Abstract
Restaurants are key venues for reducing sodium intake in the U.S., but little is known about consumer perceptions of sodium in restaurant foods. This study quantifies the difference between estimated and actual sodium content of restaurant meals and examines predictors of underestimation in adult and adolescent diners at fast food restaurants. In 2013 and 2014, meal receipts and questionnaires were collected from adults and adolescents dining at six restaurant chains in four New England cities. The sample included 993 adults surveyed during 229 dinnertime visits to 44 restaurants and 794 adolescents surveyed during 298 visits to 49 restaurants after school or at lunchtime. Diners were asked to estimate the amount of sodium (mg) in the meal they had just purchased. Sodium estimates were compared with actual sodium in the meal, calculated by matching all items that the respondent purchased for personal consumption to sodium information on chain restaurant websites. Mean (SD) actual sodium (mg) content of meals was 1,292 (970) for adults and 1,128 (891) for adolescents. One-quarter of diners (176 (23%) adults, 155 (25%) adolescents) were unable or unwilling to provide estimates of the sodium content of their meals. Of those who provided estimates, 90% of adults and 88%of adolescents underestimated sodium in their meals, with adults underestimating sodium by a mean (SD) of 1,013 mg (1,055) and adolescents underestimating by 876 mg (1,021). Respondents underestimated sodium content more for meals with greater sodium content. Education about sodium at point-of-purchase, such as provision of sodium information on restaurant menu boards, may help correct consumer underestimation, particularly for meals of high sodium content.
Keywords: sodium, knowledge, nutrition labeling, nutrition policy, restaurants
Introduction
Population-wide sodium reduction is an important strategy for reducing cardiovascular disease and mortality in the U.S., where sodium consumption among children, adolescents, and adults exceeds the Institute of Medicine’s upper limit (2,300 mg/day) by nearly 1,000 mg/day (National Academies of Sciences, Engineering, Medicine, 2004, New York City Department of Health & Mental Hygiene & American Heart Association, 2014, Cogswell et al., 2014, Centers for Disease Control and Prevention, 2012). In the U.S., adults and adolescents consume nearly 25% of dietary sodium from restaurant sources, and restaurant food contains more sodium per calorie than foods purchased from grocery stores or other food outlets (Cogswell et al., 2014, Centers for Disease Control and Prevention, 2012). In the National Health and Nutrition Examination Surveys, consumption of restaurant foods is associated with significantly higher average daily sodium intake among adolescents and adults (An, 2016, Nguyen & Powell, 2014, Powell & Nguyen, 2013). A 2012 study of menu items served by the 400 top-earning restaurants in the U.S. found that the average sodium content of entrees was 1,512 mg, more than half the upper limit recommended for daily consumption (Wu & Sturm, 2013, National Academies of Sciences, Engineering, Medicine, 2004).
Recognition of the health consequences of high sodium intake and the concentration of such a high proportion of total intake in restaurant food has compelled policymakers to propose measures to highlight items with high sodium levels. The New York City Board of Health recently issued a mandate requiring all restaurants with 15 or more locations to place salt warning labels on items that exceed the recommended daily upper limit of 2,300 mg of sodium (New York City, 2015). Other municipalities could proceed with similar policies, especially considering prior rapid adoption of calorie labeling after New York City implemented its calorie labeling policy in 2008 (Long et al., 2015). Labeling policies intend to correct a perceived consumer knowledge deficit and have successfully increased consumer knowledge and awareness of health risks in other settings. For example, there is evidence that placing prominent text warning labels on cigarette packages increased consumer risk perceptions and decreased intent to purchase cigarettes (Hammond, 2011). In experimental settings, similar effects have been found when health warning labels are displayed prominently on sugary drinks (Roberto et al., 2016, VanEpps & Roberto, 2016). Although research on how calorie labels in restaurants influence consumer food choices has been mixed, several studies have found that the labels increase consumer awareness of calories, and may influence purchase intentions, particularly when the information displayed defies consumer expectations (Long et al., 2015, Chen et al., 2015, Dumanovsky et al., 2010, Krieger et al., 2013, Burton et al., 2009, Reale & Flint, 2016).
Sodium warning labels may have a similar effect on consumer awareness of sodium in restaurant food; however, little research has documented this. Experimental studies have found that consumers likely significantly underestimate sodium in restaurant foods. In a 2006 study, 193 adults received a mail survey and were asked to estimate the sodium content of several selected restaurant items. Participants underestimated sodium content in entrees by 115–811%, with less accuracy for the highest sodium items (Burton et al., 2006).
The aim of this study was to fill a gap in our understanding of consumer knowledge of sodium in restaurant foods by examining the accuracy of consumer estimates of sodium in restaurant meals. To our knowledge, this is the first study to assess consumer estimates of sodium in a real-world setting and the first study of any kind to examine sodium estimates among adolescents. Using a sample of adolescents and adults dining at six fast food restaurant chains in four New England cities, this study quantified the difference between estimated and actual sodium content of restaurant meals and examined predictors of underestimation. Consistent with prior studies of nutrition knowledge and label reading, we hypothesized that age, gender, race, body mass index, restaurant chain, importance of nutrition information in making food choices, and ability to accurately estimate recommendations for daily sodium intake would be associated with accuracy of sodium estimation (Long et al., 2015, Campos et al., 2011, Ayala et al., 2010). This research provides evidence quantifying consumer misperceptions about sodium in restaurant food and potential demographic disparities, which will inform ongoing policy debates around the need for sodium warning labels, or other methods for conveying sodium information, in restaurant settings.
Methods
Study Design
Data for this study were collected in the context of a separate study evaluating the effects of calorie labels on adult, adolescent, and child fast-food meal purchases. Data for the calorie labeling study were collected from 2010–2014, but questions about sodium were not added to adult and adolescent questionnaires until June 2013. This analysis is based on the subsample of adults and adolescents who were asked questions about sodium in 2013 and 2014. Data were collected from June-September in 2013 and May-September in 2014.
Restaurants selected for the study were located in four New England cities: Boston, MA; Springfield, MA; Providence, RI; and Hartford, CT. These cities range in size from 179,000–650,000 people and are demographically diverse, with populations ranging from 16–38% black, 18–44% Hispanic, and 22–33% of individuals in poverty (U.S. Census Bureau, 2015). Restaurant chains with the highest U.S. sales and at least two locations in each city were selected for the adult sample, and restaurant chains with at least two locations within one mile of a high school were selected for the adolescent sample. The restaurant chains for the adult sample were McDonald’s, Burger King, Wendy’s, Kentucky Fried Chicken (KFC) and Subway. The same restaurant chains were used for the adolescent sample except Dunkin’ Donuts was substituted for KFC. A detailed description of restaurant chain sampling has been described elsewhere (Block et al., 2013). No restaurant chains in the adult or adolescent sample printed sodium information on menus. In some stores, sodium information was available on wall posters, food containers/wrappers, napkins, or cups. All chains listed nutrition information, including sodium content, on their websites.
Street intercept survey methodology was used to collect data from participants outside restaurant entrances or, if research assistants were not permitted to work on the restaurant’s property, on a public sidewalk adjacent to the restaurant. Every effort was made to visit the same restaurants in 2013 and 2014; however, this was not always possible due to management refusals. In the adolescent sample, four of 36 restaurants visited in 2013 were replaced with two new restaurants in 2014 and in the adult sample four of 43 restaurants visited in 2013 were replaced with three new restaurants in 2014. Research assistants approached diners who appeared eligible based on age for each of the samples and asked them to save their receipts if interested in participating in a study about “choices in fast food restaurants.” Age eligibility for the different samples was 18+ years of age for adults and 11 to 20 years of age for adolescents. The adolescent group included a relatively wide range of ages, from adolescent to young adult, but we refer to this group as “adolescents” for the ease of presentation. We included this wide range of age for the adolescent category to recruit as many young people as possible. While there was age overlap between the two samples, it was highly unlikely that individuals would cross over both samples as we collected data at lunchtime for adolescents and in the evening for adults. When customers exited the restaurant, research assistants collected receipts, asked participants to identify items (or portions of items, if items were intended for sharing) purchased for individual consumption, and completed an item questionnaire. The item questionnaire clarified details about the order, such as whether the meal was shared, fountain beverage choices, and meal customization (e.g., addition of condiments or dipping sauces). A respondent’s meal was defined as all purchased items intended for individual consumption. To calculate actual calorie and sodium content of meals, information for each item on receipts was linked to nutrition information from restaurant websites, collected in July of each year of data collection. Research comparing nutrition information on restaurant menus to measurements taken in a lab shows that the stated energy content of restaurant foods is generally accurate (Urban et al., 2011). While no studies have validated the accuracy of sodium information stated on restaurant websites, a study of Canadian food labels found that laboratory values for sodium were within 20% of stated values for most items (Fitzpatrick et al., 2014). A brief questionnaire was administered to capture the participant’s estimation of the meal’s calorie and sodium content, importance of calories, convenience, price, and taste in food choices (“a lot,” “a little,” or “not at all”), awareness of calorie information in the restaurant (“yes,” “no,” “unsure”), BMI (calculated from self-reported height and weight), and basic demographic information (age, gender, race/ethnicity). Participants were also asked to estimate the average daily calorie (kcal) and sodium (mg) recommendations (“Less than 1,000,” “At least 1,000 but no more than 2,000,” “At least 2,000 but no more than 3,000,” “At least 3,000 but no more than 4,000,” “At least 4,000 but no more than 5,000,” “Greater than 5,000”). For both calories and sodium, a wide range of estimates (1,000–3,000) was considered accurate to allow for variation within individuals included in this study. Estimates of less than 1,000 were considered underestimates, and estimates greater than 3,000 were considered overestimates. Questionnaires were administered in English, but were available in Spanish to guide participants who were Spanish-speaking and had limited English proficiency. Each participant received a $2 gift card for enrolling in the study.
Statistical Analysis
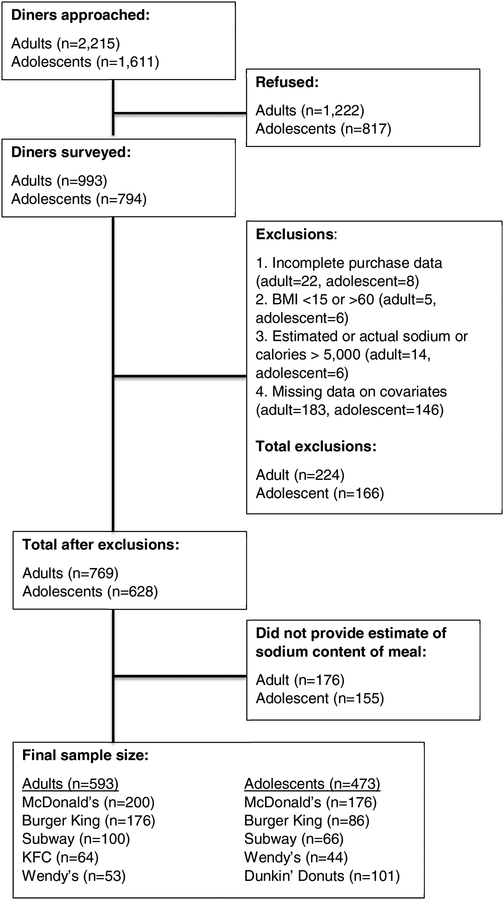
For this study, 993 adults were surveyed during 229 visits to 44 restaurants, and 794 adolescents were surveyed during 298 visits to 49 restaurants (Figure 1). Of the participants surveyed, 22 (2%) adult and 8 (1%) adolescent surveys were excluded due to incomplete information on foods purchased. Nineteen (2%) adults and 12 (2%) adolescents were excluded due to outlier values for estimated or actual sodium or calories (>5,000 kcals and >5,000 mg, respectively) or outlier values for BMI (<15 or >58 kg/m2). For consistency across statistical models, participants missing data on covariates were also excluded (183 (18%) adults, 146 (19%) adolescents). After exclusions, the sample included 769 adults and 628 adolescents. Of these, 176 (23%) adults and 155 (25%) adolescents did not provide an estimate of the sodium in their meals and thus were not eligible for inclusion in the final analysis. The final sample for analyzing estimation of sodium content included 593 adults and 473 adolescents.
Figure 1.
Flow diagram of sampling selection and total number of adults and adolescents included in the analysis.
Characteristics of respondents who did versus did not provide estimates of meal sodium content were compared using Student’s t-tests for age, BMI, and mean of meal sodium content and Chi-squared tests were used to compare year of data collection, sex, race/ethnicity, importance of taste, calories, price, and convenience in food choices, whether or not the participant noticed calorie information in the restaurant, and estimates of the daily sodium recommendation.
Among those respondents who provided sodium estimates, multivariable linear models were used to identify predictors of underestimation of sodium content. The model outcome was the difference between estimated and actual sodium content; independent variables included restaurant chain and multiple other predictors determined a priori as possible determinants of estimated sodium content, including underestimation of calorie content (as a proxy for nutrition knowledge), age, BMI, year of data collection, gender, race/ethnicity, whether participants noticed calorie information in the restaurant, importance of calories, taste, price, and convenience in food choices, and accuracy of estimates of the daily sodium recommendation. Actual sodium content was mean-centered; intercepts from each model represent the degree of underestimation for meals of mean actual sodium content. Positive parameter estimates indicate better estimation of sodium content per unit increase for linear predictors or compared with a reference group for categorical predictors. Data were analyzed in 2015 using SAS Version 9.4 (Cary, NC).
Results
Most diners were of non-white race/ethnicity (377 (64%) adults, 377 (80%) adolescents), and just over 50% of respondents in both samples were male. Taste was the most important driver of food choices, with over three quarters of participants reporting taste mattered “a lot” (481 (81%) adults, 356 (75%) adolescents). Most participants underestimated the daily sodium recommendation (486 (82%) adults, 314 (66%) adolescents).
Several differences were evident when comparing characteristics of participants who provided sodium estimates and those who did not (sodium “non-responders”). In the adult sample, nonresponders were slightly older (mean [SD] age=36.8 [14.8] for responders vs 39.7 [15.6] for nonresponders) and were more likely to be of white race (n [%] white=216 [36] vs 85 [48]). Fewer non-responders reported taste mattered “a lot” when making food choices (481 [81] vs 124 [70]) and, surprisingly, non-responders were more likely to accurately estimate the daily sodium recommendation (98 [17] vs 55 [31]). Among adolescents, there were more non-responders in 2014 (274 [58] vs 110 [71]), and non-responders were less likely to report price mattered “a lot” for food choices (140 [30] vs 25 [16]).
For those participants providing sodium estimates, mean (SD) actual sodium (mg) content of meals was 1,292 (970) for adults and 1,128 (891) for adolescents (Table 2). More than 10% of participants purchased meals containing more than than 2,300 mg of sodium (76 (13%) adult meals, 52 (11%) adolescent meals). More than 85% of participants underestimated sodium in their meals (534 (90%) adults, 415 (88%) adolescents), and more than 60% underestimated by more than 500 mg (389 (66%) adults, 297 (63%) adolescents). The mean difference between estimated and actual sodium (the underestimate) was −1,013 mg (1,055) for adults and −876 mg (1,021) for adolescents. Mean underestimation of sodium varied by restaurant, and was greatest at KFC (−1,499 [1,206]) in the adult sample and at Subway (−1,389 [1,330]) in the adolescent sample.
Table 2.
Characteristics of meals* purchased at fast food restaurant chains in four cities in New England in 2013 and 2014 by adults and adolescents included in study of consumers’ estimates of sodium content of meals. Figures are numbers (percentage) unless stated otherwise.
| Adults (n=593) | Adolescents (n=473) | |
|---|---|---|
| Sodium content of meals: | ||
| Mean (SD; range) actual content in mg | 1292 (970; 0, 4970) | 1128 (891; 0, 4435) |
| Median (IQR) actual content in mg | 1220 (550, 1800) | 990 (340, 1725) |
| Mean (SD; range) estimated content in mg | 279 (572; 0, 5000) | 261(582; 0, 5000) |
| Median (IQR) estimated content in mg | 50 (12, 300) | 50 (15, 250) |
| Difference between estimated and actual sodium content: | ||
| Mean in mg (SD, range) | −1013 (1055; −4880, 3400) | −876 (1021; −3835, 4200) |
| Median in mg (IQR) | −940 (−1580, −190) | −805; −1480, −144) |
| Calorie content of meals: | ||
| Mean (SD; range) actual content | 754 (451; 0, 2540) | 723 (438;0, 2320) |
| Median (IQR) actual content | 680 (390, 1070) | 660 (360, 1030) |
| Mean (SD; range) estimated content | 639 (674; 0, 5000) | 527 (554; 0, 5000) |
| Median (IQR) estimated content | 500 (250, 800) | 400 (200, 700) |
| Difference between estimated and actual calorie content: | ||
| Mean (SD; range) | −114 (707; −2460, 4680) | −196 (583; −1750, 4060) |
| Median (IQR) | −140 (−460, 60) | −190 (−500, 0) |
| Mean (SD) difference between estimated and actual sodium content by restaurant: | ||
| McDonald’s | −720 (827) | −611 (942) |
| Burger King | −1009 (1099) | −1367 (973) |
| Subway | −1413 (1079) | −1389 (1330) |
| KFC | −1499 (1206) | -- |
| Wendy’s | −789 (1011) | −1257 (841) |
| Dunkin’ Donuts | -- | −373 (529) |
Meals defined as all purchased items intended for individual consumption.
In the multivariable linear models, there was a linear association between actual sodium content and underestimation of sodium in both the adult and adolescent samples (Table 3). Intercepts represent mean sodium underestimation (mg) for meals of average sodium content, which was −1,243 (95% CI=−1,595, −890) for adults and −600 (−1,079, −121) for adolescents. In both samples, underestimation increased as mean sodium content of the meal increased (b=−0.88 [95% CI= −0.94, −0.83] for adults; −0.95 [−1.02, −0.88] for adolescents). Based on these parameter estimates, for every 1 mg increase in sodium content of the meal, underestimation increased by 0.88 mg for adults and by 0.95 mg for adolescents. Accuracy of calorie estimates was associated with accuracy in sodium estimates for adults only. For every 1 kcal improvement in estimates of calorie content, estimation of sodium content improved by 0.15 mg.
Table 3.
Predictors of sodium estimation among adults and adolescents purchasing meals at fast food restaurant chains in four cities in New England, US, 2013 and 2014.
| Adults (n=593) b (95% CI) | P-Value | Adolescents (n=473) b (95% CI) | P-Value | |
|---|---|---|---|---|
| Intercept (difference between estimated and actual sodium for meal of mean actual sodium content) | −1243 (−1595, −890) | <0.001 | −600 (−1079, −121) | 0.01 |
| Actual sodium content (centered on mean) | −0.88 (−0.94, −0.83) | <0.001 | −0.95 (−1.02, −0.88) | <0.001 |
| Difference between actual and estimated calorie content | 0.15 (0.08, 0.22) | <0.001 | 0.06 (−0.31, 0.16) | 0.19 |
| Age (per year) | 2.01 (−1.38, 5.40) | 0.24 | 6.95 (−14.79−28.70) | 0.53 |
| BMI (per 5 points) | 20.24 (−19.63, 60.12) | 0.32 | −32.37 (−90.69, 25.96) | 0.28 |
| Year | ||||
| 2014 | 0.0 (ref) | 0.0 (ref) | -- | |
| 2013 | 58.92 (−34.46, 154.30) | 0.23 | 86.08 (−25.81, 197.98) | 0.13 |
| Gender | ||||
| Male | 0.0 (ref) | 0.0 (ref) | -- | |
| Female | 135.62 (42.08, 229.17) | 0.005 | −88.08 (−193.39, 17.24) | 0.10 |
| Race/ethnicity | ||||
| White | 0.0 (ref) | 0.0 (ref) | -- | |
| Black | −20.71 (−131.97, 90.55) | 0.71 | 126.66 (−21.13, 274.46) | 0.09 |
| Hispanic | 10.76 (−121.36, 142.88) | 0.88 | 21.01 (−140.65, 182.67) | 0.80 |
| Asian | 239.42 (18.35, 460.49) | 0.03 | −68.17 (−329.79, 193.44) | 0.93 |
| Other race | 31.23 (−169.69, 232.16) | 0.76 | 151.64 (−39.02, 342.30) | 0.12 |
| Restaurant chain | ||||
| McDonald’s | 0.0 (ref) | 0.0 (ref) | -- | |
| Burger King | 93.49 (−24.38, 211.36) | 0.12 | −195.33 (−352.41, −38.24) | 0.01 |
| Wendy’s | 149.65 (−22.56, 321.86) | 0.09 | −166.48 (−360.0, 27.03) | 0.09 |
| KFC | 106.59 (−68.68, 281.86) | 0.23 | -- | -- |
| Subway | 29.80 (−114.14, 173.75) | 0.68 | −96.55 (−267.77, 74.67) | 0.27 |
| Dunkin’ Donuts | -- | -- | −222.52 (−371.53, −73.51) | <0.01 |
| Type 3 F-test for chain difference | 0.62 | <0.01 | ||
| Noticed posted calories in restaurant | ||||
| Yes | 0.0 (ref) | 0.0 (ref) | -- | |
| No | −122.03 (−225.71, −18.36) | 0.02 | −37.04 (−164.63, 90.56) | 0.57 |
| Unsure | −162.33 (−378.98, 54.31) | 0.14 | −41.50 (−230.52, 147.50) | 0.67 |
| Importance of calories in food choice | ||||
| Not at all | 0.0 (ref) | 0.0 (ref) | ||
| A little | 4.44 (−112.99, 121.87) | 0.94 | 55.85 (−72.93, 184.62) | 0.39 |
| A lot | 11.39 (−100.11, 122.89) | 0.84 | 168.26 (32.93, 303.58) | 0.01 |
| Personal estimate of daily sodium recommendation | ||||
| Accurate (1000–3000mg/day) | 0.0 (ref) | 0.0 (ref) | -- | |
| Underestimated (<1000mg/day) | −156.34 (−282.91, −29.76) | 0.02 | −90.82 (−207.14, 25.50) | 0.13 |
| Overestimated (>3000mg/day) | 113.70 (−272.35, 499.75) | 0.56 | 328.23 (69.81, 586.64) | 0.01 |
Note: Models additionally controlled for importance of price, taste, and convenience in food choice. Boldface indicates statistical significance (p<0.05).
In the adult sample, women (135.62 [42.08, 229.17]) and participants who identified as Asian (239.42 [18.35, 460.49]) underestimated sodium less than men and participants who identified as white, respectively. Participants who did not notice calories posted in the restaurant underestimated sodium more than people who noticed calories (−122.03 [−225.71, −18.36]). Compared to participants who accurately estimated the daily sodium recommendation, those who underestimated the recommendation also underestimated meal sodium content more (−156.34 [−282.91, −29.76]). Similarly, adolescent diners who overestimated the daily sodium recommendation were better at estimating the sodium content of their meals (328.23 [69.81, 586.64]) compared to those who provided an accurate estimate of the daily recommendation. While there were no significant differences between adolescents who did and did not notice calories posted in restaurants, those reporting calories were important in food choices provided more accurate estimates of sodium in their meals compared to diners who reported calories were “not at all” important (168.26 [32.93, 303.58]).
In the adult sample, there was little difference in estimation by restaurant chain, however, adolescent diners at Burger King (−195.33 [−352.41, −38.24]) and Dunkin’ Donuts (−222.52 [−371.53, −73.51]) provided worse estimates of the sodium in their meals, compared to diners at McDonald’s. There were no differences in sodium estimation by year of data collection or BMI in either sample.
Discussion
In this study of diners at fast food restaurants in four New England cities, nearly one-quarter of adults and adolescents did not provide estimates of the sodium content of their meals. The majority of those who provided a response substantially underestimated the amount of sodium in the meal they purchased. Average sodium content of meals – 1,128 mg for adolescents and 1,292 mg for adults – was approximately half the daily limit recommended by the 2015–2020 Dietary Guidelines for Americans (U.S. Department of Health and Human Services, 2015). On average, consumers underestimated sodium in their meals by 50–100%, and the degree of underestimation increased as sodium in meals increased. This study is the first to quantify underestimation of sodium content in real-world settings, among diners at restaurants.
These results are consistent with studies of sodium estimation in other types of settings. In a mail survey of 193 adults asked to estimate nutrient content of nine restaurant entrees, over 90% of participants underestimated sodium, and underestimation increased from 254% for the lowest sodium items (mean actual sodium=1,180 mg, mean estimated sodium=333 mg) to 811% for the highest sodium items (mean actual=4,890 mg, mean estimated=537 mg)(Burton et al., 2006). In an experimental study of 3,080 adults randomized to receive different labeling on restaurant menus, 18% of participants who were randomized to menu labels with sodium information were “shocked” by the amount of sodium in their meals (Scourboutakos et al., 2014). Taken together, these findings suggest meaningful misperceptions about sodium in restaurant foods, which is of particular concern given that 53% of U.S. adults, and up to 83% of adults who have received advice from a medical professional, report actively trying to reduce dietary sodium (Jackson et al., 2016).
This study found significant differences in sodium estimation by chain. Compared to McDonald’s, adolescents had worse estimates of sodium at Dunkin’ Donuts – findings that are likely related to consumer perceptions of the types of foods served at these restaurants. Core menu items at McDonald’s are mainly savory (e.g., hamburgers, French fries), while Dunkin’ Donuts sells primarily sweet foods (e.g., donut, pastries, muffins), which may be perceived as being lower in sodium. In a 2011 industry survey, 55% of consumers identified salty snacks, like chips and crackers, as having high amounts of sodium per serving, and 54% identified meats as high sodium. By contrast, only 3% identified baked goods, like cakes and muffins, as being high in sodium (International Food Information Council, 2011). Although a Dunkin’ Donuts muffin contains more than 20% of the recommended daily sodium limit (Dunkin’ Donuts, 2016), consumers may underestimate sodium because the food does not taste salty. Further investigation is needed to determine whether this phenomenon is consistent across similar restaurants.
This study found significant differences in sodium estimation by race and gender in the adult sample. Better estimation by women is consistent with prior studies of calorie menu labeling, which have found that women are more likely than men to report calorie information as helpful in guiding choices (Oh et al., 2015) and more likely to use calorie information when dining at fast-food restaurants (Chen et al., 2015). Better estimation by Asian adults might result from high sodium content of traditional Asian diets; this high sodium content could plausibly lead to greater awareness of salt in this population (Brown et al., 2009).
Awareness and use of calorie information appeared to have a modest association with sodium estimation in both samples. Among adults, better calorie estimation and noticing calories posted in the restaurant were associated with more accurate sodium estimates. In the adolescent sample, identifying calorie content of meals as an important factor when choosing restaurant items was associated with more accurate sodium estimates. These findings could be due to better overall nutrition knowledge among diners who can more accurately estimate calories, or the association could simply arise because of correlations between sodium and calorie content of meals (i.e., if higher calorie meals tend to also be higher in sodium, calorie labels are also conveying some information about sodium). If the latter is true, increasing the salience and use of calorie information may improve awareness of sodium for some items. Future studies are needed to assess how provision of calorie and sodium information, separately or in combination, influence consumer awareness of sodium, and, ultimately, sodium content of meals purchased.
Limitations
There are several limitations to this study that should be considered when interpreting results. During the study, diners who would likely qualify for inclusion based on age, but who chose not to participate, were tracked. Of those approached, 45% of adults and 49% of adolescents agreed to enroll in the study; this was not surprising considering the fast-paced environment in which data were collected. Nonresponse could bias effect estimates in either direction depending on characteristics of non-participants. If more educated diners were not motivated to participate in the study, due to the small monetary incentive, and those diners would have provided more accurate estimates of sodium, parameter estimates could have been biased away from the null. By contrast, diners with no interest in nutritional information might have been unmotivated to participate and less likely to correctly estimate sodium content, thereby biasing results toward the null. Due to the street intercept methodology, extensive questions about participant demographics and socioeconomic status could not be asked, and data on factors that may influence nutrition knowledge, such as income or education, were not collected. Additionally, actual food consumption could not be measured so this study relied on receipts and diner reports of foods purchased.
Conclusion
In this study of diners at six fast food restaurant chains in four New England cities, adults and adolescents substantially underestimated sodium, with underestimation greatest in the highest sodium meals. Adolescents at Dunkin’ Donuts underestimated sodium more than diners at other chains. Policies mandating provision of sodium information on menu boards, such as New York City’s Sodium Warning Label Resolution, may help correct consumer underestimation, particularly for meals of high sodium content.
Supplementary Material
Supplementary Figure 1. Mean (SE) actual and estimated sodium content of meals purchased by adults and adolescents dining in fast food restaurants in four cities in New England, 2013 and 2014.
Supplementary Figure 2. Difference between actual and estimated sodium content versus actual sodium content of adult meals in fast food restaurants in four cities in New England, 2013 and 2014. Underestimation of sodium content of meals was greater with larger meals.
Supplementary Figure 3. Difference between actual and estimated sodium content versus actual sodium content of adolescent meals in fast food restaurants in four cities in New England, 2013 and 2014. Underestimation of sodium content of meals was greater with larger meals.
Table 1.
Characteristics of adults and adolescents purchasing meals from fast food restaurant chains in four cities in New England, US, 2013 and 2014, and responses to questionnaire items. Figures are numbers (percentage of participants) unless stated otherwise. P-values are for Student’s t-tests (continuous variables) or Chi-square tests (categorical variables) for differences between participants who provided and could not provide an estimate of the amount of sodium in his/her meal.
| Adults | Adolescents | ||||||
|---|---|---|---|---|---|---|---|
| Provided estimate of sodium content of meal (n=593) | Did not provide estimate of sodium content of meal (n=176) | P-value | Estimated sodium content of meal (n=473) | Could not provide estimate of sodium content of meal (n=155) | P-value | ||
| Mean (SD; range) sodium purchased (mg) | 1292 (970; 0–4970) | 1280 (818; 0–4050) | 0.87 | 1128 (891;0–4435) | 1091 (823; 13–3665) | 0.65 | |
| Mean (SD; range) age (years) | 36.8 (14.2; 18–83) | 39.7 (15.6; 17–80) | 0.02 | 16.2 (2.7; 11–20) | 16.6 (2.8; 11–20) | 0.10 | |
| Mean (SD; range) BMI | 28.3 (5.9; 16.0–49.2) | 28.1 (6.3; 17.1–50.9) | 0.80 | 23.9 (4.8; 15.3–43.3) | 24.6 (5.7; 16.3–55.4) | 0.16 | |
| Year | 0.85 | <0.01 | |||||
| 2014 | 271 (46) | 79 (45) | 274 (58) | 110 (71) | |||
| 2013 | 322 (54) | 97 (55) | 199 (42) | 45 (29) | |||
| Gender | 0.83 | 0.82 | |||||
| Male | 328 (55) | 99 (56) | 249 (53) | 80 (52) | |||
| Female | 265 (45) | 77 (44) | 226 (47) | 75 (48) | |||
| Race | <0.001 | 0.90 | |||||
| White | 216 (36) | 85 (48) | 96 (20) | 30 (19) | |||
| Black | 201 (34) | 39 (22) | 182 (38) | 55 (35) | |||
| Hispanic | 112 (19) | 34 (19) | 116 (24) | 42 (27) | |||
| Asian | 28 (5) | 0 (0) | 24 (5) | 7 (5) | |||
| Other race | 36 (6) | 18 (10) | 57 (12) | 21 (14) | |||
| Taste important in food choice: | 0.01 | 0.06 | |||||
| A Lot | 481 (81) | 124 (70) | 356 (75) | 112 (72) | |||
| A Little | 86 (15) | 41 (23) | 84 (18) | 38 (25) | |||
| Not at All | 26 (4) | 11 (6) | 33 (7) | 5 (3) | |||
| Calories important in food choice: | 0.73 | 0.06 | |||||
| A Lot | 173 (29) | 46 (26) | 103 (22) | 21 (14) | |||
| A Little | 136 (23) | 43 (24) | 131 (28) | 42 (27) | |||
| Not at All | 284 (48) | 87 (49) | 239 (51) | 92 (59) | |||
| Price important in food choice: | 0.19 | <.01 | |||||
| A Lot | 265 (45) | 70 (40) | 140 (30) | 25 (16) | |||
| A Little | 177 (30) | 49 (28) | 163 (34) | 72 (46) | |||
| Not at All | 151 (25) | 57 (32) | 170 (36) | 58 (37) | |||
| Quick to eat important in food choice: | 0.16 | 0.16 | |||||
| A Lot | 301 (51) | 80 (45) | 154 (33) | 38 (25) | |||
| A Little | 161 (27) | 45 (26) | 154 (33) | 59 (38) | |||
| Not at All | 131 (22) | 51 (29) | 165 (35) | 58 (37) | |||
| Noticed calorie information in restaurant: | 0.15 | 0.47 | |||||
| Yes | 189 (32) | 61 (35) | 119 (25) | 41 (26) | |||
| No | 371 (63) | 99 (56) | 294 (62) | 89 (57) | |||
| Unsure | 33 (6) | 16 (9) | 60 (13) | 25 (16) | |||
| Estimate of daily sodium recommendation: | <0.001 | 0.07 | |||||
| Accurate (1000–3000 mg/day) | 98 (17) | 55 (31) | 137 (29) | 59 (38) | |||
| Underestimated (<1000 mg/day) | 486 (82) | 118 (67) | 314 (66) | 92 (59) | |||
| Overestimated (>3000 mg/day) | 9 (2) | 3 (2) | 22 (5) | 4 (3) | |||
Note: Boldface indicates statistical significance (p<0.05).
Acknowledgments
This study was reviewed by the Institutional Review Boards of Harvard Pilgrim Health Care (Protocol # 199069) and the Harvard T.H. Chan School of Public Health (Protocol# IRB15–2460). This study was funded by a grant from the Robert Wood Johnson Healthy Eating Research program (PI: Block) and the McLaughlin Family Foundation. Dr. Block was supported in this work by a career development award from NHLBI (K23 HL111211, PI: Block).
Financial disclosures statement: No financial disclosures were reported by authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: Authors have no conflicts of interest to declare.
References
- An R (2016). Fast-food and full-service restaurant consumption and daily energy and nutrient intakes in US adults. European Journal of Clinical Nutrition, 70 (1):97–103. doi: 10.1038/ejcn.2015.104 [DOI] [PubMed] [Google Scholar]
- Ayala C, Tong X, Valerrama A, Ivy A, Keenan N (2010). Actions taken to reduce sodium intake among adults with self-reported hypertension: HealthStyles survey, 2005 and 2008. Journal of Clinical Hypertension (Greenwich), 12 (10):793–9. doi: 10.1111/j.1751-7176.2010.00340.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block JP, Condon SK, Kleinman K, Mullen J, Linakis S, Rifas-Shiman S, Gillman MW (2013). Consumers’ estimation of calorie content at fast food restaurants: cross sectional observational study. British Medical Journal, 346:f2907. doi: 10.1136/bmj.f2907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown IJ, Tzoulaki I, Candeias V, Elliott P (2009). Salt intakes around the world: implications for public health. International Journal of Epidemiology, 38 (3):791–813. doi: 10.1093/ije/dyp139S. [DOI] [PubMed] [Google Scholar]
- Burton S, Creyer EH, Kees J, Huggins K (2006). Attacking the obesity epidemic: the potential health benefits of providing nutrition information in restaurants. American Journal of Public Health, 96 (9):1669–1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton S, Howlett E, Tangari AH (2009). Food for thought: how will the nutrition labeling of quick service restaurant menu items influence consumers’ product evaluations, purchase intentions, and choices? Journal of Retailing, 85 (3):258–273 [Google Scholar]
- Campos S, Doxey J, Hammond D (2011). Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutrition, 14 (8):1496–506. doi: 10.1017/S1368980010003290 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2012). Vital signs: food categories contributing the most to sodium consumption – United States, 2007–2008. MMWR Morbidity and Mortality Weekly Report, 61 (5):92–8. [PubMed] [Google Scholar]
- Chen R, Smyser M, Chan N, Ta M, Saelens BE, Krieger J (2015). Changes in awareness and use of calorie information after mandatory menu labeling in restaurants in King County, Washington. American Journal of Public Health, 105 (3):546–53. doi: 10.2105/AJPH.2014.302262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogswell ME, Yuan K, Gunn JP, Gillespie C, Sliwa S, Galuska DA et al. (2014). Vital signs: sodium intake among U.S. school-aged children – 2009–2010. MMWR Morbidity and Mortality Weekly Report, 63 (36), 789–97 [PMC free article] [PubMed] [Google Scholar]
- Dumanovsky T, Huang CY, Bassett MT, Silver LD (2010). Consumer awareness of fast-food calorie information in New York City after implementation of a menu labeling regulation. American Journal of Public Health, 100 (12):2520–5. doi: 10.2105/AJPH.2010.191908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkin’ Donuts (2016). Retrieved from http://www.dunkindonuts.com.
- Fitzpatrick L, Arcand J, L’Abbe M, Deng M, Duhaney T, Campbell N (2014). Accuracy of Canadian food labels for sodium content of food. Nutrients, 6 (8):3326–35. doi: 10.3390/nu6083326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D (2011). Health warning messages on tobacco products: a review. Tobacco Control, 20 (5):327–37. doi: 10.1136/tc.2010.037630 [DOI] [PubMed] [Google Scholar]
- International Food Information Council (2011). Consumer sodium research: concern, perceptions, and action. Retrieved from http://www.foodinsight.org.
- Jackson SL, Coleman King SM, Park S, Fang J, Odom EC, Cogswell ME (2016). Health professional advice and adult action to reduce sodium intake. American Journal of Preventive Medicine, 50 (1):30–9. doi: 10.1016/j.amepre.2015.04.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J Chan CL, Saelens BE, Ta ML, Solet D, Fleming DW (2013). Menu labeling regulations and calories purchased at chain restaurants. American Journal of Preventive Medicine, 44 (6):595–604. doi: 10.1016/j.amepre.2013.01.031 [DOI] [PubMed] [Google Scholar]
- Long MW, Tobias DK, Cradock AL, Batchelder H, Gortmaker SL (2015). Systematic review and meta-analysis of the impact of restaurant menu calorie labeling. American Journal of Public Health, 105 (5):e11–24. doi: 10.2105/AJPH.2015.302570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, Medicine. Institute of Medicine (2004). Dietary reference intakes: water, potassium, sodium, chloride, and sulfate. Retrieved from https://iom.nationalacademies.org/Reports/2004/Dietary-Reference-Intakes-Water-Potassium-Sodium-Chloride-and-Sulfate.aspx
- New York City Department of Health & Mental Hygiene & American Heart Association (2014). Concensus Statement on Sodium. Retrieved from http://www.nyc.gov/html/doh/html/pr2014/pr017-14.shtml
- New York City, NY, New York City Health Code, §81.49 (2015)
- Nguyen BT, Powell LM (2014). The impact of restaurant consumption among US adults: effects on energy and nutrient intakes. Public Health Nutrition, 17 (11):2445–52. doi: 10.1017/S1368980014001153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh A, Nguyen AB, Patrick H (2016). Correlates of reported use and perceived helpfulness of calorie information in restaurants among U.S. adults. American Journal of Health Promotion, 30 (4):242–9. doi: 10.1177/0890117116639565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Nguyen BT (2013). Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. Journal of the American Medical Association Pediatrics, 167 (1):14–20. doi: 10.1001/jamapediatrics.2013.417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Real S, Flint SW (2016). Menu labeling and food choice in obese adults: a feasibility study. BMC Obesity, 3 (17). doi: 10.1186/s40608-016-0095-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto CA, Wong D, Musicus A, Hammond D (2016). The influence of sugar-sweetened beverage health warning labels on parents’ choices. Pediatrics, 137 (2):e20153185. doi: 10.1542/peds.2015-3185 [DOI] [PubMed] [Google Scholar]
- Scourboutakos MJ, Corey PN, Mendoza J, Henson SJ, L’Abbe MR (2014). Restaurant menu labeling: is it worth adding sodium to the label? Canadian Journal of Public Health, 105 (5):e354–e361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urban LE, McCrory MA, Dallal GE (2011). Accuracy of stated energy contents of restaurant foods. Journal of the American Medical Association, 306 (3):287–93. doi: 10.1001/jama.2011.993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (2015). American Community Survey. State & City Quickfacts: Boston, MA, Hartford, CT, Springfield, MA, Providence, RI: Retrieved from http://quickfacts.census.gov [Google Scholar]
- VanEpps EM, Roberto CA (2016). The influence of sugar-sweetened beverage warnings: a randomized trial of adolescents’ choices and beliefs. American Journal of Preventive Medicine, 51 (5):664–672. doi: 10.1016/j.amepre.2016.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H, Sturm R (2013). What’s on the menu? A review of the energy and nutritional content of US chain restaurant menus. Public Health Nutrition, 16 (1):87–96. doi: 10.1017/S136898001200122X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. Mean (SE) actual and estimated sodium content of meals purchased by adults and adolescents dining in fast food restaurants in four cities in New England, 2013 and 2014.
Supplementary Figure 2. Difference between actual and estimated sodium content versus actual sodium content of adult meals in fast food restaurants in four cities in New England, 2013 and 2014. Underestimation of sodium content of meals was greater with larger meals.
Supplementary Figure 3. Difference between actual and estimated sodium content versus actual sodium content of adolescent meals in fast food restaurants in four cities in New England, 2013 and 2014. Underestimation of sodium content of meals was greater with larger meals.