Abstract
Objective
To assess contributing factors to increased obesity risk, by comparing children with autism spectrum disorder (ASD), developmental delays/disorders, and general population controls in weight status, and to examine associations between weight status and presence of co-occurring medical, behavioral, developmental, or psychiatric conditions across groups and ASD severity among children with ASD.
Study design
The Study to Explore Early Development is a multisite cross-sectional study of children, 2–5 years of age, classified as children with ASD (n = 668), children with developmental delays/disorders (n = 914), or general population controls (n = 884). Using an observational cohort design, we compared the 3 groups. Children’s heights and weights were measured during a clinical visit. Co-occurring conditions (medical, behavioral, developmental/psychiatric) were derived from medical records, interviews, and questionnaires. ASD severity was measured by the Ohio State University Global Severity Scale for Autism.
Results
The odds of overweight/obesity were 1.57 times (95% CI 1.24–2.00) higher in children with ASD than general population controls and 1.38 times (95% CI 1.10–1.72) higher in children with developmental delays/disorders than general population controls. The aORs were elevated for children with ASD after controlling for child co-occurring conditions (ASD vs general population controls: aOR = 1.51; 95% CI 1.14–2.00). Among children with ASD, those with severe ASD symptoms were 1.7 times (95% CI 1.1–2.8) more likely to be classified as overweight/obese compared with children with mild ASD symptoms.
Conclusions
Prevention of excess weight gain in children with ASD, especially those with severe symptoms, and in children with developmental delays/disorders represents an important target for intervention.
One in 5 children in the US general population, aged 2 to 19 years, meets criteria for obesity, defined as a body mass index (BMI) at or above the age- and sex-specific 95th percentile.1 The only age group that has seen a recent significant decrease in obesity prevalence is that of younger children, aged 2 to 5 years, from 13.9% to 8.4%.2 This age group is relevant as it is an important target for early obesity prevention. Children with developmental disabilities, including children with autism spectrum disorder (ASD), have been shown to be at increased risk for obesity. Hill et al reported that for ages 2–5 years, 32.1% of children with ASD compared with 23.5% of children with typical development met criteria for overweight (BMI-for-age between 85th and 94th percentile) and 16.0% of children with ASD compared with 10.1% of children with typical development met criteria for obesity.3
Although increased obesity rates among children with ASD have been documented by several studies,4–8 it remains to be examined if children with other non-ASD developmental disabilities are also at increased risk for developing obesity. Furthermore, mechanisms underlying higher obesity rates in children with ASD are poorly understood. There is evidence from cross-sectional studies that children with ASD are more selective in their food choices and show preferences for highly processed energy-dense foods, and healthier foods are often consumed less frequently.9–13 It is also possible that co-occurring medical, behavioral, developmental, or psychiatric conditions, such as endocrine abnormalities, genetic disorders, gastrointestinal symptoms, medication-associated side effects, sleep disturbances, aggression, attention-deficit/hyperactivity disorder, intellectual disability, or others may contribute to excess weight gain.14–16 Lastly, given that ASD is a spectrum disorder, more evidence is needed for whether children with more severe symptoms of autism are at greater risk of developing obesity than children with less severe symptoms. Earlier studies have measured severity of symptoms using the Autism Calibrated Severity Score (ACSS)3,17 but did not find any correlation with child weight status.
The primary aim of this study was to compare weight status for preschool children classified with ASD or non-ASD developmental delays/disorders, and general population controls. We also aimed to examine associations between child weight status and the presence of co-occurring medical, behavioral, developmental, or psychiatric conditions across groups, and associations between weight status and severity of ASD symptoms among the children with ASD.
Methods
The Study to Explore Early Development (SEED) is a multisite study of children born between September 1, 2003 and August 31, 2006 (aged 30–68 months) conducted in 6 sites across the US (in California, Colorado, Georgia, Maryland, North Carolina, and Pennsylvania). The SEED design used multiple-source, population-based ascertainment of 3 different groups: children who met study definition for ASD, children with developmental disorders other than ASD, and children drawn from the general population.18 The total enrolled sample included 3769 children. We used an unmatched observational design to compare the 3 groups. We excluded children from this analysis whose final case status could not be assigned because they did not complete the necessary developmental assessments or their results on developmental assessments were indeterminate (n = 584) and children who had either missing anthropometric data or biologically implausible values (BMI z scores <−4 or >5) (n = 849).19 The final sample included 2466 children (ASD: n = 668; developmental delays/disorders: n = 914; general population controls: n = 884).
Details of recruitment, screening, evaluation, and diagnosis have been published previously.18,20 Briefly, children eligible for inclusion in the ASD or developmental delays/disorders groups were identified from multiple special education and clinical sources providing services to children with disabilities. Children eligible for the general population controls group were randomly sampled from birth certificates from each site’s respective study area. During the invitation telephone call, caregivers of all children who enrolled in the study were administered the Social Communication Questionnaire (SCQ).21 All children who scored >11 on the SCQ were classified as possible ASD cases regardless of initial identification method. The cut-off of 11 on the SCQ was selected to maximize case-finding for this study.18
As part of the SEED data collection protocol all children were seen in person and administered the Mullen Scales of Early Learning to assess cognitive skills; anthropometric measurements were also obtained at the visit. Children with a pre-existing diagnosis of ASD and/or children who screened >11 on the SCQ completed additional assessments—the Autism Diagnostic Observation Schedule (ADOS)22,23 and their caregivers were administered the Autism Diagnostic Interview-Revised (ADI-R).24 Final ASD case classification was based on the findings from the ADOS and ADI-R.20 The clinician who conducted the in-person assessment completed the Diagnostic and Statistical Manual of Mental Disorders-IV checklist, adapted from the Ohio State University (OSU) Autism Rating Scale (OARS),25 which specifies frequency and severity of core symptoms of ASD. The study was approved by institutional review boards at the Centers for Disease Control and Prevention and all study sites. Written informed consent was obtained from the parents or guardians of the children who served as subjects of the investigation; assent was not obtained, as the subjects were too young.
Children’s height and weight were measured by trained study staff during the in-person clinic visit, with children wearing light clothing and shoes removed. Children’s age- and sex-specific BMI percentiles and z scores were calculated using the Centers for Disease Control and Prevention Growth Charts 2000.26 Children were classified as underweight (BMI-for-age <5th percentile), normal weight (BMI-for-age 5th-84th percentile), overweight (BMI-for-age 85th-94th percentile), or obese (BMI-for-age ≥95th percentile).
Medical history for all children was obtained from several sources: a telephone interview with the child’s primary care-giver (98% biological mother) that included questions on whether a healthcare provider had previously diagnosed the child with various medical, developmental, and psychiatric conditions; abstraction of child medical records for genetic conditions; and self-administered questionnaires completed by the primary caregiver with questions about previously diagnosed asthma, allergies, autoimmune conditions, gastrointestinal conditions, and gastrointestinal and sleep disorder symptoms. Additional data about the child’s behavioral and sensory difficulties were ascertained from another caregiver questionnaire, the Child Behavior Checklist27—and from the ADI-R. Co-occurring conditions were selected based on their frequency in the sample and potential for effect on children’s weight status. They were divided into 2 categories: medical conditions or symptoms and behavioral, developmental, or psychiatric conditions or symptoms. Individual subjects might have more than 1 co-occurring condition. Table I provides a Levy et al comprehensive list of co-occurring conditions, their frequency in each group, and significant differences between each group.
Table I.
Frequency of co-occurring medical, behavioral, developmental, and psychiatric conditions by group
| Characteristics | ASD n = 668 |
Developmental delays/ disorders n = 914 |
General population controls n = 884 |
P value |
|---|---|---|---|---|
| Medical conditions or symptoms | ||||
| Asthma, n (%) | 40 (6.0%) | 41 (4.5%) | 52 (5.9%) | .308 |
| Birth defects, n (%) | 37 (5.5%) | 68 (7.4%) | 20 (2.3%) | <.001†,‡ |
| Cardiac diseases/disorders, n (%) | 26 (3.9%) | 42 (4.6%) | 11 (1.2%) | <.001†,‡ |
| Endocrine diseases/disorders, n (%) | 10 (1.5%) | 20 (2.2%) | 4 (0.5%) | .007†,‡ |
| Gastrointestinal disorders/symptoms, n (%) | 161 (24.1%) | 165 (18.1%) | 154 (17.4%) | .002*,† |
| Genetic disorders, n (%) | 24 (3.6%) | 51 (5.6%) | 9 (1.0%) | <.001†,‡ |
| Immune disorders, n (%) | 0 (0%) | 4 (0.4%) | 5 (0.6%) | .169 |
| Metabolic disorders, n (%) | 2 (0.3%) | 3 (0.3%) | 2 (0.2%) | .917 |
| Neurological abnormalities/symptoms, n (%) | 47 (7.0%) | 47 (5.1%) | 10 (1.1%) | <.001†,‡ |
| Renal diseases/disorders, n (%) | 6 (0.9%) | 9 (1.0%) | 14 (1.6%) | .369 |
| Respiratory diseases/disorders, n (%) | 3 (0.5%) | 1 (0.1%) | 1 (0.1%) | .253 |
| Seizure disorders, n (%) | 24 (3.6%) | 26 (2.8%) | 1 (0.1%) | <.001†,‡ |
| Behavioral, developmental or psychiatric conditions or symptoms | ||||
| ADHD, n (%) | 52 (7.8%) | 65 (7.1%) | 5 (0.6%) | <.001†,‡ |
| Behavioral problems, n (%) | 104 (15.6%) | 81 (8.9%) | 18 (2.0%) | <.001*,†,‡ |
| Cognitive delay (Mullen < 70), n (%) | 5 (0.8%) | 2 (0.2%) | 2 (0.2%) | .157 |
| Feeding difficulties, n (%) | 48 (7.2%) | 34 (3.7%) | 22 (2.5%) | <.001*,† |
| Motor delay, n (%) | 127 (19.0%) | 138 (15.1%) | 11 (1.2%) | <.001*,†,‡ |
| Psychiatric disorders§ | 25 (3.7%) | 20 (2.2%) | 4 (0.5%) | <.001†,‡ |
| Sensory disorders, n (%) | 188 (28.1%) | 99 (10.8%) | 9 (1.0%) | <.001*,†,‡ |
| Sleep problems, n (%) | 43 (6.4%) | 24 (2.6%) | 5 (0.6%) | <.001*,†,‡ |
| Speech delay, n (%) | 426 (63.8%) | 525 (57.4%) | 76 (8.6%) | <.001*,†,‡ |
ADHD, attention-deficit/hyperactivity disorder; n, sample size.
Statistically significant difference between children with ASD and children with developmental delays/disorders (P < .05).
Statistically significant difference between children with ASD and general population control children (P < .05).
Statistically significant difference between developmental delays/disorders and general population controls children (P < .05).
Including bipolar disorder, obsessive compulsive disorder, oppositional defiant disorder, and personality disorder.
Autism severity was measured in subjects that met the SEED ASD case definition using the ACSS28 and by quantifying functional impairment using the OARS.25 The severity scores for the ADOS Calibrated Severity Score were derived from the ADOS scores, resulting in a calibrated severity metric based on ADOS raw totals.29 The OARS was completed by the senior clinician, who considered all available information collected on a child. The OARS is based on the clinical global impression scale,30 with a Likert score indicating a range of severity from 1 (no autism in evidence) to 7 (“classic” autism) as a measure of impairment and clinician certainty of a diagnosis of ASD. Children with a score of 1, in the range of non-ASD, were not included as cases. For the purpose of this study, we followed the rubric of the Research Unit on Pediatric Psychopharmacology OARS clinical global impression,31 where scores 2–3 were in the mild range of severity (n = 139; 21%), scores 4–5 moderate severity (n = 328; 49%), and scores 6–7 severe (n = 150; 22%). Twenty-four children (3.5%) had a missing clinical global impression score and were not included in this analysis.
Statistical Analyses
Bivariate analyses to assess baseline differences for each aim and child weight outcomes were computed for all covariates of interest first, using ANOVA, Kruskal-Wallis, independent t tests, or Wilcoxon tests for continuous variables and χ2 or Fisher exact tests for categorical variables. Pairwise differences between categories of case status were assessed similarly.
Associations between study group and categorical variables were determined using Cochran-Mantel-Haenszel χ2 test and determined between group membership and continuous variables using ANOVA. Multivariable logistic regression models were developed to assess the association between the presence of co-occurring medical, behavioral, developmental, and psychiatric conditions and child weight outcomes. An unadjusted model was run for the outcome of overweight/obese with child classification as the predictor variable. A second model was run for the outcome with the predictor of child classification adjusting for demographic variables, including child sex, child age at time of assessment, child race/ethnicity, mother’s education, and poverty status. Poverty status was determined using the US Census Bureau 2015 Poverty Thresholds.32 A third model was run for the outcome with the predictor of child classification adjusting for child medical and behavioral confounders. The third model did not contain demographic variables because of collinearity and model instability. Subanalyses were run for those with autism using a bivariate logistic regression model to determine the unadjusted and adjusted effects (using same confounders) of autism severity on child weight status. All analyses were conducted in SAS v 9.3 (SAS Institute, Cary, North Carolina), and a P value of <.05 was considered statistically significant.
Results
Children were, on average, 59 months of age across groups (Table II). A significantly higher proportion of children with ASD were male (82%), and a higher proportion of mothers of general population controls children were white (71%). A significantly smaller proportion of mothers in the ASD (79%) and developmental delays/disorders (76%) groups attended college compared with mothers in the general population control group (88.4%). A significantly higher proportion of mothers in the ASD group (11%) lived below the poverty level compared with mothers in the developmental delays/disorders (4%) and general population control (6%) groups. Children in the ASD and developmental delays/disorders groups showed significantly higher mean BMI z scores (0.35 ± 1.16 and 0.26 ± 1.20, respectively) than children in the general population control (0.14 ± 1.12) group (P < .02). Children with ASD or developmental delays/disorders also had higher frequencies of overweight/obesity (ASD 27.5%, developmental delays/disorders 25.0%) compared with general population control children (19.5%) (P < .007).
Table II.
Demographic and anthropometric characteristics of children by group*
| Characteristics | ASD n = 668 |
Developmental delays/disorders n = 914 |
General population controls n = 884 |
P value* |
|---|---|---|---|---|
| Children | ||||
| Age (mo), mean ±SD | 59.3 ± 6.6 | 59.2 ± 7.2 | 59.2 ± 7.4 | .99 |
| Sex (male/female), n (%) | 545 (81.6%) / 123 (18.4%) | 605 (66.2%) / 309 (33.8%) | 462 (52.3%) / 422 (47.7%) | <.001 |
| BMI z score, mean ±SD | 0.35 ± 1.16 | 0.26 ± 1.20 | 0.14 ± 1.12 | .001 |
| Weight status, n (%) | .007 | |||
| Underweight (BMI-for-age <5th percentile) | 30 (4.5%) | 44 (4.8%) | 56 (6.3%) | |
| Normal-weight (BMI-for-age 5–84th percentile) | 454 (68.0%) | 642 (70.2%) | 656 (74.2%) | |
| Overweight (BMI-for-age 85–94th percentile) | 101 (15.1%) | 125 (13.7%) | 103 (11.7%) | |
| Obese (BMI-for-age ≥95th percentile) | 83 (12.4%) | 103 (11.3%) | 69 (7.8%) | |
| Mothers | ||||
| Education, n (%) | <.001 | |||
| Less than high school | 43 (6.6%) | 81 (9.1%) | 26 (3.1%) | |
| High school | 92 (14.2%) | 130 (14.7%) | 73 (8.6%) | |
| Some college or more | 515 (79.2%) | 676 (76.2%) | 751 (88.4%) | |
| Race/ethnicity, n (%) | <.001 | |||
| White | 408 (61.1%) | 583 (63.8%) | 646 (73.1%) | |
| Black | 123 (18.4%) | 154 (16.9%) | 94 (10.6%) | |
| Asian | 58 (8.7%) | 42 (4.6%) | 39 (4.4%) | |
| American Indian or Pacific Islander | 5 (0.8%) | 7 (0.1%) | 5 (0.6%) | |
| Multiracial | 27 (4.0%) | 43 (4.7%) | 36 (4.1%) | |
| Hispanic | 21 (3.1%) | 43 (4.7%) | 19 (2.2%) | |
| Below federal poverty level, n (% yes) | 68 (10.7) | 93 (4.0) | 47 (5.7) | <.001 |
Cochran-Mantel-Haenszel χ2 test.
Association between Medical, Behavioral, Developmental, and Psychiatric Conditions and Child Weight Status
Table I presents the frequency of co-occurring conditions by group status. Co-occurring conditions that did not differ by case status included asthma, immune disorders, metabolic disorders, renal disease, respiratory disorders, and cognitive delay (by Mullen). Children in the ASD and developmental delays/disorders groups had more frequent history of birth defects; cardiac, genetic, endocrine, neurologic disorders/symptoms; seizure disorder; attention-deficit/hyperactivity disorder; and psychiatric disorders. Behavior problems, motor delay, sensory disorders, sleep problems, and speech delay were more common in ASD >developmental delays/disorders >general population controls children, respectively.
In bivariate analyses, based on the entire sample, several co-occurring medical conditions (ie, asthma; birth defects; endocrine diseases/disorders and genetic disorders) and speech delay were associated with overweight/obesity (Table III). No other medical conditions or symptoms or behavioral, developmental, or psychiatric conditions or symptoms were associated with weight status.
Table III.
Frequency of co-occurring medical, behavioral, developmental and psychiatric conditions by weight status for groups combined
| Characteristics | Children with underweight/ normal weight n = 1882 |
Children with overweight/obesity n = 584 |
P value |
|---|---|---|---|
| Medical conditions or symptoms | |||
| Asthma, n (%) | 78 (4.1%) | 55 (9.4%) | <.001 |
| Birth defects, n (%) | 85 (4.5%) | 40 (6.8%) | .025 |
| Cardiac diseases/disorders, n (%) | 57 (3.0%) | 22 (3.8%) | .376 |
| Endocrine diseases/disorders, n (%) | 17 (0.9%) | 17 (2.9%) | <.001 |
| Gastrointestinal disorders/symptoms, n (%) | 368 (19.6%) | 112 (19.2%) | .841 |
| Genetic disorders, n (%) | 49 (2.6%) | 35 (6.0%) | <.001 |
| Immune disorders, n (%) | 5 (0.3%) | 4 (0.7%) | .229 |
| Metabolic disorders, n (%) | 4 (0.2%) | 3 (0.5%) | .367 |
| Neurological abnormalities/symptoms, n (%) | 72 (3.8%) | 32 (5.5%) | .082 |
| Renal diseases/disorders, n (%) | 19 (1.0%) | 10 (1.7%) | .169 |
| Respiratory diseases/disorders, n (%) | 4 (0.2%) | 1 (0.2%) | .846 |
| Seizure disorder, n (%) | 36 (1.9%) | 15 (2.6%) | .331 |
| Behavioral, developmental or psychiatric conditions or symptoms | |||
| ADHD, n (%) | 91 (4.8%) | 31 (5.3%) | .645 |
| Behavioral problems, n (%) | 153 (8.1%) | 50 (8.6%) | .740 |
| Cognitive delay (Mullen < 70), n (%) | 6 (0.3%) | 3 (0.5%) | .450 |
| Feeding difficulties, n (%) | 83 (4.4%) | 21 (3.6%) | .392 |
| Motor delay, n (%) | 199 (10.6%) | 77 (13.2%) | .084 |
| Psychiatric disorders, n (%) | 34 (1.8%) | 15 (2.6%) | .239 |
| Sensory disorders, n (%) | 231 (12.3%) | 65 (11.1%) | .457 |
| Sleep problems, n (%) | 50 (2.7%) | 22 (3.8%) | .164 |
| Speech delay, n (%) | 745 (39.6%) | 282 (48.3%) | <.001 |
We examined associations between child weight status and presence of co-occurring conditions using multivariate logistic regression models (Table IV). In unadjusted analyses, children with ASD were 1.57 times (95% CI 1.24–2.00) more likely and children with developmental delays/disorders were 1.38 times (95% CI 1.10–1.72) more likely to have overweight or obesity than general population control children (P < .005). These associations remained statistically significant between ASD vs general population control children when controlling for demographic covariates for ASD vs general population controls (P = .002) and co-occurring medical, behavioral, and/or developmental/psychiatric conditions (P = .004). After adjusting the model for co-occurring conditions, the difference between developmental delays/disorders group and general population controls in child weight status was not significant (P = .157).
Table IV.
Associations between child weight status at ages 2–5 years and the presence of co-occurring medical, behavioral, and/or developmental/psychiatric conditions across groups
| Unadjusted (n = 2466) |
Adjusted for demographic covariates* (n = 2204) |
Adjusted for child medical, behavioral, and/or developmental/ psychiatric conditions† (n = 2466) |
||||
|---|---|---|---|---|---|---|
| Child classifications | OR (95% CI) |
P value | OR (95%CI) |
P value | OR (95% CI) |
P value |
| ASD vs developmental delays/disorders | 1.14 (0.91, 1.43) |
.245 | 1.18 (0.93, 1.50) |
.181 | 1.25 (0.99, 1.59) |
.063 |
| ASD vs general population controls | 1.57 (1.24, 2.00) |
<.001 | 1.50 (1.16, 1.94) |
.002 | 1.51 (1.14, 2.00) |
.004 |
| Developmental delays/disorders vs general population controls | 1.38 (1.10, 1.72) |
.005 | 1.27 (1.00, 1.62) |
.047 | 1.20 (0.93, 1.56) |
.157 |
Demographic covariates are child age, child sex, maternal race (proxy for child race), maternal education, and poverty status.
Child medical, behavioral, and developmental/psychiatric co-occurring conditions include the following categories: allergy-mediated, cardiac, and endocrine conditions; genetic conditions or birth defects; gastrointestinal disorders and symptoms; hematologic, immune, infectious, neurologic, medication-associated, and renal conditions; sleep, eating, and behavioral difficulties; attentional and cognitive conditions; hearing loss; and psychiatric conditions.
Association between Weight Outcome and Severity of ASD Symptoms
Children with ASD, whose severity of ASD symptoms were higher (moderate or severe) using the OARS were 1.71 times (95% CI 1.06–2.75) more likely to have overweight or obesity (P = .026) compared with children with mild ASD symptoms (Figure). In contrast, children with moderate or severe ASD symptoms, quantified using the ACSS, did not show any statistical differences between those with mild, moderate, or severe symptoms of autism and the presence of overweight or obesity (P = .858).
Figure.
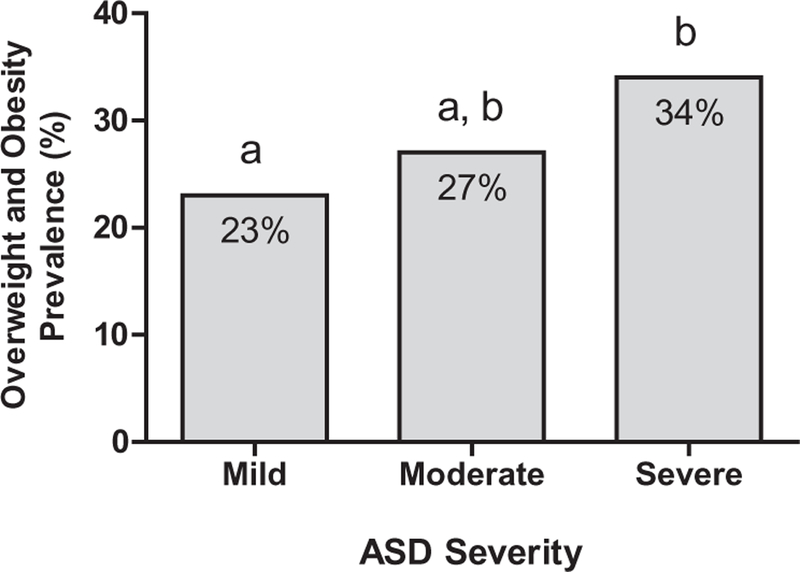
Prevalence (%) of overweight and obesity in children with ASD, aged 2–5 years, by ASD severity status (n = 668). Severity was measured with the OARS. For OARS, means with different letters are significantly different (P < .05).
Discussion
Data from this study showed that children with ASD or with developmental delays/disorders had increased prevalence of overweight or obesity than general population control children. When controlling for a range of co-occurring medical, behavioral, and developmental/psychiatric conditions children with ASD were more likely to have overweight or obesity than children with developmental delays/disorders or general population controls. In addition, this study showed that among children with ASD, those with more severe symptoms had significantly higher odds of being classified overweight or obese.
Among children with ASD, the prevalence estimate for overweight/obesity (BMI-for-age ≥85th percentile) was 27.5% and prevalence estimate for obesity (BMI-for-age ≥95th percentile) was 12.4%. These rates are slightly lower than prevalence estimates for overweight/obesity (32.1%) and obesity (16.0%) from a sample of 2- to 5-year-old children with ASD in the Autism Speaks—Autism Treatment Network.3 Our data further showed that among children with developmental delays/disorders, prevalence estimates for overweight/obesity and obesity alone were 25.0% and 11.3%, respectively. There are limited data available from prior studies about obesity prevalence rates for children with developmental delays/disorders in this age range. A review paper that summarized data from 3 nationally representative data sources (ie, National Health and Nutrition Examination Survey [2005–2012; ages 5–27 years]; National Health Interview Survey [2008–2013; child ages 12–17 years]; National Survey of Children’s Health [2011; child ages 10–17 years]) indicated that youth with disabilities or special healthcare needs have a higher prevalence of obesity (27%–59%) than their peers without disabling conditions or special needs.33 In the current analysis, prevalence estimates for overweight/obesity (19.5%) and obesity alone (7.8%) among general population controls children were slightly lower compared with estimates from a nationally representative sample of children with typical development (overweight/obesity: 23.4%; obesity alone: 10.1%).3 Despite these small differences in overall obesity prevalence rates, however, our analy-ses showed that children with ASD were 1.57 times more likely, and children with developmental delays/disorders were 1.38 times more likely, to have overweight or obesity than general population control children and, therefore, represent impor-tant targets for intervention.
Our findings show that children with developmental delays/disorders and ASD both had elevated obesity risk. One study reported that children with intellectual disability had increased obesity risk.34 The current findings are novel as they provide support that children with developmental delays/disorders (without ASD diagnosis) are at an equally high risk of developing obesity. Prevention efforts should focus on this group also, not just children with ASD. Our data also showed that the differences in risk for developmental delays/disorders and general population controls did not persist when controlling for co-occurring conditions. Studies are needed that delineate the specific co-occurring condition(s) that exert an impact on the likelihood of overweight or obesity in this heterogeneous population.
Our study identified co-occurring conditions in the entire sample and ASD status that were associated with increased odds for overweight or obesity, such as medical conditions, including asthma, endocrine disorders, and known genetic syndromes. This is consistent with other studies that report elevated risk of overweight or obesity in children with non-ASD learning or behavioral disorders and genetic disorders (such as Down syndrome) and medical conditions (such as asthma).35 A recent review of medical factors associated with childhood obesity reported associations with genetic disorders, endocrine disorders, and use of medication.36 However, children in our sample with reported or measured cognitive delays did not have increased risk of overweight or obesity. This differs from Pan et al, who reported increased obesity in individuals with moderate intellectual disability (without genetic disorders).37 This difference may be partially explained by the inclusion of older individuals (7–18 years of age) in the study of Pan et al and that children in our sample did not have as significant cognitive impairment.
In our sample, seizures and neurologic abnormalities or symptoms were not associated with increased risk of overweight/obesity. A recent study of adults with epilepsy reported increased risk of obesity.38 Our findings may be related to the small number of subjects in our sample with reported epilepsy (n = 89) and younger age. In our sample, sleep problems were not found to be associated with increased risk of overweight/obesity, which is not consistent with other studies where sleep abnormalities were associated with higher risk.14,39 However, in a large clinical sample of preschool children with autism, sleep, eating, and behavioral difficulties were also not found to be associated with obesity.40
This study reported severity of symptoms using standardized criteria of severity, such as the ACSS and OARS clinical global impression, informed by gold standard tools and Diagnostic and Statistical Manual of Mental Disorders-IV criteria. Few studies have examined the correlation of severity of ASD symptoms and the risk for overweight or obesity in pre-school children.14,41,42 We measured severity of autism in pre-school children using 2 measures: the ACSS and the OARS. When severity of ASD symptoms was measured using the ACSS, we did not find a relationship of severity of ASD symptoms with the presence of overweight or obesity. However, the ACSS measures severity of ASD symptoms, independent of other developmental factors, such as language and adaptive abilities,28 and may not take into account the overall degree of impairment, which may be related to co-occurring and noncore symptoms.
In children with more severe impairment measured using the OARS, they were 70% more likely to have overweight or obesity. The OARS measures severity of global child functioning and is most impacted by adaptive abilities and expressive language skills.
Other studies have reported similar findings. Ho et al used an assessment tool (the Childhood Autism Rating Scale), a tool developed for screening and diagnosis, to quantify severity of symptoms, and found that children with more severe symptoms were more likely to have obesity.42 A study of older pre-schoolers (average age 5.5 years) used the ADOS Calibrated Severity Score and did not find a correlation to BMI status.17 A number of factors, in addition to the presence of co-occurring medical conditions, may account for increased risk of obesity with more severe autism symptoms. In an older population, McCoy et al reported that adolescents with ASD had increased risk factors for obesity associated with their decreased frequency of physical activity.43 Other co-occurring behavioral difficulties, which may be under-reported (by caregiver history), may have significant impact on known factors associated with obesity, such as unusual nutrient intake, high sugar content of diet, selective diet, elimination diets (or other non-traditional treatments), and others.
The large, geographically diverse sample, the thorough case-classification based on in-person examinations, and measured child anthropometric data are considered strengths of this study. Limitations include a possible recall bias of maternally reported co-occurring conditions, and possible selection bias in the study sample.44
A prior analysis of characteristics of responders and nonresponders during recruitment revealed that several demographic characteristics, such as maternal age, education, and race/ethnicity, were associated with nonresponse.45 We adjusted for these demographic factors and co-occurring conditions in this analysis and have no reason to believe that a child’s BMI would have independently impacted response to the recruitment letter.
Our findings indicate that children with ASD or developmental delays/disorders are more likely to be classified as overweight/obese by age 5 years. The association for children with ASD remained statistically significant when controlling for a range of medical, behavioral, and developmental/psychiatric co-occurring conditions, which suggests that developmental disabilities, such as ASD, confer an independent risk of overweight and obesity in children. Children with ASD with a higher degree of impairment and more severe symptoms were found to be at even greater risk of developing over-weight and obesity. Although the mechanisms underlying these associations are less well understood, children who receive a diagnosis of ASD or developmental delays/disorders could potentially benefit from enhanced monitoring for the development of obesity and anticipatory guidance for their parents in an effort to prevent obesity.
Acknowledgments
Supported by Centers for Disease Control and Prevention Cooperative Agreement Numbers U10DD000180 (Colorado Department of Public Health); U10DD000181 (Kaiser Foundation Research Institute [CA]); U10DD000182 (University of Pennsylvania); U10DD000183 (Johns Hopkins University); U10DD000184 (University of North Carolina at Chapel Hill); and U10DD000498 (Michigan State University).
Glossary
- ACSS
Autism Calibrated Severity Score
- ADI-R
Autism Diagnostic Interview-Revised
- ADOS
Autism Diagnostic Observation Schedule
- ASD
Autism spectrum disorder
- BMI
Body mass index
- OSU
Ohio State University
- OARS
OSU autism rating scale
- SCQ
Social Communication Questionnaire
- SEED
Study to Explore Early Development
Footnotes
The authors declare no conflicts of interest.
References
- 1.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 Through 2013–2014. JAMA 2016;315:2292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill AP, Zuckerman KE, Fombonne E. Obesity and autism. Pediatrics 2015;136:1051–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Criado KK, Sharp WG, McCracken CE, De Vinck-Baroody O, Dong L, Aman MG, et al. Overweight and obese status in children with autism spectrum disorder and disruptive behavior. Autism 2018;22:450–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawson LM, Foster L. Sensory patterns, bbesity, and physical activity participation of children with autism spectrum disorder. Am J Occup Ther 2016;70:7005180070 p1–8. [DOI] [PubMed] [Google Scholar]
- 6.Must A, Eliasziw M, Phillips SM, Curtin C, Kral TV, Segal M, et al. The effect of age on the prevalence of obesity among US youth with autism spectrum disorder. Child Obes 2017;13:25–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Granich J, Lin A, Hunt A, Wray J, Dass A, Whitehouse AJ. Obesity and associated factors in youth with an autism spectrum disorder. Autism 2016;20:916–26. [DOI] [PubMed] [Google Scholar]
- 8.Corvey K, Menear KS, Preskitt J, Goldfarb S, Menachemi N. Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Matern Child Health J 2016;20:466–76. [DOI] [PubMed] [Google Scholar]
- 9.Schmitt L, Heiss CJ, Campbell EE. A comparison of nutrient intake and eating behaviors of boys with and without autism. Topics Clin Nutr 2008;23:23–31. [Google Scholar]
- 10.Evans EW, Must A, Anderson SE, Curtin C, Scampini R, Maslin M, et al. Dietary patterns and body mass index in children with autism and typically developing children. Res Autism Spectr Disord 2012;6:399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schreck KA, Williams K. Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Res Dev Disabil 2006;27:353–63. [DOI] [PubMed] [Google Scholar]
- 12.Hubbard KL, Anderson SE, Curtin C, Must A, Bandini LG. A comparison of food refusal related to characteristics of food in children with autism spectrum disorder and typically developing children. J Acad Nutr Diet 2014;114:1981–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, et al. Food selectivity in children with autism spectrum disorders and typically developing children. J Pediatr 2010;157:259–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broder-Fingert S, Brazauskas K, Lindgren K, Iannuzzi D, Van Cleave J. Prevalence of overweight and obesity in a large clinical sample of children with autism. Acad Pediatr 2014;14:408–14. [DOI] [PubMed] [Google Scholar]
- 15.Barnhill K, Gutierrez A, Ghossainy M, Marediya Z, Marti CN, Hewitson L. Growth status of children with autism spectrum disorder: a case-control study. J Hum Nutr Diet 2017;30:59–65. [DOI] [PubMed] [Google Scholar]
- 16.Scahill L, Jeon S, Boorin SJ, McDougle CJ, Aman MG, Dziura J, et al. Weight gain and metabolic consequences of risperidone in young children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2016;55:415–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zuckerman KE, Hill AP, Guion K, Voltolina L, Fombonne E. Overweight and obesity: prevalence and correlates in a large clinical sample of children with autism spectrum disorder. J Autism Dev Disord 2014;44:1708–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schendel DE, Diguiseppi C, Croen LA, Fallin MD, Reed PL, Schieve LA, et al. The Study to Explore Early Development (SEED): a multisite epidemiologic study of autism by the Centers for Autism and Developmental Disabilities Research and Epidemiology (CADDRE) network. J Autism Dev Disord 2012;42:2121–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. A SAS program for the 2000 CDC growth charts (ages 0 to <20 years) https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed July 25, 2018.
- 20.Wiggins LD, Reynolds A, Rice CE, Moody EJ, Bernal P, Blaskey L, et al. Using standardized diagnostic instruments to classify children with autism in the study to explore early development. J Autism Dev Disord 2015;45:1271–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rutter M, Bailey A, Lord C. SCQ: Social Communication Questionnaire Los Angeles (CA): Western Psychological Services; 2003. [Google Scholar]
- 22.Lord C, Rutter M, DiLavore PC, Risi S. Autism diagnostic observation schedule 2nd ed. Los Angeles (CA): Western Psychological Services; 2012. [Google Scholar]
- 23.Gotham K, Risi S, Pickles A, Lord C. The Autism Diagnostic Observation Schedule: revised algorithms for improved diagnostic validity. J Autism Dev Disord 2007;37:613–27. [DOI] [PubMed] [Google Scholar]
- 24.Rutter M, Le Couteur A, Lord C. The autism diagnostic interview-revised Los Angeles (CA): Western Psychological Services; 2003. [Google Scholar]
- 25.The Ohio State University (OSU) Research Unit on Pediatric Psychopharmacology OSU Autism Rating Scale (OARS) and Clinical Global Impression (CGI) 2005. [Google Scholar]
- 26.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002;109:45–60. [DOI] [PubMed] [Google Scholar]
- 27.Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev 2000;21:265–71. [DOI] [PubMed] [Google Scholar]
- 28.Wiggins LD, Barger B, Moody E, Soke G, Pandey J, Levy S. Brief Report: the ADOS Calibrated Severity Score best measures autism diagnostic symptom severity in pre-school children. J Autism Dev Disord 2017;doi: 10.1007/s10803-017-3072-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord 2009;39:693–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choque Olsson N, Bolte S. Brief report: “Quick and (not so) dirty” assessment of change in autism: cross-cultural reliability of the Developmental Disabilities CGAS and the OSU Autism CGI. J Autism Dev Disord 2014;44:1773–8. [DOI] [PubMed] [Google Scholar]
- 31.Research Units on Pediatric Psychopharmacology Autism. OSU Research Unit on Pediatric Psychopharmacology (OSU RUPP): OSU Autism Rating Scale—DSM-IV (OARS-4) 2005.
- 32.United States Census Bureau. Poverty thresholds by size of family and number of children 2015.
- 33.Bandini L, Danielson M, Esposito LE, Foley JT, Fox MH, Frey GC, et al. Obesity in children with developmental and/or physical disabilities. Disabil Health J 2015;8:309–16. [DOI] [PubMed] [Google Scholar]
- 34.Segal M, Eliasziw M, Phillips S, Bandini L, Curtin C, Kral TV, et al. Intellectual disability is associated with increased risk for obesity in a nationally representative sample of U.S. children. Disabil Health J 2016;9:392–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips KL, Schieve LA, Visser S, Boulet S, Sharma AJ, Kogan MD, et al. Prevalence and impact of unhealthy weight in a national sample of US adolescents with autism and other learning and behavioral disabilities. Matern Child Health J 2014;18:1964–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar S, Kelly AS. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc 2017;92:251–65. [DOI] [PubMed] [Google Scholar]
- 37.Pan CC, Davis R, Nichols D, Hwang SH, Hsieh K. Prevalence of overweight and obesity among students with intellectual disabilities in Taiwan: a secondary analysis. Res Dev Disabil 2016;53–54:305–13. [DOI] [PubMed] [Google Scholar]
- 38.Ladino LD, Hernandez-Ronquillo L, Tellez-Zenteno JF. Obesity and its association with generalised epilepsy, idiopathic syndrome, and family history of epilepsy. Epileptic Disord 2014;16:343–53. [DOI] [PubMed] [Google Scholar]
- 39.Dev DA, McBride BA, Fiese BH, Jones BL, Cho H. Risk factors for overweight/obesity in preschool children: an ecological approach. Child Obes 2013;9:399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Vinck-Baroody O, Shui A, Macklin EA, Hyman SL, Leventhal JM, Weitzman C. Overweight and obesity in a sample of children with autism spectrum disorder. Acad Pediatr 2015;15:396–404. [DOI] [PubMed] [Google Scholar]
- 41.Egan AM, Dreyer ML, Odar CC, Beckwith M, Garrison CB. Obesity in young children with autism spectrum disorders: prevalence and associated factors. Child Obes 2013;9:125–31. [DOI] [PubMed] [Google Scholar]
- 42.Ho HH, Eaves LC, Peabody D. Nutrient intake and obesity in children with autism. Focus Autism Other Dev Disabl 1997;12:187–92. [Google Scholar]
- 43.McCoy SM, Jakicic JM, Gibbs BB. Comparison of obesity, physical activity, and sedentary behaviors between adolescents with autism spectrum disorders and without. J Autism Dev Disord 2016;46: 2317–26. [DOI] [PubMed] [Google Scholar]
- 44.DiGuiseppi CG, Daniels JL, Fallin DM, Rosenberg SA, Schieve LA, Thomas KC, et al. Demographic profile of families and children in the Study to Explore Early Development (SEED): case-control study of autism spectrum disorder. Disabil Health J 2016;9:544–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bradley CB, Browne EN, Alexander AA, Collins J, Dahm JL, DiGuiseppi CG, et al. Demographic and operational factors predicting study comple-tion in a multisite case-control study of preschool children. Am J Epidemiol 2018;187:592–603. [DOI] [PMC free article] [PubMed] [Google Scholar]


