Abstract
Background
A clitoral frenuloreduction surgical intervention has not been described in the medical literature and through clinical-scientific research, a new surgical clitoral frenuloreduction intervention was developed. This procedure is based on the new anatomical discovery of the clitoral infrafrenulum fascial bundle, which is the deep stratum of the clitoral frenulum.
Methods
A descriptive case series clinical research was designed with objectives to: develop a new clitoral frenuloreduction surgical intervention; evaluate surgical outcomes; assess the impact of this operation on genital self-perceived body image; female sexual activities; and to record complications. The primary outcome measured the ability to implement a new clitoral frenuloreduction surgical intervention. The secondary outcome measured: surgical outcome; the impact of this operation on external genital self-perceived body image; female sexual activities; quality of life; and recording potential complications. The validated instruments were used in the study.
Results
A clitoral frenuloreduction surgical intervention was executed in the procedure room on an outpatient basis under local anesthesia with light conscious sedation (oral Valium and Phenergan rectal suppositories). No complications were recorded. Three-consecutive women were subjected to a new clitoral frenuloreduction surgical procedure. The average time of surgery was 27 minutes. Improvement of sexual activities, quality of life, self-perceived body image, social life, and no feelings of regret of undergoing surgery was recorded.
Conclusions
In the current study, clitoral frenuloreduction was easy to implement without complications and with very pleasing aesthetic surgical outcomes. Self-perceived body image, quality of life, and sexual activities improved.
Keywords: Reproductive medicine, Surgery
1. Introduction
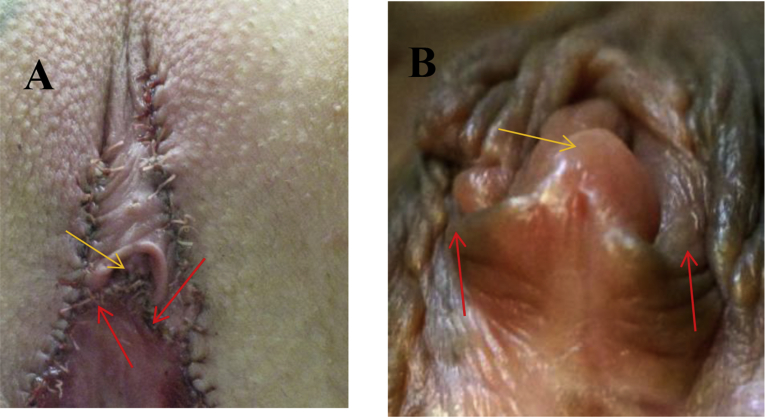
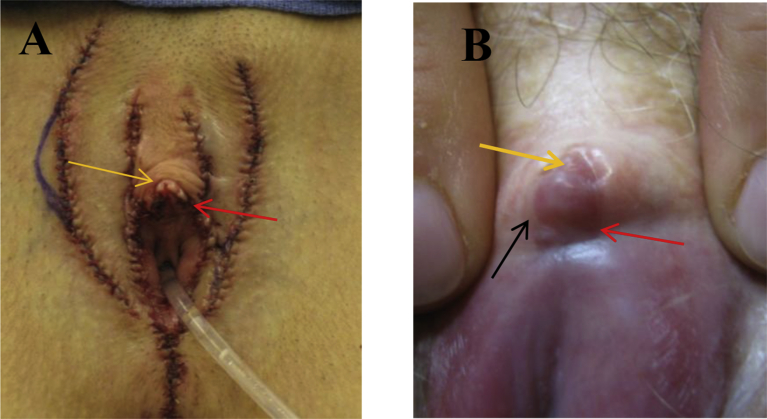
Recently, Ostrzenski discovered the existence of the clitoral infrafrenulum fascial bundle anatomical structure, which creates the deep layer of the clitoral frenulum [1]. This discovery was incorporated into the current clinical-scientific research in which a new clitoral frenuloreduction surgical intervention was developed. Disrupting this anatomical structure during surgery leads to severe complications of the clitoral stabilizing mechanism, particularly, the clitoral glans stability, Figs. 1 and 2. A new surgical concept of frenuloreduction was to minimize or eliminate severe surgical complications.
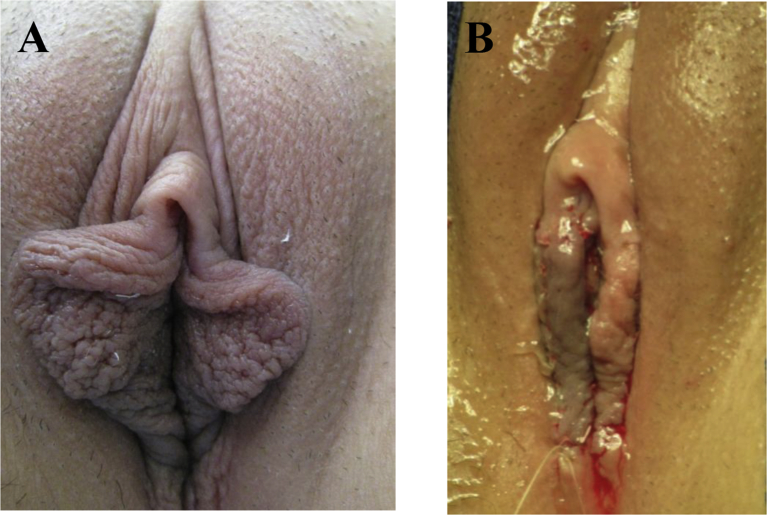
Fig. 1.
Used with permission from original surgeons who requested consultations. A. The immediate postoperative image depicts severe complications resulted from over-resection of the clitoral frenula with clitoral infrafrenulum fascial bundles (the red arrows) and partially resecting the posterior clitoral glans (the yellow arrow). The clitoral glans is elevated and retracted. The clitoral prepuce is rippling with wrinkles and irregular appearance. The clitoral preputial orifice wide opened and gapping. The fragment of over-resected labia minora is also visible. B. Post corrective surgery on the clitoral frenulum is presented. The partially amputated clitoral frenulum was reattached to the lateral aspect of the labia minora (the red arrows) creating unnatural and permanent surgical fusion between the clitoral frenula and the upper part of the labia minora. After the corrective surgery, the clitoral glans is elevated, facing upward, and retracted (the yellow arrow). The elevated and retracted clitoral glans exposed the clitoral root (the area between the clitoral glans and the external urethral meatus area) and such a skin exposure caused severe dryness, pruritus, and skin wrinkling of this area.
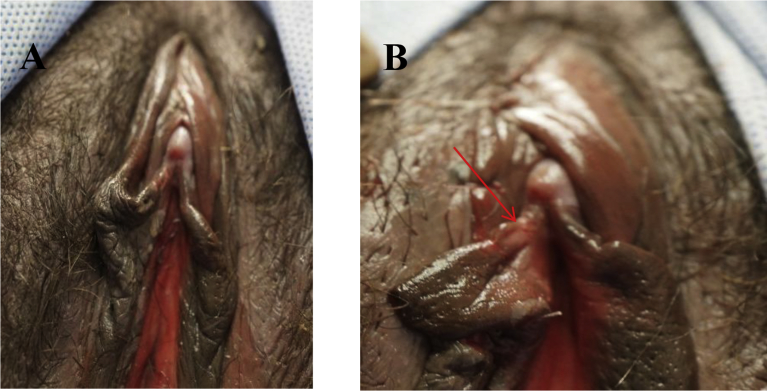
Fig. 2.
Used with permission from original surgeons who requested consultations. A. The immediate postoperative image depicts severe complications resulted from inadvertently removing clitoral frenula with the infrafrenulum fascial bundle of the clitoris. The yellow arrow shows the partially everted clitoral glance and the retracted clitoral prepuce after total resection of the clitoral frenula and labia minora. The red arrow indicates posterior clitoral glans partially resected and the resected clitoral frenulum. B. Two year after the original surgery. Iatrogenic fusion resulted from clitoral hoodoreduction and clitoral frenuloreduction. The anterior clitoral glance is fused with the inner surface and this fusion precludes the clitoral hood natural from natural ability to retract as well as it causes severe pain at the time of clitoral engorgement. The clitoral frenula resected (the red arrow) and unnaturally fuses with the clitoral glans and the inners surface of the clitoral prepuce (the black arrow). The clitoral glance was partially resected.
Typically, the clitoral frenulum is described as one stratum skin fold and in the form of band-like anatomical structure. The upper part of the labium minus divergences anteriorly into two branches: 1) the superior branch of the labium minus is termed as the clitoral prepuce; 2) the inferior branch is labeled as the clitoral frenulum. The proximal clitoral frenulum structure inserts into the posterior surface of the clitoral glans and the distal part connects with the labium minus bifurcation area [2, 3, 4]. The distal clitoral prepuce is laterally adjacent to the clitoral frenulum. Neither the anatomical function of the clitoral frenulum nor the description of the deep stratum of the clitoral frenulum was presented in the medical literature or textbooks. A surgical clitoral prepucioplasty technique for aesthetic motives was described by Alter and termed as central V-plasty with extension [5]. Ostrzenski developed a new clitoral hoodoplasty surgical intervention. This surgical procedure was labeled as hydrodissection with reverse V-plasty [6]. However, a clitoral frenuloreduction surgical technique has never been described in the medical literature.
The clitoral frenulum hypertrophy, asymmetry in length or in width, or thickness, asymmetrical attachment to the clitoral glans, or unnatural fusions with the neighboring anatomical structures can be responsible for a woman's negative self-perceived body image of external genitalia. Therefore, to meet a woman's aesthetic expectation, a female genital cosmetic surgery is performed on the clitoral frenulum without the anatomical appreciation of the clitoral stabilizing mechanism existence and surgical injuro of this mechanism leads to severe, but avoidable, complications. The most commonly observed complication resulted from clitoral frenuloreduction is related to severing the infrafrenulum fascial bundle of the clitoris, which leads to clitoral glans losing anatomical stabilizing support, Figs. 1 and 2.
In the view of the British's audit, cosmetic gynecologic surgical interventions are on the rise; therefore, the number of frenuloreduction or frenuloplasty is also on the rise [7]. Consequently, developing a new surgical intervention(s) for the clitoral frenulum surgical reduction is the necessity in order to minimize or eliminate surgical severe complications.
The objectives of this clinical descriptive case series study were to develop and to implement a new surgical intervention of clitoral frenuloreduction with the primary outcome measured the ability to implement this newly developed procedure, and the secondary outcome measured aesthetic surgical outcomes, the impact of this operation on external genital self-perceived body image, impact on female sexual activities, impact on quality of life, and to report potential intraoperative and postoperative complications.
2. Materials and methods
2.1. Study design and eligibility criteria
A long-term (60 months), postoperative follow-up has been conducted. Eligibility criteria included the presence of anatomical aberrations of the clitoral frenulum, which negatively affect the overall aesthetic look and cause emotional symptoms (aesthetic dissatisfaction from the external genital appearance; decreased self-perceived body image; and feeling of being an inadequate woman). Such a clinical screening allows selecting a candidate for type I, for type II or for type III clitoral frenuloreduction. Those subjects who were pregnant, suffer from clinical depression, autoimmune disorders, and underwent a prior surgery on external genitalia were excluded from this study.
Subjects sexual activities, self-perceived body image, and quality of life were evaluated with a validated, multidimensional, self-reported Female Sexual Function Index (FSFI) questionnaire [8]. Surgical outcome results were determined and reported by women to the examining physicians. The FSFI test was applied pre-operatively, 6-month, 2-year and 5-year post-operative period. Postoperative examination and FSFI tests were conducted in the office of referring physicians. The doctors' notes and the results of validated FSFI questionnaire were sent back to the author in the sealed envelope. The Ethics Committee approved the study's protocol (AKBE 146/12).
2.2. Informed consent
The subjects were advised that the clitoral frenuloreduction was a new surgical intervention and could not be considered as a routine, accepted or standard operation; no promises were made that this procedure can enhance subjects' sexual gratification. Written informed consent was prepared within the standards delineated by the American College of Obstetricians and Gynecologists and was signed by both the subject and the witness [9]. The clitoral frenuloreduction was performed under local anesthesia with light conscious sedation. An informed consent for the local anesthesia was also obtained. An authorization for taking digital images and their potential distributions in the clinical-scientific literature as well as to utilize them for educational purposes were obtained from each subject.
2.3. Local anesthesia
The frenuloreduction procedure was executed under local anesthesia with light conscious sedation by administrating 2. 5 -5 mg Valium orally and 12.5 mg Phenergan suppository rectally for light conscious sedation, thirty-minutes before surgery. One hour before surgery, a thick layer of Lidocaine-Prilocaine (2.5%/2.5%) cream was applied to the clitoral glans, the clitoral prepuce, the clitoral frenula, the intra-labial crease and immediately adjacent areas of the labia minora and labia majora. After applying the cream, the region was covered with sterile gauze. Also, thirty-minutes before the procedure, an ice pack was added to the vulvar area and was resting on the sterile gauze. Upon removing the ice pack and wiping-off remaining anesthetic cream, the operative field was prepped with skin cleanser solution. Lidocaine 1% solution was injected using a 27 G x 1/2-inch needle to the perineal nerve and the posterior labial nerves. The anterior labial branch of the ilioinguinal nerve, the distal part of the perineal branch of the posterior femoral cutaneous nerve, and the distal part of the dorsal clitoral nerve were infiltrated with Lidocaine 1% at the half-way point between the insertion of the clitoral frenulum and the inguinal crease.
2.4. Surgical technique
Clinically, clitoral frenulo reduction can be classified into three different types:
type I, clitoral frenuloreduction by superficial stratum partial resection, Figs. 3, 4, and 5;
type II, clitoral frenuloreduction by both strata, the skin and the infrafrenulum fascial bundle of the clitoris, partial resections were performed, Fig. 6;
type III, clitoral frenuloreduction executed in two phases: phase 1, surgical dissection of the clitoral frenulum from intimate fusions with adjacent anatomical structure and phase 2, the application either a type I procedure or a type II procedure, Fig. 8.
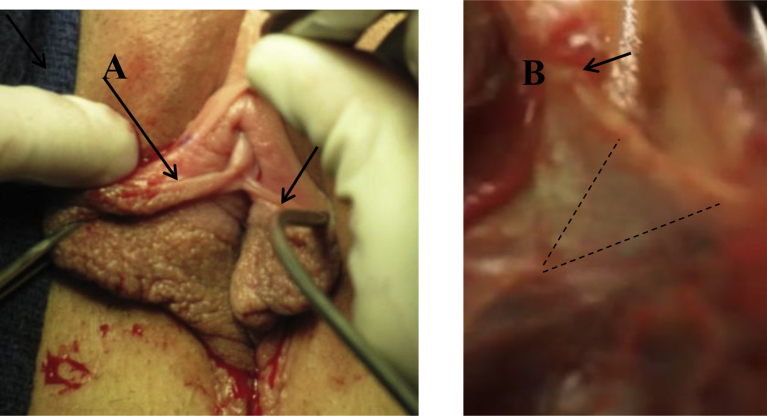
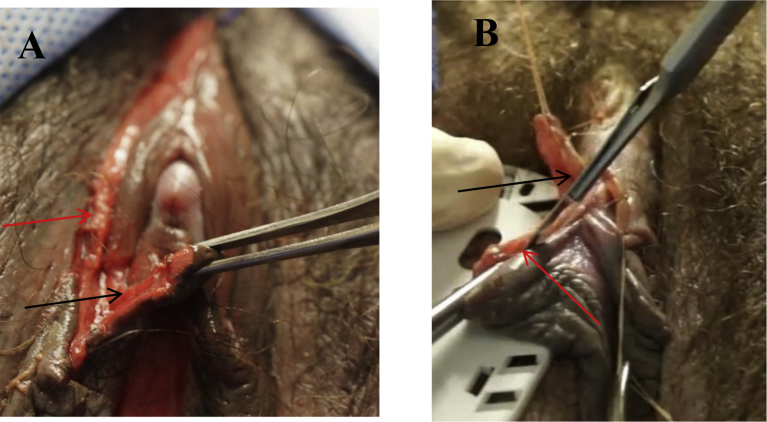
Fig. 3.
The clitoral frenulum and the infrafrenulum fascial bundle are presented. A. The case asymmetrical clitoral frenulum is presented. The right clitoral frenulum is much longer and thicker than left and is fused with the inner labium minus surface (black arrows indicate the superficial layer of the both clitoral frenula). B. The clitoral frenulum superficial stratum was removed and the clitoral infrafrenulum fascial bundle is depicted (clitoral frenulum deep stratum). Black dot-lines indicate the excision of the superficial stratum and emerging deep stratum (the clitoral infrafrenulum fascial bundle) are presented. The predetermined reduction of both strata of clitoral frenula is carried-out (black dot-lines).
Fig. 4.
Clitoral frenuloreduction type I is displayed. A. Two-sutures ware placed laterally and superficially on the skin of the clitoral prepuce for retraction (yellow arrows). The incision was made on the labium minus to get access to Fusion between the right distal clitoral frenulum and labium minus as well as to create de novo the labium minus bifurcation. B. A tong depressor was used to protect surrounding tissues from inadvertent surgical injury. Separation of the right clitoral frenulum from the labium minus unnatural fusion is executed and followed by the length and thickness reductions. The black arrow points to the reduced length and thickness of the right clitoral frenulum. The partially resected superficial layer (the skin) and deep stratum (the infrafrenulum fascial bundle of the clitoris) were done. The length of the right clitoral frenulum was reduced to match the length of the left clitoral frenulum.
Fig. 5.
The external genitalia before and after the surgery are exhibited. A. The external genitalia appearance before surgery. B. The same subject is depicted after surgery. Clitoral frenuloplasty, clitoral preputial reconstruction, and labioreduction of the labia minora were executed. To minimize the male scrotum-like appearance of the labia minora, fenestration labioreduction was performed without preserving the original labial contour. The new counter was established and the natural edges were preserved.
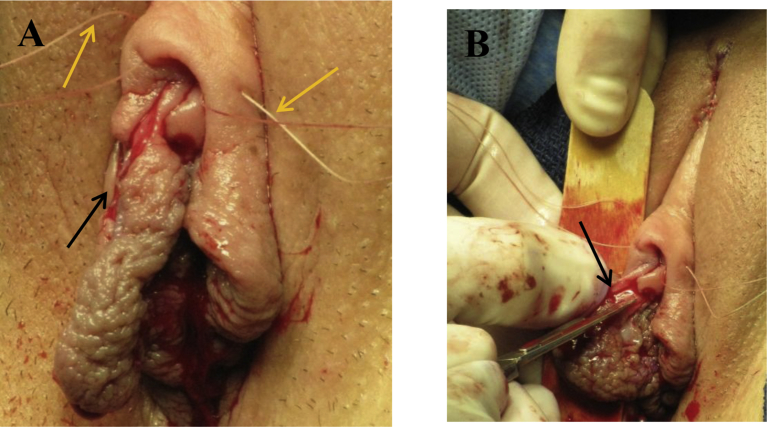
Fig. 6.
Unnatural suspension and fusion of the right clitoral frenulum is depicted. A. The clitoral frenulum together with the labium minus and the redundant clitoral prepuce create a pocket (the red arrow). The packet is suspended by preputial band-like tissue (the black arrow). B. Multiple and different in sizes, small structures whitish in color are present in the packet (the white circle). These casts were consisted of dry-hard materials and were loosely adhered to surrounding tissue with producing offensive odor (the white circle).
Fig. 8.
The right clitoral frenulum anatomical aberrations before and after surgery are depicted. A. External genitalia with multiple anatomical aberrations before surgery is presented. B. After clitoral frenuloreduction and frenuloplasty and have been completed (the red arrow).
In all types of frenuloreductive procedures, 4-0 Chromic sutures were temporarily placed on the lateral aspects of the clitoral prepuce for retraction, Fig. 4A. The skin edges were approximated by simple interrupted sutures using with 5-0 Chromic suture on a small taper needle. Additionally, a squeezable rubber ball syringe (a bulb syringe) filled with body temperature normal saline solution was used for irrigation throughout the procedure to avoid rubbing effects on the tissues from surgical sponges.
2.4.1. Type I procedure (the superficial stratum partial resection)
A small elliptical incision was made on the superficial stratum of the right outer surface of the clitoral frenulum, Fig. 3A and the predetermined amount of the superficial frenulum stratum were removed, Fig. 3B. Such a surgically reduced clitoral frenulum on one side was used as a sample to match another side in length, width, and thickness. The deep stratum of the clitoral frenulum was not incorporated into this procedure and by doing so, the integrity of the infrafrenulum fascial bundle of the clitoris was preserved, Fig. 3A.
The absence of the natural labium minus bifurcation requires a de novo creation of it, Fig. 4A. The procedure is performed by making an elliptical incision and removing a slice of tissue from the upper part of labium minus, Fig. 4A. The labial upper branch is creating by surgically approximating the edge-to-edge with the clitoral prepuce. The lower branch is executed the same method as the upper part and is surgically unified with the clitoral frenulum. Both branches were closed separately with single interrupted, 5-0 Chromic suture on a taper needle.
2.4.2. Type II procedure (clitoral frenulum superficial stratum and deep stratum resections)
When the clitoral frenulum one side is longer and thicker than another side, the type II of clitoral frenuloreduction is implemented, Fig. 6. The superficial and deep strata of the clitoral frenulum were resected with no. 15-surgical blade in the reversed V-shape Fig. 6B. The surgical defect of the clitoral frenulum deep stratum was reconstructed by a simple interrupted 4-0 PDS suture on the taper needle. The edges of the clitoral superficial stratum (the skin fold) were approximated by vertical mattress type of suturing with 5-0 Chromic suture on a taper small needle. The clitoral frenulum length and thickness were reduced, Fig. 6A and B.
2.4.3. Type III procedure (two-phases procedure)
The clitoral frenulum unnatural suspension and fusion with the clitoral prepuce and the upper anterior labium minus create a pocket, which was intimately suspended by the preputial band-like tissue and the upper labium minus, Fig. 7A. The packet was filled with multiple and different sizes, small casts, whitish in color structures, Fig. 7B. These small casts produced an offensive odor. In phase I of the procedure, the objective was to release the packet from the fusion, Fig. 8A. A magnifying 3.5–4.0 X surgical loop was utilized for surgical stratum-by-stratum dissections. Sharp surgical dissections were performed with a no. 11-surgical blade, Fig. 8B. The outer part of the right clitoral frenulum superficial stratum was resected to match the left clitoral frenulum, Fig. 8B. The skin edges of the rope-like redundant anatomical structure and clitoral frenulum lateral skin surgical defects were approximated with simple interrupted 5-0 Chromic sutures on a taper small needle, Fig. 8B. A comparison between the preoperative look and the postoperative appearance is presented. The multiple surgical interventions on the clitoral prepuce, the clitoral frenulum, the labia minora, and the labial frenulum were completed, Fig. 8A and B.
Fig. 7.
Clitoral frenuloreduction (type II) is performed in two-surgical phases. A. Phase I, separation of the right clitoral frenulum from the clitoral prepuce band-like skin (the red arrow) and the upper part of the labium minus (the red arrow). B. Phase II, the resection process of the right clitoral frenulum is demonstrated (the red arrow). A white plastic plate from a surgical package was used to protect surrounding anatomical structures from inadvertent injury. The black arrow shows the fragment of the clitoral prepuce and the part of the labium minus.
2.5. Postoperative care
Postoperatively, the subjects reported minimal discomfort that was predominantly managed with external application of Dermoplast®, an antiseptic and pain-relieving container in spray (a red cup container, Medtech, Jackson, WY, U.S.A.). Occasionally, the subjects took acetaminophen 2 tablets as needed. Each patient was instructed how to prevent potential adhesion or fusion formation between adjacent anatomical structures to the clitoral frenula.
3. Results
Three-women were selected for this clinical study and each of them was qualified for a different 3-type of clitoral frenuloreduction Figs. 3A, 6A, and 7. All subject met inclusion criteria and completed 5-year follow-up.
Subject number one was a 27-year-old Caucasian healthy woman, a nurse, G0P0, who was not sexually active due to her external genital unnatural look. She reported aesthetic concerns about her external genital anomalies, which caused her embarrassment and sexual phobia. She pointed out that the most troubling appearance was the upper left labium minus, the clitoris being bulking, and did not look right, Fig. 3A. On physical examination, the right side of the clitoral frenulum was longer, much thinner, and unnaturally fused with the upper part of the right labium minus surface, Fig. 3A. The left clitoral frenulum was shorter and appreciably thicker than the right side, Fig. 3A. She met criteria to be qualified for type I clitoral frenuloplasty (superficial stratum partial reconstruction).
The subject number two was a 20-year-old Caucasian woman, G0P0. Her chief complaint was sexual phobia and low self-perceived body image due to the abnormal look of her external genitalia. She presented with hypertrophic clitoral frenula and the absence labium minus bifurcation causes bilateral inner folding of the labia minora upper edges, Figs. 4A and 5A. The upper fragment of the labium minus migrates into the clitoral hood and fuses laterally to the distal clitoral glans, Figs. 4A, 5A. The right frenulum is much longer and thicker than the left one, Fig. 5A. The posterior surface of the right clitoral frenulum has a brownish color and texture similar to the labium majus when compared the left clitoral frenulum, Fig. 5A. The right and left clitoral frenula are unnaturally elongated. The clitoral frenula were uneven in thickness and created an unnatural groove with the labia minora, Fig. 5A. The frenulum and the distal part of the labia minora were covered by the unnaturally elongated clitoral prepuce, Fig. 5A. There are also identifiable anatomical aberrations of the external genitalia such as the clitoral prepuce presents unnatural cord-like three-structures and clitoral hood banded, Fig. 5A; the hypertrophic, asymmetrical, and the upper part of the labia minora are folded. The general tissue texture of the labia minora resembles the male scrotum and they are unnaturally suspended to the clitoral hood and the clitoral glans, Fig. 5A. This patient was selected for the type II clitoral frenuloreduction (superficial and deep stratum resections).
Subject number three was a 31-year-old Caucasian woman, G0P0, an attorney. Her chief complaint was the absence of interest in sexual activities with any partner due to external genital anatomic aberrations and very offensive odors of the external genitalia, Fig. 7A and B. She extensively used perfumes on the genital area to suppress odors. The subject requested medical consultations form several practitioners for her condition. She received reassurance from doctors that her external genital appearance is “normal variations” and advised her to learn more how to cope with offensive odors and to try different techniques in maintaining her personal hygiene. She also was troubled by the fact that her labia minora were aesthetically unattractive, asymmetric, and had a pocket in which she noticed small, solid cast structures and the area was tender to her touch, underwear, and caused discomfort during bathing, Fig. 7B. Altogether, these anatomic aberrations associated with offensive odors causing disturbances of her physical, emotional, and social well-being as well as causing her embarrassment and sexual social phobia. Due to these complex medical issues, she lost interest in intimate sexual contact. The physical examinations revealed that the right clitoral frenulum being fused with the labia minora and with the clitoral redundant preputial cord-like tissues, Fig. 7A and B. All these structures created a pocket, which was permanently fused with and suspended to unnatural clitoral redundant preputial cord-like tissues, Fig. 7A. Upon stretching the margin-free pocket's edge, “stalagmite-like” multiple small cast structures, white in color, were noted, Fig. 7B. The pocket was filled with small casts structures, which emanated offensive odors. “Stalagmite-like” multiple structures loosely adhered to the inner tissue of the pocket, Fig. 7B; upon removing “stalagmite-like” materials, the area appeared as reactive inflammation within the pocket. Additionally, an unnatural appearance of the reverse triangular-shaped deformity was created by the base of the pocket, Fig. 7A and B. This subject was selected for type III clitoral frenuloreduction (two-phases of surgical intervention).
The clitoral frenuloreduction was easy to execute without technical difficulties and with negligible blood loss. No intraoperative or post-operative short-, or long-term complications were observed. The total FSFI scores prior to clitoral frenulum reconstruction were at the low 2 in all subjects. At the 6-month postoperative follow-up documented increasing sexual activities and these results remained the same until the last testing at 5-year. The subject no. 1 improved from 2 to 29; subject no. 2 improved from 2 to 27; subject no. 3 improved from 2 to 28, Table 1. The FSFI did not differ between 6-month and 5-year. All subjects in this study reported overall sexual activities improvement after surgery. The resolution of physical signs and presenting symptoms of an offensive odor (the subject no. 3) were eliminated by a surgical therapy. Emotional disturbances, social embarrassment, and social phobia subsided. Also, FSFI established that the quality of life improved, Table 1.
Table 1.
Female sexual function index.
| Domain tested | Subject I |
Subject II |
Subject III |
|||
|---|---|---|---|---|---|---|
| Time point |
Time point |
Time point |
||||
| Before | 6-month After | Before | 6-month After | Before | 6-month After | |
| Desire | 2 | 6 | 2 | 5 | 2 | 6 |
| Arousal | 0 | 6 | 0 | 5 | 0 | 4 |
| Lubrication | 0 | 6 | 0 | 6 | 0 | 6 |
| Orgasm | 0 | 5 | 0 | 5 | 0 | 6 |
| Satisfaction | 0 | 6 | 0 | 6 | 0 | 6 |
| Pain | 0 | 0 | 0 | 0 | 0 | 0 |
| Full scale score | 2 | 29 | 2 | 27 | 2 | 28 |
All subjects reported increased interest in a frequency of sexual activities due to increased self-perceived body image. Postoperatively, all subjects gave a very high grade for aesthetic and functional outcomes and reported no feelings of regrets in subjecting themselves to the operation. Additionally, all patients noticed the meaningful improvement in their self-perceived body images.
Electronic and manual searches documented that the concept of these surgical interventions for clitoral frenuloreduction was the first description in the scientific-clinical medical literature. Also, the study determined that there is no standard approach to clitoral frenuloreduction, and the procedure must be tailored to meet a woman's individual aesthetic expectation.
4. Discussion
The current intraoperative study verified the anatomical existence of the newly discovered clitoral infrafrenulum fascial bundle (the deep clitoral frenulum stratum) within the clitoral frenulum [1]. This anatomical structure plays an important role in the clitoral anatomical stabilizing mechanism, Figs. 1 and 2. Severing this structure leads to severe clinical complications within the clitoral anatomical stabilizing mechanism, Figs. 1 and 2. The clitoral frenulum anatomy was not addressed adequately in the medical literature or textbooks, or surgical atlases [2, 3, 4, 10, 11] and surgeons were operating on the clitoral frenulum without the knowledge of infrafrenulum fascial bundle existence, Figs. 2 and 3. Additionally, this study established that clitoral frenulum can be unnaturally fused with neighboring anatomic structures, Figs. 7A, 8A and can create an unnatural pocket, Fig. 7A and B. This packet can retaine debridement, Fig. 7B, which are able to produce offensive odors.
The current clinical-scientific presentation illustrates that surgery executed correctly on the female external genitalia can play a meaningful role in the improvement of sexual activities, quality of life, self-perceived body image, and improved social intimate function. Subjects presented here represented different anatomic aberrations of the clitoral frenulum Figs. 3A, 5A, 6A and 7. Retained smegma mixed with debris (exfoliated cells and soap) within the pocket was responsible for very offensive odors (case no. 3). In the no. 2 case, the labia minora migrate into the clitoral hood and the upper part of the labia minora was unnaturally folded bilaterally, Fig. 5A.
Preserving anatomical integrity of the deep stratum of the clitoral frenulum is the surgical concept of the clitoral frenuloreduction. The three-subtypes of clitoral frenuloreduction reflect different anatomical layers being reconstructed. The case no.1 exemplifies partial resections of the superficial stratum (the cutis) with preservation of the clitoral frenulum deep stratum (the infrafrenulum fascial bundle), Fig. 3. The case no. 2 illustrates surgical partial resections of both, superficial and deep strata of the clitoral frenulum, Fig. 6. The case no. 3 demonstrates the need of two-phases of clitoral frenuloreduction, Fig. 8. In phase I, the clitoral frenulum is released from unnatural fusion(s) and suspensions to create surgical access to the clitoral frenulum, Fig. 8A. In phase II of the frenuloreduction, either type I or type II clitoral frenuloreduction, is selected and executed, Fig. 8B.
At the commencement of this study, subjects reported low sexual desire, difficulty to get sexually arouse and decrease the ability to reach orgasms, Table 1. When the hypoactive sexual desire phase is present, the sexual arousal phase can also be low, since both of these phases of the female sexual response cycle demonstrates the highest correlation [8]. In the current study, the sexual arousal phase was tested by lubrication, which was examined by FSFI and presented in Table 1 [8]. When the initial desire phases and aerosol phase were low, the orgasmic phase was either delay or absence [8].
The present investigation did not study the desired phase specific components such as sexual fantasies or sexual aversion. The sexual arousal phase was studied by evaluating only lubrication and not engorgement or ability to maintain it. Additionally, the orgasmic phase was not evaluated from the perspective of delay or different orgasmic origins (mental, clitoral, vaginal, cervical or anal). Since female sexual response cycle incorporates both emotional and organic aspects and both translate into timing, sequencing, and coordinating of sexual several phases. To determine all these aspects of female response cycle was beyond the scope of this clinical investigation. Simply, the current study protocol calls for establishing a hint whether a female clitoral frenuloreduction surgery plays a role in improving overall sexual activities in women.
A surgical severing of the infrafrenulum fascial bundle of the clitoris causes severe complications, which include the clitoral glans and body lose stability, the clitoral prepuce bends and elevates as well as the clitoral unnatural upward and lateral hypermobility occur, Figs. 1 and 2. The clitoris is naturally an immobile organ, therefore, to create iatrogenic clitoral hypermobility interferes with a woman's sexual life. Such complications create not only anatomic iatrogenic disfigurements, Figs. 1 and 2, but also cause pain and difficulties in clitoral stimulations. To perform corrective surgery for these types of complications is technically very demanding since reconstruction is executed on the retracted, fibrotic infrafrenulum fascial bundle, and in the close vicinity of the vestibule vaginal bulbs. The clitoral frenulum functional anatomy plays a significant role in stabilization of the clitoris. The gross anatomy of the clitoral frenulum has significant input on the overall aesthetic appearance of the human female external genitalia.
4.1. Limitations and strength of the study
The weakness of this study is the small sample size; however, the university Esthetics Committee suggested to limit the number of subjects to three and to treat this study as preliminary research. The subjects of this research represent most common anatomical aberrations of the clitoral frenulum and numbers were sufficient to answer a leading question of the study whether the newly developed frenuloreduction surgical intervention is able to be surgically implemented and cures symptoms. The present study was not specifically designed to establish causation of low desire phase, low arousal phase, and decreased the ability to reach orgasms or to determine the hierarchy of any female response cycle phase inhibition.
The strength of this study is the intraoperative confirmation of the clitoral infrafrenulum fascial bundle existence and establishing the anatomical role of clitoral frenulum in the stabilizing mechanism as well as understanding the function of the infrafrenulum fascial bundle of the clitoris. A new frenuloreduction intervention assists to minimize or to eliminate severe complications relating to injuries of the deep stratum of the clitoral frenulum.
5. Conclusions
In the current study, clitoral frenuloreduction was easy to implement without complications and with pleasing aesthetic surgical outcomes. Self-perceived body image, quality of life, and sexual activities improved. An additional study(s) is needed to establish a correlation between female genital cosmetic-plastic surgeries and self-perceived body image, quality of life and sexual function.
Declarations
Author contribution statement
Adam Ostrzenski: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Ostrzenski A. The clitoral infrafrenulum fascial bundle: the Anatomy and histology. Clin. Anat. 2018 Jun 5 doi: 10.1002/ca.23215. [DOI] [PubMed] [Google Scholar]
- 2.Clemente C.D. U.S.A. Lea & Febiger; Philadelphia, PA: 1985. Gray's Anatomy. 30th American Edition; p. 1580. [Google Scholar]
- 3.Netter F.H. Ciba-Geigy Corporation; West Caldwell, NJ, U.S.A.: 1989. Atlas of Human Anatomy; pp. 354–356. [Google Scholar]
- 4.Rock J.A., Jones H.W., editors. Te Linde's Operative Gynecology. eleventh ed. Wolters Kluwer; Philadelphia, PA, U.S.A.: 2015. pp. 93–94. [Google Scholar]
- 5.Alter G.J. Aesthetic labia minora and clitoral hood reduction using extended central wedge resection. Plast. Reconstr. Surg. 2008;122:1780–1789. doi: 10.1097/PRS.0b013e31818a9b25. [DOI] [PubMed] [Google Scholar]
- 6.Ostrzenski A. A new, hydrodissection with reverse V-plasty technique for the buried clitoris associated with Lichen Sclerosus. J. Gynecol. Surg. 2010;26:41–48. [Google Scholar]
- 7.Audit British Association of Aesthetic Surgeons. www.baaps.org.uk. 2010 (accessed 12, 23, 2018).
- 8.Rose R., Brown C., Heiman J., Leiblum S., Meston C., Shabsigh R., Ferguson D., D'Agostino R. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J. Sex Marital Ther. 2000;26(2):191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 9.ACOG Committee Opinion No. 390. Ethical Decision Making in Obstetrics and Gynecology. The American College of Obstetrics and Gynecology; Washington, D.C., U.S.A.: December 2007. [DOI] [PubMed] [Google Scholar]
- 10.O'Connell H.E., Sanjeevan K.V., Hutson J.M. Anatomy of the clitoris. J. Urol. 2005 Oct;174(4 Pt 1):1189–1195. doi: 10.1097/01.ju.0000173639.38898.cd. [DOI] [PubMed] [Google Scholar]
- 11.Baggish M.S., Karram M.M. WB Suonders Company; Philadelphia, PA. U.S.A.: 2001. Atlas of Pelvic Anatomy and Gynecologic Surgery; pp. 530–537. [Google Scholar]