Abstract
BACKGROUND:
The US Centers for Disease Control and Prevention (CDC) promotes school-based strategies to increase physical activity (PA). Implementation feasibility and effect of these interventions on cardiovascular fitness (CVF) is unknown.
METHODS:
Forty-nine low-SES schools were randomly assigned to either (1) continue routine PA programs (N=24 schools, 2399 students) or (2) implement 4 CDC-based PA strategies (N=25 schools, 2495 students). CVF assessed by PACER (Progressive Aerobic Cardiovascular Endurance Run) was obtained at the beginning and end of the school year. A post-study questionnaire was administered at each school to assess adherence.
RESULTS:
Overall, PACER z-scores were not augmented by CDC-based PA strategies. In boys, PACER z-scores increased similarly in both intervention and control schools. In girls, increased mean PACER z-score was greater in control schools (p < .01). Fifty-two percent of intervention school’s staff reported inability to implement or sustain 4 CDC-based PA strategies.
CONCLUSIONS:
Planned implementation of school-based CDC PA strategies did not increase CVF compared to routine PA programming. Lack of efficacy in girls suggests need for sex-specific targeted strategies. These findings highlight limited efficacy of CDC-based PA recommendations alone in low-SES schools. Schools may require additional support to successfully implement recommendations and meaningfully affect health outcomes.
Keywords: physical activity, fitness, children, schools
Routine physical activity improves cardiovascular fitness (CVF) and reduces the risk for obesity, cardiovascular disease, Type 2 diabetes and overall mortality.1,2 CVF is an independent risk factor for insulin resistance, distinct from BMI.3–5 In addition to the numerous health benefits, physical activity improves academic engagement and achievement in school settings.6 The 2008 Physical Activity Guidelines include a recommendation that children participate in one or more hours of moderate to vigorous physical activity daily. Despite these recommendations and the known benefits of physical activity,7 more than half of children ages 6–11 years and more than 90% of adolescents fail to meet the current recommendations.8 Levels of physical activity decrease with age and girls are less likely to meet physical activity recommendations than boys across all age groups.8 Like obesity, the burden of co-morbidities associated with low physical activity are not equally distributed across society, with minorities and individuals of low socio-economic status (SES) being disproportionately affected. In adults, individuals from low SES have lower rates of physical activity; reports of the association between low SES and low physical activity in childhood are variable.9–12
Given high rates of physical inactivity among US youth and the association of physical inactivity with disease burden and premature death, public health interventions to increase physical activity are needed.13 Schools provide attractive opportunities to reach children and apply interventions across ages, sexes and races/ethnicities. Accordingly, the US Centers for Disease Control and Prevention (CDC) promotes school-based strategies to increase physical activity including the implementation of high quality physical education classes and increased opportunities for students to be physically active through school settings.14 Current evidence from research studies of focused school-based interventions shows modest improvements in physical activity rates and CVF measured using maximum oxygen uptake (VO2 max) as an indicator of CVF.15
Since CVF assessment using laboratory methods is labor intensive and impractical in community settings, including schools, feasible systems of measuring CVF on the population level are needed. We previously demonstrated a strong correlation between the school-environment PACER test (Progressive Aerobic Cardiovascular Endurance Run) and maximal VO2 measured by treadmill test (r = .83, p < .0001).16 PACER is a 20 meter shuttle run where the time allowed for students to complete the run gradually decreases until a student is unable to complete the lap in the allotted time. The entire class performs that test at the same time, so that all students are included. Scores are provided based on the total number of laps the student was able to complete successfully. In this study we evaluated the feasibility and effects of a large-scale implementation program for CDC recommended school based physical activity strategies on CVF measured by PACER in low SES Wisconsin schools.
METHODS
Participants
Low SES Wisconsin public schools defined as having 40% or more of students qualifying for free or reduced lunch, were recruited by the Wisconsin Department of Public Instruction to participate in the study. Low SES schools were studied in order to highlight potential impact and benefit of intervention in schools with fewer resources. Students ranged from grade 3 through 8.
Instrumentation
Stratified randomization by geography was used to categorize the 49 participating schools as either intervention or control schools. Principals and physical education teachers of intervention schools (N=25 schools, 2495 students) agreed to attempt implementation of 4 CDC recommended evidenced-based strategies to promote increased physical activity in schools including: (1) increasing the amount of time spent in moderate to vigorous physical activity in physical education class, (2) encouraging active classroom breaks, (3) providing organized physical activity opportunities during recess, and (4) providing organized physical activity opportunities before and after school. These “core four” physical activity strategies had previously been shown in a pilot study to increase students’ mean daily steps from 9,849 to 11,148 (p < .01) after implementation in separate Wisconsin school settings. Teachers from all schools attended trainings on Core-4 strategies and implementation. Control schools (N=24 schools, 2399 students) continued with prior routine physical activity programming and did not receive any additional instruction or training on the “core four” physical activity strategies. The Wisconsin Department of Public Instruction provided technical assistance and financial support to all participating schools. Physical education teachers from intervention schools received professional development and consultation to support implementation of the “core four” physical activity strategies.
Procedure
The PACER, a component of Fitnessgram®, is a multistage progressive 20-meter shuttle run. Participants run back and forth along a 20-meter course, and each minute the pace required to run the 20 meters increases. The pace is set from a pre-recorded audio file. The initial running speed is 8.5 km/hour, and the speed increases by 0.5 km/hour every minute. The test is finished when the participant fails to complete the 20-meter run in the allotted time twice.17 The PACER is expressed as number of laps completed. All schools performed PACER testing at baseline and repeat PACER testing at the beginning and end of each school year. Schools submitted data either with paper reports or by electronic submission. To account for expected age-related increases in CVF, absolute PACER was converted to PACER z-scores for age and sex in addition to analyzing PACER data by absolute PACER score. The reference values for the z-scores were derived from previously collected large population study of 20,631 Wisconsin school children.17 The PACER score has been shown to correlate closely with VO2 max, as well as insulin resistance.16
All schools performed PACER testing at baseline and repeat PACER testing at the end of the school year as part of the regular physical education class. Schools submitted data either with paper reports or by electronic submission at the start and end of the school year. To account for expected age-related increases in CVF, absolute PACER was converted to PACER z-scores (PACER standard deviation score accounting for age and sex in addition to analyzing PACER data by absolute PACER score). This conversion was derived from previously collected data on 20,631 Wisconsin school children.18 Knowing that implementation fidelity was an important part of this study analysis, at the conclusion of the study, physical education teachers at intervention schools completed a questionnaire to self-report implementation success with each of the 4 PA strategies. Qualitative assessment of barriers to implementation was also assessed.
Data Analysis
All outcome measures were summarized in terms of means and standard errors. Linear mixed effects modeling with school-specific random effects were conducted to perform the comparisons of outcome measures at baseline between the two study arms. Age, study arm, sex and study-arm-times-sex interaction effects were included as covariates in the model. Analogously, a linear mixed effects model was used to evaluate changes from the baseline to the post-test assessment within and between study arms. Model assumptions were verified by examining residual plots. The intent-to-treat population was used as the primary analysis population. A sensitivity analysis was conducted by comparing the results analyzed using the intent-to-treat population to those obtained using only intervention schools reporting full compliance on post-study survey. All reported p-values are two-sided and p < .05 was used to define statistical significance. Data analysis was conducted using SAS software (SAS Institute, Cary NC) version 9.3.
RESULTS
Forty-nine schools participated in the study with a total of 4894 students. Intervention and control schools were similar at baseline with no statistical differences between sex, ethnicity, or baseline PACER score representing number of labs completed (Table 1). Girls in non-intervention schools had significantly higher mean baseline PACER scores compared to girls in intervention schools. At baseline, age, sex and ethnicity were all found to have significant effect on PACER. Specifically, older age, being male and non-Hispanic ethnicity were all associated with increased fitness at baseline and were consistent with published data.19
Table 1:
Baseline Demographics
| Intervention School (N=25 Schools, 2495 Students) |
Control Schools (N=24 Schools, 2399 Students) |
p-value | |
|---|---|---|---|
| Age in years (mean ± SE) | 11.1 ± 0.02 | 11.2 ± 0.02 | <.01 |
| % Females | 48.9 ± 1.00 | 46.0 ± 1.03 | .06 |
| % Hispanic | 23.1 ± 0.91 | 21.5 ± 0.86 | .22 |
| PACER (mean ± SE) | |||
| All students | 26.3 ± 0.3 | 26.6 ± 0.3 | .47 |
| Males | 30.1 ± 0.4 | 29.0 ± 0.4 | .09 |
| Females | 22.6 ± 0.4 | 24.1 ± 0.4 | .03 |
| BMI (mean ± SE) | 22.0 ± 0.2 | 21.7 ± 0.1 | .21 |
| BMI z-score (mean ± SE) | 1.00 ± 0.04 | 0.91 ± 0.02 | .09 |
Study results are shown in Table 2. Mean PACER and PACER z-scores increased from baseline in both groups. However, a greater CVF change in control vs. intervention schools (p < .001) indicated no additional benefit of CDC-based physical activity interventions related to education on these policies and their implementation alone.
Table 2:
Change in PACER and PACER Z-score from Baseline
| Intervention | p-value1 | Control | p-value2 | p-value3 | |
|---|---|---|---|---|---|
|
PACER (mean ± SE) |
|||||
| All students | 4.7 ± 0.4 | <.001 | 5.8 ± 0.4 | <.001 | .05 |
| Males | 9.7 ± 0.5 | <.001 | 9.2 ± 0.5 | <.001 | .53 |
| Females | −0.1 ± 0.5 | .796 | 2.5 ± 0.6 | <.001 | .002 |
|
PACER z-score (mean ± SE) |
|||||
| All students | +0.09 ± 0.02 | <.001 | 0.19 ± 0.02 | <.001 | <.001 |
| Males | +0.14 ± 0.03 | <.001 | +0.16 ± 0.03 | <.001 | .69 |
| Females | +0.04 ± 0.03 | .155 | +0.22 ± 0.03 | <.001 | <.001 |
p-value – Change from baseline in intervention schools
p-value – Change from baseline in control schools
p-value – Change from baseline intervention compared to control schools
A significant interaction between intervention effects and sex was observed (Figures 1 and 2). In girls from intervention schools, there was no significant change from baseline in mean PACER (p = .796) or PACER z-score (p = .692), while in girls from control schools, a small increase in mean PACER and PACER z-score was observed (PACER +2.5 ± 0.6, p < .001, and PACER z-score +0.22 ± 0.03, p < .001), as shown in figure 2. In boys, the mean PACER and PACER z-score increased compared to baseline in both intervention and control schools. When comparing the magnitude of increases in boys’ mean PACER and PACER z-scores between intervention and control schools, no statistically significant differences were detected (p = .53 and p = .69). In the intervention schools, there was no significant correlation between change in mean PACER or PACER z-score and schools’ self-reported compliance level.
Figure 1:
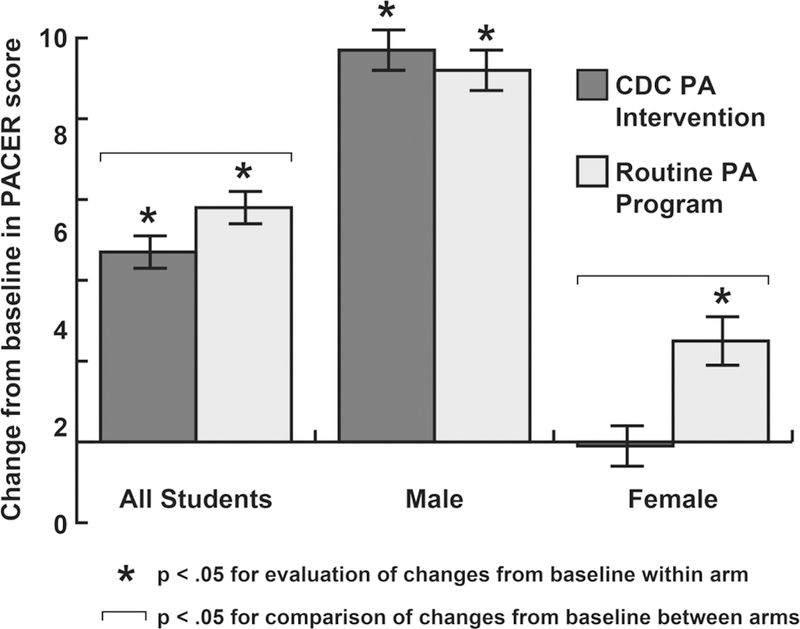
Change in PACER Scores, Overall and Stratified by Sex
Figure 2:
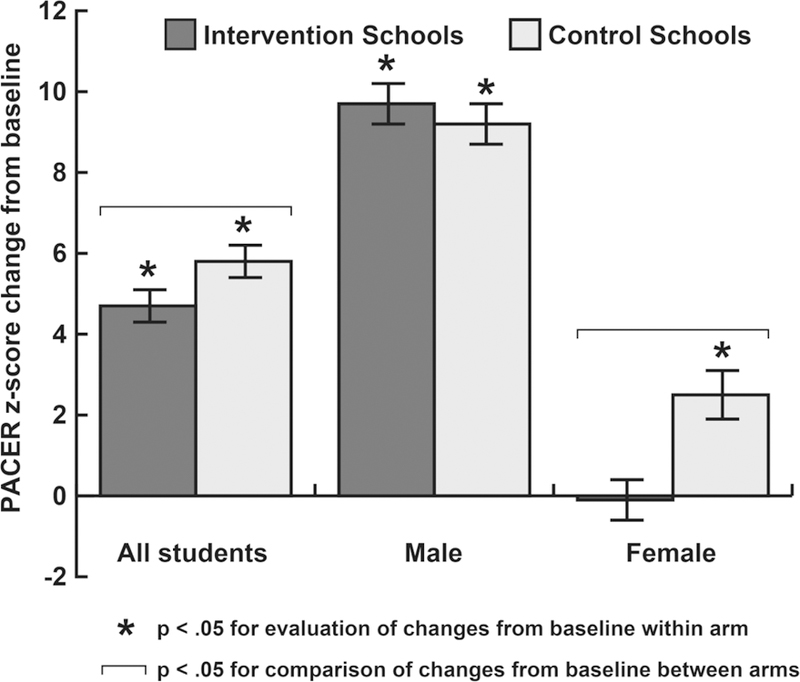
Change in PACER Scores, Overall and Stratified by Sex
Adherence to Core-4 strategies implementation was specifically examined with a post-study questionnaire filled out by the lead physical education teacher at each school. There were 13 schools that completed all 4 strategies, 8 completed only 2 strategies, and 4 completed only 1 strategy. A subgroup analysis was performed excluding schools within the physical activity intervention arm that reported less than 100% compliance with implementation of Core-4 strategies (N=13 schools). This subgroup analysis revealed no differences in fitness changes associated with Core-4 exposure compared to the intent-to-treat analysis used above.
DISCUSSION
A program designed for large-scale implementation of CDC-recommended strategies to increase physical activity did not augment changes in fitness levels of students in Wisconsin low SES schools compared to routine physical activity programming. Overall, students achieved age-related increase in CVF over the 9-month study period whether in intervention or control schools. The absence of intervention effect could be due to insufficient increases in physical activity levels from the intervention, implementation challenges, or both. Since CDC “core four” physical activity strategies had previously been shown to increase students’ mean daily steps from 9,849 to 11,148 (p < .01) in similar settings, one plausible explanation is that changes in physical activity resulting from CDC strategies are insufficient to improve cardiovascular fitness. Further studies, which include direct assessment of CVF, are needed to determine the amount and type of physical activity needed to improve childhood fitness and health.16
Survey data collected from participating intervention schools indicated that despite best efforts many schools were not able to implement all of the four physical activity strategies. That being said, analyses of “all” schools and of “only schools that successfully completed all 4 strategies” did not reveal any differences. While variation in intervention adherence could clearly lead to underestimation of the potential impact of CDC physical activity interventions, it also highlights factors that influence the true effectiveness of an “evidence-based” program applied in the real world setting. Barriers identified to implementation of all CDC recommendations – time constraints, inadequate staffing and insufficient funding – suggest that successful implementation of CDC recommended physical activity strategies in schools requires additional staffing and increased funding. Nearly all physical education teachers reported successful implementation of increased time spent in moderate to vigorous activity in physical education class. However, this strategy, which appears to be the easiest to implement, would be expected to have limited effectiveness when students do not participate in daily physical education class. Thus, policy initiatives to increase physical education class frequency and funding for after school programs are likely needed to enable successful implementation of CDC physical activity strategies.
Interestingly, when analyzing the data by sex, there was an unexpected and paradoxical negative effect observed in girls exposed to the CDC-based physical activity intervention. Male students, on the other hand, showed a positive change in fitness that was similar in magnitude regardless of intervention. Possible explanations for this sex discrepancy include a negative perception of the intervention by girls resulting in decreased physical activity and/or a negative perception of PACER testing by girls in intervention schools resulting in decreased effort and leading to inaccurate CVF results. Such a response may be consistent with prior research demonstrating that girls at this age tend to opt out of competitive sports and activities.20,21 Additional research is needed to determine whether this observation persists over a longer study period and, if so, to inform physical activity interventions that benefit all children, especially those at high risk for physical inactivity and low fitness.
Strength and Limitations
Strengths of this report include a randomized controlled study of a large number of children designed to assess feasibility - and therefore the true effect - of these CDC-promoted policies in the real-world setting. Given normal increases in CVF with advancing age, the analysis here was also strengthened by use of PACER z-scores based on previously collected data from Wisconsin children.18 Limitations of the study include a focus on low SES schools where implementation was likely to be especially challenging and effort-dependency of the PACER test itself. While there was a difference in baseline mean PACER scores in girls, since the primary outcome measure was change in PACER, this is unlikely to have affected the primary outcome. In addition, we were unable to regulate and assess the quality and consistency with which daily CDC strategies were implemented and to define and maintain consistency of the level of standard physical activity programming at control schools. While we acknowledge this is a significant limitation, it is also a necessary component to limit observation bias and evaluate the “real world” effectiveness of these recommendations.
This study is particularly relevant to the evaluation of public health interventions that are promoted as and predicted to be effective based on data obtained from more controlled settings. Application of such programs in the non-research school setting (“real world”) is accompanied by constraints in time, personnel, and resources that influence the effectiveness and effect of these interventions. Justification for widespread adoption of CDC school-based physical activity interventions, therefore, is likely to require simultaneous attention to potential adherence-limiting factors.
Conclusions
In Wisconsin low SES schools, a program implementing CDC recommended strategies to increase physical activity was not robust enough and/or not implemented with sufficient completeness to change childhood fitness trajectories compared to standard programming. Girls in particular showed lack of benefit from exposure to these strategies. These results suggest that, in order to have meaningful positive impact on cardiovascular fitness and childhood public health, school-based physical activity interventions need to be more vigorous, more acceptable to students, and implemented more effectively. Additional research is needed to clarify physical activity interventions that are well received by all children, especially those at highest risk for physical inactivity and low fitness.
IMPLICATIONS FOR SCHOOL HEALTH
While the CDC promotes school-based strategies to increase physical activity, this study suggests that these recommendations in isolation without additional support and funding do not translate to improved fitness in children. Similar to other areas, effective instruction in theory and practice of physical activity and implementation of these life-style habits has lifelong implications on students’ well-being. In addition to numerous physical health benefits, the importance of physical activity is amplified considering its association with increased academic engagement and achievement. Despite this evidence, physical activity and education is often overlooked or prioritized below other subject areas due to time and budgetary constraints.
In this study, physical education teachers reported lack of knowledge regarding benefits of physical activity and lack of support from administration as barriers to implementation of school-based physical activity. Thus, staff education about health and academic benefits of physical activity is an important first step in implementation of physical activity initiatives. An example of this would be inviting a local expert to speak to staff regarding the health and academic benefits of physical activity and to discuss opportunities to incorporate physical activity into a variety of school settings. Alternatively knowledgeable staff can also assist with education of colleagues.
Another important step to enhance feasibility of school-based interventions to increase opportunities for physical activity is mobilization of community resources. Without additional funding and/or staffing, schools may not have resources to offer or expand organized physical activity opportunities before or after school. In this case, schools could consider contacting local fitness centers, community organizations and/or seeking parent volunteers to assist with organization, funding and supervision of these activities. Schools can also apply for grants and/or organize local fundraisers to provide funding for additional equipment and/or staff.
Finally, policy changes at the state and national level are also likely needed to create momentum for school-based physical activity requirements that meaningfully impact health outcomes. It is imperative for school administrators and knowledgeable staff to advocate for these policy changes at both the state and national levels. Support for each of the above steps appears to be critical to improving the ability of the school environment to increase physical activity.
Human Subjects Approval Statement:
This study was determined to be exempt from research by the University Human Subjects Committee because there were no identifiable research participants and PACER was performed as part of routine school curriculum.
ACKNOWLEDGEMENTS
We thank the Wisconsin Department of Public Instruction for their assistance with this study. Funding for the study was provided by The University of Wisconsin-Madison Wisconsin Partnership Program and NIH T32 DK077586. The sponsors had no involvement in the: (1) study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; and (4) the decision to submit the paper for publication. The study is registered at clinicaltrials.gov: NCT02411552. The authors have no financial relationships or conflict of interest to disclose.
Contributor Information
Tasa Seibert, Department of Pediatrics, University Hospitals-Rainbow Babies and Children’s Hospital, Case Western Reserve University School of Medicine, 11100 Euclid Avenue, RBC 737, Cleveland, Ohio 44106, Phone: 216-844-3661, Fax: 216-844-8900.
David B. Allen, Department of Pediatrics, University of Wisconsin-Madison School of Medicine and Public Health, 600 Highland Avenue, CSC H4/407, Madison WI 53792, Phone: 608-263-9059, Fax: 608-265-7957, Dballen@pediatrics.wisc.edu.
Aaron L. Carrel, Department of Pediatrics, University of Wisconsin-Madison School of Medicine and Public Health, 600 Highland Avenue, CSC H4/407, Madison WI 53792, Phone: 608-265-8182, Fax: 608-265-7957, Alcarrel@pediatrics.wisc.edu.
Jens C. Eickhoff, Department of Pediatrics, University of Wisconsin-Madison School of Medicine and Public Health, 600 Highland Avenue, CSC H4/407, Madison WI 53792, Phone: (608) 265-5376, eickhoff@biostat.wisc.edu.
REFERENCES
- 1.Goran MI. Metabolic precursors and effects of obesity in children: a decade of progress, 1990–1999. Am J Clin Nutr 2001;73(2):158–171. [DOI] [PubMed] [Google Scholar]
- 2.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Public Health 2013;13(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cummings DM, Dubose KD, Imai S, Collier DN. Fitness versus Fatness and Insulin Resistance in U.S. Adolescents. J Obes 2010;2010. [DOI] [PMC free article] [PubMed]
- 4.Allen DB, Nemeth BA, Clark RR, Peterson SE, Eickhoff J, Carrel AL. Fitness is a stronger predictor of fasting insulin levels than fatness in overweight male middle-school children. J Pediatr 2007;150(4):383–387. [DOI] [PubMed] [Google Scholar]
- 5.Jimenez-Pavon DA, Castillo MJ, Moreno LA, Kafatos A, Manios Y, Kondaki K, et al. Fitness and fatness are independently associated with markers of insulin resistance in European adolescents; the HELENA study. Int J Pediatr Obes 2011;6(3–4):253–260. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. The Association Between School Based Physical Activity, Including Physical Education, and Academic Performance Atlanta, GA: U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 7.Williams SL, Mummery WK. We can do that! Collaborative Assessment of School Environments to Promote Healthy Adolescent Nutrition and Physical Activity Behaviors. Health Educ Res 2015;30(2):272–284. [DOI] [PubMed] [Google Scholar]
- 8.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical Activity in the United States Measured by Accelerometer. Med Sci Sports Exerc 2008;40(1):181–188. [DOI] [PubMed] [Google Scholar]
- 9.Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc 2010;42(12):2211–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drenowatz C, Eisenmann JC, Pfeiffer KA, Welk G, Heelan K, Gentile D, et al. Influence of socio-economic status on habitual physical activity and sedentary behavior in 8- to 11-year old children. BMC Public Health 2010;10:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Cocker K, Artero EG, De Henauw S, Dietrich S, Gottrand F, Béghin L, et al. Can differences in physical activity by socio-economic status in European adolescents be explained by differences in psychosocial correlates? A mediation analysis within the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Public Health Nutr 2012;15(11):2100–2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eyre EL, Duncan MJ. The impact of ethnicity on objectively measured physical activity in children. ISRN Obes 2013;2013:757431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li S, Chen W, Srinivasan SR, Xu J, Berenson GS. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol 2012;1(176):S142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Make a Difference at Your School: CDC Resources Can Help You Implement Strategies to Prevent Obesity Among Children and Adolescents. US Department of Health and Human Services Centers for Disease Control and Prevention Published January 2008 Available at: http://www.cdc.gov/healthyyouth/keystrategies/pdf/make-a-difference.pdf. Accessed December 1, 2017.
- 15.Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev 2013;2:Cd007651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varness T, Carrel AL, Eickhoff JC, Allen DB. Reliable prediction of insulin resistance by a school-based fitness test in middle-school children. Int J Pediatr Endocrinol 2009;2009:487804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Plowman SA. Muscular Strength, Endurance, and Flexibility Assessments. In: Plowman SA and Meredith MD, eds. Fitnessgram/Activitygram Reference Guide Vol 8-1 4th ed. Dallas, TX: The Cooper Institute; 2013. [Google Scholar]
- 18.Carrel AL, Bowser J, White D, Moberg DP, Weaver B, Hisgen J, et al. Standardized childhood fitness percentiles derived from school-based testing. J Pediatr 2012;161(1):120–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pillsbury L, Oria M, Pate R. Fitness Measures and Health Outcomes in Youth Washington D.C: National Academies Press; 2013. [PubMed] [Google Scholar]
- 20.Stevens J, Murray DM, Catellier DJ, Hannan PJ, Simons-Morton DG, Webber LS. Design of the Trial of Activity in Adolescent Girls (TAAG). Contemp Clin Trials 2005;26:223–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sandercock G, Voss C, McConnell D, Rayner P. Ten year secular declines in the cardiorespiratory fitness of affluent English children are largely independent of changes in body mass index. Arch Dis Child 2010;95(1):46–47. [DOI] [PubMed] [Google Scholar]


