Abstract
BACKGROUND
Patients with ulcerative colitis (UC) may be exposed to opioids over their disease duration. The use of such medications carries significant risk, including intestinal dysmotility and potential for addiction. However, the rates of narcotic use and misuse in patients with UC have not been studied extensively. Functional gastrointestinal disorders (FGID) are prevalent in patients with UC, and have been shown to increase the risk of narcotic use and misuse in patients with Crohn’s disease. We hypothesized that patients with UC and a concurrent diagnosis of FGID would have increased rates of both opioid use and misuse in our patient cohort.
AIM
To evaluate the prevalence of chronic opioid use and misuse in UC.
METHODS
A retrospective chart review of UC patients seen at the University of Virginia Digestive Health Center was performed on all patients evaluated between 2006 and 2011. Patient demographics, medical, surgical, and medication histories were obtained from the electronic medical record. Concomitant diagnosis of FGID was also noted at the time. The electronic prescription monitoring program was accessed to obtain prescription opioid filling histories. Prescription opioid misuse was defined as opioid prescriptions filled from four or more prescribers and four or more different pharmacies in a 12-mo period.
RESULTS
A total of 497 patients with UC were included. Patients with UC and FGID were more likely to be female, but no other demographic variables were associated with FGID. Of the UC patients who had FGID, a greater proportion were found to be using opioids chronically (36% with FGID vs 9% without FGID, P < 0.0001) and were misusing prescription opioids (12.8% vs 1.3%, P < 0.001). Multivariate logistic regression demonstrated a significant association with FGID and chronic opioid use (OR = 4.50; 95%CI: 1.91-10.59) and opioid misuse (OR = 5.19; 95%CI 1.04-25.76). Tobacco use (OR 2.53; 95%CI: 1.06-6.08) and anxiety (OR 3.17; 95%CI: 1.08-9.26) were other variables associated with an increased risk of chronic narcotic use.
CONCLUSION
FGID was associated with a 4.5-fold increase in chronic opioid use and a 5-fold increased risk of opioid misuse in this patient cohort with UC.
Keywords: Ulcerative colitis, Chronic opioid use, Opioid misuse, Narcotic, Functional gastrointestinal disorder
Core tip: Rates of chronic opioid use and misuse among patients with ulcerative colitis (UC) have not been studied extensively, and it is unknown whether functional gastrointestinal disorder (FGID) affects these rates. The aims of this study were to evaluate rates of opioid use and misuse in UC and determine whether these rates were affected by concomitant FGID. Patients with FGID and UC were 4.5 times more likely to be using chronic opioids and 5 times more likely to be misusing opioids. This highlights the potential risks of opioid use in the management of UC, particularly in those patients with concomitant FGID.
INTRODUCTION
Ulcerative colitis (UC) is a chronic inflammatory gastrointestinal condition which can manifest with recurrent bouts of abdominal pain, rectal bleeding, and diarrhea. During disease flares, opioid medications may be prescribed in the acute setting for the treatment of pain, but carry significant negative consequences including worsening intestinal dysmotility and visceral hyperalgesia, along with the potential risk for medication dependency and addiction[1,2].
Rates of opioid addiction, diversion, and overdose have risen dramatically in the United States over the past two decades[3,4] and are currently at epidemic levels. State-run prescription monitoring programs (PMPs) have been established to combat this issue and make it possible to identify patients who have behaviors suggesting opioid misuse, such as “doctor shopping,” obtaining prescriptions from multiple prescribers, using multiple pharmacies, using multiple opioids simultaneously, and obtaining early refills of medications. While there is no standard definition for opioid misuse, Katz et al[5] defined the use of greater than or equal to four pharmacies and greater than or equal to four prescribers of schedule II medications within a 12-mo period as “questionable activity” which is consistent with opioid misuse.
Functional gastrointestinal disorders (FGID) have been shown to be prevalent among patients with inflammatory bowel disease (IBD)[2]. Simrén et al[6] demonstrated that irritable bowel syndrome-like symptoms were two to three–fold more prevalent in patients with IBD in remission than in the general population, and patients with these symptoms also exhibited increased levels of depression and anxiety. FGID has been shown to be a significant risk factor for chronic opioid use and misuse among patients with Crohn’s disease[7], representing a two-fold and three-fold increased risk of chronic opioid use and misuse, respectively. While the prevalence of opioid use has been previously reported in UC[1,8], to our knowledge, the prevalence of opioid misuse has not been specifically studied in this population. The primary aim of this study was to determine whether patients with UC and concurrent FGID had higher rates of chronic opioid use, and to determine the prevalence and risk factors for prescription opioid misuse in this patient population.
MATERIALS AND METHODS
Patients
A retrospective chart review was performed on patients with UC treated at the University of Virginia Digestive Health outpatient clinic from 2006 to 2011. Patient demographics were obtained from the electronic medical record (Epic Hyperspace, Verona, WI) including patient age, sex, race, insurance status, geographic area of residence, tobacco use, and alcohol use. Medical, surgical and psychiatric histories were recorded for each patient; including the diagnosis of any co-existing FGID. The Rome III criteria and diagnoses served as the basis for our inclusion of FGIDs in this study, and all patients with a FGID, regardless of whether their FGID related to upper or lower gastrointestinal symptoms, were marked as having FGID. Patients with symptoms of FGID without an existing diagnosis made by a clinician were not recorded as having FGID. Medication history was obtained from the electronic medical record including IBD-related therapy and non-IBD medications. Information on opioid use was also collected using electronic prescription monitoring program databases from Virginia and West Virginia (https://virginia.pmpaware.net). To access the PMP database, patient name, date of birth, and date of initial clinic visit were entered into the database, and information regarding the type and number of opioid prescriptions, as well as the number of different prescribers and pharmacies, were recorded. Prescription data was collected for a one-year period following the date of the initial office visit, and thus patients had an established diagnosis of UC at the time at which prescription data collection began.
Chronic opioid use was defined as having three consecutive prescriptions for opioids filled or having two or more opioid prescriptions filled within a six-month period. Opioid misuse was defined as a patient meeting the “4 + 4 criteria” of having opioid prescriptions given by four or more prescribing physicians and using four or more pharmacies in a 12-mo period[5]. Post-operative pain medication prescriptions that were limited to one prescription were not counted toward the analysis.
Statistical analysis
Statistical analysis was performed by a biomedical statistician (Northup PG) using SAS 9.2 (SAS Institute Inc., Cary, NC). Comparisons of categorical variables were made using Chi-squared tests, odds ratios and 95%CI were used to assess the interaction between chronic opioid use and opioid misuse and the following variables: age, sex, alcohol use, cigarette smoking, Medicaid/disability insurance status, anxiety, depression, and FGID. Similar interactions were assessed between FGID and the following variables: age, sex, alcohol use, cigarette smoking, Medicaid/disability insurance status, anxiety, depression, chronic opioid use, and chronic opioid misuse. Univariate and multivariate logistic regression analyses were conducted to identify potential variables affecting rates of chronic opioid use and misuse. Approval for the study was obtained through the Institutional Review Board for Health Sciences Research at the University of Virginia.
RESULTS
A total of 497 patients with UC seen at the University of Virginia Digestive Health Clinic from 2006 to 2011 were included in the study cohort (Table 1). Of these, 39 (7.8%) patients were identified as having concurrent FGID. In addition, 103 (20.7%) patients had concomitant psychiatric disease including 68 patients with depression, 22 with anxiety, and 13 with an alternative psychiatric diagnosis. Forty-three (8.7%) patients were current tobacco users.
Table 1.
Patient characteristics n (%)
| FGID patients (n = 39) | Non-FGID patients (n = 458) | Total (n = 497) | |
| Mean age (yr) | 51.2 | 53.0 | 52.9 |
| Sex (Female) | 29 (74.4) | 220 (48.0) | 249 (50.1) |
| Disability/Medicaid status | 4 (10.3) | 14 (3.1) | 18 (3.6) |
| Tobacco use | 7 (17.9) | 36 (7.9) | 43 (8.7) |
| Alcohol use | 12 (30.8) | 185 (40.4) | 197 (39.6) |
| History of depression | 9 (23.1) | 59 (12.9) | 68 (13.7) |
| History of anxiety | 9 (23.1) | 13 (2.8) | 22 (4.4) |
| Disease extent | |||
| Proctitis | 6 (15.4) | 39 (8.5) | 45 (9.1) |
| Left sided | 12(30.8) | 153 (33.4) | 165 (33.2) |
| Extensive | 20 (51.3) | 227 (49.6) | 247 (49.7) |
| Average disease duration (yr) | 8.2 | 7.5 | 7.6 |
Among the patient characteristics analyzed, only female sex was associated with functional gastrointestinal disease (FGID) in comparison to the non-FGID cohort. FGID: Functional gastrointestinal disease.
Patients with UC and FGID were no different in age than patients with UC without FGID (49.5 years vs 51.2 years, P = 0.463). Patients with FGID were more likely to be female (74% with FGID vs 48% without FGID, P= 0.010). There was a trend toward FGID and anxiety (23% with FGID vs 3% without FGID, P = 0.055). FGID was not significantly associated with depression, alcohol use, tobacco use, insurance or disability status in this patient cohort.
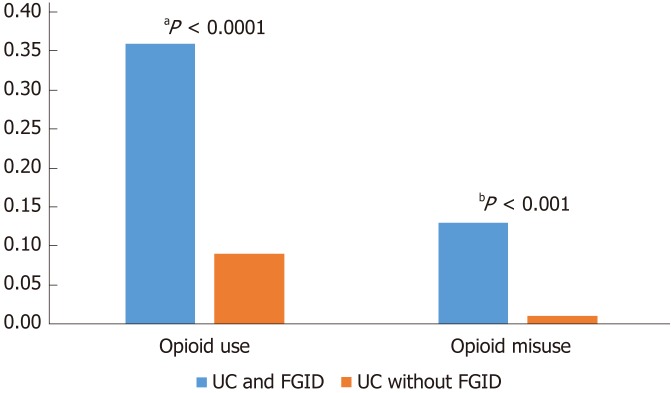
Of the 497 patients, 56 (11.3%) were identified as using chronic prescription opioids. The proportion of patients on chronic opioids was significantly greater among those with FGID than those without FGID (36% vs 9%, P < 0.0001, Figure 1). Anxiety (P = 0.035) and tobacco use (P = 0.038) were associated with significantly higher rates of chronic opioid use. Using the PMP to review prescription data, there was evidence of opioid misuse in 11 (2.2%) patients using the 4 + 4 criteria. Of these, 5 of 39 patients (12.8%) with FGID were identified as misusing prescription opioids, compared with 6 of 458 patients (1.3%) without FGID (P < 0.001, Figure 1).
Figure 1.
Rates of opioid use and misuse. Patients with ulcerative colitis and concomitant functional gastrointestinal disease had higher rates of prescription opioid use (36% vs 9%; aP < 0.0001) and opioid misuse (13% vs 1%; bP < 0.001). UC: Ulcerative colitis; FGID: Functional gastrointestinal disease.
Multivariate logistic regression analysis demonstrated a significant association of chronic opioid use and FGID. Patients with UC and FGID had a 4.5-fold higher risk of chronic opioid use than those patients without FGID (OR = 4.50; 95%CI: 1.91-10.59). There was also an association of FGID and opioid misuse, with a five-fold increase in the risk of opioid misuse in FGID patients (OR = 5.19; 95%CI: 1.04-25.76). Tobacco use (OR = 2.53; 95%CI: 1.06-6.08) and anxiety (OR = 3.17; 95%CI: 1.08-9.26) were also associated with higher risk of chronic narcotic use, whereas patient gender, alcohol use, depression, and disability status were not (Table 2).
Table 2.
Predictors of chronic narcotic use in patients with ulcerative colitis
| Variables | Odds ratio estimates (Point estimates with 95% Wald confidence limits) | P value |
| FGID | 4.50 (1.91-10.59) | < 0.001 |
| Female sex | 0.76 (0.41-1.42) | 0.390 |
| Tobacco use | 2.53 (1.06-6.08) | 0.038 |
| Alcohol use | 0.53 (0.27-1.04) | 0.065 |
| Anxiety | 3.17 (1.08-9.26) | 0.035 |
| Depression | 1.36 (0.59-3.11) | 0.468 |
| Disability/Medicaid insurance status | 1.77 (0.49-6.38) | 0.382 |
Among the risk factors included in the multivariate analysis, only functional gastrointestinal disease, tobacco use, and anxiety increased the risk for chronic narcotic use in ulcerative colitis. FGID: Functional gastrointestinal disease.
DISCUSSION
Within this UC patient cohort, chronic opioid use was identified in 11.3% of patients overall. UC patients with concomitant FGID were over four-fold more likely to be using chronic opioids than those UC patients without FGID. Prescription monitoring program data identified 2% of the total UC patient cohort to be misusing prescription opioids. Patients with UC and concurrent FGID had a 5-fold increased risk of opioid misuse, with 13% of patients in this group showing evidence of opioid misuse based on PMP data. The rates of chronic use and misuse of opioids are significant given the negative impacts that opioids have on disease outcomes in UC and FGID[1,2], in addition to the potential risks of opioid dependency and addiction in this population.
Our study also found an increased risk of opioid misuse in patients with UC and FGID (OR = 5.19, 95%CI: 1.04-25.76); however the overall number of patients identified with opioid misuse was small, and larger numbers of patients would be needed to confirm this association. Tobacco use and anxiety were also associated with an increased risk of chronic narcotic use, associations which have been identified in prior studies[9-11] and are also identified in our population to be risk factors for opioid misuse.
Given this was a retrospective study at a single tertiary care center, these results may not be generalizable to the UC population in the United States as a whole. The majority of our patient cohort resides in Virginia and West Virginia, and the opioid prescription information was limited to the PMPs from these two states. It is possible that some patients obtained opioid medications from other neighboring states and thus were not identified in the PMP data search, and this model does not account for patients using opioids that they have obtained outside of a provider’s prescription. This model also assumes that all patients who filled opioid prescriptions took the medications themselves, and does not account for diversion of opioid medications. Another limitation of this study was that it was not possible in all instances to know the circumstances for which patients were using opioids (e.g., flaring disease, abdominal pain in the absence of active UC). Thus it was not possible to stratify patients according to disease activity or severity, as patients often sought care in places other than our institution, such as from a local gastroenterologist, primary care provider, urgent care, or local emergency room.
Despite these limitations, this is the first study to our knowledge that assesses the risk of prescription opioid misuse in the UC population and identifies a subgroup of patients with concomitant FGID to be at particular risk for chronic opioid use and misuse. This has important implications in managing patients with UC and FGID as a particularly “at risk” group for opioid misuse and a population to be monitored for early intervention if this is occurring.
In conclusion, patients with UC and concomitant FGID have a 4.5-fold increased risk of chronic opioid use. Patients with UC and FGID are also at risk for opioid misuse, based on prescription monitoring program data. There is significant risk for development of opioid-related complications including opioid dependency and misuse in this population.
ARTICLE HIGHLIGHTS
Research background
Opioid use in the inflammatory bowel disease (IBD) population is common, given that symptoms of disease activity often include abdominal pain. While opioids may provide temporary relief, they carry long-term risks such as narcotic bowel syndrome and the potential for dependence and addiction. However, little is known about the specific rates of opioid use and misuse in the ulcerative colitis (UC) population. Functional gastrointestinal diseases often overlap with symptoms of IBD, and abdominal pain or functional symptoms in patients with UC with a concomitant diagnosis of functional gastrointestinal disorders (FGID) may be easily mistaken as a manifestation of active UC during periods of disease remission. In a previous study, we showed that rates of chronic opioid use and misuse among patients with Crohn’s disease (CD) and concomitant FGID were two-fold and three-fold higher, respectively, than in patients with CD without a diagnosis of FGID.
Research motivation
Identification of risk factors for opioid abuse in the IBD population, specifically in UC patients, is key in prevention of complications of these medications. Patients at risk for chronic opioid use and misuse can be identified, and prescribers can be better informed, thereby preventing many of the adverse effects – physical, mental and psychosocial – associated with long-term opioid therapy in this vulnerable population.
Research objectives
The purpose of this study was to characterize rates of chronic opioid use and misuse in the UC population, as these have not been studied extensively. One of the objectives of this study was to investigate whether FGID was a risk factor for chronic opioid use and misuse in UC patients, as has been demonstrated in patients with CD and FGID.
Research methods
Following approval through the institutional review board, a retrospective chart review was conducted at the University of Virginia Digestive Health Center including all patients who had been evaluated for ulcerative colitis between 2006 and 2011. Patient demographics and selected variables (tobacco use, alcohol use, etc.), medical, surgical and psychiatric histories, and concomitant diagnoses of FGID (as outlined by Rome III criteria) were collected from the electronic medical record. Data on opioid use was collected from the electronic prescription monitoring program databases for the states of Virginia and West Virginia (https://virginia.pmpaware.net). Statistical analysis was conducted by a biomedical statistician and both univariate and multivariate regression analyses were performed.
Research results
This study cohort consisted of 497 patients with UC, who were seen at the University of Virginia from 2006 to 2011. Of these patients, 7.8% had a concurrent diagnosis of FGID as defined by Rome III criteria, 20.7% had concomitant psychiatric disease, and 8.7% were current tobacco users. Patients with UC and FGID were more likely to be female (P = 0.010), but no other risk factors were found to be associated with FGID in the UC cohort. A greater proportion of patients with FGID and UC were on chronic opioid therapy than patients with UC without FGID (36% vs 9%, P < 0.0001), and a greater proportion of patients with FGID and UC met criteria for opioid misuse (12.8% vs 1.3%, P < 0.001). In the multivariate logistic regression analysis, patients with FGID and UC had a 4.5-fold increased risk for chronic opioid use and 5-fold increased risk for opioid misuse in comparison to their UC counterparts without FGID. Tobacco use and anxiety also conferred higher risks for chronic narcotic use.
Research conclusions
To our knowledge, this is the first study which assesses the rates of and risk factors for both chronic opioid use and misuse in the UC population. This study sheds light on the need for careful prescription practices among providers who have patients with UC, particularly those with concomitant diagnoses of FGID. As we hypothesized, FGID increased the risk for both chronic opioid use and misuse in our cohort of UC patients, which is a novel finding and may set the foundation for future studies. Tobacco use and anxiety also conferred an increased risk for chronic narcotic use in UC patients, as demonstrated in prior studies, but were not variables associated with FGID. While FGID did increase the risk for opioid misuse five-fold in our UC cohort, our numbers of patients meeting the definition of opioid misuse was small, and thus more associations may not have reached statistical significance.
Research perspectives
The insights gained from this study may provide the basis for practitioners to monitor opioid use in their UC cohorts, and potentially intervene when chronic opioid use and misuse are suspected. Furthermore, this study emphasizes that PMP databases are useful tools not only in the general population, but also in specific populations such as the IBD population. While this study was conducted at a tertiary referral center in the United States and a large number of patients were included, the results may not be generalizable to the US and worldwide, as this was a single-center study and the opioid epidemic has disproportionately affected some of the geographic areas (e.g., Southwest Virginia) in which our patients reside. Future studies with a similar design and the inclusion of multiple sites may help to further define risk factors for chronic opioid use and misuse in the UC cohort. The data obtained from this study may, in the near future, also serve as a basis for quality improvement studies in which at-risk UC patients are identified and treated with alternatives for opioids in the appropriate situations.
ACKNOWLEDGEMENTS
The authors wish to thank Joseph Mock, MD, for his contributions to data collection.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: This study was reviewed and approved by the University of Virginia Institutional Review Board for Health Sciences Research (IRB-HSR).
Informed consent statement: Patients were not required to give informed consent for this study as the analysis was conducted retrospectively and no identifying factors were used in the analysis.
Conflict-of-interest statement: The authors declare no potential conflicts of interest related to this article.
Data sharing statement: No additional data are available.
Peer-review started: October 19, 2018
First decision: November 15, 2018
Article in press: January 9, 2019
P- Reviewer: Chiba T, Lan C S- Editor: Wang JL L- Editor: A E- Editor: Bian YN
Contributor Information
Maithili V Chitnavis, Division of Gastroenterology and Hepatology, Virginia Tech Carilion School of Medicine, Roanoke, VA 24016, United States. mvchitnavis@carilionclinic.org.
Merwise Baray, University of Virginia School of Medicine, Charlottesville, VA 22908, United States.
Patrick G Northup, Division of Gastroenterology and Hepatology, University of Virginia School of Medicine, Charlottesville, VA 22908, United States.
Anne G Tuskey, Division of Gastroenterology and Hepatology, University of Virginia School of Medicine, Charlottesville, VA 22908, United States.
Brian W Behm, Division of Gastroenterology and Hepatology, University of Virginia School of Medicine, Charlottesville, VA 22908, United States.
References
- 1.Targownik LE, Nugent Z, Singh H, Bugden S, Bernstein CN. The prevalence and predictors of opioid use in inflammatory bowel disease: a population-based analysis. Am J Gastroenterol. 2014;109:1613–1620. doi: 10.1038/ajg.2014.230. [DOI] [PubMed] [Google Scholar]
- 2.Edwards JT, Radford-Smith GL, Florin TH. Chronic narcotic use in inflammatory bowel disease patients: prevalence and clinical characteristics. J Gastroenterol Hepatol. 2001;16:1235–1238. doi: 10.1046/j.1440-1746.2001.02468.x. [DOI] [PubMed] [Google Scholar]
- 3.Volkow ND, McLellan AT. Opioid Abuse in Chronic Pain--Misconceptions and Mitigation Strategies. N Engl J Med. 2016;374:1253–1263. doi: 10.1056/NEJMra1507771. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Health, United States, 2014: With Special Feature on Adults Aged 55–64. Hyattsville: U.S. Department of Health and Human Services, 2015. [PubMed] [Google Scholar]
- 5.Katz N, Panas L, Kim M, Audet AD, Bilansky A, Eadie J, Kreiner P, Paillard FC, Thomas C, Carrow G. Usefulness of prescription monitoring programs for surveillance--analysis of Schedule II opioid prescription data in Massachusetts, 1996-2006. Pharmacoepidemiol Drug Saf. 2010;19:115–123. doi: 10.1002/pds.1878. [DOI] [PubMed] [Google Scholar]
- 6.Simrén M, Axelsson J, Gillberg R, Abrahamsson H, Svedlund J, Björnsson ES. Quality of life in inflammatory bowel disease in remission: the impact of IBS-like symptoms and associated psychological factors. Am J Gastroenterol. 2002;97:389–396. doi: 10.1111/j.1572-0241.2002.05475.x. [DOI] [PubMed] [Google Scholar]
- 7.Crocker JA, Yu H, Conaway M, Tuskey AG, Behm BW. Narcotic use and misuse in Crohn's disease. Inflamm Bowel Dis. 2014;20:2234–2238. doi: 10.1097/MIB.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan MA, Korelitz BI. Narcotic dependence in inflammatory bowel disease. J Clin Gastroenterol. 1988;10:275–278. doi: 10.1097/00004836-198806000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Wasan AD, Butler SF, Budman SH, Benoit C, Fernandez K, Jamison RN. Psychiatric history and psychologic adjustment as risk factors for aberrant drug-related behavior among patients with chronic pain. Clin J Pain. 2007;23:307–315. doi: 10.1097/AJP.0b013e3180330dc5. [DOI] [PubMed] [Google Scholar]
- 10.John WS, Zhu H, Mannelli P, Schwartz RP, Subramaniam GA, Wu LT. Prevalence, patterns, and correlates of multiple substance use disorders among adult primary care patients. Drug Alcohol Depend. 2018;187:79–87. doi: 10.1016/j.drugalcdep.2018.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson A, Click B, Ramos-Rivers C, Koutroubakis IE, Hashash JG, Dunn MA, Schwartz M, Swoger J, Barrie A 3rd, Regueiro M, Binion DG. The Association Between Sustained Poor Quality of Life and Future Opioid Use in Inflammatory Bowel Disease. Inflamm Bowel Dis. 2018;24:1380–1388. doi: 10.1093/ibd/izy040. [DOI] [PMC free article] [PubMed] [Google Scholar]