---|---|---|---|
| R2 | F | β | t | R2 | F | β | t | |
| Overall Model | 0.04 | 1.56 | 0.16 | 8.94 | ||||
| Neurocog. | 0.16 | 1.83 | 0.35 | 3.76** | ||||
| DPAS | −0.06 | −0.79 | −0.12 | −1.53 | ||||
| Neurocog x DPAS | 0.03 | 0.42 | −0.02 | −0.25 | ||||
| Overall Model | 0.16 | 0.03 | 0.2 | 10.64 | ||||
| ToM | 0.14 | 1.68 | 0.4 | 4.74** | ||||
| DPAS | −0.05 | −0.64 | −0.18 | −2.01 | ||||
| ToM x DPAS | −0.003 | −0.04 | 0.1 | 0.96 | ||||
Note. Neurocog = Neurocognition; DPAS = Defeatist Performance Attitude Scale; ILSS = Independent Living Skills Survey; MASC = Maryland Assessment of Social Competence.
p < 0.01
p < 0.001
Figure 1.
Moderating effect of defeatist performance beliefs on the relationship between cognition and functional outcome. Moderation effects were not significant for any combination of variables shown. Note. NP = Neurocognition; ToM = Theory of Mind; ILSS = Independent Living Skills Survey; MASC = Maryland Assessment of Social Competence; Solid line = −1 SD below (Low Defeatist Performance Beliefs); Dash line = Mean (Moderate Defeatist Performance Beliefs); Dotted line = 1 SD above (High Defeatist Performance Beliefs).
3.3. Moderating effects of social disinterest attitudes
The interaction term for social disinterest attitudes and neurocognition did not account for significant variance in everyday functioning (Table 4). Similarly, the cross product for social disinterest attitudes and theory of mind did not significantly predict everyday functioning (Table 4).
Table 4.
Multiple regression for the prediction of functional outcome by cognition, social disinterest attitudes, and their interaction.
| ILSS | MASC | |||||||
|---|---|---|---|---|---|---|---|---|
| R2 | F | β | t | R2 | F | β | t | |
| Overall Model | 0.06 | 2.79 | 0.23 | 14.79 | ||||
| Neurocog. | 0.15 | 1.76 | 0.33 | 4.00** | ||||
| Social Dis. Att. | −0.14 | −1.52 | −0.26 | −3.67** | ||||
| Neurocog x Social Dis. Att. | 0.16 | 1.42 | 0.22 | 3.93** | ||||
| Overall Model | 0.04 | 2.02 | 0.24 | 16.7 | ||||
| ToM | 0.15 | 1.76 | 0.35 | 4.66** | ||||
| Social Dis. Att. | −0.11 | −1.16 | −0.21 | −3.05* | ||||
| ToM x Social Dis. Att. | −0.08 | −0.93 | 0.17 | 2.68* | ||||
Note. Neurocog = Neurocognition; Social Dis. Att. = Social Disinterest Attitudes; ILSS = Independent Living Skills Survey; MASC = Maryland Assessment of Social Competence.
p < 0.01
p < 0.001
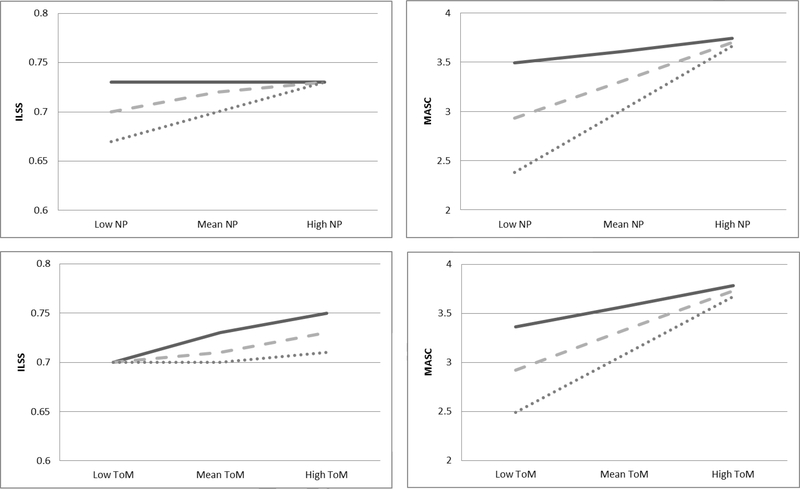
However, the cross product of these variables (e.g., social disinterest x neurocognition, social disinterest x theory of mind) did account for significant variance in social competence (β = .22, p < .001) even after accounting for the independent influences of social disinterest attitudes and neurocognition. For the group endorsing moderate or high levels of social disinterest attitude, scores of neurocognition were related to MASC scores (moderate: β =.33; p < .001; high: β =.56; p < .001), but this relationship was not significant for participants endorsing low levels of social disinterest attitudes (β =.11; p=.26; see Figure 2). This moderating effect was further examined using the Johnson–Neyman technique and links between neurocognition and social competence were significant once individuals exhibited moderate levels of social disinterest (M = 4.10; SE = 0.01).
Figure 2.
Moderating effect of social disinterest attitudes on the relationship between cognition and functional outcome. Significant moderation effects were not found for everyday functioning (ILSS) but were found for social competence (MASC) for both neurocognition and theory of mind. Note. NP = Neurocognition; ToM = Theory of Mind; ILSS = Independent Living Skills Survey; MASC = Maryland Assessment of Social Competence; Solid line = 1 SD below (Low Social Disinterest Attitudes); Dash line = Mean (Moderate Social Disinterest Attitudes); Dotted line = 1 SD above (High Social Disinterest Attitudes).
The moderating effects of social disinterest attitudes on the association between theory of mind and social competence was also significant (β = .16; p<.01; see Table 4). As was found for the moderation effects on neurocognition, theory of mind was significantly associated with MASC effectiveness only in participants with moderate and high levels of social disinterest attitudes (moderate: β =.35; p < .001; high: β =.52; p < .001). Importantly, this relationship was non-significant for participants at low levels of social disinterest attitudes (moderate: β =.18; p=.08; see Figure 2). When using the Johnson–Neyman technique, links between theory of mind and social competence were significant once individuals exhibited moderate levels of social disinterest (M = 3.62; SE = 0.03). These findings support our initial hypothesis that cognitive deficits are more likely to influence social competence in participants with more severe social disinterest attitudes.1,2
4. Discussion
The central aim of the current study was to determine how dysfunctional attitudes influence the associations between cognitive processes (i.e., neurocognition and theory of mind) and functional outcomes in schizophrenia. While there has been consistent support for associations between neurocognition, theory of mind, dysfunctional attitudes, and functional outcome, this is first study to examine how interactions among these specific factors (e.g., cognition, dysfunctional attitudes) may potentially influence everyday and social functioning. Small to medium associations were found among these variables, findings that are consistent with prior literature (Horan et al., 2010; Kiwanuka et al., 2014) . Neurocognition was modestly correlated with everyday functioning and social competence while theory of mind and both types of dysfunctional attitudes (e.g., defeatist performance beliefs, social disinterest attitudes) were only associated with social competence. Only partial support was found for the hypothesis that dysfunctional attitudes and cognition interact to predict functional outcomes in schizophrenia. Social disinterest attitudes significantly moderated associations between neurocognitive and social cognitive abilities and social competence, such that greater impairment in cognitive abilities were only related with social competence deficits in participants with more severe social disinterest attitudes. However, social disinterest attitudes did not significantly moderate relationships between cognitive abilities and everyday functioning, and the interaction between defeatist performance beliefs and cognitive abilities did not significantly predict everyday functioning or social competence. The specificity of the moderation findings may have important implications for treatment targets and identifying which patients are most likely to benefit from different treatments.
Research on factors associated with poor functioning in schizophrenia has largely focused on mediation models (i.e., cognition ➔ dysfunctional attitudes ➔ amotivation ➔ functioning; Green et al., 2012; Horan et al., 2010; Quinlan et al., 2014). Modest associations between more distal factors in these models (e.g., cognition and functioning) can be explained by mediator variables. The findings in the present study suggest that modest associations between cognition and functioning may also be explained by dysfunctional attitude moderator variables. Previous studies have suggested that an individual must first possess adequate neurocognitive and social cognitive abilities before they can successfully pursue real-world functional goals (Green et al., 2004; Harvey and Strassnig, 2012). In the present study, associations between cognitive abilities and social competence, defined here as the ability, rather than expectancy, to resolve interpersonal conflicts through successful communication, were found only in individuals with more severe social disinterest attitudes, but not in participants with low social disinterest attitudes. This finding is not consistent with the notion that cognitive abilities are “necessary, but not sufficient” for functioning (Green et al., 2004; Harvey and Strassnig, 2012), at least with regard to social functioning. The finding that neurocognition and theory of mind has no effect on social competence when social disinterest is low suggest that greater interest in socialization may somehow compensate for the deleterious effects of cognitive deficits on social skills. That is, greater interest and motivation to engage in social interactions may result in more frequent practice and learning in social experiences which can improve social competence and thereby compensate for cognitive deficits. Lastly, greater interest in socialization may lead to more resilient behaviors when confronted with interpersonal problems, as in the role play task used to measure social competence in the present study.
Moderation effects were found for social disinterest but not defeatist performance beliefs and social disinterest moderation was specific to social competence. Several factors may explain this specificity for social disinterest beliefs. First, beliefs specifically related to socializing likely have a stronger relationship with social competence than more general everyday functioning. In addition, defeatist performance beliefs and social disinterest attitudes may be more distally related to everyday functioning, whereas social disinterest attitudes are likely more proximally associated with performance based social competence measures. There may be intervening variables (e.g., negative symptoms, financial status, amount of social support) connecting dysfunctional beliefs to everyday functioning. Everyday functioning is also inherently a multifaceted construct, which is reflected by the ten subscales of the ILSS everyday functioning measure. Given this, it is surprising that the more generalized defeatist performance beliefs were not strongly associated with general everyday functioning on the ILSS and did not show moderation. It is possible that more specific defeatist beliefs about different areas of functioning (e.g., specific to work, school, or maintaining housing) would show stronger associations with specific domains of functioning. Despite findings that dysfunctional attitudes are associated with negative symptoms (Campellone et al., 2016; Grant and Beck, 2010), we did not find significant moderation for negative symptoms in exploratory analyses (see Footnote 1), suggesting a unique contribution of attitudes on the association between cognition and functioning. The specificity of the findings that only social disinterest attitudes moderated relations between cognition and social functioning signals the importance of contrasting which beliefs and which individuals to target in psychosocial treatment.
The present findings suggest that social disinterest attitudes are viable treatment targets to ameliorate social functioning deficits in schizophrenia. We (Granholm et al., 2017, 2014) found that reductions in social disinterest beliefs in a relatively new group therapy intervention, cognitive-behavioral social skills training (CBSST), mediated the treatment effect on improvement in social competence. Higher interest and motivation for social engagement may lead to greater practice in social experiences, whereas participants with better cognitive abilities may be able to develop social competence despite low social interest and motivation. It is also important to note that the combination of both poor cognitive ability and more severe asocial beliefs was associated with greater social functioning impairment. This may indicate that participants with both poor cognition and greater social disinterest are most likely to benefit from psychosocial treatments like cognitive-behavioral therapy (CBT) or CBSST focused on reducing social disinterest attitudes. Importantly, a treatment targeting basic neurocognitive abilities or combined CBT and cognitive remediation in individuals with more severe asocial beliefs could also improve both social motivation and competence and ultimately impact real world functioning.
Several limitations are worth noting. The current study was comprised of a sample of community dwelling participants who volunteered for a 9-month psychosocial treatment outcome study for schizophrenia, thus possibly influencing the generalizability of the findings. As with any cross-sectional study, establishing a temporal precedence and causation was not possible. Future work with longitudinal data would be needed to replicate these findings. This study only included one social cognition measure (e.g., theory of mind) and findings may differ for other domains of social cognition (e.g., affective perception, attribution style bias). Similarly, different measures of functioning might yield different results (e.g., Social Functioning Scale, Birchwood et al., 1990; Specific Levels of Functioning, Schneider and Streuening, 1983). Lastly, a significant portion of variance in functioning remain unexplained in the current study; thus, future models would benefit by including other important predictors of functional outcomes.
Overall, our findings contribute to the extant literature on the meaningful role of dysfunctional attitudes on functional outcomes. Our findings suggest that the beliefs or attitudes that individuals maintain regarding socialization are viable treatment targets for cognitive therapy to augment social functioning in participants with schizophrenia. Concurrently, the specificity of findings also highlights which dysfunctional attitudes and which individuals to target: social disinterest attitudes rather than defeatist beliefs may be more effective to improve social functioning and participants with both poorer cognitive abilities and more severe social disinterest attitudes may be most in need of interventions targeting social disinterest attitudes. This study suggests social disinterest attitudes can be targeted to increase social motivation and compensate for neurocognitive and theory of mind impairments. Consistent with the cognitive model of schizophrenia (Grant and Beck, 2009), challenging and decreasing social disinterest attitudes in cognitive therapy may lead to improvements in social functioning even in participants with schizophrenia with severe cognitive deficits.
Highlights.
Interactions among common factors (e.g., neurocognition, theory of mind, defeatist performance beliefs, and social disinterest attitudes) of everyday and social functioning were examined.
Social disinterest attitudes significantly moderated relationships between neurocognitive and social cognitive abilities and social competence.
The specificity of the moderation findings may have important implications for treatment targets by identifying which patients are most likely to benefit from different treatments.
Acknowledgements
The authors would like to thank the study participants, and lab members for their aid in collecting and processing data.
Role of funding source
This study was supported by the Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research and Development Service, and the National Institute of Mental Health of the National Institutes of Health (R01MH071410). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veterans Affairs or National Institutes of Health.
Footnotes
Conflicts of interest
Dr. Granholm has an equity interest in Granholm Consulting, Inc., a company that may potentially benefit from the research results as he receives income from the company for CBSST workshops and consulting. The terms of this arrangement have been reviewed and approved by the University of California, San Diego in accordance with its conflict of interest policies.
Footnote 1: Dysfunctional attitudes are associated with negative symptoms. Given this, additional analyses were conducted to test the moderating effects of negative symptoms (e.g., experiential and expressive) on the relationship of cognition (e.g., neurocognition and theory of mind) to functional outcome. Consistent with the statistical procedures for defeatist performance beliefs and social disinterest attitudes, separate sets of linear regression models were conducted for experiential and expressive negative symptoms (as the moderators). No permutation of the interaction terms between negative symptoms (e.g., experiential and expressive) and cognition (i.e., neurocognition and social cognition) accounted for significant variance in everyday functioning or social competence.
Footnote 2: We also compared individuals living in Assisted Housing versus individuals living Independently on dysfunctional attitude variables. These groups did not significantly differ on defeatist performance beliefs, t (144) = .45, p = .65. They also did not significantly differ on social disinterest attitudes, t (144) = −.12, p = .90.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addington J, Young J, Addington D, 2003. Social outcome in early psychosis. Psychol. Med 33, 1119–1124. 10.1017/S0033291703007815 [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG, 1991. Multiple regression: Testing and interpreting interactions. Sage Publications, Newbury Park, CA. [Google Scholar]
- Bellack AS, Brown CH, Thomas-Lohrman S, 2006. Psychometric characteristics of role-play assessments of social skill in schizophrenia. Behav. Ther 37, 339–352. 10.1016/j.beth.2006.01.005 [DOI] [PubMed] [Google Scholar]
- Benedict B, Groninger L, Dobraski M, Shpritz B, B Benedict RH, 1996. Revision of the brief visuospatial memory test: studies of normal performance, reliability, and validity. Psychol. Assess 8, 145–153. 10.1037/1040-3590.8.2.145 [DOI] [Google Scholar]
- Benedict RHB, Schretlen D, Groninger L, Brandt J, 1998. Hopkins Verbal Learning Test-Revised: normative data and analysis of inter-form and test-retest reliability. Clin. Neuropsychol 12, 43–55. 10.1076/clin.12.1.43.1726 [DOI] [Google Scholar]
- Bergh S, Hjorthøj C, Sørensen HJ, Fagerlund B, Austin S, Secher RG, Jepsen JR, Nordentoft M, 2016. Predictors and longitudinal course of cognitive functioning in schizophrenia spectrum disorders, 10 years after baseline: The OPUS study. Schizophr. Res 175, 57–63. 10.1016/j.schres.2016.03.025 [DOI] [PubMed] [Google Scholar]
- Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S, 1990. The Social Functioning Scale: The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br. J. Psychiatry 157, 853–859. 10.1192/bjp.157.6.853 [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Gangestad SW, Brown SA, Horan WP, Blanchard SW; Brown SA; Horan WP, J.J G, 2000. Hedonic capacity and schizotypy revisited: A taxometric analysis of social anhedonia. J. Abnorm. Psychol 109, 87–95. 10.1037//0021-843X.109.1.87 [DOI] [PubMed] [Google Scholar]
- Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, Heaton RK, Harvey PD, 2008. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol. Psychiatry 63, 505–511. 10.1016/j.biopsych.2007.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brekke J, Kay DD, Lee KS, Green MF, 2005. Biosocial pathways to functional outcome in schizophrenia. Schizophr. Res 80, 213–225. 10.1016/j.schres.2005.07.008 [DOI] [PubMed] [Google Scholar]
- Brown LH, Silvia PJ, Myin-Germeys I, Kwapil TR, 2007. When the need to belong goes wrong: The expression of social anhedonia and social anxiety in daily life. Psychol. Sci 18, 778–782. 10.1111/j.1467-9280.2007.01978.x [DOI] [PubMed] [Google Scholar]
- Brüne M, Abdel-Hamid M, Lehmkämper C, Sonntag C, 2007. Mental state attribution, neurocognitive functioning, and psychopathology: What predicts poor social competence in schizophrenia best? Schizophr. Res 92, 151–159. 10.1016/j.schres.2007.01.006 [DOI] [PubMed] [Google Scholar]
- Campellone TR, Sanchez AH, Kring AM, 2016. Defeatist performance beliefs, negative symptoms, and functional outcome in schizophrenia: a meta-analytic review. Schizophr. Bull 42, 1343–1352. 10.1093/schbul/sbw026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane DB, Olinger LJ, Gotlib IH, Kuiper NA, 1986. Factor structure of the dysfunctional attitude scale in a student population. J. Clin. Psychol 42, 307–309. [DOI] [Google Scholar]
- Couture SM, Granholm EL, Fish SC, 2011. A path model investigation of neurocognition, theory of mind, social competence, negative symptoms and real-world functioning in schizophrenia. Schizophr. Res 125, 152–160. 10.1016/j.schres.2010.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis D, Kaplan E, Kramer J, 2001. Delis-Kaplan executive function system (D-KEFS). Can. J. Sch. Psychol 20, 117–128. 10.1177/0829573506295469 [DOI] [Google Scholar]
- Fett A-KJ, Viechtbauer W, Dominguez M-G, Penn DL, van Os J, Krabbendam L, 2011. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci. Biobehav. Rev 35, 573–588. 10.1016/j.neubiorev.2010.07.001 [DOI] [PubMed] [Google Scholar]
- First MB et, Spitzer RL, Gibbon M, Williams JBW, 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders Research Version, Patient Edition with Psychotic Screen (SCID-I/P), Biometrics Research, New York State Psychiatric Institute, New York. [Google Scholar]
- Granholm E, Ben-Zeev D, Fulford D, Swendsen J, 2013a. Ecological Momentary Assessment of social functioning in schizophrenia: impact of performance appraisals and affect on social interactions. Schizophr. Res 145, 120–124. 10.1016/j.schres.2013.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Ben-Zeev D, Link PC, 2009. Social disinterest attitudes and group cognitive-behavioral social skills training for functional disability in schizophrenia. Schizophr. Bull 35, 874–83. 10.1093/schbul/sbp072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Holden J, Link PC, McQuaid JR, 2014. Randomized clinical trial of cognitive behavioral social skills training for schizophrenia: Improvement in functioning and experiential negative symptoms. J. Consult. Clin. Psychol 82, 1173–1185. 10.1037/a0037098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Holden J, Link PC, McQuaid JR, Jeste DV, 2013b. Randomized controlled trial of cognitive behavioral social skills training for older consumers with schizophrenia: defeatist performance attitudes and functional outcome. Am. J. Geriatr. Psychiatry 21, 251–262. 10.1097/JGP.0b013e31823e2f70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Holden J, Worley M, 2017. Improvement in negative symptoms and functioning in cognitive-behavioral social skills training for schizophrenia: mediation by defeatist performance attitudes and asocial beliefs. Schizophr. Bull 44, 653–661. 10.1093/schbul/sbx099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Ruiz I, Gallegos-Rodriguez Y, Holden J, Link PC, 2016. Pupillary responses as a biomarker of diminished effort associated with defeatist attitudes and negative symptoms in schizophrenia. Biol. Psychiatry 80, 581–588. 10.1016/j.biopsych.2015.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant PM, Beck AT, 2010. Asocial beliefs as predictors of asocial behavior in schizophrenia. Psychiatry Res. 177, 65–70. 10.1016/j.psychres.2010.01.005 [DOI] [PubMed] [Google Scholar]
- Grant PM, Beck AT, 2009. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr. Bull 35, 798–806. 10.1093/schbul/sbn008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MF, Hellemann G, Horan WP, Lee J, Wynn JK, 2012. From perception to functional outcome in schizophrenia: Modeling the role of ability and motivation. Arch. Gen. Psychiatry 69, 1216–1224. 10.1001/archgenpsychiatry.2012.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J, 2000. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr. Bull 26, 119–136. 10.1093/oxfordjournals.schbul.a033430 [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Heaton RK, 2004. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res 72, 41–51. 10.1016/j.schres.2004.09.009 [DOI] [PubMed] [Google Scholar]
- Greig TC, Bryson GJ, Bell MD, 2004. Theory of mind performance in schizophrenia: diagnostic, symptom, and neuropsychological correlates. J. Nerv. Ment. Dis 192, 12–18. 10.1097/01.nmd.0000105995.67947.fc [DOI] [PubMed] [Google Scholar]
- Harvey PD, Heaton RK, Carpenter WT, Green MF, Gold JM, Schoenbaum M, 2012. Functional impairment in people with schizophrenia: Focus on employability and eligibility for disability compensation. Schizophr. Res 140, 1–8. 10.1016/j.schres.2012.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, Strassnig M, 2012. Predicting the severity of everyday functional disability in people with schizophrenia: Cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. 11(2), 73–79. 10.1016/j.wpsyc.2012.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, 2013. Introduction to meditaion, moderation, and conditional process analysis: A regression-based approach, Guilford Press, New York: 10.5539/ass.v11n9p207 [DOI] [Google Scholar]
- Horan WP, Rassovsky Y, Kern RS, Lee J, Wynn JK, Green MF, 2010. Further support for the role of dysfunctional attitudes in models of real-world functioning in schizophrenia. J. Psychiatr. Res 44, 499–505. 10.1016/j.jpsychires.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalin M, Kaplan S, Gould F, Pinkham AE, Penn DL, Harvey PD, 2015. Social cognition, social competence, negative symptoms and social outcomes: Inter-relationships in people with schizophrenia. J. Psychiatr. Res 68, 254–260. 10.1016/j.jpsychires.2015.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay S, Fiszbein A, Opler L, 1987. The Positive and Negative Syndrome Scale (PANSS) for Schizophrenia. Schizophr. Bull 13, 261–276. 10.1093/schbul/13.2.261 [DOI] [PubMed] [Google Scholar]
- Keefe RSE, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L, 2004. The Brief Assessment of Cognition in Schizophrenia: Reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr. Res 68, 283–297. 10.1016/j.schres.2003.09.011 [DOI] [PubMed] [Google Scholar]
- Kiwanuka JN, Strauss GP, McMahon RP, Gold JM, 2014. Psychological predictors of functional outcome in people with schizophrenia. Schizophr. Res 157, 299–304. 10.1016/j.schres.2014.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam BY, Raine A, Lee TM, 2014. The relationship between neurocognition and symptomatology in people with schizophrenia: social cognition as the mediator. BMC Psychiatry. 14, 138 10.1186/1471-244X-14-138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leak GK, 1991. An examination of the construct validity of the Social Anhedonia Scale. J. Pers. Assess 56(1), 84–95. 10.1207/s15327752jpa5601_8 [DOI] [PubMed] [Google Scholar]
- Leifker FR, Bowie CR, Harvey PD, 2009. Determinants of everyday outcomes in schizophrenia: The influences of cognitive impairment, functional capacity, and symptoms. Schizophr. Res 115, 82–87. 10.1016/j.schres.2009.09.004 [DOI] [PubMed] [Google Scholar]
- Liberman RP, Kopelowicz A, 2005. Recovery from schizophrenia: a concept in search of research. Psychiatr. Serv 56, 735–742. 10.1176/appi.ps.56.6.735 [DOI] [PubMed] [Google Scholar]
- Luther L, Salyers MP, Firmin RL, Marggraf MP, Davis B, Minor KS, 2016. Additional support for the cognitive model of schizophrenia: Evidence of elevated defeatist beliefs in schizotypy. Compr. Psychiatry 68, 40–47. 10.1016/j.comppsych.2016.03.006 [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Fenton WS, Frese FJ, Gold JM, Goldberg T, Heaton RK, Keefe RSE, Kraemer H, Mesholam-Gately R, Seidman LJ, Stover E, Weinberger DR, Young AS, Zalcman S, Marder SR, 2008. The MATRICS consensus cognitive battery, part 1: Test selection, reliability, and validity. Am. J. Psychiatry 165, 203–213. 10.1176/appi.ajp.2007.07010042 [DOI] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, 2006. Neurocognitive and social cognitive predictors of interpersonal skill in schizophrenia. Psychiatry Res. 143, 167–178. 10.1016/j.psychres.2005.09.005 [DOI] [PubMed] [Google Scholar]
- Quinlan T, Roesch S, Granholm E, 2014. The role of dysfunctional attitudes in models of negative symptoms and functioning in schizophrenia. Schizophr. Res 157, 182–189. 10.1016/j.schres.2014.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rector NA, Beck AT, Stolar N, 2005. The negative symptoms of schizophrenia: A cognitive perspective. Can. J. Psychiatry 50, 247–257. [DOI] [PubMed] [Google Scholar]
- Reitan RM, Wolfson D, 2009. The Halstead-Reitan Neuropsychological Test Battery for Adults — Theoretical, Methodological, and Validational Bases, in: Neuropsychological Assessment of Neuropsychiatric and Neuromedical Disorders. 1, 3–25. [Google Scholar]
- Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM, 2004. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am. J. Psychiatry 161, 473–479. 10.1176/appi.ajp.161.3.473 [DOI] [PubMed] [Google Scholar]
- Schmidt SJ, Mueller DR, Roder V, 2011. Social cognition as a mediator variable between neurocognition and functional outcome in schizophrenia: Empirical review and new results by structural equation modeling. Schizophr. Bull. 37(suppl_2), S41–S54. 10.1093/schbul/sbr079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider LC, Streuening EL, 1983. Specific level of functioning scale: A behavioral rating scale for assessing the mentally ill. Soc. Work Res. Abstr 19, 9–21. 10.1037/t47303-000 [DOI] [PubMed] [Google Scholar]
- Strassnig MT, Raykov T, O’Gorman C, Bowie CR, Sabbag S, Durand D, Patterson TL, Pinkham A, Penn DL, Harvey PD, 2015. Determinants of different aspects of everyday outcome in schizophrenia: The roles of negative symptoms, cognition, and functional capacity. Schizophr. Res 165, 76–82. 10.1016/j.schres.2015.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas EC, Luther L, Zullo L, Beck AT, Grant PM, 2017. From neurocognition to community participation in serious mental illness: the intermediary role of dysfunctional attitudes and motivation. Psychol. Med. 47, 822–836. 10.1017/S0033291716003019 [DOI] [PubMed] [Google Scholar]
- Vauth R, Rüsch N, Wirtz M, Corrigan PW, 2004. Does social cognition influence the relation between neurocognitive deficits and vocational functioning in schizophrenia? Psychiatry Res. 128, 155–165. 10.1016/j.psychres.2004.05.018 [DOI] [PubMed] [Google Scholar]
- Ventura J, Subotnik KL, Ered A, Gretchen-Doorly D, Hellemann GS, Vaskinn A, Nuechterlein KH, 2014. The relationship of attitudinal beliefs to negative symptoms, neurocognition, and daily functioning in recent-onset schizophrenia. Schizophr. Bull 40, 1308–1318. 10.1093/schbul/sbu002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J, Subotnik KL, Guzik LH, Hellemann GS, Gitlin MJ, Wood RC, Nuechterlein KH, 2011. Remission and recovery during the first outpatient year of the early course of schizophrenia. Schizophr. Res 132, 18–23. 10.1016/j.schres.2011.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace CJ, Liberman RP, Tauber R, Wallace J, 2000. The Independent Living Skills Survey: A comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophr. Bull 26, 631–658. 10.1093/oxfordjournals.schbul.a033483 [DOI] [PubMed] [Google Scholar]
- Wechsler D, 1997a. Wechsler Memory Scale (Third Ed.). San Antonio, TX: Psychol. Corp. [Google Scholar]
- Wechsler D, 1997bWAIS-III administration and scoring manual, The Psychological Corporation, San Antonio, TX: 10.1177/1073191102009001003 [DOI] [Google Scholar]
- Weissman AN, 1979. The Dysfunctional Attitude Scale: A Validation Study. Diss. Abstr. Int. Sect. B. Sci. Eng 40, 1389–1390. [Google Scholar]