Abstract
Objective
To investigate individual preferences or characteristics for physical activity (PA) attributes in adults with chronic knee pain, to identify clusters of individuals with similar preferences, and to identify whether individuals in these clusters differ by their demographic and health characteristics.
Design
An adaptive conjoint analysis was conducted using the PAPRIKA method to determine preference weights representing the relative importance of six physical activity attributes. Cluster analysis was performed to identify clusters of participants with similar weights. Chi-square and ANOVA with Bonferroni correction were used to assess differences in individual characteristics by cluster. Multinomial logistic regression was used to assess associations between individual characteristics and cluster assignment.
Results
The study sample included 146 participants; mean age 65, 72% female, 47% white, non-Hispanic. The six attributes (mean weights in parentheses) are: health benefit (0.26), enjoyment (0.24), convenience (0.16), financial cost (0.13), effort (0.11) and time cost (0.10). Three clusters were identified: Cluster 1 (n=33): for whom enjoyment (0.35) is twice as important as health benefit; Cluster 2 (n=63): for whom health benefit (0.38) is most important; and Cluster 3 (n=50): for whom cost (0.18), effort (0.18), health benefit (0.17) and enjoyment (0.18) are equally important. Cluster 1 was healthiest, Cluster 2 most self-efficacious, and Cluster 3 was in poorest health.
Conclusions
Patients with chronic knee pain have preferences for PA that can be distinguished effectively using ACA methods. Adults with chronic knee pain, clustered by PA preferences, share distinguishing characteristics. Understanding preferences may help clinicians and researchers target interventions better tailor PA interventions.
Keywords: Conjoint analysis, stated choice, physical activity, knee, osteoarthritis, preferences
INTRODUCTION
Symptomatic knee osteoarthritis (KOA) affects 14 million people in the US1 and presents clinically as knee pain, stiffness, functional loss, and reduced quality of life.2 KOA is the leading cause of disability in older adults and the 11th highest contributor to global disability.3 Physical activity (PA) – any movement produced by skeletal muscles requiring energy expenditure4 – is a universally accepted recommendation for improving pain, function, and quality of life in people with KOA.5,6 Insufficient PA is associated with disability onset and progression,7 representing 20% of KOA-related disability,8 and is a potential reason for the societal increase in KOA over time.9 Unfortunately, the average adult with KOA spends two-thirds of daily awake time in sedentary activities.10
Clinical guidelines recommend PA regardless of disease severity. All PA intensities (light and moderate-to-vigorous) and modes (e.g., aerobic, resistance training) provide the potential for improvement in pain or function in people with KOA.11,12 Many factors across the socio-ecological spectrum affect PA adherence in adults with knee pain.12–16 Sustained behavior change depends on individual decision-making concerning self-management.17 In order to accommodate the multi-factorial nature of PA engagement, there is a need to assess individual preferences when attempting to facilitate PA adherence.12,18
Adaptive conjoint analysis (ACA) is a method originating in mathematical psychology19 and economics20 that is used increasingly in health care to capture individual preferences related to health care services.21 ACA is based on the premise that a health care service can be described by its attributes or characteristics, and the value of the service depends on the levels of the attributes.22 Among other uses, ACA can serve as a means to estimate the relative importance of different attributes of a service.22 A recent example from the rheumatoid arthritis literature combined preference elicitation and statistical population segmentation (clustering) methods to derive ‘preference phenotypes’ to guide medical treatment decisions in the management of rheumatoid arthritis.23
The purpose of this study was to conduct an ACA with individuals who experience chronic knee pain to (1) determine the relative importance of attributes associated with PA, and (2) investigate whether clusters of individuals with similar preferences (preference phenotypes) for PA exist and, if so, to investigate whether individuals in these clusters differ by their sociodemographic and health characteristics.
METHODS
Participants and procedures
Participants were recruited at community senior centers and resource fairs and from general internal medicine clinics at Northwestern Medicine, the Shirley Ryan AbilityLab (formerly the Rehabilitation Institute of Chicago) and via flyers posted on the Northwestern University medical campus, Chicago, USA.
Participants self-reported knee pain, ache or stiffness on most days of at least one month during the last year, were at least 45 years old, expressed interest in increasing or maintaining PA, and had no prior history of knee replacement on the side of complaint. Participants underwent a standing, fixed-flexion knee x-ray to identify presence of KOA, completed the online ACA, and answered patient-reported outcome measures. Participants provided informed consent, and the Northwestern University Institutional Review Board approved all aspects of the study.
Descriptive characteristics and health outcomes
Sociodemographic factors.
Participants reported ethnicity, age, gender, education, income, and the presence of comorbidities were captured on a demographic and health history form. The presence of comorbidities was defined as having more than one comorbidity from a list of comorbidities from the Modified Charlson Comorbidity Index.24 Body mass index (BMI) was calculated from measured height and weight (kg/m2).
Patient-Reported Outcomes.
Pain Interference, Physical Function, Ability to Participate in Social Roles and Activities, and Satisfaction with Social Roles and Activities were measured using the Patient-Reported Outcomes Measurement Information System (PROMIS) in Assessment CenterSM (https://www.assessmentcenter.net). PROMIS computer adaptive tests were used and the scoring of each factor assessed results in a T-score.25 Self-efficacy for engaging in physical activity was captured using the Self-Efficacy for Exercise Scale.26
Knee Radiograph.
Radiograph were acquired using a standing fixed flexion view.27 Films were assessed for KOA presence by co-author LS using the Kellgren and Lawrence (KL) radiographic criteria.28 Presence of KOA was defined using the established and widely used definition of radiographic KOA, KL grade ≥ 2.
Conjoint analysis
A qualitative process was used to determine the six attributes and their levels for the ACA (Table 1).29 We used a community-based participatory research approach to recruit and conduct five focus groups at three locations in Chicago, USA to identify attributes of PA. In the last three focus groups, we conducted attribute prioritization exercises to begin the process of attribute selection for the ACA. We consolidated the total number of attributes from 27 attributes to six attributes by grouping those with overlapping domains, e.g. ‘intensity’ and ‘pace’ were combined to form ‘physical activity effort’ and removing those that were incapable of being traded (‘sharp’ knee pain) or not experimentally manipulable, e.g., previous physical activity experience. Finally, we conducted semi-structured interviews and pilot testing to develop instructions and to use language that was acceptable by participants with chronic knee pain. Full details of the qualitative process have been previously reported.29
Table 1.
Attributes and their Levels
| Attribute | Attribute Level | Description |
|---|---|---|
| Health benefits | Low | Small relief in discomfort, small increase in strength and ability to move |
| Medium | Moderate relief in discomfort, moderate increase in strength and ability to move | |
| High | Large relief in discomfort, large increase in strength and ability to move | |
| Enjoyment | Low | You are bored and would rather be doing something else |
| Medium | You could ‘take it or leave it’ | |
| High | You are absorbed in the activity, you find it exhilarating and feel euphoric | |
| Convenience* | Low | With ease and minimal need for modification |
| Medium | With some need for modification | |
| High | With difficulty and large need for modification | |
| Physical activity effort | Low | You can sing during the activity |
| Medium | You can talk, but can’t sing, during the activity | |
| High | You can’t say more than a few words without pausing for breath | |
| Monthly cost | Low | $20 per month |
| Medium | $50 per month | |
| High | $80 per month | |
| Time per physical activity occasion | Low | 10–44 minutes |
| Medium | 45–89 minutes | |
| High | 90 minutes or more |
How well the activity fits into your schedule
An online ACA used 1000minds software30 which implements the Potentially All Pairwise RanKings of all possible Alternatives (PAPRIKA) method.31 PAPRIKA is based on pairwise ranking – i.e., choosing one alternative from two possibilities. Each participant reviewed pairs of hypothetical PAs defined on two attributes at a time (assuming all other attributes were identical) and involving a trade-off. Participants indicated which PA they preferred, including favoring them equally (indifference). All participants were instructed that the purpose of the study was to help people with knee pain to “start and maintain physical activity programs”. An example of a pairwise-ranking question is: Which of these two PAs do you prefer: Either PA#1 which requires ‘45–89 minutes’ of time and ‘low’ effort, or PA#2 which requires ‘10–44 minutes’ of time and ‘high’ effort? Participants read pairs of PA and were asked to choose which PA they preferred. An example question from 1000minds software is in Figure 1 (additional examples are included in the Appendix).
Figure 1.
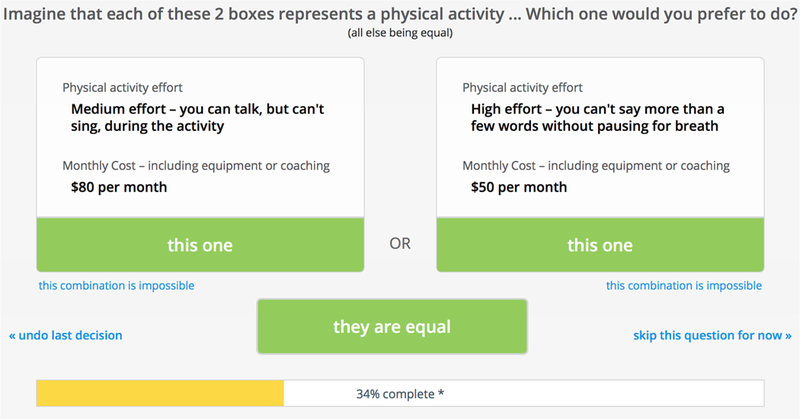
Example of a pairwise-ranking question from 1000minds conjoint analysis software
The PAPRIKA method is computer-adaptive and minimizes the number of questions each participant needs to answer. ‘Part-worth utilities’ (weights) representing the relative importance of the attributes are derived by PAPRIKA for each participant. Hansen and Ombler provide methodological details.31 The weights are averaged across all participants.
Cluster analysis
Clustering sorts objects according to their similarity on one or more dimensions and identifies groups that maximize within-group similarity and minimize between-group similarity.32 The ACA yielded preference rankings of the six attributes for each participant. We used a hierarchical clustering approach to identify preference clusters,32,33 known as average-linkage clustering.33 The first level of clustering aggregates the data into pairs of points forming the base level of clusters; the next level of clusters is obtained by considering each recently formed cluster as the new data points for clustering.32 Hierarchical clustering often produces multiple solutions, and so it is necessary to decide on the number of clusters that fits the data. Various algorithms exist to assess the fit of clustering schemes; we used the NBClust package in R (R Core Team 2013, Vienna, Austria) to determine the optimal number of clusters for our data.34 NBClust assesses clustering schemes across 30 indices and identifies the best clustering scheme based on the greatest agreement across indices.34 Using this method, a three-cluster scheme was identified as the best for this analysis. Chi-square and ANOVA were used to assess differences in patient characteristics and health outcomes by cluster.
Consistency test
1000minds software allows for three pairwise-ranking questions to be repeated at the end of the ACA, as a test of preference consistency. Based on the literature concerning inconsistent preferences our main analysis included all participants.35–37 We conducted a sensitivity analysis by removing from the analysis those who inconsistently answered two or three (all) repeated questions.
Cluster assignment
We used multinomial logistic regression to identify whether participant sociodemographic and health characteristics were associated with preference cluster assignment.38 Predictor variables included PROMIS Pain Interference score, Self-Efficacy for Exercise Scale score, presence of a co-morbidity, presence of radiographic KOA, age, gender, and BMI. A 5-point (1/2 SD) difference in T-score was used as a conservative level of important difference in PROMIS Pain Interference score.39 All analyses were performed using STATA version 15 (Stata Corp, College Station, Texas, USA).
RESULTS
Of the 150 participants who completed the ACA, four had incomplete responses and were excluded, resulting in 146 participants with usable data. Participants were 72% female, 48% white (39% black/African American), with a mean age of 65 years. Sociodemographic characteristics are reported in Table 2. On average, each participant answered 35 questions to complete the ACA, taking an average of 13 minutes. Only 12% of participants inconsistently answered two or three (all) of the repeat questions.
Table 2.
Physical Activity Preference Weights, Socio-Demographics and Health Factors by Cluster
| Full sample n=146 |
Cluster 1 n=33 |
Cluster 2 n=63 |
Cluster 3 n=50 |
|
|---|---|---|---|---|
| Physical activity preference weights* | ||||
| Health benefits | 0.26 (0.13) | 0.18 (0.07) | 0.38 (0.07)† | 0.17 (0.08) |
| Enjoyment | 0.24 (0.09) | 0.35 0.07)† | 0.23 (0.06) | 0.18 (0.07)‡ |
| Convenience | 0.16 (0.07) | 0.18 (0.08) | 0.15 (0.04) | 0.16 (0.07) |
| Effort | 0.11 (0.09) | 0.08 (0.06) | 0.06 (0.05) | 0.18 (0.09)† |
| Cost | 0.11 (0.08) | 0.12 (0.08) | 0.10 (0.04) | 0.18 (0.10)† |
| Time | 0.10 (0.07) | 0.09 (0.06) | 0.08 (0.05) | 0.13 (0.10)‡ |
| Socio-demographic characteristics (%) | ||||
| Sex (female) | 72 | 73 | 63 | 82 |
| Age (65 years and older) | 47 | 52 | 41 | 50 |
| Race (White/Caucasian) | 47 | 52 | 43 | 50 |
| Education (bachelors or greater) | 60 | 61 | 63 | 56 |
| Family income (< $25000USD/year) | 46 | 43 | 42 | 55§ |
| Health factors (mean [SD] unless indicated) | ||||
| PROMIS Pain Interference T-Score | 57.7 (7.1) | 55.2 (7.0) | 56.9 (6.6) | 60.2 (6.9) † |
| PROMIS Physical Function T-Score | 43.2 (7.3) | 46.5 (6.6) | 43.5 (7.5) | 40.5 (6.5) || |
| PROMIS Ability to Participate in Social Roles and Activities T-Score |
48.7 (7.7) | 51.7 (8.5) | 49.4 (6.7) | 46.0 (7.7) || |
| PROMIS Satisfaction with Social Roles and Activities T-Score |
47.6 (9.3) | 51.1 (10.3) | 47.3 (7.8) | 45.6 (9.8) || |
| Self-Efficacy for Exercise Scale score | 5.5 (2.7) | 5.5 (2.7) | 6.2 (2.2) | 4.5 (2.9) ¶ |
| Any comorbidity (%) | 52 | 44 | 44 | 69§ |
| BMI (% >30 kg/m2) | 47 | 39 | 46 | 50 |
| Radiographic KOA (% KL grade II or higher)** | 62 | 52§ | 68 | 62 |
PROMIS = Patient-Reported Outcomes Measurement Information System. T-score range 0–100, general population mean=50, SD=10; Self-Efficacy for Exercise Score range 0–10, higher scores = greater self-efficacy.
Preference weights– higher values represent greater importance related to physical activity choice, physical activity attributes were used for cluster analysis. Significant differences in preferences between clusters are expected due to the clustering technique and do not represent meaningful findings.
Value significantly higher than other two clusters at P<0.05 level
Cluster 3 is significantly different than Cluster 2 at P<0.05
Significantly different frequency than expected at P<0.05 level
Cluster 3 is significantly lower than Cluster 1 at P<0.05.
Participants who declined having an X-ray due to recent or numerous knee radiographs in medical management were assumed to have KL grade II or higher.
Table 2 also shows the mean preference weights for PA attributes for the entire sample and by preference clusters. Three clusters were identified by the cluster analysis, as depicted in Figure 2. For the entire sample, enjoyment and health benefit were of greatest importance with little difference between them. Significant differences between clustering variables exist for all physical activity attributes except ‘convenience’. Among Cluster 1 participants, enjoyment was the most important attribute: approximately twice as important as health benefit and convenience. In contrast, health benefit was the most important attribute for Cluster 2 participants: 62% more important than enjoyment. Cluster 3 participants found enjoyment, cost, effort, and health benefit to be of nearly equal importance. For both the entire sample and the three clusters, time was the least important attribute.
Figure 2.
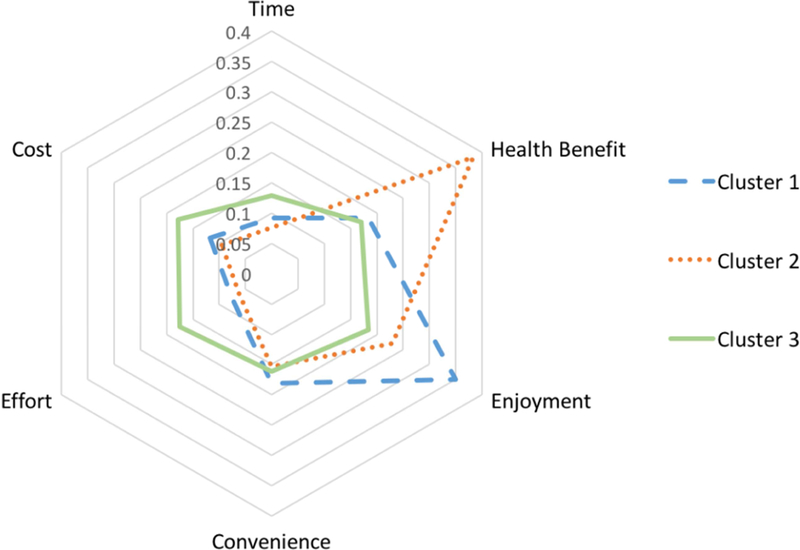
Preference weights* for physical activity attributes by cluster
* Preference weights – higher values represent greater importance related to physical activity choice
Table 2 shows participant characteristics and outcomes by cluster. Cluster 1 participants had better scores on all PROMIS measures than Clusters 2 and 3, and Cluster 1 had the fewest participants with radiographic KOA. Differences between Cluster 1 and Cluster 3 were greatest for pain interference (5.1, 95% CI: 2.0 to 8.1, p=0.004), physical function (6.0, 95% CI: 2.9 to 9.1, p=0.001), Ability to Participate in Social Roles and Activities (5.8, 95% CI: 2.5 to 9.1, p=0.002), and Satisfaction with Social Roles with Roles and Activities (5.5, 95% CI: 1.4 to 9.5, p=0.025). Differences between Cluster 1 and 2 were only significant for physical function (3.0, 95% CI: 0.03 to 6.0, p=0.048). Cluster 2 participants had significantly higher self-efficacy than Cluster 3 (15.4, 95% CI: 6.7 to 24.1, p=0.002). Despite statistical significance, the lower bounds of the 95% confidence intervals for all comparisons are less than the minimal important difference indicating that we cannot have 95% confidence that the differences between clusters were clinically significant.
Cluster assignment
Table 3 shows the results of the multinomial logistic regression, assessing the association between clinical characteristics and cluster assignment by reporting relative risk ratio comparing each cluster to reference cluster 3. With a likelihood chi-square of 38.84 (p<0.0004), the multinomial logistic regression fit significantly better than a model without predictors. Each 5-point increase in PROMIS Pain Interference score decreases the likelihood of assignment to Cluster 1 versus 3, (RRR 0.53, 95% CI: 0.34 to 0.86), and each 3-point increase in Self Efficacy for Exercise Scale score doubles the likelihood of assignment to Cluster 2 versus 3, (RRR 2.10, 95% CI: 1.16 to 3.87).
Table 3.
Relative risk ratios (and 95% confidence intervals) from multinomial logistic regression analyses assessing associations between predictors and cluster assignment
| Cluster 1 | Cluster 2 | Cluster 3 | |||
|---|---|---|---|---|---|
| Enjoyment | Health benefit | Constrained | |||
| Predictors | RRR* | 95% CI | RRR* | 95% CI | |
| Female gender | 0.88 | 0.26 to 2.96 | 1.69 | 0.62 to 4.59 | Reference |
| Any comorbidity | 0.57 | 0.19 to 1.69 | 0.54 | 0.22 to 1.36 | |
| Self-Efficacy for Exercise Scale score† | 1.00 | 0.91 to 1.06 | 2.10‡ | 1.16 to 3.87 | |
| PROMIS pain interference T score† | 0.53‡ | 0.34 to 0.86 | 0.70 | 0.47 to 1.05 | |
| Radiographic KOA (KL grade II or higher) | 0.30‡ | 0.10 to 0.96 | 1.00 | 0.35 to 2.83 | |
| Age (65 or greater) | 0.75 | 0.26 to 2.21 | 0.38‡ | 0.15 to 0.97 | |
| BMI (>= 30) | 1.62 | 0.53 to 4.96 | 1.96 | 0.76 to 5.18 | |
KOA=knee osteoarthritis, OR = adjusted odds ratio, 95% CI = 95% Confidence Interval, multinomial logistic regression includes all predictors in Table 3.
Adjusted Relative Risk Ratio (RRR) from multinomial logistic regression including all predictors in Table 3 compares each cluster to referent cluster 3.
The adjusted RRR was scaled to ½ SD (5 point) change in PROMIS score and a 3-point change in Self Efficacy for Exercise Scale.
P<0.05
DISCUSSION
This study finds that health benefit and enjoyment are the most important attributes associated with the decision to engage in PA for adults with KOA. In the whole sample, health benefit and enjoyment are approximately twice as important as the cost of PA, the physical activity effort of PA, or the time needed to engage in PA. Cluster analysis identified three subgroups. Clusters 1 and 2 participants weighted enjoyment and health benefit as more important than Cluster 3 participants, whereas Cluster 3 participants weighted effort, cost and time higher. Cluster 1 participants valued enjoyment more than health benefit and Cluster 2 participants valued health benefit more than enjoyment.
Participant characteristics were related to cluster assignment. The risk of being assigned to Cluster 1 (relative to Cluster 3) decreased with each unit increase in the PROMIS Pain Interference score, suggesting that participants were less likely to be in the cluster that most valued enjoyment with increasing levels of pain interference. The risk of assignment to Cluster 2 (relative to Cluster 3) increased with each unit increase in the Self-Efficacy for Exercise Scale score, suggesting that participants with greater self-efficacy were more likely to be in the cluster that placed the greatest value on health benefit.
Few studies describe the trade-offs specific to PA in older adults. Franco et al.40 used a best-worst scaling (case 2, profile case) survey in adults with a history of falls or disability and found non-health attributes to be of greater importance than health attributes. In our study, health benefit was either the most or second most important attribute depending on the preference cluster. There are several potential reasons for this difference in reported preference. Our study only considered one health attribute (compared to three in the Franco et al. study), and we described health differently. Our study used general terms to convey that health benefits can be improved to a small, moderate or large degree. The Franco et al. study included specific levels of improvement, reported as percentages and, for falls, changes were shown as improvement in falls risk. Risk attributes can be understood differently by how they are framed, and an examination of such framing has been suggested.41 The authors conducted a pilot study where participants were “able to answer the scenarios presented without reporting excessive difficulty,” but an examination of risk attribute framing was not specifically reported.
Our findings highlight the variability of patient’s values for physical activity and may have implications for how clinicians and researchers interact with people with chronic knee pain who express an interest in being more active. Cluster 1 participants were slightly younger and healthier and experienced less interference in their daily activities due to their knee complaints. These participants may have been more inclined to consider a PA framed as enjoyable versus a PA with known health benefits for managing KOA. Advances in exercise psychology that reframe PA within the context of a social experience42 may be effective for individuals similar to those in Cluster 1. PA alternatives without social experiences can be structured to emphasize enjoyment. Partfitt, Alrumh, and Rowlands43 used affect-regulated exercise prescription with high retention rates and increased cardiovascular fitness when participants were instructed to ‘feel good’. Zenko, Ekkekakis, and Ariely44 affected post-exercise pleasure, remembered pleasure and forecasted pleasure in an treadmill training exercise by ordering exercise intensity. These strategies may be suited optimally for individuals like those with Cluster 1’s characteristics.
Cluster 2 participants had a greater interest in the health benefit of PA and had higher levels of self-efficacy for exercise. Therefore, individuals like Cluster 2 participants may be more likely to adhere to PA regimens that are likely to improve, pain, function, and quality of life. Recent meta-analyses have shown structured exercise programs led by a trained instructor and delivered at a frequency of 3 times per week over 12 weeks deliver the greatest effect over the short term.12 With higher levels of self-efficacy, individuals like Cluster 2 participants may also be better suited for self-management strategies.45
Cluster 3 participants were older, had the most co-morbidities, lowest levels of education, lowest self-efficacy, and fewest financial resources. They appear to be resource constrained or otherwise disadvantaged and may have little ability to conceive of incorporating PA into their lives. Strategies to build self-efficacy coupled with an incremental lifestyle PA approach may be most suitable for individuals similar to Cluster 3 participants.46
Limitations:
ACA results are affected by the selection of PA attributes and how they are worded. Important physical activity attributes may have been omitted from the study and the wording of attributes may have created a scenario in which more than one construct was considered in a single attribute. For example, the importance attributed to health benefit may have differed if specific health benefits, such as physical function or pain, were separately addressed. With respect to attribute wording, our enjoyment attribute included the word ‘bored’ as part of the lowest attribute level description; it could be argued that ‘bored’ represents a different construct. When developing the attributes for this study we followed a robust qualitative research process, as suggested for stated choice experiments.47,48 When writing attribute level descriptions we selected and tested words expressed by respondents of focus groups, semi-structured interviews, and pilot-studies. Our use of participant language may limit the generalizability of conclusions related to the enjoyment attribute.
Our study had a modest sample size. Minimum sample sizes in ACA depend on several considerations, including the question format, the complexity of the task, the desired precision of the results, and the need to conduct subgroup analyses.21 Despite this, the identification of three distinct clusters – Cluster 1 (n=33), Cluster 2 (n=63), Cluster 3, (n=50) – was robust, even after removal of participants with inconsistent preferences as a sensitivity analysis. Likewise, the sensitivity analysis did not alter our main findings (see Appendix, Tables S1 and S2).
The generalizability of these findings is affected by our inclusion criteria and our sample’s characteristics. In particular, we recruited individuals interested in increasing or maintaining their physical activity, and so the findings may be most relevant to people like them. Our sample also had an average BMI of 31kg/m2, 46% earned less than USD$25,000 per year, and 50% had at least one comorbidity. In characterizing our sample, we did not assess current level of physical activity which may influence preferences. The dynamic nature of a person’s preferences in the context of their physical activity experiences is a subject for future research.
Finally, there is need for caution when interpreting stated preferences as they may represent an ideal rather than realistic decision-making setting. The behavioral science literature suggests that systematic biases make it difficult for individuals to fully understand and control their decisions.49,50 These biases are also present when considering physical activity with some variance between physical activity intention and physical activity behavior explained by factors outside of our rational conscious.51,52 For example, stairwell use increases with natural lighting, stairwell visibility, music, artwork, and point-of-decision messaging.53,54 Consequently, behavioral economic interventions seek to change behavior through external interventions, i.e. ‘nudges’, versus engaging executive function. Nonetheless, ACA may inform how to create ideal physical activity conditions, to which behavioral strategies can be added to further optimize adherence.55 Despite its limitations, this study lays the foundation for preference-aligned PA intervention studies in adults with chronic knee pain.
In conclusion, adults with chronic knee pain have preferences for PA that can be distinguished effectively using ACA methods. Adults with chronic knee pain, clustered by physical activity preferences, share distinguishing characteristics. This study provides new evidence for targeting and framing specific PA attributes as a novel strategy for developing PA interventions.
Supplementary Material
Acknowledgements:
The authors would like to thank the study participants.
Role of the funding source:
The study was funded through an Agency for Healthcare Research and Quality training award (K12HS023011) and The Foundation for Physical Therapy’s Center on Health Services Training and Research. This study was supported by P60-AR064464 from the National Institute for Arthritis and Musculoskeletal Diseases and by the Northwestern University Clinical and Translational Science (NUCATS) Institute, Grant Number UL1TR001422.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest:
PH is a co-inventor of 1000minds conjoint analysis software. All other authors have declared that no competing interests exist.
Contributor Information
Daniel Pinto, Marquette University, Walter Schroeder Complex, Room 346, P.O. Box 1881, Milwaukee, WI 53201-1881, 414-288-4495.
Ulf Bockenholt, Northwestern University, Kellogg School of Management, Evanston, IL, USA.
Julia Lee, Department of Preventive Medicine - Biostatistics, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Rowland W. Chang, Institute for Public Health and Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Leena Sharma, Department of Medicine (Rheumatology), Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Daniel J. Finn, Center for Healthcare Studies, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Allen W. Heinemann, Shirley Ryan AbilityLab, Chicago, IL, USA.
Jane L. Holl, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Paul Hansen, Department of Economics, University of Otago, Dunedin, New Zealand.
References
- 1.Deshpande BR, Katz JN, Solomon DH, et al. Number of Persons With Symptomatic Knee Osteoarthritis in the US: Impact of Race and Ethnicity, Age, Sex, and Obesity. Arthritis Care Res (Hoboken) 2016;68(12):1743–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Felson DT. Developments in the clinical understanding of osteoarthritis. Arthritis Res Ther 2009;11:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014;73(7):1323–1330. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Physical Activity 2014; http://www.who.int/topics/physical_activity/en/. Accessed Accessed June 22, 2014.
- 5.Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64(4):465–474. [DOI] [PubMed] [Google Scholar]
- 6.McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22(3):363–388. [DOI] [PubMed] [Google Scholar]
- 7.Dunlop DD, Song J, Semanik PA, et al. Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: prospective cohort study. BMJ 2014;348:g2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis National Health Interview Survey, 2002. Am J Prev Med 2006;30:385–393. [DOI] [PubMed] [Google Scholar]
- 9.Wallace IJ, Worthington S, Felson DT, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A 2017;114(35):9332–9336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 2008;167(7):875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White DK, Lee J, Song J, Chang RW, Dunlop D. Potential Functional Benefit From Light Intensity Physical Activity in Knee Osteoarthritis. Am J Prev Med 2017;53(5):689–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bennell KL, Dobson F, Hinman RS. Exercise in osteoarthritis: moving from prescription to adherence. Best Pract Res Clin Rheumatol 2014;28(1):93–117. [DOI] [PubMed] [Google Scholar]
- 13.Holden MA, Nicholls EE, Young J, Hay EM, Foster NE. Role of exercise for knee pain: what do older adults in the community think? Arthritis Care Res (Hoboken) 2012;64(10):1554–1564. [DOI] [PubMed] [Google Scholar]
- 14.Petursdottir U, Arnadottir SA, Halldorsdottir S. Facilitators and barriers to exercising among people with osteoarthritis: a phenomenological study. Phys Ther 2010;90(7):1014–1025. [DOI] [PubMed] [Google Scholar]
- 15.Stone RC, Baker J. Painful Choices: A Qualitative Exploration of Facilitators and Barriers to Active Lifestyles Among Adults With Osteoarthritis. J Appl Gerontol 2015. [DOI] [PubMed]
- 16.Veenhof C, van Hasselt TJ, Koke AJ, Dekker J, Bijlsma JW, van den Ende CH. Active involvement and long-term goals influence long-term adherence to behavioural graded activity in patients with osteoarthritis: a qualitative study. Aust J Physiother 2006;52(4):273–278. [DOI] [PubMed] [Google Scholar]
- 17.Brug J, Oenema A, Ferreira I. Theory, evidence and Intervention Mapping to improve behavior nutrition and physical activity interventions. Int J Behav Nutr Phys Act 2005;2(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann Phys Rehabil Med 2016;59(3):174–183. [DOI] [PubMed] [Google Scholar]
- 19.Luce RD. Individual Choice Behavior: A Theoretical Analysis New York: John Wiley & Sons, Inc.; 1959. [Google Scholar]
- 20.McFadden D Conditional Logit Analysis Of Qualitative Choice Behaviour. In: Zarembka P, ed. Frontiers in Econometrics New York, NY: Academic Press; 1974:105–142. [Google Scholar]
- 21.Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health--a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14(4):403–413. [DOI] [PubMed] [Google Scholar]
- 22.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ 2000;320(7248):1530–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fraenkel L, Nowell WB, Michel G, Wiedmeyer C. Preference phenotypes to facilitate shared decision-making in rheumatoid arthritis. Ann Rheum Dis 2017. [DOI] [PMC free article] [PubMed]
- 24.Intakes IoMUPoMaSCotSEoDR. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids / Panel on Macronutrients, Panel on the Definition of Dietary Fiber, Subcommittee on Upper Reference Levels of Nutrients, Subcommittee on Interpretation and Uses of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine of the National Academies Washington, DC: National Academies Press; 2005. [Google Scholar]
- 25.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap Cooperative Group During its First Two Years. Medical care 2007;45(5 Suppl 1):S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Resnick B, Jenkins LS. Testing the reliability and validity of the Self-Efficacy for Exercise scale. Nurs Res 2000;49(3):154–159. [DOI] [PubMed] [Google Scholar]
- 27.Botha-Scheepers S, Kloppenburg M, Kroon HM, et al. Fixed-flexion knee radiography: the sensitivity to detect knee joint space narrowing in osteoarthritis. Osteoarthritis Cartilage 2007;15(3):350–353. [DOI] [PubMed] [Google Scholar]
- 28.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pinto D, Danilovich MK, Hansen P, et al. Qualitative Development of a Discrete Choice Experiment for Physical Activity Interventions to Improve Knee Osteoarthritis. Arch Phys Med Rehabil 2016. [DOI] [PubMed]
- 30.1000minds - Decision-making software 2017; https://www.1000minds.com/.
- 31.Hansen P, Ombler F. A New Method for Scoring Additive Multi-attribute Value Models Using Pairwise Rankings of Alternatives. Journal of Multi-Criteria Decision Analysis 2008;15:87–107. [Google Scholar]
- 32.Henry DB, Tolan PH, Gorman-Smith D. Cluster analysis in family psychology research. J Fam Psychol 2005;19(1):121–132. [DOI] [PubMed] [Google Scholar]
- 33.Manning CD, Raghavan P, Schütze H. Hierarchical Clustering. Introduction to Information Retrieval Cambridge, England: Cambridge University Press; 2008. [Google Scholar]
- 34.Charrad M, Ghazzali N, Boiteau V, Niknafs A. NbClust: An R Package for Determining the Relevant Number of Clusters in a Data Set. J Statistical Software 2014;61(6):1–36. [Google Scholar]
- 35.Lancsar E, Louviere J. Deleting ‘irrational’ responses from discrete choice experiments: a case of investigating or imposing preferences? Health Econ 2006;15(8):797–811. [DOI] [PubMed] [Google Scholar]
- 36.Miguel FS, Ryan M, Amaya-Amaya M. ‘Irrational’ stated preferences: a quantitative and qualitative investigation. Health Econ 2005;14(3):307–322. [DOI] [PubMed] [Google Scholar]
- 37.Ryan M, Watson V, Entwistle V. Rationalising the ‘irrational’: a think aloud study of discrete choice experiment responses. Health Econ 2009;18(3):321–336. [DOI] [PubMed] [Google Scholar]
- 38.Dominguez-Almendros S, Benitez-Parejo N, Gonzalez-Ramirez AR. Logistic regression models. Allergol Immunopathol (Madr) 2011;39(5):295–305. [DOI] [PubMed] [Google Scholar]
- 39.Chen CX, Kroenke K, Stump TE, et al. Estimating minimally important differences for the PROMIS pain interference scales: results from 3 randomized clinical trials. Pain 2018;159(4):775–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Franco MR, Howard K, Sherrington C, et al. Eliciting older people’s preferences for exercise programs: a best-worst scaling choice experiment. J Physiother 2015;61(1):34–41. [DOI] [PubMed] [Google Scholar]
- 41.Harrison M, Rigby D, Vass C, Flynn T, Louviere J, Payne K. Risk as an attribute in discrete choice experiments: a systematic review of the literature. Patient 2014;7(2):151–170. [DOI] [PubMed] [Google Scholar]
- 42.Dowd AJ, Schmader T, Sylvester BD, et al. Effects of social belonging and task framing on exercise cognitions and behavior. J Sport Exerc Psychol 2014;36(1):80–92. [DOI] [PubMed] [Google Scholar]
- 43.Parfitt G, Alrumh A, Rowlands AV. Affect-regulated exercise intensity: does training at an intensity that feels ‘good’ improve physical health? J Sci Med Sport 2012;15(6):548–553. [DOI] [PubMed] [Google Scholar]
- 44.Zenko Z, Ekkekakis P, Ariely D. Can You Have Your Vigorous Exercise and Enjoy It Too? Ramping Intensity Down Increases Postexercise, Remembered, and Forecasted Pleasure. J Sport Exerc Psychol 2016;38(2):149–159. [DOI] [PubMed] [Google Scholar]
- 45.Brady T, Murphy L, Beauchesne D, et al. Executive Summary of ASMP/CDSMP Meta-Analyses 2011.
- 46.Resnicow K, McMaster F. Motivational Interviewing: moving from why to how with autonomy support. Int J Behav Nutr Phys Act 2012;9:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coast J, Al-Janabi H, Sutton EJ, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ 2012;21(6):730–741. [DOI] [PubMed] [Google Scholar]
- 48.Coast J, Horrocks S. Developing attributes and levels for discrete choice experiments using qualitative methods. J Health Serv Res Policy 2007;12(1):25–30. [DOI] [PubMed] [Google Scholar]
- 49.Thorgeirsson T, Kawachi I. Behavioral economics: merging psychology and economics for lifestyle interventions. Am J Prev Med 2013;44(2):185–189. [DOI] [PubMed] [Google Scholar]
- 50.Zimmerman FJ. Using behavioral economics to promote physical activity. Prev Med 2009;49(4):289–291. [DOI] [PubMed] [Google Scholar]
- 51.Hall PA, Fong GT. Temporal self-regulation theory: a neurobiologically informed model for physical activity behavior. Front Hum Neurosci 2015;9:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brand R, Ekkekakis P. Affective–Reflective Theory of physical inactivity and exercise: Foundations and preliminary evidence. Ger J Exerc Sport Res 2018;48:48–58. [Google Scholar]
- 53.Graham DJ, Linde JA, Cousins JM, Jeffery RW. Environmental modifications and 2-year measured and self-reported stair-use: a worksite randomized trial. J Prim Prev 2013;34(6):413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ruff RR, Rosenblum R, Fischer S, Meghani H, Adamic J, Lee KK. Associations between building design, point-of-decision stair prompts, and stair use in urban worksites. Prev Med 2014;60:60–64. [DOI] [PubMed] [Google Scholar]
- 55.Thaler RH, Sunstein CR. Nudge: Improving decisions about health, wealth, and happiness New York: Penguin Books; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


