Abstract
Background:
Prenatal exposure to certain xenobiotics has been associated with adverse birth outcomes. We examined the associations of triclocarban, phenols and parabens in a cohort of 922 pregnant women in Puerto Rico, the Puerto Rico Testsite for Exploring Contamination Threats Program (PROTECT).
Methods:
Urinary triclocarban, phenols and parabens were measured at three time points in pregnancy (visit 1: 16-20 weeks, visit 2: 20-24 weeks, visit 3: 24-28 weeks gestation). Multiple linear regression (MLR) models were conducted to regress gestational age and birthweight z-scores against each woman’s log average concentrations of exposure biomarkers. Logistic regression models were conducted to calculate odds of preterm birth, small or large for gestational age (SGA and LGA) in association with each of the exposure biomarkers. An interaction term between the average urinary biomarker concentration and infant sex was included in models to identify effect modification. The results were additionally stratified by study visit to look for windows of vulnerability. Results were transformed into the change in the birth outcome for an inter-quartile-range difference in biomarker concentration (Δ).
Results:
Average benzophenone-3, methyl- and propyl-paraben concentrations were associated with an increase in gestational age [(Δ 1.90 days; 95% CI: 0.54, 3.26); (Δ 1.63; 95% CI: 0.37, 2.89); (Δ 2.06; 95% CI: 0.63, 3.48), respectively]. Triclocarban was associated with a suggestive 2-day decrease in gestational age (Δ −1.96; 95% CI: −4.11, 0.19). Bisphenol A measured at visit 1 was associated with a suggestive increase in gestational age (Δ 1.37; 95% CI: −0.05, 2.79). Triclosan was positively associated with gestational age among males, and negatively associated with gestational age among females. Methyl-, butyl- and propyl-paraben were associated with significant 0.50-0.66 decreased odds of SGA. BPS was associated with an increase in the odds of SGA at visit 3, and a suggestive increase in the odds of LGA at visit 1.
Conclusion:
Benzophenone-3, methyl-paraben and propyl-paraben were associated with an increase in gestational age. Concentrations of triclocarban, which were much higher than reported in other populations, were associated with a suggestive decrease in gestational age. The direction of the association between triclosan and gestational age differed by infant sex. Parabens were associated with a decrease in SGA, and BPS was associated with both SGA and LGA depending on the study visit. Further studies are required to substantiate these findings.
Keywords: Gestational age, birth outcomes, phenols, parabens, triclocarban
1. Introduction
Gestational age at delivery and birth weight are important predictors of fetal and infant health. For example, preterm birth (PTB), defined as gestational age less than 37 weeks is a leading cause of neonatal death in the United States and most high and middle income countries, accounting for over a third of the 3.1 million global neonatal deaths every year (Blencowe et al., 2013; Liu et al., 2012). Babies born following a short gestation or having low birth weight (less than 2500 grams at birth) face lifelong risks for adverse health effects, including an increased risk of cerebral palsy, neurological conditions, and a number of developmental disabilities such as vision and hearing impairment. In addition, babies born preterm are more likely to have respiratory conditions, such as asthma, and chronic diseases later in life (Blencowe et al., 2013; Centers for Disease Control and Prevention, 2015; Luu et al., 2015; Marlow et al., 2005; McCormick, 1985; Valdez et al., 1994). The U.S. PTB rate has been declining since 1997 and have begun to increase nationally since 2016 and remains at one of the highest rates in the developed world at 9.6% (Hamilton et al., 2015; Schoen et al., 2015).
On the other hand, pregnancies lasting over 40 weeks are associated with their own risks, to the baby and the mother. The rate of fetal death or stillbirth, birth injuries, and neonatal complications are increased as well as maternal complications including perineal lacerations, postpartum hemorrhage, and increase rate of caesarean deliveries (Caughey et al., 2007; Galal et al., 2012). In the United States, induction of labor after 40 weeks gestation has reduced the rates of post-term pregnancy (pregnancies over 42 weeks) from approximately 14% to 4% in 2005 (Martin et al., 2007).
Thyroid and reproductive hormones, inflammatory responses and oxidative stress play an important role in maintaining a healthy pregnancy and an adequate gestational duration (Casey, 2006; Castracane, 2000; Kemp, 2014; Kumar and Magon, 2012; Smith et al., 2009). Therefore, environmental chemicals that influence hormones and inflammatory responses could potentially lead to adverse health effects during pregnancy. Phenols and parabens are a group of ubiquitous chemicals commonly found in personal care products and household items that have been associated with changes in reproductive and thyroid hormones, as well as increased inflammation levels in pregnancy (Aker et al., 2016; Boas et al., 2009; Kolatorova et al., 2018; Neier et al., 2015; Watkins et al., 2015). For example, BPA was associated with an increase in FT4 (Aker et al., 2016), and parabens were generally associated with a decrease in thyroid hormones (Koeppe et al., 2013). These groups of chemicals have also been linked to a number of growth parameters during pregnancy and at birth, including birth weight, birth length and gestational age (Ferguson et al., 2018; Lassen et al., 2016; Philippat et al., 2014; Tang et al., 2013; Wolff et al., 2008). Studies are lacking on birth outcomes in relation to triclocarban, a chemical with antibacterial properties, as well as bisphenol A (BPA) replacement phenols such as bisphenol S (BPS) and bisphenol F (BPF), even though BPA replacements are found in a high prevalence of urine samples from the general population, and have comparable endocrine disrupting effects to BPA (Rochester and Bolden, 2015)
We were interested in exploring the association between triclocarban, phenols and parabens in relation to birth outcomes in a cohort in Puerto Rico. Puerto Rico has increased rates of adverse birth outcomes, such as preterm birth, and the reasons behind this elevated rate are unclear (2017 Premature Birth Report Card: Puerto Rico, 2017). There is also evidence for elevated exposures to a range of contaminants on the island. The Puerto Rico Testsite for Exploring Contamination Threats (PROTECT), is a multi-disciplinary center that established a pregnancy cohort in Puerto Rico to investigate the role of environmental contamination in adverse birth outcomes. This analysis explores relationships between birth outcomes and urinary concentrations of triclocarban and 11 phenols and parabens: 2,4-dichlorophenol, 2,5-dichlorophenol, BPA, BPS, BPF, benzophenone-3, triclosan, and ethyl-, methyl-, butyl- and propyl-paraben.
2. Methods
2.1. Study Population
Participants for this study were from the PROTECT cohort, an ongoing prospective cohort of pregnant women based in Northern Puerto Rico. Details on the recruitment and inclusion criteria have been described previously (Cantonwine et al., 2014; Meeker et al., 2013). The 922 study participants in the present analysis were recruited from 2011-2017 at 18 ± 2 weeks gestation from five affiliated health clinics whose patients deliver at two collaborating hospitals were older than 18 years old, and indicated that they were planning to deliver at one of the collaborating hospitals. The exclusion criteria included: 1) women who lived outside the region, 2) multiple gestations, 3) use of oral contraceptives within three months prior to getting pregnant, 4) pregnancy through in vitro fertilization, and 5) any known medical health complications (including diabetes, hypertension, etc.). Each woman participated in a total of up to three study visits which coincided with routine clinical visits and rapid fetal growth. Visit 1 was targeted at 16-20 weeks gestation; visit 2 was targeted at 20-24 weeks gestation; and, visit 3 was targeted at 24-28 weeks gestation. Demographic information was collected via questionnaire at visit 1. Spot urine samples were collected at each of the study visits, and blood samples were collected at the first and third visit. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Puerto. Rico (Harris et al., 2009).
This study was approved by the research and ethics committees of the University Of Michigan School Of Public Health, University of Puerto Rico, Northeastern University, and the University of Georgia. All study participants provided full informed consent prior to participation.
2.2. Urinary biomarker measurement
Spot urine samples collected during the three study visits were divided into aliquots and frozen at −80 °C until they were shipped overnight on dry ice to the Centers for Disease Control and Prevention for analysis. Samples were analyzed for triclocarban, seven phenols (2,4-dichlorophenol, 2,5-dichlorophenol, BPA, BPS, BPF, benzophenone-3, triclosan), and four parabens (ethyl-paraben, methyl-paraben, butyl-paraben, propyl-paraben) using online solid phase extraction-high-performance liquid chromatography-isotope dilution tandem mass spectrometry (Watkins et al., 2015; Ye et al., 2005, 2006). Biomarker concentrations below the limit of detection (LOD) were assigned a value of the LOD divided by √2 (Hornung and Reed, 1990). Urinary dilution was accounted for using urinary specific gravity (SG), and was measured using a digital handheld refractometer (AtagoCo., Ltd., Tokyo, Japan) at the time of the urine collection. Urinary biomarkers were corrected for SG in preliminary analyses using the following formula:
Equation 1: Specific gravity correction of exposure biomarkers where Pc is the SG-corrected biomarker concentration (ng/mL), M is the measured biomarker concentration, SGm is the study population median urinary specific gravity (1.0196), and SGi is the individual’s urinary specific gravity. The sample size for BPF, BPS, triclocarban and ethyl-paraben was smaller than for the other urinary biomarkers because they were added to the analytical panel mid-way through the study, and thus, only available on a subset of the cohort.
2.3. Gestational Age Calculation
The gestational age for complete pregnancies was calculated according to the American Congress of Gynecologists (ACOG) recommendations (Committee on Obstetric Practice, the American Institute of Ultrasound in Medicine, and the Society for Maternal-Fetal Medicine, 2017), and it is described as the best obstetrical estimate. In brief, gestational age determination utilizes both the last menstrual cycle date (LMP) as reported by the mother, and the gestational age from the first ultrasound obtained before 20 weeks gestation. The selection between the gestational age from the LMP or ultrasound depends on two criteria: 1) gestational age at which the ultrasound was conducted, and 2) whether the difference in the estimated date of delivery (EDD) calculated from the LMP and from the ultrasound is less or more than seven days. Further details on this calculation can be found in the ACOG Committee Opinion document (Committee on Obstetric Practice, the American Institute of Ultrasound in Medicine, and the Society for Maternal-Fetal Medicine, 2017). A PTB is defined as giving birth prior to 37 gestational weeks.
2.4. Birthweight Calculation
Birthweight values extracted from medical records were converted to gestational age and sex specific z-scores, calculated according to the INTERGROWTH-21st standards (Villar et al., 2014).
Infants were considered small for gestational age (SGA) if they fell below the 10th percentile of birthweight z-scores. Infants were considered large for gestational age (LGA) if they fell above the 90% percentile of birthweight z-scores.
2.5. Statistical Analyses
Distributions of key demographic characteristics were calculated. Spearman correlations were calculated to examine correlations between specific gravity-corrected average biomarker concentrations. Distributions of subject-specific average biomarker concentrations were examined using select percentiles. Distributions were also examined by study visit. Ethyl-paraben and BPF were detected in less than 50% of the samples. Therefore, we transformed BPF and ethyl-paraben into dichotomous variables, where 0 represents concentrations below the LOD, and 1 represents concentrations above the LOD (i.e. detected versus non-detected). These categorical BPF and ethyl-paraben variables were used for all regression analyses. The remaining urinary biomarkers were all positively-skewed, so they were log-transformed for the remainder of the analyses.
Models were constructed to regress each of the four birth outcome variables against each of the exposure biomarker variables. Multiple linear regressions (MLR) were conducted to examine associations between gestational age and one average exposure biomarker, as well as birthweight z-scores and one average exposure biomarker. Logistic regression models were conducted to examine associations between PTB, SGA or LGA and one average exposure biomarker. Due to the similar complications SGA and LGA may incur, SGA models did not include LGA births, and LGA models did not include SGA births. The average urinary exposure biomarker variables are the average urinary exposure biomarker concentrations across the three study visits. In the case of a missing value at one of the study visits, the average was taken of the two remaining concentrations. In the case of two missing concentrations, the “average” phenol or paraben concentration was equal to the single available concentration. Crude analyses included only the average urinary biomarker and the average specific gravity. Additional covariates were included in the model in a step-wise fashion. A covariate was maintained in the model if it changed the main effect estimate by >10%. Finals models were controlled for the following covariates: specific gravity, maternal age, insurance type, alcohol use, and exposure to second-hand smoking. Other variables considered include parity, smoking, maternal education, marital status, number of children, and BMI. To increase interpretability of our results, we transformed regression coefficients from MLRs and odds ratios from logistic models to the change in the birth outcome in relation to the interquartile range (IQR) increase in urinary biomarker concentrations. The alpha level was set at 0.05. All statistical analyses were conducted in R Version 3.4.2.
We performed two sensitivity analyses. First, we ran the same MLR and logistic regression models regressing the birth outcome measure against biomarkers concentrations stratified by study visit of sample collection. Second, we examined an interaction term between the average urinary biomarker concentration and infant sex in the models to examine any potential effect modification by infant sex, and then stratified the models by infant sex if the p value exceeded 0.05.
Given the right-skewed distribution of gestational age, we ran sensitivity analyses to test the robustness of our results. We created a new variable by subtracting the individual gestational age from the maximum gestational age, and then took the log of the result. The resulting variable had a normal distribution. We re-ran the MLR models using this new gestational age variable. There was no difference in the interpretation of the results; therefore, we maintained our original models. We also ran multinomial logistic regression models to examine associations between the chemicals and size at birth (SGA, LGA and 10-90% percentile at birth). There were no differences in the results between the multinomial logistic regression models and the original logistic regression modes; therefore, we maintained our original models.
3. Results
The mean age of the 922 study participants was 26.7 years (Table 1). Almost half of the participants had a body mass index (BMI) <25 kg/m2, and 14% had a BMI > 29.9 kg/m2, but 17% of the BMI values were missing. Sixty percent of the study population was dependent on government health insurance, suggesting a low socio-economic status (SES), and 50% of the population had household incomes up to $30,000. This is representative of the general Puerto Rican population (Fact Sheet Puerto Rico: Fast Facts, 2017). Only 13% had a household income of >$50,000, though 43% of the women attended college or technical school. Three percent of the women smoked during pregnancy (the questionnaire was administered at 16-20 weeks gestation), and 6% reported over one hour of second-hand smoking exposure per day. Six and a half percent reported drinking alcohol within the last few months. Almost 80% of the women reported being married or living with their partner, while 20% reported being single. Nearly half of the women had no other children at home.
Table 1:
Summary demographics of the 922 pregnant women in the study population
| Overall | |
|---|---|
| Total N | 922 |
| Gestational Age | 38.8 (2.0) |
| Birthweight (Mean (SD)) | 110.6oz (19.4) |
| Preterm Birth | 10.3% |
| Small for Gestational Age | 9.9% |
| Large for Gestational Age | 9.1% |
| Maternal Age (Mean (SD)) | 26.70 (5.5) |
| BMI (%) | |
| <25 kg/m2 | 437 (47.4) |
| 25-29.9 kg/m2 | 201 (21.8) |
| >29.9 kg/m2 | 129 (14.0) |
| Missing | 155 (16.8) |
| Insurance type (%) | |
| Public (Mi Salud) | 555 (60.2) |
| Private | 322 (34.9) |
| Missing | 45 (4.9) |
| Household Income (%) | |
| <$10,000 | 234 (25.4) |
| $10,000-$30,000 | 246 (26.7) |
| $30,000-$50,000 | 184 (20.0) |
| >$50,000 | 123 (13.3) |
| Missing | 135 (14.6) |
| Maternal Education (%) | |
| ≤High School/GED | 187 (20.3) |
| Some College or technical school | 331 (35.9) |
| College graduate or technical school | 392 (42.5) |
| Missing | 12 (1.3) |
| Smoking (%) | |
| Never | 763 (82.8) |
| Ever | 120 (13.0) |
| Current | 29 (3.1) |
| Missing | 10 (1.1) |
| Exposure to second hand smoking (%) | |
| None | 781 (84.7) |
| Up to 1 hour | 44 (4.8) |
| More than 1 hour | 59 (6.4) |
| Missing | 38 (4.1) |
| Alcohol Consumption (%) | |
| None | 463 (50.2) |
| Before pregnancy | 385 (41.8) |
| Yes within the last few months | 60 (6.5) |
| Missing | 14 (1.5) |
| Marital Status (%) | |
| Single | 180 (19.5) |
| Married | 517 (56.1) |
| Divorced | 11 (1.2) |
| Living together | 205 (22.2) |
| Missing | 9 (1.0) |
| Number of previous children (%) | |
| 0 | 436 (47.3) |
| 1 | 364 (39.5) |
| >1 | 111 (12.0) |
| Missing | 11 (1.2) |
Demographic variables collected during the second study visit (20-24 weeks).
Up to 867 women had available data on urinary exposure biomarker concentrations (Table 2). The target biomarkers were highly detected in the study population, with the exception of BPF and ethyl-paraben. Fifty-seven and 43 percent of BPF and ethyl-paraben concentrations were below the LOD. Biomarker concentrations remained relatively consistent across the three study visits, with the exception of 2,5-dichlorophenol (p value=0.02) and butyl-paraben (p value=0.004) that had higher concentrations during visit 1 versus visits 2 and 3. Average methyl- and propyl-paraben concentrations were strongly correlated (Spearman correlation=0.78, p value<0.001) (Supplemental Figure 2). Propyl-paraben was also moderately correlated with butyl-paraben and ethyl-paraben (Spearman correlation=0.42, p value<0.001). 2,4-Dichlorophenol and 2,5-dichlorophenol were strongly correlated (Spearman correlation=0.67, p value<0.001), and 2,4-dichlorophenol was also moderately correlated with triclosan (Spearman correlation=0.51, p value<0.001).
Table 2:
SG-corrected urinary biomarker average concentrations and by study visit of sample collection in pregnancy. Range of gestational weeks for sample collection: Visit 1: 16-20 weeks gestation, Visit 2: 20-24 weeks gestation Visit 3: 24-28 weeks gestation.
| All | Visit 1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % <LOD | N | GM (GSD) | 25% | 50% | 75% | % <LOD | N | GM (GSD) | 25% | 50% | 75% | |
| 2,4-Dichlorophenol | 1.1 | 1871 | 1.09 (3.42) | 0.50 | 0.99 | 2.17 | 0.7 | 674 | 1.16 (3.29) | 0.50 | 1.01 | 2.10 |
| 2,5-Dichlorophenola | 0.1 | 1872 | 13.14 (5.40) | 4.10 | 10.22 | 31.64 | 0.1 | 672 | 14.18 (5.42) | 4.40 | 11.05 | 36.41 |
| BPA | 0.6 | 1868 | 2.02 (2.54) | 1.10 | 1.98 | 3.49 | 0.1 | 667 | 2.16 (2.49) | 1.21 | 2.09 | 3.68 |
| BPS | 6.1 | 1310 | 0.46 (3.16) | 0.20 | 0.40 | 0.90 | 5.5 | 465 | 0.47 (3.32) | 0.20 | 0.40 | 0.99 |
| BPF | 56.8 | 1144 | 0.27 (2.97) | 0.14 | 0.14 | 0.40 | 54 | 416 | 0.30 (3.22) | 0.14 | 0.14 | 0.50 |
| Benzophenone-3 | 0.2 | 1869 | 39.45 (6.63) | 10.36 | 26.50 | 124.85 | 0.4 | 671 | 42.06 (6.37) | 11.35 | 29.27 | 126.61 |
| Triclosan | 1.6 | 1874 | 22.75 (8.65) | 3.61 | 15.79 | 139.27 | 2.1 | 669 | 23.76 (8.85) | 3.71 | 15.75 | 149.51 |
| Triclocarban | 6.4 | 1312 | 3.41 (10.90) | 0.50 | 2.31 | 26.79 | 6.5 | 469 | 3.42 (10.79) | 0.50 | 2.28 | 25.52 |
| Ethyl-paraben | 42.9 | 1318 | 2.56 (6.48) | 0.71 | 1.24 | 7.83 | 39.7 | 470 | 3.10 (7.11) | 0.71 | 1.55 | 10.52 |
| Methyl-paraben | 0.5 | 1876 | 74.74 (5.28) | 23.56 | 88.54 | 249.93 | 0.4 | 670 | 77.67 (5.24) | 25.50 | 97.51 | 262.15 |
| Butyl-parabena | 26.3 | 1865 | 0.45 (7.61) | 0.07 | 0.20 | 1.80 | 23.4 | 664 | 0.53 (8.43) | 0.10 | 0.20 | 2.84 |
| Propyl-paraben | 0.3 | 1875 | 14.78 (7.60) | 3.19 | 17.17 | 76.76 | 0 | 670 | 15.96 (7.43) | 3.39 | 20.06 | 78.86 |
| Visit 2 | Visit 3 | |||||||||||
| % <LOD | N | GM (GSD) | 25% | 50% | 75% | % <LOD | N | GM (GSD) | 25% | 50% | 75% | |
| 2,4-Dichlorophenol | 0.9 | 674 | 1.08 (3.42) | 0.50 | 0.91 | 2.11 | 1.9 | 523 | 1.04 (3.58) | 0.40 | 0.90 | 2.19 |
| 2,5-Dichlorophenola | 0 | 675 | 12.22 (5.33) | 3.83 | 9.58 | 27.29 | 0.2 | 525 | 13.08 (5.47) | 4.01 | 9.84 | 29.67 |
| BPA | 1.2 | 678 | 2.07 (2.69) | 1.10 | 2.01 | 3.71 | 0.6 | 523 | 1.78 (2.40) | 1.00 | 1.71 | 3.09 |
| BPS | 6.9 | 476 | 0.45 (3.02) | 0.20 | 0.40 | 0.90 | 5.7 | 369 | 0.45 (3.16) | 0.20 | 0.40 | 0.90 |
| BPF | 56.6 | 410 | 0.28 (3.05) | 0.14 | 0.14 | 0.40 | 60.5 | 318 | 0.24 (2.52) | 0.14 | 0.14 | 0.37 |
| Benzophenone-3 | 0 | 675 | 39.83 (6.49) | 10.35 | 26.62 | 128.77 | 0.2 | 523 | 35.88 (7.17) | 8.87 | 23.67 | 112.91 |
| Triclosan | 1.2 | 676 | 22.56 (8.77) | 3.57 | 16.18 | 147.99 | 1.5 | 529 | 21.76 (8.28) | 3.61 | 15.72 | 121.40 |
| Triclocarban | 6.9 | 476 | 3.27 (11.06) | 0.50 | 2.31 | 28.94 | 5.5 | 367 | 3.58 (10.88) | 0.51 | 3.30 | 27.45 |
| Ethyl-paraben | 42 | 478 | 2.36 (5.98) | 0.71 | 1.30 | 5.96 | 47.9 | 370 | 2.23 (6.25) | 0.71 | 0.85 | 6.70 |
| Methyl-paraben | 0.6 | 678 | 69.43 (5.37) | 21.48 | 78.36 | 236.91 | 0.6 | 528 | 78.24 (5.23) | 23.99 | 94.39 | 251.31 |
| Butyl-parabenaa | 26.8 | 675 | 0.41 (6.81) | 0.07 | 0.20 | 1.39 | 29.4 | 526 | 0.43 (7.59) | 0.07 | 0.20 | 1.49 |
| Propyl-paraben | 0.4 | 677 | 13.48 (7.50) | 3.04 | 14.16 | 69.40 | 0.4 | 528 | 15.08 (7.92) | 3.08 | 18.87 | 78.10 |
GM: Geometric mean
GSD: Geometric standard deviation
Significant difference (p<0.05) in urinary exposure metabolite or hormone compared to reference (visit 1) using linear mixed models with a random intercept. All biomarker units: μg/mL.
LODs for biomarkers: 2,4-dichlorphenol and 2,5-dichlorophenol, BPS, triclocarban, butylparaben, propylparaben: 0.1 μg/L. BPA and BPF: 0.2 μg/L. BPF: 0.4 μg/L. Methyl-paraben and ethyl-paraben: 1 μg/L. Triclosan: 1.7 μg/L.
3.1. Gestational Age
The sensitivity analysis showed no difference in the interpretation of results between the transformed and untransformed gestational age variables (Supplementary Table 1); therefore, the remainder of the results are retrieved from MLR models using the untransformed gestational age variable.
Benzophenone-3, methyl-paraben and propyl-paraben were associated with an increase in gestational age [(1.90 change in gestational age days per IQR increase in biomarker concentration (Δ/IQR); 95% CI: 0.54, 3.26); (Δ/IQR 1.63; 95% CI: 0.37, 2.89); (Δ/IQR 2.06; 95% CI: 0.63, 3.48), respectively] (Table 3). Conversely, triclocarban was associated with a suggestive decrease in gestational age (Δ/IQR −1.96; 95% CI: −4.11, 0.19).
Table 3:
Adjusteda change in gestational age or odds ratios in relation to average exposure biomarker concentration across three time points during pregnancy. Beta coefficients were transformed to change or odds ratio for an IQR increase in exposure biomarker concentration.
| Gestational Age | Preterm Birth | ||||
|---|---|---|---|---|---|
| N | Change in days/IQR (95% CI) | p | OR/IQR change (95% CI) | p | |
| 2,4-Dichlorophenol | 748 | 0.07 (−1.20, 1.33) | 0.92 | 1.04 (0.75, 1.43) | 0.81 |
| 2,5-Dichlorophenol | 749 | −0.46 (−1.68, 0.76) | 0.46 | 1.18 (0.87, 1.61) | 0.29 |
| BPA | 748 | 0.98 (−0.41, 2.37) | 0.17 | 0.72 (0.48, 1.07) | 0.10 |
| BPFb | 500 | 0.06 (−0.28, 0.41) | 0.72 | 0.60 (0.31, 1.17) | 0.14 |
| BPS | 540 | −0.52 (−2.14, 1.09) | 0.53 | 1.08 (0.70, 1.66) | 0.72 |
| Benzophenone-3 | 749 | 1.90 (0.54, 3.26) | 0.006** | 0.54 (0.36, 0.83) | 0.01** |
| Triclosan | 749 | 0.12 (−1.64, 1.87) | 0.90 | 0.94 (0.58, 1.51) | 0.79 |
| Triclocarban | 544 | −1.96 (−4.11, 0.19) | 0.08* | 1.50 (0.84, 2.67) | 0.17 |
| Ethyl-parabenb | 550 | −0.11 (−0.44, 0.23) | 0.53 | 0.89 (0.47, 1.68) | 0.71 |
| Methyl-paraben | 751 | 1.63 (0.37, 2.89) | 0.01** | 0.70 (0.49, 0.98) | 0.04** |
| Butyl-paraben | 746 | 0.60 (−1.23, 2.42) | 0.52 | 0.90 (0.54, 1.49) | 0.67 |
| Propyl-paraben | 752 | 2.06 (0.63, 3.48) | 0.005** | 0.64 (0.44, 0.94) | 0.02** |
Models adjusted for specific gravity, maternal age, insurance type, alcohol use, and exposure to second-hand smoking.
Categorical variable.
0.05 < p value < 0.10;
p value < 0.05
After stratification by study visit, visit 1 (16-20 weeks gestational age) showed stronger associations for a number of exposure biomarkers (Table 4). At visit 1, BPA was suggestively associated with an increase in gestational age (Δ/IQR 1.37; 95% CI:−0.05, 2.79). Additionally, associations between gestational age and triclocarban, methyl-paraben and propyl-paraben were strongest (largest change in days and lowest p values) at visit 1. Propyl-paraben was also associated with a significant increase in gestational age at 24-28 weeks gestation (Δ/IQR 1.84; 95% CI: 0.02, 3.65), but not at 20-24 weeks gestation. Benzophenone-3 was consistently associated with an approximate 1.5 day increase in gestational age at all three study visits.
Table 4:
Adjusteda change or odds ratio in relation to exposure biomarker concentration, stratified by visit during pregnancy. Beta coefficients were transformed to the change in the number of gestational days or odds ratio per IQR change in exposure biomarker concentration.
| Gestational Age | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (16-20 weeks) | Visit 2 (20-24 weeks) | Visit 3 (24-28 weeks) | |||||||
| N | Change in days (95% CI) | p | N | Change in days (95% CI) | p | N | Change in days (95% CI) | p | |
| 2,4-DCP | 613 | 0.05 (−1.21, 1.31) | 0.94 | 624 | 0.65 (−0.59, 1.89) | 0.30 | 470 | −0.28 (−1.87, 1.31) | 0.73 |
| 2,5-DCP | 612 | −0.50 (−1.78, 0.78) | 0.45 | 624 | 0.29 (−0.95, 1.52) | 0.65 | 472 | −0.92 (−2.30, 0.45) | 0.19 |
| BPA | 607 | 1.37 (−0.05, 2.79) | 0.06* | 626 | 1.13 (−0.26, 2.53) | 0.11 | 470 | 0.90 (−0.81, 2.62) | 0.30 |
| BPFb | 381 | 0.12 (−0.27, 0.51) | 0.55 | 381 | −0.22 (−0.62, 0.18) | 0.28 | 291 | 0.24 (−0.19, 0.68) | 0.27 |
| BPS | 422 | −0.58 (−2.27, 1.11) | 0.5 | 438 | −0.27 (−2.02, 1.47) | 0.76 | 329 | 0.44 (−1.34, 2.23) | 0.63 |
| BP-3 | 611 | 1.56 (0.18, 2.93) | 0.03** | 623 | 1.44 (0.05, 2.83) | 0.04** | 470 | 1.63 (0.15, 3.12) | 0.03** |
| TCS | 609 | 0.21 (−1.49, 1.91) | 0.81 | 625 | 0.41 (−1.28, 2.09) | 0.63 | 476 | 0.85 (−1.07, 2.76) | 0.39 |
| TCC | 426 | −2.21 (−4.43, 0.01) | 0.05* | 437 | −2.10 (−4.33, 0.14) | 0.07* | 328 | −1.33 (−3.62, 0.96) | 0.26 |
| EPBb | 428 | −0.20 (−0.55, 0.16) | 0.28 | 440 | 0.06 (−0.30, 0.41) | 0.75 | 330 | −0.12 (−0.51, 0.26) | 0.53 |
| MPB | 610 | 2.24 (0.75, 3.73) | 0.003** | 625 | 0.56 (−0.91, 2.03) | 0.45 | 475 | 1.03 (−0.59, 2.65) | 0.21 |
| BPB | 604 | 1.17 (−0.44, 2.79) | 0.15 | 622 | 0.15 (−1.41, 1.72) | 0.85 | 474 | −0.13 (−1.91, 1.65) | 0.89 |
| PPB | 610 | 2.59 (0.97, 4.21) | 0.002** | 625 | 0.90 (−0.67, 2.46) | 0.26 | 475 | 1.84 (0.02, 3.65) | 0.05** |
| Preterm Birth | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (16-20 weeks) | Visit 2 (20-24 weeks) | Visit 3 (24-28 weeks) | |||||||
| N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | |
| 2,4-DCP | 613 | 1.16 (0.83, 1.61) | 0.38 | 624 | 0.85 (0.60, 1.21) | 0.37 | 470 | 1.12 (0.74, 1.72) | 0.59 |
| 2,5-DCP | 612 | 1.29 (0.92, 1.80) | 0.14 | 624 | 0.99 (0.70, 1.39) | 0.95 | 472 | 1.34 (0.93, 1.93) | 0.11 |
| BPA | 607 | 0.69 (0.45, 1.05) | 0.09* | 626 | 0.77 (0.51, 1.15) | 0.20 | 470 | 0.98 (0.60, 1.60) | 0.94 |
| BPFa | 381 | 0.83 (0.41, 1.70) | 0.62 | 381 | 1.30 (0.63, 2.67) | 0.48 | 291 | 0.36 (0.15, 0.84) | 0.02** |
| BPS | 422 | 1.07 (0.69, 1.66) | 0.77 | 438 | 1.11 (0.71, 1.75) | 0.64 | 329 | 0.98 (0.57, 1.69) | 0.95 |
| BP-3 | 611 | 0.64 (0.42, 0.98) | 0.04** | 623 | 0.66 (0.43, 1.02) | 0.06* | 470 | 0.67 (0.41, 1.07) | 0.10* |
| TCS | 609 | 0.98 (0.60, 1.58) | 0.92 | 625 | 0.76 (0.46, 1.26) | 0.29 | 476 | 0.77 (0.44, 1.36) | 0.37 |
| TCC | 426 | 1.71 (0.94, 3.10) | 0.08* | 437 | 1.61 (0.88, 2.94) | 0.12 | 328 | 1.04 (0.51, 2.10) | 0.92 |
| EPBa | 428 | 1.35 (0.69, 2.62) | 0.38 | 440 | 0.79 (0.40, 1.54) | 0.49 | 330 | 1.04 (0.46, 2.34) | 0.93 |
| MPB | 610 | 0.58 (0.38, 0.89) | 0.01** | 625 | 0.81 (0.53, 1.24) | 0.34 | 475 | 0.75 (0.47, 1.19) | 0.22 |
| BPB | 604 | 0.75 (0.46, 1.21) | 0.24 | 622 | 1.02 (0.65, 1.60) | 0.92 | 474 | 0.95 (0.57, 1.59) | 0.85 |
| PPB | 610 | 0.51 (0.32, 0.80) | 0.004** | 625 | 0.76 (0.49, 1.18) | 0.22 | 475 | 0.69 (0.42, 1.14) | 0.15 |
2,4-DCP: 2,4-dichlorophenol; 2,5-DCP: 2,5-dichlorophenol; BP-3: Benzophenone; TCS: Triclosan; TCC: Triclocarban; EPB: Ethyl-paraben; MPB: Methyl-paraben; BPB: Butyl-paraben; PPB: Propyl-paraben
Models adjusted for specific gravity, maternal age, insurance type, alcohol use, and exposure to second-hand smoking.
Categorical variable.
0.05 < p value < 0.10;
p value < 0.05
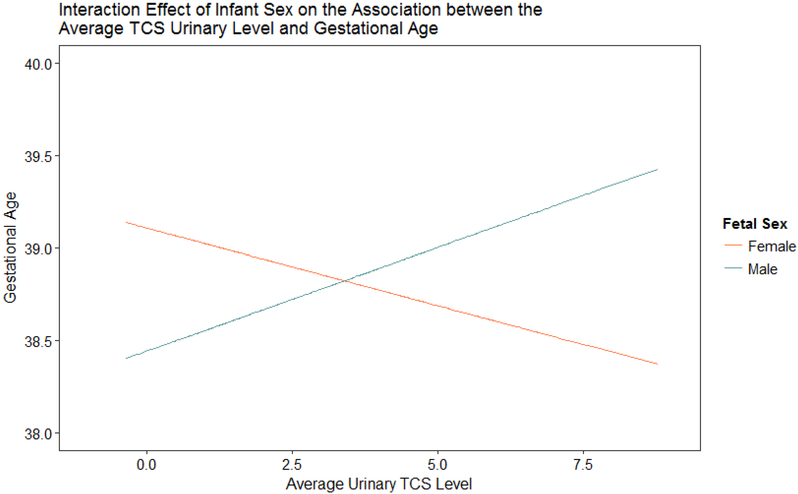
Sex differences were then explored by including an interaction term between the urinary biomarkers and infant sex (Supplementary Table 2). The infant sex*biomarker interaction term was significant in the model for gestational age and triclosan (p value=0.006). Urinary triclosan concentration was associated with a suggestive decrease in gestational age among females (Δ/IQR −2.31; 95% CI:−4.86, 0.24; p value = 0.08), and associated with an increase in gestational age among males (Δ/IQR 2.96; 95% CI: 0.41, 5.51; p value = 0.02). Figure 1 is a graph of the interaction effect of infant sex on the association between the average triclosan concentration and gestational age. Supplemental Figure 2 shows the conditional effect of the average triclosan concentration on gestational age stratified by infant sex to better view the difference in the direction of association between male and female infants.
Figure 1:
Interaction effect of infant sex on the association between the average triclosan urinary concentration and gestational age. Female p value = 0.06. Male p value = 0.03.
3.2. Preterm Birth (PTB)
Results from these models regressing PTB resembled the results observed in models regressing gestational age against the exposure biomarkers. Average BP-3, MPB and PPB were associated with a decreased odds of PTB [(OR/IQR 0.54; 95% CI: 0.36, 0.83); (OR/IQR 0.70; 95% CI: 0.49, 0.98); and (OR/IQR 0.64; 95% CI: 0.44, 0.94). The associations with BP-3 did not differ by study visit, but associations with MPB and PPB with PTB were stronger at study visit 1 [(OR/IQR 0.58; 95% CI: 0.38, 0.89) and (OR/IQR 0.51; 95% CI: 0.32, 0.80)]. BPA and TCC were also associated with PTB at visit 1 only. BPA was associated with a suggestive decreased odds of PTB at 16-20 weeks (OR/IQR 0.69; 95% CI: 0.45, 1.05), while TCC was associated with a suggestive increased odds of PTB at 16-20 weeks (OR/IQR 1.71; 95% CI: 0.94, 3.10). Lastly, BPF was associated with a decreased odds of PTB at 24-28 weeks (OR/IQR 0.36; 95% CI: 0.15, 0.84).
3.3. Birthweight
No averaged exposure biomarkers were associated with the birthweight z-score (Table 5). After stratification by study visit, butyl-paraben was associated with a suggestive increase of 0.12 in the birthweight z-score at visit 2 (z-score Δ/IQR 0.12; 95% CI: −0.02, 0.26). Fetal sex did not modify any of the associations with birthweight z-scores; interaction terms between biomarkers and fetal sex were all above 0.10.
Table 5:
Adjusteda change in birth weight z-scores or odds ratios associated with average exposure biomarker concentration across three time points during pregnancy. Effect estimates presented as change or odds ratio for IQR increase in exposure biomarker concentration.
| Birthweight z-scores | SGA | LGA | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Change in z-score (95% CI) | p | N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | |
| 2,4-DCP | 736 | −0.02 (−0.13, 0.09) | 0.70 | 662 | 1.32 (0.95, 1.84) | 0.10 | 667 | 1.04 (0.74, 1.47) | 0.82 |
| 2,5-DCP | 737 | 0.00 (−0.11, 0.10) | 0.97 | 663 | 1.16 (0.84, 1.60) | 0.36 | 668 | 1.11 (0.81, 1.54) | 0.51 |
| BPA | 736 | −0.01 (−0.13, 0.11) | 0.90 | 662 | 1.09 (0.75, 1.58) | 0.66 | 667 | 0.94 (0.65, 1.36) | 0.74 |
| BPFb | 496 | −0.09 (−0.30, 0.12) | 0.39 | 444 | 1.00 (0.53, 1.89) | 0.99 | 446 | 0.69 (0.36, 1.32) | 0.26 |
| BPS | 535 | 0.05 (−0.09, 0.20) | 0.46 | 479 | 1.49 (0.97, 2.29) | 0.07* | 482 | 1.62 (1.06, 2.45) | 0.02** |
| BP-3 | 737 | 0.08 (−0.04, 0.20) | 0.17 | 664 | 0.91 (0.62, 1.33) | 0.63 | 668 | 1.38 (0.99, 1.93) | 0.06* |
| TCS | 737 | −0.09 (−0.24, 0.06) | 0.26 | 663 | 1.70 (1.06, 2.73) | 0.03** | 668 | 0.91 (0.57, 1.46) | 0.70 |
| TCC | 539 | −0.10 (−0.29, 0.09) | 0.31 | 483 | 0.91 (0.50, 1.67) | 0.77 | 486 | 1.04 (0.60, 1.81) | 0.89 |
| EPBb | 545 | −0.06 (−0.26, 0.15) | 0.58 | 489 | 1.57 (0.86, 2.89) | 0.15 | 492 | 1.25 (0.68, 2.30) | 0.47 |
| MPB | 739 | −0.01 (−0.12, 0.10) | 0.88 | 665 | 0.66 (0.47, 0.93) | 0.02** | 670 | 0.92 (0.66, 1.30) | 0.65 |
| BPB | 734 | 0.11 (−0.05, 0.27) | 0.16 | 660 | 0.50 (0.28, 0.88) | 0.02** | 666 | 1.02 (0.63, 1.65) | 0.93 |
| PPB | 740 | 0.01 (−0.11, 0.14) | 0.85 | 666 | 0.61 (0.41, 0.91) | 0.01** | 671 | 0.96 (0.65, 1.41) | 0.82 |
2,4-DCP: 2,4-dichlorophenol; 2,5-DCP: 2,5-dichlorophenol; BP-3: Benzophenone; TCS: Triclosan; TCC: Triclocarban; EPB: Ethyl-paraben; MPB: Methyl-paraben; BPB: Butyl-paraben; PPB: Propyl-paraben
Models adjusted for specific gravity, maternal age, insurance type, alcohol use, and exposure to second-hand smoking.
Categorical variable.
3.4. Small for Gestational Age (SGA)
Average triclosan was associated with a 70% increased odds of SGA (OR/IQR 1.70; 95% CI: 1.06, 2.73); average 2,4-dichlorophenol was associated with a suggestive 32% increased odds of SGA (OR/IQR 1.32; 95% CI: 0.95, 1.84). Methyl-, butyl- and propyl-paraben were all associated with a 34-50% decrease in the odds of SGA [(OR/IQR 0.66; 95% CI: 0.47, 0.93); (OR/IQR 0.50; 95% CI: 0.28, 0.88); (OR/IQR 0.61; 95% CI: 0.41, 0.91), respectively].
After stratification of the results by study visit (Table 6), BPS was significantly associated with 82% increased odds of SGA at visit 3 (OR/IQR 1.82; 95% CI: 1.17, 2.84). Associations between parabens and SGA by study visit differed slightly by the type of paraben. There was no difference in association between SGA and methyl-paraben across the three time points. Associations between butyl-paraben and SGA was only significant at visit 2 and visit 3 [(OR/IQR 0.47; 95% CI: 0.26, 0.84) and (OR/IQR 0.51; 95% CI: 0.28, 0.91), respectively], while propyl-paraben was associated with a decrease in the odds of SGA at visit 1 and visit 3 [(OR/IQR 0.58; 95% CI: 0.38, 0.97); (OR/IQR 0.53; 95% CI: 0.32, 0.87), respectively]. Associations between triclosan and 2,4-dichlorophenol with SGA were significant at 20-24 weeks [(OR/IQR 1.51; 95% CI: 0.95, 2.42) and (OR/IQR 1.34; 95% CI: 0.96, 1.85), respectively]. Fetal sex did not modify any of the associations with SGA; interaction terms between biomarkers and fetal sex were all above 0.05.
Table 6:
Adjusteda change in birth weight z-scores or odds in relation to exposure biomarker concentration, stratified by visit during pregnancy. Effect estimates presented as change or odds ratio for IQR increase in exposure biomarker concentration.
| Birthweight | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (16-20 weeks) | Visit 2 (20-24 weeks) | Visit 3 (24-28 weeks) | |||||||
| N | Z-score change (95% CI) | p | N | Z-score change (95% CI) | p | N | Z-score change (95% CI) | p | |
| 2,4-DCP | 603 | −0.04 (−0.15, 0.08) | 0.52 | 613 | −0.01 (−0.12, 0.10) | 0.88 | 462 | −0.04 (−0.18, 0.10) | 0.59 |
| 2,5-DCP | 602 | −0.04 (−0.15, 0.08) | 0.53 | 613 | 0.02 (−0.09, 0.13) | 0.73 | 464 | 0.00 (−0.12, 0.13) | 0.94 |
| BPA | 597 | 0.01 (−0.12, 0.13) | 0.92 | 615 | 0.05 (−0.07, 0.18) | 0.41 | 462 | −0.05 (−0.20, 0.10) | 0.51 |
| BPFa | 379 | 0.04 (−0.20, 0.28) | 0.73 | 379 | −0.20 (−0.43, 0.04) | 0.10 | 289 | −0.14 (−0.42, 0.14) | 0.33 |
| BPS | 418 | 0.08 (−0.07, 0.24) | 0.28 | 433 | 0.03 (−0.13, 0.18) | 0.73 | 325 | 0.02 (−0.15, 0.19) | 0.80 |
| BP-3 | 601 | 0.06 (−0.06, 0.18) | 0.31 | 612 | 0.10 (−0.02, 0.22) | 0.12 | 462 | 0.06 (−0.07, 0.20) | 0.35 |
| TCS | 599 | −0.02 (−0.17, 0.13) | 0.79 | 614 | −0.11 (−0.26, 0.04) | 0.15 | 468 | −0.03 (−0.20, 0.14) | 0.76 |
| TCC | 422 | −0.11 (−0.31, 0.09) | 0.28 | 432 | −0.07 (−0.26, 0.13) | 0.49 | 324 | −0.02 (−0.23, 0.20) | 0.88 |
| EPBa | 424 | −0.05 (−0.28, 0.17) | 0.64 | 435 | −0.08 (−0.30, 0.14) | 0.46 | 326 | −0.20 (−0.45, 0.05) | 0.12 |
| MPB | 600 | 0.03 (−0.10, 0.16) | 0.67 | 614 | −0.01 (−0.13, 0.12) | 0.93 | 467 | 0.03 (−0.11, 0.18) | 0.65 |
| BPB | 594 | −0.04 (−0.18, 0.11) | 0.62 | 611 | 0.12 (−0.02, 0.26) | 0.08* | 466 | 0.11 (−0.04, 0.27) | 0.15 |
| PPB | 600 | 0.04 (−0.11, 0.18) | 0.60 | 614 | 0.00 (−0.13, 0.14) | 0.96 | 467 | 0.04 (−0.12, 0.20) | 0.63 |
| SGA | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (16-20 weeks) | Visit 2 (20-24 weeks) | Visit 3 (24-28 weeks) | |||||||
| N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | |
| 2,4-DCP | 530 | 1.15 (0.82, 1.60) | 0.41 | 547 | 1.34 (0.96, 1.85) | 0.08* | 431 | 1.36 (0.90, 2.05) | 0.14 |
| 2,5-DCP | 529 | 1.03 (0.73, 1.46) | 0.87 | 547 | 1.24 (0.89, 1.72) | 0.20 | 433 | 1.23 (0.86, 1.75) | 0.25 |
| BPA | 524 | 1.02 (0.71, 1.47) | 0.90 | 549 | 1.07 (0.73, 1.55) | 0.74 | 431 | 1.12 (0.74, 1.69) | 0.59 |
| BPFa | 444 | 1.00 (0.53, 1.89) | 0.99 | 444 | 1.00 (0.53, 1.89) | 0.99 | 444 | 1.00 (0.53, 1.89) | 0.99 |
| BPS | 369 | 0.91 (0.57, 1.46) | 0.70 | 389 | 1.40 (0.89, 2.22) | 0.14 | 304 | 1.82 (1.17, 2.84) | 0.01** |
| BP-3 | 528 | 1.07 (0.74, 1.55) | 0.70 | 547 | 0.99 (0.67, 1.49) | 0.98 | 431 | 0.69 (0.44, 1.08) | 0.11 |
| TCS | 526 | 1.44 (0.92, 2.26) | 0.11 | 548 | 1.51 (0.95, 2.42) | 0.08* | 435 | 1.15 (0.69, 1.91) | 0.60 |
| TCC | 373 | 0.85 (0.46, 1.56) | 0.59 | 389 | 1.06 (0.58, 1.94) | 0.85 | 304 | 0.81 (0.43, 1.52) | 0.51 |
| EPBa | 489 | 1.57 (0.86, 2.89) | 0.15 | 489 | 1.57 (0.86, 2.89) | 0.15 | 489 | 1.57 (0.86, 2.89) | 0.15 |
| MPB | 527 | 0.61 (0.42, 0.90) | 0.01** | 549 | 0.68 (0.45, 1.02) | 0.06* | 435 | 0.66 (0.43, 1.01) | 0.06* |
| BPB | 522 | 0.76 (0.48, 1.20) | 0.24 | 547 | 0.47 (0.26, 0.84) | 0.01** | 433 | 0.51 (0.28, 0.91) | 0.02** |
| PPB | 527 | 0.58 (0.38, 0.91) | 0.02** | 548 | 0.81 (0.52, 1.27) | 0.37 | 435 | 0.53 (0.32, 0.87) | 0.01** |
| LGA | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 (16-20 weeks) | Visit 2 (20-24 weeks) | Visit 3 (24-28 weeks) | |||||||
| N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | N | OR/IQR change (95% CI) | p | |
| 2,4-DCP | 535 | 1.06 (0.75, 1.50) | 0.73 | 556 | 1.05 (0.76, 1.47) | 0.76 | 425 | 1.07 (0.68, 1.68) | 0.76 |
| 2,5-DCP | 534 | 1.02 (0.72, 1.45) | 0.90 | 556 | 1.15 (0.83, 1.60) | 0.39 | 427 | 1.06 (0.72, 1.56) | 0.78 |
| BPA | 529 | 0.85 (0.59, 1.24) | 0.40 | 558 | 1.22 (0.86, 1.72) | 0.26 | 425 | 0.88 (0.56, 1.40) | 0.60 |
| BPFa | 446 | 0.69 (0.36, 1.32) | 0.26 | 446 | 0.69 (0.36, 1.32) | 0.26 | 446 | 0.69 (0.36, 1.32) | 0.26 |
| BPS | 370 | 1.49 (0.99, 2.25) | 0.06* | 396 | 1.33 (0.88, 2.01) | 0.18 | 299 | 1.46 (0.86, 2.49) | 0.16 |
| BP-3 | 533 | 1.34 (0.96, 1.89) | 0.09* | 555 | 1.52 (1.09, 2.13) | 0.01** | 425 | 1.00 (0.67, 1.51) | 0.98 |
| TCS | 531 | 1.26 (0.81, 1.96) | 0.31 | 557 | 0.77 (0.49, 1.22) | 0.27 | 430 | 1.05 (0.61, 1.82) | 0.85 |
| TCC | 374 | 0.99 (0.55, 1.76) | 0.97 | 395 | 1.10 (0.63, 1.91) | 0.73 | 299 | 0.73 (0.37, 1.43) | 0.36 |
| EPBa | 492 | 1.25 (0.68, 2.30) | 0.47 | 492 | 1.25 (0.68, 2.30) | 0.47 | 492 | 1.25 (0.68, 2.30) | 0.47 |
| MPB | 532 | 1.02 (0.69, 1.50) | 0.94 | 557 | 1.03 (0.69, 1.54) | 0.88 | 430 | 0.99 (0.62, 1.56) | 0.95 |
| BPB | 527 | 0.88 (0.58, 1.35) | 0.56 | 557 | 1.08 (0.72, 1.61) | 0.72 | 428 | 1.21 (0.75, 1.95) | 0.43 |
| PPB | 532 | 1.09 (0.70, 1.70) | 0.69 | 557 | 1.22 (0.81, 1.86) | 0.34 | 430 | 0.91 (0.53, 1.55) | 0.73 |
2,4-DCP: 2,4-dichlorophenol; 2,5-DCP: 2,5-dichlorophenol; BP-3: Benzophenone; TCS: Triclosan; TCC: Triclocarban; EPB: Ethyl-paraben; MPB: Methyl-paraben; BPB: Butyl-paraben; PPB: Propyl-paraben
Models adjusted for specific gravity, maternal age, insurance type, alcohol use, and exposure to second-hand smoking.
Categorical variable.
3.5. Large for Gestational age (LGA)
Average BPS and BP-3 concentrations were associated with an increased odds of LGA [(OR/IQR 1.62; 95% CI: 1.06, 2.45) and (OR/IQR 1.38; 95% CI: 0.99, 1.93), respectively]. The association between BPS and SGA was strongest at study visit 1 (OR/IQR 1.49; 95% CI: 0.99, 2.25), whereas the association between BP-3 and LGA was strongest at study visit 2 (OR/IQR 1.52; 95% CI: 1.09, 2.13). Fetal sex did not modify any of the associations with LGA; interaction terms between biomarkers and fetal sex were all above 0.10.
4. Discussion
Urinary concentrations of benzophenone-3, methyl-paraben and propyl-paraben measured at up to 3 times during pregnancy were associated with an increase in gestational age. Urinary BPA concentrations at 16-20 weeks were also associated with a suggestive increase in gestational age. Triclocarban was associated with a suggestive decrease in gestational age, while the relationship between triclosan and gestational age differed by infant sex. PTB results mirrored gestational age results, with the addition of a decrease in the odds of PTB in association with BPF at 24-28 weeks gestation. No exposure biomarkers were associated with birth weight; however 2,4-dichlorophenol, triclosan and BPS were associated with an increase in the odds of SGA, while parabens were associated with a decrease in the odds of SGA. BP-3 and BPS were also associated with an increase in the odds of LGA.
Benzophenone-3 was consistently associated with an increase in gestational age at all study visits and in both sexes in this study. However, in contrast to our results, a previous study reported a decrease in gestational age in association with urinary benzophenone-3 concentrations at delivery in 567 infants (Tang et al., 2013). We could not identify other studies that examined the effect of benzophenone-3 on gestational age, but did identify studies that reported associations between benzophenone-3 and other gestation growth parameters. Philippat et al. reported an increase in birth weight and head circumference in association with benzophenone-3 among 520 male infants in France (Philippat et al., 2012, 2014), whereas Wolff et al. found an increase in birth weight among boys and a decrease in birth weight among girls in a cohort of 404 pregnant women in New York City (Wolff et al., 2008).
Benzophenone-3 was also associated with a decrease in the abdominal circumference among boys, and a suggestive increase in abdominal circumference among females in a cohort of 476 women in Boston (Ferguson et al., 2018). The reported increases in gestational growth parameters in association with benzophenone-3 are consistent with our finding of an increased odds of LGA with benzophenone-3.
The biological mechanisms involved in the observed associations between benzophenone-3 and birth outcomes are unclear. Benzophenone-3 exhibits estrogenic activity and can bind to estrogen receptors α and β, as well as other estrogen-related receptors (Krause et al., 2012). Therefore, an endocrine-mediated mechanism could potentially be leading to the increase in gestational age. Alternatively, BP-3 was associated with lower concentrations of pro-inflammatory markers in a large pregnancy cohort (Aung et al., 2019) which may also impact duration of pregnancy.
Methyl- and propyl-paraben were also associated with an increase in gestational age in this study, particularly at 16-20 weeks gestation, in addition to a decreased odds of SGA. One other study looked into the effect of parabens on gestational age. Geer et al. reported a decrease in gestational age in association with maternal urinary butyl-paraben at the third trimester, and a protective effect on PTB in association with cord blood propyl-paraben (but no effect on gestational age) in a small (N=185) immigrant population in New York (Geer et al., 2017). Although we did not identify any associations between butyl-paraben and gestational age, we did observe a decrease in the odds of PTB with urinary propyl-paraben concentrations, which was similar to the results observed in the New York study. With regards to other growth parameters, parabens, including methyl-paraben and propyl-paraben, were associated with an increase in birth weight among boys (Philippat et al., 2014; Wu et al., 2017). A large Chinese cohort (N=1006) also reported an increase in birth length in association with methyl-paraben in boys (Wu et al., 2017). We observed a similar association between butyl-paraben and an increase in birthweight, as well as a protective effect of parabens on SGA; however, the associations were not specific to infant sex. Parabens have demonstrated endocrine disrupting effects (Vo et al., 2011; Watanabe et al., 2013; Wróbel and Gregoraszczuk, 2014), and have been associated with changes in estriol, progesterone, sex-hormone binding globulin, and thyroid-stimulating hormone in this cohort (Aker el al., in press). These potential effects on hormone levels may play a role in the relationships between parabens and birth outcomes, though more research is needed to help clarify relevant biological mechanisms. Butyl-paraben has also been shown to activate PPARγ and increase adipogenesis, which could explain the decrease in the odds of SGA, although only butyl-paraben was included in this in vitro study (Taxvig et al., 2012).
In the current study, BPA was associated with a suggestive increase in pregnancy duration, particularly for urinary measures at 16-20 weeks gestation. One study did observe an increase in gestational age with maternal plasma BPA levels, particularly among female infants (Veiga-Lopez et al., 2015). The plasma was analyzed during early pregnancy, which is reflective of the timing of our study visit 1; however it is difficult to compare BPA concentrations in plasma versus urine. In contrast, other studies have found a decrease in gestational age in association with BPA. Urinary BPA at the third trimester was found to increase preterm birth in a nested case-control study conducted in Mexico (Cantonwine et al., 2015). Another nested case-control study found that maternal plasma BPA concentrations at time of delivery were associated with preterm birth, although interestingly, amniotic fluid BPA concentrations were not (Behnia et al., 2016). Three more cross-sectional studies looked at BPA levels at delivery, two of which reported a decrease in gestational age, particularly among male infants (Tang et al., 2013; Weinberger et al., 2014), and one that reported no association between BPA and gestation age among 496 mother-infant pairs (Ding et al., 2017). It is important to note the difference in the timing of exposure assessment between past studies and our current study. Our study looked at earlier time points of BPA exposure, so it is possible that the differences in our results could be attributed to this difference in timing of the exposure measures, and possibly indicating a susceptible window of exposure. There are also noted differences in urine versus plasma BPA concentrations, with some possible bias in measuring plasma BPA concentrations as an exposure proxy given the high potential for contamination (Cho et al., 2017). This difference in measurement could also explain the differences in our results.
BPS was associated with an increased odds of both SGA and LGA, depending on the timing of exposure. While BPS concentrations at 16-20 weeks were associated with LGA, BPS concentrations at 24-28 weeks were associated with SGA. We did not identify any other studies that reported associations between BPS and SGA or LGA; however, similar to our results, two cohort studies found no association between BPS and overall birth weight (Ferguson et al., 2018; Wan et al., 2018). This difference in the potential effect on the size of the fetus could be attributed to the transient hormonal levels present throughout the different stages of pregnancy. For example, in a previous study by our group, BPS was associated with changes to thyroid-stimulating hormone and corticotropin-releasing hormone at different time points in pregnancy (Aker et al., in press). Although the increase in both SGA and LGA in association with BPS differed by time point, these results are difficult to explain. Therefore, we caution over-interpretation of these results until these association are studied in other cohorts, and experimental studies help to better understand the biological mechanisms by which BPS may impact birth outcomes.
We identified a relationship between triclosan and gestational age that differs by the sex of the infant, and an increase in the odds of SGA with urinary triclosan. There was an increase in gestational age among boys, and a suggestive decrease in gestational age among females. In fact, four other studies observed associations between triclosan and birth outcomes among only boys (Ferguson et al., 2018; Lassen et al., 2016; Philippat et al., 2014; Wolff et al., 2008). The sex-specific effects observed could be attributed to sex hormone-specific targets of triclosan in the developing fetus. For example, triclosan was associated with an increase in maternal testosterone in this cohort (Aker et al., in press), which may impact the developing male fetus differently than the female fetus. Another birth cohort of 376 mother-infant pairs in Cincinnati collected urine at 16 and 26 weeks pregnancy (Etzel et al., 2017). Average triclosan concentrations were associated with a decrease in gestational age, but was not modified by infant sex. A large cohort study in China including over 1000 pregnant women found no association between urinary triclosan concentrations and gestational age after confounder adjustment (Huo et al., 2018). There were also no differences by infant sex. Differences in our results could be due to the difference in the timing of triclosan exposure as the Chinese study measured urinary triclosan just prior to delivery. Differences may also be due to the lower urinary triclosan concentrations in comparison to our cohort. Several other studies also reported no association between triclosan and birth outcomes, including gestational age (Ding et al., 2017; Geer et al., 2017; Philippat et al., 2012; Wolff et al., 2008). However, our triclosan concentrations were 3-20 times higher than the concentrations reported in these studies.
Similar to our results, no association was observed between triclosan and birth weight in two large prospective cohorts of pregnant Chinese women (Ding et al., 2017; Huo et al., 2018). A study on a cohort of 378 mother-infant pairs in Ohio did observe a decrease in birth weight, birth length and head circumference with a 10-fold increase in urinary triclosan (Etzel et al., 2017). While we did not observe any effects in birth weight, results in the Ohio cohort could be consistent with an increase in SGA, as we observed in our cohort. Conversely, another large (N=620) Chinese cohort identified an increase in the birth weight of newborns among females (Ouyang et al., 2018). However, that study modeled birth weight, and included gestational age as a covariate in the model, as opposed to our gestational age-adjusted z-scores. This difference in statistical methods may partially explain some the differences in our results.
A small study (N=185) reported no association between third trimester maternal urine triclosan concentrations and gestational age in an immigrant population in New York, but did find a significant decrease in gestational age with an increase in triclocarban neonatal cord blood plasma (N=34) (Geer et al., 2017). This is similar to our finding of a suggestive decrease in gestational age in association with average urinary triclocarban, where we also found stronger associations with triclocarban measured earlier in pregnancy. To our knowledge, no other studies reported associations between triclocarban and gestational age. Triclocarban concentrations in PROTECT were exceptionally high compared to other studies (Ashrap et al., 2018). The median urinary concentrations of triclocarban in the U.S. National Health and Nutrition Examination Survey (NHANES) in 2013-2014 was < LOD (0.1 μg/L), and 0.2 μg/L was the 75th percentile (Ye et al., 2016). Our cohort, on the other hand, had a median of 2.3 μg/L and a 75th percentile of 26.8 μg/L. Similarly, a recent review reported a relatively low detection (4-25%) of urinary triclocarban in Canada, Greece and Denmark (Rochester et al., 2017). This points to the variability of exposure to triclocarban worldwide. Our findings and previous studies suggest an association between triclocarban and birth outcomes (Rochester et al., 2017). Therefore, additional studies will be useful to better understand these associations and potential mechanisms of action.
While there was some consistency between our results and other studies, the differences with regards to observed associations, as well as the directions of association make the interpretations of results across studies difficult. However, this also may indicate the importance of 1) the timing of exposure on birth outcomes, 2) the methodological techniques used in analyzing exposure and outcome, and perhaps most importantly, 3) the undefined confounders and/or modifiers that may exist from one population to the other. Future studies should attempt to explore other factors that may interact with these chemicals that could explain the differences observed across cohorts.
Our study had a few limitations. While data at three time points are a great improvement from the more common cross-sectional study design, it may not be sufficient to understand the effects of these biomarkers on gestational age. The variation of concentrations of these exposure biomarkers over time may also introduce potential bias, stemming from random measurement error, but most likely towards the null. We also had a smaller sample size for some of the emerging phenols of concern, such as BPA replacement chemicals, as these were added to the analytical panel part-way through the study. Finally, given the multiple comparisons conducted, there is a possibility of chance findings due to Type I error.
Our study also had many strengths, including a robust sample size and the collection of exposure biomarkers data at three time points during pregnancy to help account for the chemicals’ short lifespan in the body and likely episodic nature of the exposures, as previously reported (Ashrap et al., 2018) The repeated measures also allowed us to explore potential windows of susceptibility for these associations. Additionally, our urinary biomarker panel included triclocarban, BPS and BPF, all of which have not been well studied in the current literature. Finally, the relatively high biomarkers concentrations in our cohort, particularly triclocarban, triclosan and BPF, provides as opportunity to study the potential effects of these chemicals in a vulnerable human population. The results of this study add evidence to the possibility of an influence by exposure to phenols and parabens on birth outcomes. Further studies are needed to better understand how they impact birth outcomes, but in the meantime advising parents on simple ways to reduce exposure to these chemicals is warranted.
5. Conclusion
Our study showed a significant association between triclocarban, and select phenols and parabens in association with gestational age and SGA. In particular, benzophenone-3, BPA, methyl- and propylparaben were associated with an increase in gestational age, while triclocarban was associated with a suggestive decrease in gestational age. Urinary biomarker concentrations at the earliest time point, 16-20 weeks gestation, may be a susceptible window of exposure for triclocarban and other chemicals.Triclosan, BPF and BPS were associated with an increase in SGA, whereas parabens were associated with a decrease in SGA. The association between triclosan and gestational age differed by infant sex, wherein triclosan was associated with an increase in gestational age among males, and a suggestive decrease in gestational age among females. These associations should be verified in further studies with repeated measures of exposure.
Supplementary Material
Highlights.
Biomarker concentrations were measured at three time points in pregnant women
Benzophenone-3 was associated with an increase in gestational age
Methylparaben and propylparaben were associated with an increase in gestational age
Triclocarban was associated with a decrease in gestational age
Fetal sex and study visit moderated some associations
Acknowledgements:
We gratefully acknowledge Antonia Calafat and Xiaoyun Ye at the U.S. Centers for Disease Control and Prevention for the quantification of urinary phenols, parabens and triclocarban concentrations. This work was supported by the National Institute of Environmental Health Sciences, National Institutes of Health (Grants P42ES017198, P50ES026049, and UG3OD023251), and for RedCap by U54 MD007600 from the National Institute on Minority Health and Health Disparities.
Funding Sources: This work was supported by the National Institute of Environmental Health Sciences, National Institutes of Health (Grants P42ES017198, P50ES026049, and UG3OD023251), and for RedCap by U54 MD007600 from the National Institute on Minority Health and Health Disparities.
Review by an IRB: This study was approved by the research and ethics committees of the University Of Michigan School Of Public Health, University of Puerto Rico, Northeastern University and the University of Georgia. All study participants provided full informed consent prior to participation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 2017 Premature Birth Report Card: Puerto Rico, 2017. . March of Dimes. [Google Scholar]
- Aker AM, Watkins DJ, Johns LE, Ferguson KK, Soldin OP, Anzalota Del Toro LV, Alshawabkeh AN, Cordero JF, Meeker JD, 2016. Phenols and parabens in relation to reproductive and thyroid hormones in pregnant women. Environ. Res 151, 30–37. 10.1016/j.envres.2016.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashrap P, Watkins DJ, Calafat AM, Ye X, Rosario Z, Brown P, Vélez-Vega CM, Alshawabkeh A, Cordero JF, Meeker JD, 2018. Elevated concentrations of urinary triclocarban, phenol and paraben among pregnant women in Northern Puerto Rico: Predictors and trends. Environ. Int 10.1016/j.envint.2018.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aung MT, Ferguson KK, Cantonwine DE, Bakulski KM, Mukherjee B, Loch-Caruso R, McElrath TF, Meeker JD, 2019. Associations between maternal plasma measurements of inflammatory markers and urinary levels of phenols and parabens during pregnancy: A repeated measures study. Sci. Total Environ 650, 1131–1140. 10.1016/j.scitotenv.2018.08.356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnia F, Peltier M, Getahun D, Watson C, Saade G, Menon R, 2016. High bisphenol A (BPA) concentration in the maternal, but not fetal, compartment increases the risk of spontaneous preterm delivery. J. Matern.-Fetal Neonatal Med. Off. J. Eur. Assoc. Perinat. Med. Fed. Asia Ocean. Perinat. Soc. Int. Soc. Perinat. Obstet. 1–7. 10.3109/14767058.2016.1139570 [DOI] [PubMed] [Google Scholar]
- Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller A-B, Kinney M, Lawn J, 2013. Born Too Soon: The global epidemiology of 15 million preterm births. Reprod. Health 10, S2 10.1186/1742-4755-10-S1-S2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boas M, Main KM, Feldt-Rasmussen U, 2009. Environmental chemicals and thyroid function: an update. Curr. Opin. Endocrinol. Diabetes Obes 16, 385–391. 10.1097/MED.0b013e3283305af7 [DOI] [PubMed] [Google Scholar]
- Cantonwine DE, Cordero JF, Rivera-González LO, Anzalota Del Toro LV, Ferguson KK, Mukherjee B, Calafat AM, Crespo N, Jiménez-Vélez B, Padilla IY, Alshawabkeh AN, Meeker JD, 2014. Urinary phthalate metabolite concentrations among pregnant women in Northern Puerto Rico: Distribution, temporal variability, and predictors. Environ. Int 62, 1–11. 10.1016/j.envint.2013.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantonwine DE, Ferguson KK, Mukherjee B, McElrath TF, Meeker JD, 2015. Urinary Bisphenol A Levels during Pregnancy and Risk of Preterm Birth. Environ. Health Perspect 123, 895–901. 10.1289/ehp.1408126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BM, 2006. Subclinical Hypothyroidism and Pregnancy: Obstet. Gynecol. Surv 61, 415–420. 10.1097/01.ogx.0000223331.51424.9b [DOI] [PubMed] [Google Scholar]
- Castracane VD, 2000. Endocrinology of preterm labor. Clin. Obstet. Gynecol 43, 717–726. [DOI] [PubMed] [Google Scholar]
- Caughey AB, Stotland NE, Washington AE, Escobar GJ, 2007. Maternal and obstetric complications of pregnancy are associated with increasing gestational age at term. Am. J. Obstet. Gynecol 196, 155e1–6. 10.1016/j.ajog.2006.08.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2015. Preterm Birth ∣ Maternal and Infant Health ∣ Reproductive Health ∣ CDC [WWW Document]. Preterm Birth URL http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm (accessed 2.8.16).
- Cho SH, Choi Y, Kim SH, Kim SJ, Chang J, 2017. Urinary bisphenol A versus serum bisphenol A concentration and ovarian reproductive outcomes among IVF patients: Which is a better biomarker of BPA exposure? Mol. Cell. Toxicol 13, 351–359. 10.1007/s13273-017-0039-0 [DOI] [Google Scholar]
- Committee on Obstetric Practice, the American Institute of Ultrasound in Medicine, and the Society for Maternal-Fetal Medicine, 2017. Committee Opinion No 700: Methods for Estimating the Due Date. Obstet. Gynecol 129, e150–e154. 10.1097/AOG.0000000000002046 [DOI] [PubMed] [Google Scholar]
- Ding G, Wang C, Vinturache A, Zhao S, Pan R, Han W, Chen L, Wang W, Yuan T, Gao Y, Tian Y, 2017. Prenatal low-level phenol exposures and birth outcomes in China. Sci. Total Environ 607–608, 1400–1407. 10.1016/j.scitotenv.2017.07.084 [DOI] [PubMed] [Google Scholar]
- Etzel TM, Calafat AM, Ye X, Chen A, Lanphear BP, Savitz DA, Yolton K, Braun JM, 2017. Urinary triclosan concentrations during pregnancy and birth outcomes. Environ. Res 156, 505–511. 10.1016/j.envres.2017.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fact Sheet Puerto Rico: Fast Facts, 2017. . The Henry J. Kaiser Family Foundation, Menlo Park, CA. [Google Scholar]
- Ferguson KK, Meeker JD, Cantonwine DE, Mukherjee B, Pace GG, Weller D, McElrath TF, 2018. Environmental phenol associations with ultrasound and delivery measures of fetal growth. Environ. Int 112, 243–250. 10.1016/j.envint.2017.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galal M, Symonds I, Murray H, Petraglia F, Smith R, 2012. Postterm pregnancy. Facts Views Vis. ObGyn 4, 175–187. [PMC free article] [PubMed] [Google Scholar]
- Geer LA, Pycke BFG, Waxenbaum J, Sherer DM, Abulafia O, Halden RU, 2017. Association of birth outcomes with fetal exposure to parabens, triclosan and triclocarban in an immigrant population in Brooklyn, New York. J. Hazard. Mater, Special Issue on Emerging Contaminants in engineered and natural environment 323, Part A, 177–183. 10.1016/j.jhazmat.2016.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, Osterman MJK, Curtin SC, Matthews TJ, 2015. Births: Final Data for 2014. Natl. Vital Stat. Rep. Cent. Dis. Control Prev. Natl. Cent. Health Stat. Natl. Vital Stat. Syst 64, 1–64. [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, 2009. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform 42, 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornung RW, Reed LD, 1990. Estimation of Average Concentration in the Presence of Nondetectable Values. Appl. Occup. Environ. Hyg 5, 46–51. 10.1080/1047322X.1990.10389587 [DOI] [Google Scholar]
- Huo W, Xia W, Wu C, Zhu Y, Zhang B, Wan Y, Zhou A, Qian Z, Chen Z, Jiang Y, Liu H, Hu J, Xu B, Xu S, Li Y, 2018. Urinary level of triclosan in a population of Chinese pregnant women and its association with birth outcomes. Environ. Pollut. Barking Essex 1987 233, 872–879. 10.1016/j.envpol.2017.08.073 [DOI] [PubMed] [Google Scholar]
- Kemp MW, 2014. Preterm Birth, Intrauterine Infection, and Fetal Inflammation. Front. Immunol 5 10.3389/fimmu.2014.00574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koeppe ES, Ferguson KK, Colacino JA, Meeker JD, 2013. Relationship between urinary triclosan and paraben concentrations and serum thyroid measures in NHANES 2007-2008. Sci. Total Environ 445–446, 299–305. 10.1016/j.scitotenv.2012.12.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolatorova L, Vitku J, Hampl R, Adamcova K, Skodova T, Simkova M, Parizek A, Starka L, Duskova M, 2018. Exposure to bisphenols and parabens during pregnancy and relations to steroid changes. Environ. Res 163, 115–122. 10.1016/j.envres.2018.01.031 [DOI] [PubMed] [Google Scholar]
- Krause M, Klit A, Blomberg Jensen M, Søeborg T, Frederiksen H, Schlumpf M, Lichtensteiger W, Skakkebaek NE, Drzewiecki KT, 2012. Sunscreens: are they beneficial for health? An overview of endocrine disrupting properties of UV-filters. Int. J. Androl 35, 424–436. 10.1111/j.1365-2605.2012.01280.x [DOI] [PubMed] [Google Scholar]
- Kumar P, Magon N, 2012. Hormones in pregnancy. Niger. Med. J. J. Niger. Med. Assoc 53, 179 10.4103/0300-1652.107549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassen TH, Frederiksen H, Kyhl HB, Swan SH, Main KM, Andersson A-M, Lind DV, Husby S, Wohlfahrt-Veje C, Skakkebæk NE, Jensen TK, 2016. Prenatal Triclosan Exposure and Anthropometric Measures including Anogenital Distance in Danish Infants. Environ. Health Perspect 10.1289/ehp.1409637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE, 2012. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. The Lancet 379, 2151–2161. 10.1016/S0140-6736(12)60560-1 [DOI] [PubMed] [Google Scholar]
- Luu TM, Katz SL, Leeson P, Thébaud B, Nuyt A-M, 2015. Preterm birth: risk factor for early-onset chronic diseases. CMAJ Can. Med. Assoc. J. J. Assoc. Medicale Can 10.1503/cmaj.150450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlow N, Wolke D, Bracewell MA, Samara M, 2005. Neurologic and Developmental Disability at Six Years of Age after Extremely Preterm Birth. N. Engl. J. Med 352, 9–19. 10.1056/NEJMoa041367 [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, Munson ML, Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System, 2007. Births: final data for 2005. Natl. Vital Stat. Rep. Cent. Dis. Control Prev. Natl. Cent. Health Stat. Natl. Vital Stat. Syst 56, 1–103. [PubMed] [Google Scholar]
- McCormick MC, 1985. The contribution of low birth weight to infant mortality and childhood morbidity. N. Engl. J. Med 312, 82–90. 10.1056/NEJM198501103120204 [DOI] [PubMed] [Google Scholar]
- Meeker JD, Cantonwine DE, Rivera-González LO, Ferguson KK, Mukherjee B, Calafat AM, Ye X, Anzalota Del Toro LV, Crespo-Hernández N, Jiménez-Vélez B, Alshawabkeh AN, Cordero JF, 2013. Distribution, variability, and predictors of urinary concentrations of phenols and parabens among pregnant women in Puerto Rico. Environ. Sci. Technol 47, 3439–3447. 10.1021/es400510g [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neier K, Marchlewicz EH, Dolinoy DC, Padmanabhan V, 2015. Assessing Human Health Risk to Endocrine Disrupting Chemicals: a Focus on Prenatal Exposures and Oxidative Stress. Endocr. Disruptors Austin Tex 3 10.1080/23273747.2015.1069916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang F, Tang N, Zhang H-J, Wang X, Zhao S, Wang W, Zhang J, Cheng W, 2018. Maternal urinary triclosan level, gestational diabetes mellitus and birth weight in Chinese women. Sci. Total Environ 626, 451–457. 10.1016/j.scitotenv.2018.01.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philippat C, Botton J, Calafat AM, Ye X, Charles M-A, Slama R, EDEN Study Group, 2014. Prenatal exposure to phenols and growth in boys. Epidemiol. Camb. Mass 25, 625–635. 10.1097/EDE.0000000000000132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philippat C, Mortamais M, Chevrier C, Petit C, Calafat AM, Ye X, Silva MJ, Brambilla C, Pin I, Charles M-A, Cordier S, Slama R, 2012. Exposure to phthalates and phenols during pregnancy and offspring size at birth. Environ. Health Perspect 120, 464–470. 10.1289/ehp.1103634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochester JR, Bolden AL, 2015. Bisphenol S and F: A Systematic Review and Comparison of the Hormonal Activity of Bisphenol A Substitutes. Environ. Health Perspect 123, 643–650. 10.1289/ehp.1408989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochester JR, Bolden AL, Pelch KE, Kwiatkowski CF, 2017. Potential Developmental and Reproductive Impacts of Triclocarban: A Scoping Review. J. Toxicol 2017. 10.1155/2017/9679738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoen CN, Tabbah S, Iams JD, Caughey AB, Berghella V, 2015. Why the United States preterm birth rate is declining. Am. J. Obstet. Gynecol 213, 175–180. 10.1016/j.ajog.2014.12.011 [DOI] [PubMed] [Google Scholar]
- Smith R, Smith JI, Shen X, Engel PJ, Bowman ME, McGrath SA, Bisits AM, McElduff P, Giles WB, Smith DW, 2009. Patterns of plasma corticotropin-releasing hormone, progesterone, estradiol, and estriol change and the onset of human labor. J. Clin. Endocrinol. Metab 94, 2066–2074. 10.1210/jc.2008-2257 [DOI] [PubMed] [Google Scholar]
- Tang R, Chen M-J, Ding G-D, Chen X-J, Han X-M, Zhou K, Chen L-M, Xia Y-K, Tian Y, Wang X-R, 2013. Associations of prenatal exposure to phenols with birth outcomes. Environ. Pollut. Barking Essex 1987 178, 115–120. 10.1016/j.envpol.2013.03.023 [DOI] [PubMed] [Google Scholar]
- Taxvig C, Dreisig K, Boberg J, Nellemann C, Schelde AB, Pedersen D, Boergesen M, Mandrup S, Vinggaard AM, 2012. Differential effects of environmental chemicals and food contaminants on adipogenesis, biomarker release and PPARγ activation. Mol. Cell. Endocrinol 361, 106–115. 10.1016/j.mce.2012.03.021 [DOI] [PubMed] [Google Scholar]
- Valdez R, Athens MA, Thompson GH, Bradshaw BS, Stern MP, 1994. Birthweight and adult health outcomes in a biethnic population in the USA. Diabetologia 37, 624–631. [DOI] [PubMed] [Google Scholar]
- Veiga-Lopez A, Kannan K, Liao C, Ye W, Domino SE, Padmanabhan V, 2015. Gender-Specific Effects on Gestational Length and Birth Weight by Early Pregnancy BPA Exposure. J. Clin. Endocrinol. Metab 100, E1394–1403. 10.1210/jc.2015-1724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villar J, Ismail LC, Victora CG, Ohuma EO, Bertino E, Altman DG, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, Gravett MG, Purwar M, Frederick IO, Noble AJ, Pang R, Barros FC, Chumlea C, Bhutta ZA, Kennedy SH, 2014. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. The Lancet 384, 857–868. 10.1016/S0140-6736(14)60932-6 [DOI] [PubMed] [Google Scholar]
- Vo TTB, Jung E-M, Choi K-C, Yu FH, Jeung E-B, 2011. Estrogen receptor α is involved in the induction of Calbindin-D(9k) and progesterone receptor by parabens in GH3 cells: a biomarker gene for screening xenoestrogens. Steroids 76, 675–681. 10.1016/j.steroids.2011.03.006 [DOI] [PubMed] [Google Scholar]
- Wan Y, Huo W, Xu S, Zheng T, Zhang B, Li Y, Zhou A, Zhang Y, Hu J, Zhu Y, Chen Z, Lu S, Wu C, Jiang M, Jiang Y, Liu H, Yang X, Xia W, 2018. Relationship between maternal exposure to bisphenol S and pregnancy duration. Environ. Pollut. Barking Essex 1987 238, 717–724. 10.1016/j.envpol.2018.03.057 [DOI] [PubMed] [Google Scholar]
- Watanabe Y, Kojima H, Takeuchi S, Uramaru N, Ohta S, Kitamura S, 2013. Comparative study on transcriptional activity of 17 parabens mediated by estrogen receptor α and β and androgen receptor. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc 57, 227–234. 10.1016/j.fct.2013.03.036 [DOI] [PubMed] [Google Scholar]
- Watkins DJ, Ferguson KK, Anzalota Del Toro LV, Alshawabkeh AN, Cordero JF, Meeker JD, 2015. Associations between urinary phenol and paraben concentrations and markers of oxidative stress and inflammation among pregnant women in Puerto Rico. Int. J. Hyg. Environ. Health 218, 212–219. 10.1016/j.ijheh.2014.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger B, Vetrano AM, Archer FE, Marcella SW, Buckley B, Wartenberg D, Robson MG, Klim J, Azhar S, Cavin S, Wang L, Rich DQ, 2014. Effects of maternal exposure to phthalates and bisphenol A during pregnancy on gestational age. J. Matern.-Fetal Neonatal Med. Off. J. Eur. Assoc. Perinat. Med. Fed. Asia Ocean. Perinat. Soc. Int. Soc. Perinat. Obstet 27, 323–327. 10.3109/14767058.2013.815718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff MS, Engel SM, Berkowitz GS, Ye X, Silva MJ, Zhu C, Wetmur J, Calafat AM, 2008. Prenatal phenol and phthalate exposures and birth outcomes. Environ. Health Perspect 116, 1092–1097. 10.1289/ehp.11007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wróbel AM, Gregoraszczuk EŁ, 2014. Actions of methyl-, propyl- and butylparaben on estrogen receptor-α and -β and the progesterone receptor in MCF-7 cancer cells and non-cancerous MCF-10A cells. Toxicol. Lett 230, 375–381. 10.1016/j.toxlet.2014.08.012 [DOI] [PubMed] [Google Scholar]
- Wu C, Huo W, Li Y, Zhang B, Wan Y, Zheng T, Zhou A, Chen Z, Qian M, Zhu Y, Jiang Y, Liu H, Hu J, Chen X, Xu B, Xia W, Xu S, 2017. Maternal urinary paraben levels and offspring size at birth from a Chinese birth cohort. Chemosphere 172, 29–36. 10.1016/j.chemosphere.2016.12.131 [DOI] [PubMed] [Google Scholar]
- Ye X, Bishop AM, Reidy JA, Needham LL, Calafat AM, 2006. Parabens as Urinary Biomarkers of Exposure in Humans. Environ. Health Perspect 114, 1843–1846. 10.1289/ehp.9413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X, Kuklenyik Z, Needham LL, Calafat AM, 2005. Quantification of urinary conjugates of bisphenol A, 2,5-dichlorophenol, and 2-hydroxy-4-methoxybenzophenone in humans by online solid phase extraction-high performance liquid chromatography-tandem mass spectrometry. Anal. Bioanal. Chem 383, 638–644. 10.1007/s00216-005-0019-4 [DOI] [PubMed] [Google Scholar]
- Ye X, Wong L-Y, Dwivedi P, Zhou X, Jia T, Calafat AM, 2016. Urinary Concentrations of the Antibacterial Agent Triclocarban in United States Residents: 2013–2014 National Health and Nutrition Examination Survey. Environ. Sci. Technol 50, 13548–13554. 10.1021/acs.est.6b04668 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.